Abstract
Purpose
To investigate whether cardiovascular drug classes and specific beta-blockers are associated with antidepressant drug use in a large study population of older people.
Methods
We analyzed data from the Swedish Prescribed Drug Register from October-December 2005 for people aged 75 years and older (n = 732,230). Logistic regression analysis was used to study the association between the cardiovascular drugs and antidepressants, after adjustment for age, sex, and number of other dispensed drugs.
Results
All the cardiovascular drug classes were negatively or not associated with use of any antidepressant, non-selective monoamine reuptake inhibitors, and SSRIs, after adjustment for age, sex, and number of other dispensed drugs. However, propranolol was associated with an increased use of any antidepressant, non-selective monoamine reuptake inhibitors, and SSRIs, after adjustment for age, sex, and number of other dispensed drugs. Atenolol was positively associated with non-selective monoamine reuptake inhibitors, although to a lesser extent than propranolol.
Conclusions
None of the cardiovascular drug classes were associated with increased antidepressant drug use, after adjustment for age, sex, and use of other drugs. However, when focusing specifically on beta-blockers, our results indicate that propranolol may be the beta-blocker most closely associated with use of antidepressants in the elderly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many cardiovascular drugs have been postulated to have depressive symptoms as side effects. However, with the exception of beta-blockers, few of these drugs have been epidemiologically studied in relation to depression outside the controlled environment of the clinical trial [1, 2]. Nevertheless, digitalis, diuretics, calcium-channel blockers, angiotensin converting enzyme (ACE) inhibitors, and lipid-lowering agents have been associated with depression [2–7], although this has been disputed by others [3, 4, 7–9]. Regarding studies on beta-blockers and depression, the results are inconsistent [3, 4, 10–13], and this matter is still open for debate. In particular, the lipophilic beta-blocker propanolol has been suggested to be linked to depression [4, 11, 12, 14]. However, many of the studies on cardiovascular drugs and depressive symptoms were conducted quite a few years ago, used small study samples, did not adjust for any measure of comorbidity, and focused on beta-blockers. Therefore, we wanted to provide an updated analysis on the association between different cardiovascular drugs and antidepressants in a nationwide study population.
Depression and depressive symptoms are common disorders among older people and decrease their quality of life, impair functional abilities, and increase use of health care. Drug-induced depression might be a potentially preventable cause of depressive symptoms in the elderly [3], and cardiovascular drugs are among the most frequently used drugs among older people [15, 16]. Thus, if cardiovascular drugs cause depression in the elderly, a great deal of suffering and costs related to depression could be saved by alternative solutions. On the other hand, older people should not be denied valuable cardiovascular drug therapy due to unjustified reluctance to prescribe these drugs due to fear of depressive side effects.
The aims of this study were to investigate whether (1) cardiovascular drug classes (i.e., digitalis, thiazide diuretics, loop diuretics, potassium-sparing diuretics, beta-blockers, calcium-channel blockers, ACE inhibitors, angiotensin II antagonists, and lipid-lowering agents) and (2) specific beta-blockers (according to lipophilicity) are associated with antidepressant drug use [i.e., any antidepressant, non-selective monoamine reuptake inhibitors, and selective serotonin reuptake inhibitors (SSRIs)] in a large study population of older people.
Methods
Study population
The Swedish Prescribed Drug Register (SPDR) contains data with unique personal identification numbers of all dispensed prescriptions to the whole population of Sweden (about 9 million inhabitants). The data collection is administered by the state-owned National Corporation of Swedish Pharmacies and then transferred to the Centre for Epidemiology at the National Board of Health and Welfare, responsible for keeping the register [17]. The SPDR is intended for epidemiological studies, research, and statistics within the health-care area.
We analyzed nonidentifiable data from individuals aged 75 years and older who were registered in the SPDR during October-December 2005, with information about every individual’s age, sex, and dispensed drugs [Anatomical Therapeutic Chemical (ATC)-code [18], amount of prescribed drug, when the prescription was filled, and prescribed dosage (i.e., from the prescriptions written by the prescribers)]. The study population consisted of 732,230 older people.
First, information from the 3-month period about when the prescription was filled, amount of drug, and prescribed dosage was processed to calculate the duration of drug exposure [19]. When prescribed dosage was incomplete or missing, we used defined daily doses (DDDs) [18] for calculation of the duration of drug exposure. We assumed 0.9 DDDs for regularly used drugs (based on calculations for regularly used drugs among the elderly in the database) and 0.45 DDDs (50% of 0.9) for drugs prescribed as needed, as indicated on the prescription. We assumed 1 DDD for drugs for external use and for the eye. Second, a list of current prescriptions was constructed based on the calculations of the duration of drug exposures for every individual on the arbitrarily chosen date of December 31, 2005. If a person was dispensed the same drug in different doses during the study period, it was counted as one dispensed drug [20].
This study was approved by the ethical board in Stockholm (Dnr 2006/948–31).
Definitions
Use of any antidepressant was defined by the ATC-code N06A and subdivided into non-selective monoamine reuptake inhibitors (N06AA) and SSRIs (N06AB) because these two types of antidepressants may be used differently [21–24].
The cardiovascular drugs classes were digitalis (C01AA), thiazide diuretics (C03A), loop diuretics (C03C), potassium-sparing diuretics (C03D), beta-blockers (C07A), calcium-channel blockers (C08), ACE inhibitors (C09A), angiotensin II antagonists (C09C), and lipid-lowering agents (C10A). The beta-blockers were classified according to their lipophilicity [25] into high [propranolol (C07AA05) and carvedilol (C07AG02)], moderate [pindolol (C07AA03), metoprolol (C07AB02), and labetalol (C07AG01)], and low lipophilicity [sotalol (C07AA07), atenolol (C07AB03), and bisoprolol (C07AB07)].
Age was used as a continuous variable.
Number of other dispensed drugs (a proxy for comorbidity [26–28]) was also a continuous variable and consisted of the number of dispensed drugs used by the person other than the specific cardiovascular drug and antidepressant under study.
Statistical analysis
Multivariate logistic regression analysis was used to study the association between the cardiovascular drugs and antidepressants. In model i, we adjusted for age and sex, and in model ii, we also included number of other dispensed drugs.
The results are shown as odds ratios (ORs) with 95% confidence intervals (CIs). SPSS 14.0 for Windows (SPSS, 1989–2005) was used for the analyses.
Results
Mean age among the 732,230 elderly was 82.1 years. They received on average 5.4 dispensed drugs per person, and 61.6% were women (Table 1).
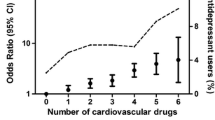
At least one antidepressant was used by 15.2% of the study population, including non-selective monoamine reuptake inhibitors by 1.6% and SSRIs by 11.3%. Cardiovascular drugs were used by 66.4%. Among the cardiovascular-drug users, 15.6, 1.6, and 11.7% used any antidepressant, non-selective monoamine reuptake inhibitors, and SSRIs, respectively. The most frequently used cardiovascular drug class was beta-blockers (35.1%), followed by loop diuretics (24.9%), calcium-channel blockers (16.9%), lipid-lowering agents (16.7%), and ACE inhibitors (14.4%) (Table 1).
Digitalis, loop diuretics, and potassium-sparing diuretics were positively associated with any antidepressant, non-selective monoamine reuptake inhibitors, or SSRIs, after adjustment for age and sex (Table 2). However, after additional adjustment for number of other drugs (i.e., a proxy for comorbidity), all the cardiovascular drug classes were negatively or not associated with antidepressants. Regarding the different beta-blockers, propranolol was associated with any antidepressant, non-selective monoamine reuptake inhibitors, and SSRIs, including after additional adjustment for number of other drugs. Sotalol, atenolol, and bisoprolol were weakly associated with antidepressants, non-selective monoamine reuptake inhibitors, or SSRIs, after adjustment for age and sex. However, after additional adjustment for number of other drugs, the only remaining association was between atenolol and non-selective monoamine reuptake inhibitors.
In addition, we studied interactions in the different analyses. However, due to the large study sample and, hence, great statistical power in the analyses, many interactions were statistically significant, although not necessarily clinically significant. Noteworthy, there was an interaction between loop diuretics and number of other drugs [any antidepressant: ORloop diuretics × number of other dispensed drugs = 0.95 (95% CI 0.95–0.96)], with the interpretation that those who used fewer other drugs had a positive association between loop diuretics and antidepressants and those who used several other drugs had a negative association between loop diuretics and antidepressants.
Discussion
Main findings
In our large study population of older people, none of the cardiovascular drug classes were associated with an increased use of antidepressants, after adjustment for age, sex, and use of other drugs (i.e., a proxy for comorbidity). Thereby, our results support the previous reports claiming that there is no evidence that digitalis, diuretics, calcium-channel blockers, ACE inhibitors, and lipid-lowering agents cause depressive symptoms [1, 3, 4, 7–9]. However, there is also research supporting depressive effects of these cardiovascular drugs [2–7]. In general, the studies in this field are quite old, have used small study samples, have not controlled for any measure of comorbidity, or have relied on case reports.
The relationship between beta-blockers, in particular propranolol, and depression has been more extensively studied [3, 4, 10–12]. There is both evidence for [4, 12, 14] and against [2, 13] an association between propranolol and depressive symptoms. In other words, the issue of propranolol has not yet been resolved, and more large-scale studies comparing different beta-blockers are needed [11]. We observed that propranolol, but not beta-blockers in general [2, 4, 6, 10, 11, 28], was associated with use of any antidepressant, non-selective monoamine reuptake inhibitors, and SSRIs, after adjustment for age, sex, and use of other drugs. Moreover, atenolol was associated, although more weakly than propranolol, with non-selective monoamine reuptake inhibitors, after adjustment for age, sex, and use of other drugs. One suggested explanation for the relationship between beta-blockers and depression has been that these drugs alter noradrenergic activity in the brain. In that case, propranolol would be the beta-blocker most likely to cause depression because propranolol is the most lipophilic beta-blocker and, therefore, most likely to cross the blood-brain barrier [12]. However, this lipophilic hypothesis was not entirely supported by our data, as the hydrophilic beta-blocker atenolol was associated with non-selective monoamine reuptake inhibitors, although to a lesser extent than propranolol. An alternative explanation for our finding may be that propranolol is used among the elderly to a higher extent for other indications possibly related to depression, e.g., tremor and migraine, than the other beta-blockers.
Limitations
The cross-sectional design of our study does not allow us to draw conclusions regarding causality. Also, confounding by indication is difficult or even impossible to avoid in pharmacoepidemiological studies [2]. Unmeasured confounding may provide an alternative explanation for our findings. However, we did control for a proxy for comorbidity (i.e., number of other dispensed drugs) [26–28], regarded as one of the most important confounders, particularly in studies of older people with multiple medical conditions [11]. Further, older people may be prescribed antidepressants, especially non-selective monoamine reuptake inhibitors, for other reasons than depression, e.g., sleep disturbances and chronic pain [21], which may result in misclassification. Therefore, we subdivided the antidepressants into non-selective monoamine reuptake inhibitors and SSRIs.
We have used data on elderly registered in the SPDR during October-December 2005, corresponding to 92% of the population 75 years and older in Sweden [29]. The SPDR does not include data on over-the-counter drugs, herbal drugs, and drugs used in hospitals. Also, the register is incomplete with regard to drugs used in nursing homes, which may lead to an underestimation of the drug use. Moreover, our method is built on an assumption that all current drugs were dispensed during the observed 3-month period, which is based on the fact that drugs are prescribed for use for at most 90 days in Sweden. In this way, we might miss drugs that were dispensed before the 3-month period and used at a slower rate than intended. At the same time, we might include drugs that were dispensed during the 3-month period but discontinued prematurely. In addition, our method is built on interpretations of the entries describing the dispensed drugs’ dosages, as well as assumptions about DDDs when the information about dosage was incomplete or missing [19, 30]. Finally, a general limitation of studies on drug registers is that dispensed drugs may not reflect what is actually used by the patients [31], as the adherence rate may be low [32].
Implications
Until a relationship between different beta-blockers and depression has been established, caution might be exercised when prescribing propranolol to elderly patients with susceptibility to depression.
Previous studies have been severely limited by insufficient number of participants, and larger study samples are necessary to study specific drugs [3]. Large observational studies, such as this one, may complement clinical trials with data from real-world patients who would be excluded from clinical trials due to advanced ages, comorbidities, and multiple drug use [1, 33, 34].
Conclusion
None of the cardiovascular drug classes were associated with increased antidepressant drug use, after adjustment for age, sex, and use of other drugs. However, when focusing specifically on beta-blockers, our results indicate that propranolol may be the beta-blocker most closely associated with use of antidepressants in the elderly, although high lipophilicity may not be the explanation. Future research at large scales is warranted for elucidating the relationship between different beta-blockers and depression.
References
Agostini JV, Tinetti ME, Han L, Peduzzi P, Foody JM, Concato J (2007) Association between antihypertensive medication use and non-cardiovascular outcomes in older men. J Gen Intern Med 22:1661–1667
Hallas J (1996) Evidence of depression provoked by cardiovascular medication: a prescription sequence symmetry analysis. Epidemiology 7:478–484
Kotlyar M, Dysken M, Adson DE (2005) Update on drug-induced depression in the elderly. Am J Geriatr Pharmacother 3:288–300
Patten SB, Barbui C (2004) Drug-induced depression: a systematic review to inform clinical practice. Psychother Psychosom 73:207–215
Okada F (1985) Depression after treatment with thiazide diuretics for hypertension. Am J Psychiatry 142:1101–1102
Schleifer SJ, Slater WR, Macari-Hinson MM et al (1991) Digitalis and beta-blocking agents: effects on depression following myocardial infarction. Am Heart J 121:1397–1402
Ried LD, Johnson RE, McFarland BH, Brody KK (2000) Antihypertensive drug use and the risk of depression among older hypertensives in an HMO. J Pharmacoepidemiol 8:1–28
Dunn NR, Freemantle SN, Mann RD (1999) Cohort study on calcium channel blockers, other cardiovascular agents, and the prevalence of depression. Br J Clin Pharmacol 48:230–233
Patten SB, Williams JV, Love EJ (1995) Self-reported depressive symptoms in association with medication exposures among medical inpatients: a cross-sectional study. Can J Psychiatry 40:264–269
Ko DT, Hebert PR, Coffey CS, Sedrakyan A, Curtis JP, Krumholz HM (2002) Beta-blocker therapy and symptoms of depression, fatigue, and sexual dysfunction. JAMA 288:351–357
Ried LD, McFarland BH, Johnson RE, Brody KK (1998) Beta-blockers and depression: the more the murkier? Ann Pharmacother 32:699–708
Steffensmeier JJ, Ernst ME, Kelly M, Hartz AJ (2006) Do randomized controlled trials always trump case reports? A second look at propranolol and depression. Pharmacotherapy 26:162–167
van Melle JP, Verbeek DE, van den Berg MP, Ormel J, van der Linde MR, de Jonge P (2006) Beta-blockers and depression after myocardial infarction: a multicenter prospective study. J Am Coll Cardiol 48:2209–2214
Johnson JA, Wallace SM (1997) Investigating the relationship between beta-blocker and antidepressant use through linkage of the administrative databases of Saskatchewan Health. Pharmacoepidemiol Drug Saf 6:1–11
Jyrkka J, Vartiainen L, Hartikainen S, Sulkava R, Enlund H (2006) Increasing use of medicines in elderly persons: a five-year follow-up of the Kuopio 75+ Study. Eur J Clin Pharmacol 62:151–158
Silwer L, Lundborg CS, Petzold M (2008) Prevalence of purchase of antihypertensive and serum lipid-reducing drugs in Sweden–individual data from national registers. Pharmacoepidemiol Drug Saf 17:37–42
Wettermark B, Hammar N, Fored CM et al (2007) The new Swedish Prescribed Drug Register–opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf 16:726–735
WHO Collaborating Centre for Drug Statistics Methodology (2008) About the ATC/DDD system. http://www.whocc.no/atcddd/. Accessed 17 July 2008
Lau HS, de Boer A, Beuning KS, Porsius A (1997) Validation of pharmacy records in drug exposure assessment. J Clin Epidemiol 50:619–625
Johnell K, Klarin I (2007) The relationship between number of drugs and potential drug-drug interactions in the elderly: a study of over 600,000 elderly patients from the Swedish Prescribed Drug Register. Drug Saf 30:911–918
Patten SB, Esposito E, Carter B (2007) Reasons for antidepressant prescriptions in Canada. Pharmacoepidemiol Drug Saf 16:746–752
Salzman C (1999) Practical considerations for the treatment of depression in elderly and very elderly long-term care patients. J Clin Psychiatry 60 Suppl 20:30–33
The Swedish Medical Products Agency (2004) Pharmacotherapy in unipolar depression in adults and elderly - treatment guidelines (in Swedish). Information from the Swedish Medical Products Agency 5:2004
Rosholm JU, Andersen M, Gram LF (2001) Are there differences in the use of selective serotonin reuptake inhibitors and tricyclic antidepressants? A prescription database study. Eur J Clin Pharmacol 56:923–929
Hoffman BB (2007) Adrenoceptor antagonist drugs. In: Katzung BG (ed) Basic and clinical pharmacology, 10th ed. McGraw-Hill, New York
Benazon NR, Mamdani MM, Coyne JC (2005) Trends in the prescribing of antidepressants following acute myocardial infarction, 1993–2002. Psychosom Med 67:916–920
Schneeweiss S, Seeger JD, Maclure M, Wang PS, Avorn J, Glynn RJ (2001) Performance of comorbidity scores to control for confounding in epidemiologic studies using claims data. Am J Epidemiol 154:854–864
Bright RA, Everitt DE (1992) Beta-blockers and depression. Evidence against an association. JAMA 267:1783–1787
Statistics Sweden (2005) The population in Sweden according to sex and age 31/12/2005 (in Swedish). SCB, Stockholm
Johnell K, Fastbom J, Rosen M, Leimanis A (2007) Inappropriate drug use in the elderly: a nationwide register-based study. Ann Pharmacother 41:1243–1248
Haukka J, Suvisaari J, Tuulio-Henriksson A, Lonnqvist J (2007) High concordance between self-reported medication and official prescription database information. Eur J Clin Pharmacol 63:1069–1074
Poluzzi E, Strahinja P, Vargiu A et al (2005) Initial treatment of hypertension and adherence to therapy in general practice in Italy. Eur J Clin Pharmacol 61:603–609
Giron MS, Fastbom J, Winblad B (2005) Clinical trials of potential antidepressants: to what extent are the elderly represented: a review. Int J Geriatr Psychiatry 20:201–217
Van Spall HG, Toren A, Kiss A, Fowler RA (2007) Eligibility criteria of randomized controlled trials published in high-impact general medical journals: a systematic sampling review. JAMA 297:1233–1240
Acknowledgements
We thank the National Board of Health and Welfare for providing us the data. We also wish to thank Associate Professor Ingemar Kåreholt for statistical advice. This study was supported by grants from the Swedish Council for Working Life and Social Research and The Swedish Research Council.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johnell, K., Fastbom, J. The association between use of cardiovascular drugs and antidepressants: a nationwide register-based study. Eur J Clin Pharmacol 64, 1119–1124 (2008). https://doi.org/10.1007/s00228-008-0541-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-008-0541-3