Abstract
Background
In patients on oral anticoagulation with warfarin, genetic variations of the cytochrome P 450–CYP2C9 have recently been associated with very low warfarin requirements. Patients needing low doses had an increased risk for bleeding complications. In Germany, phenprocoumon (having a similar metabolic pathway) is the most commonly employed vitamin K antagonist. Treatment is usually monitored by general practitioners (GPs).
Objectives
To determine whether CYP2C9 variant alleles can serve as risk markers in general-practice patients anticoagulated with phenprocoumon.
Methods
All adult anticoagulated patients in 12 teaching general practices and one university outpatient clinic were to be recruited. Blood samples were taken from 185 patients during routine anticoagulation controls and tested for CYP2C9 mutations. Subjects answered a questionnaire concerning bleeding complications, drug intolerance, and personal and family medical history. Phenprocoumon dosages required for stable anticoagulation were recorded. Odds ratios (OR) with 95% confidence intervals (CI) were calculated based on 2-way cross-tabulations and multivariate logistic regression models, t-tests used where appropriate.
Results
Bleeding was reported by 19% of the patients, 2.2% of whom had suffered life-threatening bleeding. CYP2C9 variants were carried by 26.3% of 179 patients tested (17.9% *1/*2, 7.8% *1/*3, 0.6% *2/*3). While presence of a *2 allele was not associated with an increased risk (OR 0.35, CI 0.10–1.24), carriers of the rare *3 alleles had a higher risk of bleeding (OR 3.10, CI 1.02–9.40). With regard to bleeding, carrying CYP2C9*3 was highly specific (94%), though sensitivity was low at 17%; post-test probability of bleeding was 40%.
Conclusions
CYP2C9*3 variants are associated with an increased bleeding risk in patients anticoagulated with phenprocoumon. Screening can identify patients with a high risk of bleeding. Appropriate clinical consequences (restricted indication for anticoagulation, careful induction, adjustment of target INR, closer monitoring or self-testing of INR) as well as the cost-effectiveness of screening for variant CYP2C9 with regard to patient outcomes should be subject of further research.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Oral anticoagulation is a high-risk therapy: Incidence of bleeding complications has been reported as 10–17 per 100 patient-years (any severity) and 2–5 per 100 patient-years (major bleeding) [1]. In Germany, some 172.5 million defined daily doses (DDD) of phenprocoumon were prescribed in 2000 [2],corresponding to approximately 473,000 anticoagulated patients and some 10,000–80,000 patients with bleeding complications per year.
Phenprocoumon, the drug almost exclusively used for oral anticoagulation in Germany[2, 3], is a vitamin K antagonist similarly structured to warfarin (with a much longer half-life: 6.5 vs 1.5 days) [4], but considered to be less prone to drug interactions.[5] Despite the differences in molecular structure and pharmacokinetics, the metabolism of both warfarin and phenprocoumon depends (to some extent) on the CYP2C9 isoenzyme of the cytochrome P450.[6] The exact pathway of the phenprocoumon metabolism, however, remains to be clarified. Interindividual differences in drug response caused by variable metabolizing enzyme activity due to genetic variants of CYP2C9 have been described. Next to a wild-type allele CYP2C9*1, two variant alleles with decreased enzyme activity have been described: people with a *1/*2 polymorphism have a somewhat reduced enzyme activity, carriers of *1/*3 or *2/*2 genotypes have a significantly reduced metabolism, and *2/*3 and *3/*3 carriers are classified as slow metabolizers [7].
In 1999, Aithal et al. reported that selected anticoagulated patients presenting genetic variants of CYP2C9 often needed very low doses of warfarin, and that low-dose patients had more than a threefold increased risk of major bleeding complications (a direct association of bleeding risk and presence of a variant allele was, however, not demonstrated)[8]. Margaglione et al. [9] and Higashi et al. [10] have shown a two- to threefold increased bleeding risk in warfarin-anticoagulated patients with any variant CYP2C9 allele who were followed up in specialized clinics. In contrast to the UK, where patients are usually followed up in hospital-based anticoagulation clinics, in Germany most patients with oral anticoagulation are managed in general practice (an approach which has shown to be feasible in the UK also) [11, 12].
The aim of our study was to determine whether CYP2C9 polymorphisms are relevant for patients taking phenprocoumon, and to evaluate their feasibility and validity as risk markers in a (unselected) cross-sectional sample of anticoagulated general practice patients [9, 13, 14, 15, 16].
Methods
The study was approved by the Göttingen University ethics committee.
The prevalence of *3 polymorphisms in general populations is reported to be 7–10% [17, 18]. On this basis a sample size of 170–500 would be necessary to demonstrate a sixfold increased bleeding risk with a 5% significance level and a power of 80%.
All 25 teaching general practices in the city of Göttingen, as well as the university outpatient clinic for cardiovascular diseases, were invited to participate. Five of the twelve participating practices (response rate 48%) were run by one GP, 6 had two GPs, and 1 was a group practice with four partners. Respondents were asked to recruit all their patients taking phenprocoumon. Eligible patients were determined using the practice computers. After obtaining written informed consent, an extra 9 ml of venous blood (EDTA-filled vacutainer) was drawn during a routine INR control, sent to the local institute of human genetics, and frozen until genotyping of CYP2C9. Samples were identified by a patient code number to insure blind analysis. Additionally, patients and GPs (or practice staff) were asked to complete a short questionnaire on the indication, duration frequency of INR controls, past bleeding, complications (site and severity), concurrent chronic disorders and treatments, as well as a history of drug intolerance. Patients and GPs were also asked to provide information on dosage schedules and past INR values (copy of the patients' anticoagulation pass or relevant chart documentation). The questionnaires were returned by mail or collected by one of the researchers. Questionnaires and blood samples were matched by means of the patient code number.
Phenprocoumon dose requirements were determined as follows[12]: The six most recent INR values within the therapeutic range (target INR as recommended for each indication [19]) were determined in each patient's documentation.
Blood samples were analyzed using PCR-based procedures as described by Stubbins [20]. DNA fragments were examined for restriction fragment length polymorphisms (RFLPs); incomplete digestion was ruled out by application of controls in every batch and double-checking suspect samples. Genotyping was blind with regard to patient identity and questionnaire responses; results were matched with the questionnaires by means of the patient code number in the department of GP. Descriptive statistics, t-tests, odds ratios (OR), and 95% confidence intervals (CI) based on 2×2 contingency tables were calculated, relating occurrence of bleeding with presence of variant alleles, phenprocoumon requirement, target INR, and comedication. To assess the influence of variant alleles on bleeding compared with other possible factors, multivariate (logistic regression) models were determined using SAS Version 8.1 [21] Accuracy of genotyping as a diagnostic test was calculated according to Sackett. [22].
Results
From August 1999 to February 2000, 185 patients (137 general practice and 48 hospital outpatients) were included into the study. Fifty-eight general practice patients could not be included because they did not contact their practice within the research period, refused consent, or were not recruited by their GP for logistic reasons. Information on these patients could not be gathered due to the particularities of the German healthcare system (no gatekeeping, no practice lists). Five practices had included all their eligible patients, 5 practices between 50 and 100%, two practices had recruited less than half of their patients. A mean of 14 patients (range 2–31) were recruited per practice. Patient characteristics and indications for anticoagulation are summarized in Table 1.
Phenprocoumon dosages could be retrieved for 155 patients (83.8%), documentation of INR and/or dosages was incomplete in the others. A vast majority of patients (88.1%) took other long-term drugs in addition to phenprocoumon (mean number of drugs 3.6, 95% CI 3.3–3.9). Comorbidity was documented in 159 patients (86%, average number of codiagnoses 2.6, 95% CI 2.3–2.9) 92.5% of whom were treated (the most frequent comorbidities and comedications are shown in Table 2).
Genotypes
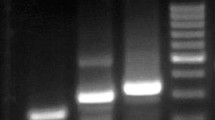
Genotyping of CYP2C9 alleles was performed for 179 (of the 185) patients (blood samples did not arrive at the institute of human genetics in six cases: four hospital outpatients and two general practice patients). Wild-type (*1/*1) alleles were most common (n=132, 73.7%); 26.3% had CYP2C9 polymorphisms: *1/*2 genotype in 32 patients (17.9%), *1/*3 genotype in 14 patients (7.8%), and *2/*3 genotype in 1 (0.6%) patient. Mean treatment duration did not differ significantly between wild-type or variant allele carriers, nor did target INR or age. Significantly less *2 carriers were on comedication compared with wild-type carriers (76 versus 92%, P=0.01), the difference between wild-type and *3 carriers was not significant (80% vs 92%). There was no significant difference in the mean phenprocoumon doses required by patients with wild-type, (15.29 mg/week, 95% CI 14.13–16.45), *1/*2 (16.02 mg/week, 95% CI 13.53–18.51), and *1/*3 (13.29 mg/week, 95% CI 10.45–16.13) genotype (no dosage information was available for the only *2/*3 patient); details on dose distributions are shown in Fig. 1.
However, patients who had bled required significantly lower weekly doses than patients without hemorrhagic complications: 12.58 mg (95% CI 10.92–14.23) vs 15.90 mg (95% CI 14.80–17.00). Comorbidity and comedication were not associated with increased bleeding risk, nor were individual codiagnoses or drug classes (details not shown).
Carriers of a CYP2C9*2 polymorphism did not have an increased bleeding risk (OR 0.35, CI 0.10–1.24). However, a threefold increased bleeding risk (OR 3.10, CI 1.02–9.40) was detected in the 8.4% of our patients carrying *3 polymorphisms (*1/*3 and *2/*3), resulting in a positive predictive value of 40%, i.e., four of ten patients with *3 polymorphisms will suffer bleeding complications; details are shown in Tables 3 and 4.
Risk identification by CYP2C9*3 genotype persisted in a multivariate (logistic regression) analysis with sex, age (less than 60 years or 60 years and older), target INR, presence of drug intolerance, comedication, and presence of a *3 polymorphism as predictive variables model (OR 3.64, 95% CI 1.08–12.26). Reporting drug intolerance was also associated with an increased bleeding risk (OR 3.57, 95% CI 1.34–9.51), as well as age over 60 years (OR 3.37, CI 1.12–10.20). The other predicting variables had no significant influence.
Discussion
Identifying carriers of variant CYP2C9 alleles proved to be feasible in general practice, as genotyping could be performed on a blood sample taken during a routine INR control, and is relatively inexpensive. The prevalence of variant alleles was lower in our cross-sectional sample (27%) than in Aithal's control groups (48% in anticoagulated patients, 40% in community controls) [8], and frequencies reported in European volunteer populations (33–35%) [17, 18].
In a relatively small sample of unselected general practice patients, screening for variant CYP2C9 alleles could identify patients with a high bleeding risk: carriers of rare genotypes *1/*3 and *2/*3 proved to have a 3 times higher risk of bleeding complications than patients with wild-type or the more common *1/*2 variant alleles. This is in line with previous reports of CYP2C9*2 carriers having only a moderately reduced enzyme activity (which is in some contrast to in vitro studies [23]), while CYP2C9*3 carriers have significantly reduced function[7]. Phenprocoumon, like warfarin, is a substrate for CYP2C9 [6], and genetic variance in the metabolism appears to have significant influence on patients' bleeding risk. Consequently, a revision of the recent proposal to use phenprocoumon instead of warfarin in patients presenting variant CYP2C9 alleles should be considered [24]. The third vitamin K antagonist used for anticoagulation, acenocoumarol, does not seem to be a safe alternative either [25]. More studies may be necessary to determine and compare the metabolic pathways and pharmacogenetic implications for all three drugs.
Bleeding risk may be affected by several factors including vitamin K intake, which is difficult to measure reliably as questionnaires on dietary habits are of low validity [26]. Patient compliance as well as the quality of care (e.g., anticoagulation control, dose adjustment) are likely to influence the individual bleeding risk. However, assessing the quality of primary care and its influence on patient outcomes was not the focus of this study. To be useful in general practice patients, risk markers have to be prominent in patients with variable dietary habits, comorbidity, and compliance levels. Despite the sensitivity of "genetic testing" for bleeding being only 17%, our results indicate that, due to the high specificity (94%), CYP2C9 screening for *3 polymorphisms can identify 8.4% of patients—a subgroup with a particularly high risk of 40%.
However, as all anticoagulated patients have (or should have) regular INR controls, the additional value of genetic screening and the impact on the management of high-risk patients remains to be determined. Closer monitoring of drug interactions and INR values could be a consequence, with self-control of INR being a management option [27, 28]. To maximize the benefit, genotyping should probably be performed before the induction of anticoagulation. A slower, low-dose induction under close supervision of INR would then be chosen for patients at risk. Indications for anticoagulation or drugs interacting with anticoagulants (particularly those metabolized via CYP2C9) may be set more restrictively for patients with variant alleles, and target INR values may have to be adjusted according to individual risks for bleeding and thrombotic events. Risk adjustment for genotype could also be included in computer systems for dosage advice [29], though these devices are only occasionally used in Germany. Effectiveness of these measures with regard to bleeding and thromboembolic risk would have to be subject of further studies. Larger population-based trials are necessary to determine the number of bleeding episodes that could be prevented by genetic screening of patients requiring anticoagulation.
Some methodological problems may influence the validity of our study (some of them typical for studies in a general practice setting). For confidentiality and feasibility, patient recruitment was not centrally organized, but was done by individual GPs. Though GPs were instructed to include all their patients on phenprocoumon into our trial, the inclusion rate was variable and incomplete in many practices, as can be commonly observed in studies where patients are recruited by their GP, particularly in countries without a list system [30, 31]. For most patients, detailed information on the induction period of phenprocoumon could not be provided, nor could difficulties in dose adjustment be reliably recalled. In Germany, induction of anticoagulation often takes place when patients are still in hospital and is then not documented in the patient's pass or the GPs' charts.
As frequently seen in general practice-based surveys, documentation quality was variable between and within practices. However, recall or documentation bias is unlikely to affect the study outcome, as genotyping was performed blind with regard to patients' identity or questionnaire responses. As there was not contact between the researchers and patients, we had to rely on patients' answers on the questionnaires, which had been kept short and concise in order to ensure a high acceptance. For example, instead of asking patients how often and when they had experienced bleeding in several years (which seemed likely to elicit recall bias rather than reliable data), patients were asked whether there had been bleeding episodes at all. This approach did not allow for expression as bleeding episodes per patient year (and thus for controlling bleeding risk for duration of therapy). However, in our population, bleeding risk was of similar magnitude to that reported in other surveys [32],and there was no significant difference in duration of treatment between patients with or without bleeding complications.
In our cross-sectional study, patients having suffered adverse events of phenprocoumon may be underrepresented due to death or switch to other forms of treatment. If these (early) adverse events were related to rare CYP2C9 variants, it seems possible that the overall importance of the CYP2C9 genotype for phenprocoumon-induced bleeding was underestimated (and carriers of rare variant alleles underrepresented). The mean length of treatment being 5 years, patients in our study can be expected to be stabilized on phenprocoumon, but still the CYP2C9 genotype stands out as a risk factor for bleeding.
The high rate of comorbidity, typical for (mostly) elderly patients in general practice, explains the high comedication of anticoagulated patients [33, 34] and highlights the need for monitoring with regard to drug interactions and susceptibility to complications. Previous studies did not report details on comedication [35], they excluded patients "with drug interactions as apparent cause for low-dose requirements"[8] or adjusted for any [9] or CYP2C9-dependent [10] comedication. Judicious use of genetic testing may be justified in patients starting oral anticoagulation or presenting additional risk factors, including consumption of drugs that may increase hypocoagulation or have a CYP2C9-dependent metabolism. Intolerance of losartan as well as diclofenac (and other NSAIDs) reported by a few patients merits further studies, because metabolism of losartan and diclofenac depends on CYP2C9. [36, 37] We cannot exclude, however, that the association of bleeding risk and reported drug intolerance was confounded by patients reporting GPs' recommendations to avoid certain drugs (such as aspirin) as "drug intolerance."
References
Kuijer PM, Hutten BA, Prins MH, Buller HR (1999) Prediction of the risk of bleeding during anticoagulant treatment for venous thromboembolism. Arch Intern Med 159:457–460
Schwabe U (2000) Anticoagulants. In: Schwabe U, Paffrath D (eds) Drug prescribing report 2000 [in German]. Springer, Berlin, Heidelberg, pp 186–194
Hirsh J, Ginsberg JS, Marder VJ (1994) Anticoagulant therapy with coumarin agents. In: Colman RW, Hirsh J, Marder VJ, Salzman EW (eds) Hemostasis and thrombosis: basic principles and clinical practice, 3rd edn. Lippincott, Philadelphia, pp 1567–1583
Kristiansen C, Lassen JF, Dahler-Eriksen BS, Dahler-Eriksen K, Larsen TB, Brandslund I (2000) Evaluation of a simple dosage scheme for transition from phenprocoumon to warfarin in oral anticoagulation. Thromb Res 98:157–163
Harder S, Thurmann P (1996) Clinically important drug interactions with anticoagulants. An update. Clin Pharmacokinet 30:416–444
He M, Korzekwa KR, Jones JP, Rettie AE, Trager WF (1999) Structural forms of phenprocoumon and warfarin that are metabolized at the active site of CYP2C9. Arch Biochem Biophys 372:16–28
Brockmöller J, Kirchheiner J, Meisel C, Roots I (2000) Pharmacogenetic diagnostics of cytochrome P450 polymorphisms in clinical drug development and in drug treatment. Pharmacogenomics 1:125–151
Aithal GP, Day CP, Kesteven PJ, Daly AK (1999) Association of polymorphisms in the cytochrome P450 CYP2C9 with warfarin dose requirement and risk of bleeding complications. Lancet 353:717–719
Margaglione M, Colaizzo D, D'Andrea G et al. (2000) Genetic modulation of oral anticoagulation with warfarin. Thromb Haemost 84:775–778
Higashi MK, Veenstra DL, Kondo LM et al. (2002) Association between CYP2C9 genetic variants and anticoagulation-related outcomes during warfarin therapy. JAMA 287:1690–1698
Fitzmaurice DA, Hobbs FD, Murray ET (1998) Primary care anticoagulant clinic management using computerized decision support and near patient International Normalized Ratio (INR) testing: routine data from a practice nurse-led clinic. Fam Pract 15:144–146
Hobbs FD, Fitzmaurice DA (1997) Where should oral anticoagulation monitoring take place? Br J Gen Pract 47:479–480
Baglin T (2001) Avoiding overanticoagulation: pharmacogenomics or pragmatism? Thromb Haemost 85:945–946
Holtzman NA, Marteau TM (2001) Will genetics revolutionize medicine? N Engl J Med 343:141–144
Emery J, Hayflick S (2001) The challenge of integrating genetic medicine into primary care. BMJ 322:1027–1030
Wolf CR, Smith G, Smith RL (2000) Science, medicine, and the future: pharmacogenetics. BMJ 320:987–990
Yasar U, Eliasson E, Dahl ML, Johansson I, Ingelman-Sundberg M, Sjoqvist F (1999) Validation of methods for CYP2C9 genotyping: frequencies of mutant alleles in a Swedish population. Biochem Biophys Res Commun 254:628–631
Scordo MG, Aklillu E, Yasar U, Dahl ML, Spina E, Ingelman-Sundberg M (2001) Genetic polymorphism of cytochrome P450 2C9 in a Caucasian and a black African population. Br J Clin Pharmacol 52:447–450
Scottish Intercollegiate Guidelines Network (1999) Antithrombotic therapy. A national clinical guideline. Edinburgh (Scotland). SIGN publication no. 36. http://www.guideline.gov/VIEWS/full_text.asp?guideline=002133 (accessed on 30 December 2002)
Stubbins MJ, Harries LW, Smith G, Tarbit MH, Wolf CR (1996) Genetic analysis of the human cytochrome P450 CYP2C9 locus. Pharmacogenetics 6:429–439
SAS Institute (1999) SAS/STAT. User's guide, version 8, vol 3. SAS Institute, Cary, NC
Sackett DL, Richardson WS, Rosenberg W, Haynes RB (1997) Evidence-based medicine. Churchill Livingstone, New York
Crespi CL, Miller VP (1997) The R144C change in the CYP2C9*2 allele alters interaction of the cytochrome P450 with NADPH:cytochrome P450 oxidoreductase. Pharmacogenetics 7:203–210
Mannucci PM (1999) Genetic control of anticoagulation. Lancet 353:688–689
Verstuyft C, Morin S, Robert A et al. (2001) Early acenocoumarol overanticoagulation among cytochrome P450 2C9 poor metabolizers. Pharmacogenetics 11:735–737
Halkin H, Lubetsky A (1999) Warfarin dose requirement and CYP2C9 polymorphisms. Lancet 353:1972–1973
Kortke H, Korfer R (2001) International normalized ratio self-management after mechanical heart valve replacement: is an early start advantageous? Ann Thorac Surg 72:44–48
Cromheecke ME, Levi M, Colly LP et al. (2000) Oral anticoagulation self-management and management by a specialist anticoagulation clinic: a randomized cross-over comparison. Lancet 356:97–102
Walton RT, Harvey E, Dovey S, Freemantle N (2001) Computerised advice on drug dosage to improve prescribing practice. Cochrane Database Syst Rev 1
Bell-Syer SE, Moffett JA (2000) Recruiting patients to randomized trials in primary care: principles and case study. Fam Pract 17:187–191
Wilson S, Delaney BC, Roalfe A et al.(2000) Randomised controlled trials in primary care: case study. BMJ 321:24–27
Beyth RJ (2001) Hemorrhagic complications of oral anticoagulant therapy. Clin Geriatr Med 17:49–56
Akker M van den, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA (1998) Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol 51:367–375
Veehof L, Stewart R, Haaijer-Ruskamp F, Jong BM (2000) The development of polypharmacy. A longitudinal study. Fam Pract 17:261–267
Taube J, Halsall D, Baglin T (2000) Influence of cytochrome P-450 CYP2C9 polymorphisms on warfarin sensitivity and risk of over-anticoagulation in patients on long-term treatment. Blood 96:1816–1819
Morin S, Loriot MA, Poirier JM et al. (2000) Is diclofenac a valuable CYP2C9 probe in humans? Eur J Clin Pharmacol 56:793–797
Yasar U, Forslund-Bergengren C, Tybring G et al. (2002) Pharmacokinetics of losartan and its metabolite E-3174 in relation to the CYP2C9 genotype. Clin Pharmacol Ther 71:89–98
Acknowledgements
We thank all participating patients and GPs for their cooperation, and Sabine Buth, Susanne Herlt, and Ulrike Lenz for performing the DNA extraction. We are indebted to Prof. Jürgen Brockmöller, Göttingen, and Dr. Robert Walton, Oxford, for critically reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hummers-Pradier, E., Hess, S., Adham, I.M. et al. Determination of bleeding risk using genetic markers in patients taking phenprocoumon. Eur J Clin Pharmacol 59, 213–219 (2003). https://doi.org/10.1007/s00228-003-0580-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-003-0580-8