Abstract
The aim of this study was to assess the spatial stability of stroke patients while holding a freely movable object. Twenty-two acute stroke patients with mild hand impairment performed a grip and lift task using the thumb and index finger. The displacement of the center of pressure (COP) trajectory, the grip force (GF) and several clinical parameters were monitored. Although the GF was not different between paretic and nonparetic hands, the COP trajectory of the paretic index finger was increased. Moreover, the COP trajectories of the thumb and index finger in hemorrhagic patients were longer than those in ischemic patients. These discrepancies between kinetic parameters suggest that different aspects of grip force control may be considered in patients with mild stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Grip force (GF) control while holding an object is the fundamental basis of hand function. Healthy subjects produce a minimal GF to optimize sensory information from the finger pads to conserve energy. On the other hand, stroke patients use a higher GF in the paretic hand. Exaggerated GF is considered to be a strategic response to sensory deficits (Nowak and Hermsdörfer 2005), and decreased force output control and selective activation of hemiparetic muscles caused by damage to the corticospinal system (Lang and Schieber 2009). Moreover, an exaggerated GF also implies altered cortical control of grasping. A previous study reported that nonparetic hands had a higher GF after stroke (Quaney et al. 2005), and deficits in sensorimotor processing or slowed motor learning are suggested as possible causes.
In addition to the GF amplitude referred to above, altered temporal regulation has been studied after stroke. For example, stroke patients demonstrated a delay between the onset of GF and onset of the upward lift force in paretic hands (McDonnell et al. 2006). After an object was lifted, there were irregular fluctuating forces and reduced safety margin adaptation (Blennerhassett et al. 2006). When patients were asked to track the GF according to visual instruction, they were unable to smoothly increase and decrease the GF (Grichting et al. 2000).
In contrast to the numerous studies on the GF amplitude and its temporal regulation, studies on the force direction (Marquardt and Li 2013) in stroke patients are limited. Apart from a study on force direction during power grip (Enders and Seo 2015), stroke patients were found to demonstrate a more deviated fingertip force direction in the paretic hand than in the nonparetic hand (Seo et al. 2010). The deviated force direction can cause spatial instability such as unwanted object rotation or finger slipping.
The purpose of this study was to examine the fingertip force direction in more natural reach-to-grasp movement. The spatial stability while holding a freely movable object by stroke patients was assessed. We monitored the total length of the center of pressure (COP) trajectory of the area between the finger pad and contact surface based on biomechanical relationships suggesting that the COP displacement can be caused by deviated force direction during the lifting and holding of an object (Parikh and Cole 2012). One technical challenge in monitoring COP trajectory within a fingertip is spatial resolution. To resolve this challenge, we used a pressure sensor sheet with a high spatial resolution of 248 sensels per square cm. We considered the high spatial resolution sheet sensor to be useful to monitor the trajectory within a fingertip. Additionally, the relationships between the kinetic parameters in the paretic hand and clinical tests were assessed.
Methods
Subjects
Twenty-two patients diagnosed with stroke (15 males and 7 females, 67.1 ± 13.0 years, 14 ischemic and 8 hemorrhagic) admitted to a district general hospital were recruited (Table 1). Nine patients had lesions in the right hemisphere and 13 had lesions in the left hemisphere. The inclusion criteria were (1) the occurrence of first ischemic or hemorrhagic hemispheric stroke; (2) mild/moderate upper extremity impairment (Fugl-Meyer Assessment Scale for Upper Extremity, UE-FMA ≥ 32/66) (Hoonhorst et al. 2015); (3) ability to perform the holding task with the thumb and index finger, and (4) ability to follow commands. The exclusion criteria were (1) cerebellar lesion, (2) poor physical condition, or (3) clinical signs of motor apraxia/spatial neglect. The average time after the onset of stroke was 5.9 ± 3.5 days. All patients were admitted in the acute phase and underwent rehabilitation. To evaluate the sensorimotor control in the nonparetic hand after stroke, data on 21 healthy controls (3 males and 18 females, 78.5 ± 5.6 years) were also collected.
Handedness prior to stroke was evaluated with the Edinburgh Handedness Inventory (EHI, mean laterality quotient: 91.5). Informed consent was obtained prior to the study. This study was approved by the University Ethical Review Board for Medical Research Involving Human Subjects.
Grip and lift task
The experimental procedure was similar with that in a previous study (Westling and Johansson 1984). The patients sat on a chair/wheelchair facing a height-adjustable table, and patients’ finger pads were wiped with an alcohol swab to reduce inter-individual variability in finger skin friction. An iron cube (250 g, 31 × 31 × 31 mm) was placed on the table 30 cm from the patient in the midsagittal plane. A verbal instruction was given to grip the cube using the thumb and index finger, lift approximately 10 cm, and hold for 5–7 s. The patients were also instructed to use minimal force to perform the task. Before each lift, patients were allowed to touch the cube slightly without exceeding 0.5 N. Ten lifts were performed for each hand, and the interval between lifts was approximately 5 s. A maximum of five lifts was performed as practice, but practice trial was stopped early when patients reported full understanding of the task. Half of the patients performed the first session with the paretic hand and the other half with the nonparetic hand.
Materials
Two pressure sensor sheets (Pressure Mapping Sensor 5027, Tekscan, South Boston, MA, USA) were attached to the grip surfaces of the cube. The sensor had a sensing area of 27.9 by 27.9 mm with 1936 sensing elements (sensels) distributed over 44 rows and 44 columns, a thickness of 0.1 mm, a spatial resolution of 248 sensels per square cm and a sensitivity range of 0–345 KPa for each sensel. Before each recording, the sensor sheet was equilibrated and calibrated using the test instrument. The pressure distributions were recorded with a frequency of 100 Hz in 8-bit resolution using I-Scan 100 System (Nitta, Japan).
Three kinetic parameters were used to quantify the sensorimotor control of grasping; the COP trajectory (mm/4 s), mean GF and maximal GF (N). For each lift, the onset was calculated as the time when the force of 0.5 N was initially loaded on a sensel. The COP is the center of all the forces in the X- and Y-axes at each recording point, representing how the forces are balanced on the sensor sheet. The COP trajectory was calculated from the total length of the COP displacement during the first 4 s. The mean GF was then calculated from the sum of the pressure in all 1936 sensing elements during the first 4 s. The maximal GF was defined as the peak GF during the first 4 s.
Clinical tests
Several clinical tests were used to characterize the patients. The cutaneous pressure threshold of the thumb and index finger pads was assessed with Semmes-Weinstein Monofilaments, which apply target forces of 0.07, 0.4, 2.0, 4.0 or 300 g. The lowest perceived monofilament was considered normal and higher monofilaments indicate severe sensory disturbance. Trail-making A- and B-tests (TMT A/B) were used to assess the relationship between kinetic parameters and cognitive function, respectively, to evaluate basic and higher-order executive abilities (Tamez et al. 2011). In addition, the upper extremity function was evaluated using a peg test. The peg test protocol was similar to nine-hole peg test which involves grasping a peg out of multiple pegs in a container, placing the peg in a hole, and repeating it for 9 pegs, and unload them one by one back to the container (Mathiowetz et al. 1985). In the present study, on the other hand, 12 pegs (15 × 50 mm, diameter/height) were already placed in the pegboard, the patients reached and pinched a peg, and moved it up and down in any order. The time to complete the test (s) was measured.
Statistical analysis
The intra-subject repeatability was assessed using intra-rater reliability (ICC) for each hand. Assumptions of distributional normality were tested using the Shapiro–Wilk test, and as a result, normality was not satisfied in the EIH, the cutaneous pressure threshold, the peg test and UE-FMA.
Differences between control and stroke groups, and ischemic and hemorrhage patients were examined using the unpaired t test, Chi-square test (sex and location of stroke) and Mann–Whitney test (EHI, the cutaneous pressure threshold, the peg test and UE-FMA). In order to compare the baseline characteristics between stroke and control groups, a three-way analysis of variance (ANOVA) was performed for the COP trajectory, the mean GF and the maximal GF. The factors were ‘hand’ with two levels (nonparetic hand in the stroke group and dominant hand in the control group), and ‘sex’ with two levels (male and female). Because age could affect GFs, age was therefore included as a covariate. If there was no main effect of ‘hand’, patients were assumed to be able to control their nonparetic hand normally.
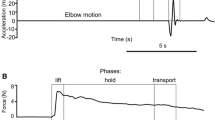
Secondly, a two-way ANOVA was used to investigate differences within the stroke group. The factors were ‘paresis’ with two levels (paretic and nonparetic hand) and ‘type’ with two levels (ischemic and hemorrhagic). To analyze the change in applied forces in detail, we divided the 4 s into the first two and last two seconds, indicating the lifting and holding phases, respectively (Johansson and Flanagan 2009).
Associations between kinetic parameters in the paretic hand and other tests were examined. Total values were calculated by summing the two fingers (three kinetic parameters and the cutaneous threshold). The statistical software SPSS ver. 23.0J for Windows (SPSS Japan., Tokyo, Japan) was used for the analysis. Effect sizes were reported as r for the unpaired t test, Chi-square test and Mann–Whitney test, and η2 for the ANOVA analysis. Values of p < 0.05 were considered significant.
Results
Figure 1 shows the COP trajectories (A) and the GF traces (B) for a representative patient. In Fig. 1a, the blue color indicates the area of finger pad contact, and the gray line indicates the COP trajectory during a single grip and lift task. The COP trajectories of the paretic hand were relatively long. Moreover, the GFs in the paretic hand decreased with the holding time, and the GF traces were therefore unstable.
The COP trajectory in paretic and nonparetic hands demonstrated substantial intra-rater reliability (ICC (1, 1) = 0.62 and 0.78, respectively). The mean GF and the maximal GF were also reliable (mean ICC (1, 1) = 0.89, range 0.85–0.90).
Table 1 shows the results of comparisons between control and stroke groups, and ischemic and hemorrhage patients. In addition, age ranges were 45–86 years (stroke group), and 68–89 (control group). The EHI ranges were − 47 to 100 (stroke group), and 80–100 (control group). The score range of UE-FMA were 45–66 (ischemic), and 53–66 (hemorrhage). The average age and female ratio were significantly higher in the control group. Moreover, the cutaneous pressure threshold for the paretic hand was higher in hemorrhage patients.
Table 2 shows the results of comparisons between the stroke and control groups. The three-way ANOVA did not reveal any significant main effect or interaction. Although the effect of age was observed in GFs (P = 0.07–0.08), the effect did not reach statistical significance.
Table 3 shows the results of comparisons among stroke patients. The two-way ANOVA revealed a significant main effect of paresis in the index finger COP trajectory (first 2 s: F1, 40 = 4.23, P = 0.04; last 2 s F1, 40 = 7.09, P = 0.01), and a main effect of stroke type in thumb (first 2 s: F1, 40 = 7.57, P < 0.01; last 2 s F1, 40 = 8.94, P < 0.01) and index finger COP trajectories (first 2 s: F1,40 = 5.84, P = 0.02; last 2 s F1, 40 = 5.31, P = 0.02). However, the analysis did not reveal a significant interaction between paresis and stroke type. The results consistently presented a functional disadvantage in the paretic hand (vs. nonparetic hand) and hemorrhagic stroke (vs. ischemic type).
The COP trajectory in the paretic hand was negatively correlated with the mean/maximal GFs, and the COP trajectory in the paretic thumb positively correlated with the cutaneous pressure threshold. Moreover, four of six kinetic parameters were correlated with the TMT-B (Table 4).
Discussion
We found that the spatial stability while holding a freely movable object is altered after stroke. Although the mean/maximal GFs were not significantly different from the nonparetic hand, the COP trajectory was increased after stroke. Moreover, the kinetic parameters were correlated with the TMT-B, implying a relationship between the kinetic alteration and cognitive flexibility.
The COP trajectory within the fingertip in stroke patients was found to be reliable. Traditionally, the COP displacement on a force plate under the feet has been used for evaluating postural stability (Palmieri et al. 2002). However, there were technical difficulties in adapting this technique for quantifying hand function because of the limits of spatial resolution. To resolve this problem, we used a high spatial resolution pressure sensor, which was useful to monitor the COP trajectory within the fingertip. We expect the COP trajectory to serve as an objective index for evaluating the spatial stability of grasping.
Although the mean/maximal GFs were not significantly different, the COP trajectory was increased in the paretic hand. This discrepancy is consistent with a previous study that analyzed multiple grip-lift parameters in patients with stroke (McDonnell et al. 2006). They found no significant differences in maximal or average GFs. In contrast, the temporal regulation (time between the onset of GF and onset of load force) was disrupted in the affected hand. Their results were from patients with mild stroke (mean UE-FMA: 48.2/66), although their patients showed a more severe level of motor impairment than our patient population (61.0 ± 5.2). These discrepancies between temporal/spatial regulation and GF amplitudes suggest that different aspects of grip force control may be considered in patients with mild stroke.
The age effect on the kinetic parameters was not found between the control and stroke groups. It is known that the GF increases with age (Cole. 1991). For example, Kinoshita and Francis (1996), who compared force parameters of two groups of elderly adults (69–79 years and 80–93 years) and a group of young adults (18–32 years), found that force parameters for the 80–93 year group increased, on average, 10% compared with the group aged 69–79 years. However, the age effect did not reach statistical significance in the present study, despite the control grip is more than 11 years older than the patient group. One potential reason may be that the age effect was reduced because of increased GF in the nonparetic hand of acute stroke patients. This observation is consistent with the previous study that reported a higher GF in the nonparetic hands of chronic stroke patients (Quaney et al. 2005).
The key finding in the present study is that the COP trajectory only increased in the index finger. The reason is unclear at this time, but one underlying cause may be spastic movement in the index finger after stroke. A study comparing stretch reflexes in thumb and finger flexors after stroke found that the responses of the paretic finger flexors were elevated than those in thumb flexors (Towles et al. 2010). The study suggested that spinal motoneurons of the finger flexors may have a lower activation threshold or were associated with a higher reflex loop gain. Previous studies also reported that hyperexcitability of the flexor muscles occurred in the paretic index finger (Kamper and Rymer 2001; Cruz et al. 2005), and this abnormal muscle tone may alter the grip force direction (Seo et al. 2010). This may account for subsequent slipping, rolling or twisting between the fingertip and the object. As a result, simultaneous displacement of the COP occurred.
The present study provides new knowledge on the kinetic difference between ischemic and hemorrhagic stroke. The COP trajectories of the thumb and index finger were longer after hemorrhagic stroke (Table 3). Our observation is consistent with previous studies that reported severe impairment on average after hemorrhagic stroke, such as high Glasgow Coma Scale score in the acute stage and lower Functional Independence Measure score, on admission to a rehabilitation facility (Kelly et al. 2003; Wei et al. 2010).
Considering the positive correlation between the COP trajectory and cutaneous pressure threshold in the paretic hand (Table 4) and severe sensory impairment in hemorrhagic stroke (Table 1), the lack of sensory information may be related to the COP trajectory. It is known that the loss of sensation under local cutaneous anesthesia results in increased GF (Augurelle et al. 2003). In addition, the lack of sensory information in stroke patients is correlated with pinch grip deficit (Blennerhassett et al. 2007). Thus, it is reasonable to assume that the lack of sensory information may be related to incomplete grip force coordination after stroke.
The kinetic parameters were correlated with the TMT-B time, suggesting that grip control is not only related to somatosensory function, but also to cognitive function. The common feature of precision grasp and the TMT is eye and arm coordination. In a precision grasp task, the patients need to fix the target, reach their arm and maintain a hold on the cube. During this object manipulation process, hand–eye coordination is essential (Johansson et al. 2001). Indeed, as long as there is visual information, force control can be still maintained even if digit sensibility is impaired (Jenmalm and Johanssen 1997). The TMT task also requires a similar process that depends on a visual–spatial search and hand–eye coordination (Ble et al. 2005). Of note, there was no correlation between the kinetic parameters and the TMT-A. A similar result was seen in a walking task. Alexander et al. (2005) developed a walking trail making test in which participants step on instrumented targets with increasing sequential numbers (i.e., 1-2-3; Walking TMT-A), and increasing sequential numbers and letters (ie. 1-A-2B; Walking TMT-B). They found that the Walking TMT-A/B was highly correlated with the paper TMT-B but not the paper TMT-A in the older group. Another study found a similar association between the paper TMT-B (vs. TMT-A) and lower extremity function (Binder et al. 1999). Cognitive flexibility may partially account for the spatial stability during precision grasping in stroke patients.
One limitation of this study is that the biomechanics of the COP trajectory are unknown. A slip, roll or twist between the finger pads and contact area is considered to result in COP displacement (Yamada et al. 2011). Future studies analyzing three-dimensional grasping movement may clarify the biomechanical factors affecting the COP displacement. Furthermore, no relationship between the kinetic parameters and the upper extremity function (the peg test) was found in this study, possibly because of our experimental condition. During the peg test, the patients were allowed to use a compensatory strategy (Michaelsen et al. 2004). Increased trunk and shoulder movements upon hand orientation for grasping may compensate for the kinetic alterations.
In conclusion, although the mean/maximal GFs were not different between hands, the COP trajectory in the paretic index finger was increased in patients with mild stroke. The kinetic parameters in the paretic hand were associated with sensory impairment and cognitive flexibility. This new knowledge may improve our understanding of spatial instability in precision grasping and sensory/cognitive impairments after stroke.
References
Alexander NB, Ashton-Miller JA, Giordani B, Guire K, Schultz AB (2005) Age differences in timed accurate stepping with increasing cognitive and visual demand: a walking trail making test. J Gerontol A Biol Sci Med Sci 60:1558–1562
Augurelle AS, Smith AM, Lejeune T, Thonnard JL (2003) Importance of cutaneous feedback in maintaining a secure grip during manipulation of hand-held objects. J Neurophysiol 89:665–671
Binder EF, Storandt M, Birge SJ (1999) The relation between psychometric test performance and physical performance in older adults. J Gerontol A Biol Sci Med Sci 54:M428–M432
Ble A, Volpato S, Zuliani G, Guralnik JM, Bandinelli S, Lauretani F, Bartali B, Maraldi C, Fellin R, Ferrucci L (2005) Executive function correlates with walking speed in older persons: the InCHIANTI study. J Am Geriatr Soc 53:410–415
Blennerhassett JM, Carey LM, Matyas TA (2006) Grip force regulation during pinch grip lifts under somatosensory guidance: comparison between people with stroke and healthy controls. Arch Phys Med Rehabil 87:418–429
Blennerhassett JM, Matyas TA, Carey LM (2007) Impaired discrimination of surface friction contributes to pinch grip deficit after stroke. Neurorehabil Neural Repair 21:263–272
Cole KJ (1991) Grasp force control in older adults. J Mot Behav 23:251–258
Cruz EG, Waldinger HC, Kamper DG (2005) Kinetic and kinematic workspaces of the index finger following stroke. Brain 128:1112–1121
Enders LR, Seo NJ (2015) Altered phalanx force direction during power grip following stroke. Exp Brain Res 233:1677–1688
Grichting B, Hediger V, Kaluzny P, Wiesendanger M (2000) Impaired proactive and reactive grip force control in chronic hemiparetic patients. Clin Neurophysiol 111:1661–1671
Hoonhorst MH, Nijland RH, Van den Berg JS, Emmelot CH, Kollen BJ, Kwakkel G (2015) How do fugl-meyer arm motor scores relate to dexterity according to the action research arm test at 6 months poststroke? Arch Phys Med Rehabil 96:1845–1849
Jenmalm P, Johansson RS (1997) Visual and somatosensory information about object shape control manipulative fingertip forces. J Neurosci 17:4486–4499
Johansson RS, Flanagan JR (2009) Coding and use of tactile signals from the fingertips in object manipulation tasks. Nat Rev Neurosci 10:345–359
Johansson RS, Westling G, Bäckström A, Flanagan JR (2001) hand eye coordination in object manipulation. J Neurosci 21:6917–6932
Kamper DG, Rymer WZ (2001) Impairment of voluntary control of finger motion following stroke: role of inappropriate muscle coactivation. Muscle Nerve 24:673–681
Kelly PJ, Furie KL, Shafqat S, Rallis N, Chang Y, Stein J (2003) Functional recovery following rehabilitation after hemorrhagic and ischemic stroke. Arch Phys Med Rehabil 84:968–972
Kinoshita and Francis (1996) A comparison of prehension force control in young and elderly individuals. Eur J Appl Physiol Occup Physiol 74:450–460
Lang CE, Schieber MH (2009) Stroke. In: Nowak DA, Hermsdörfer J (eds) Sensorimotor control of grasping, 1st edn. Cambridge University, Cambridge, pp 296–310
Marquardt TL, Li ZM (2013) Quantifying digit force vector coordination during precision pinch. J Mech Med Biol 13:1350047
Mathiowetz V, Weber K, Kashman N, Volland G (1985) Adult norms for the Nine Hole Peg Test of finger dexterity. Occup Ther J Res 5:24–38
McDonnell MN, Hillier SL, Ridding MC, Miles TS (2006) Impairments in precision grip correlate with functional measures in adult hemiplegia. Clin Neurophysiol 117:1474–1480
Michaelsen SM, Jacobs S, Roby-Brami A, Levin MF (2004) Compensation for distal impairments of grasping in adults with hemiparesis. Exp Brain Res 157:162–173
Nowak DA, Hermsdörfer J (2005) Grip force behavior during object manipulation in neurological disorders: toward an objective evaluation of manual performance deficits. Mov Disord 20:11–25
Palmieri RM, Ingersoll CD, Stone MB, Krause BA (2002) Center-of-pressure parameters used in the assessment of postural control. J Sport Rehabil 11:51–66
Parikh PJ, Cole KJ (2012) Handling objects in old age: forces and moments acting on the object. J Appl Physiol 112:1095–1104
Quaney BM, Perera S, Maletsky R, Luchies CW, Nudo RJ (2005) Impaired grip force modulation in he ipsilesional hand after unilateral middle cerebral artery stroke. Neurorehabil Neural Repair 19:338–349
Seo NJ, Rymer WZ, Kamper DG (2010) Altered digit force direction during pinch grip following stroke. Exp Brain Res 202:891–901
Tamez E, Myerson J, Morris L, White DA, Baum C, Connor LT (2011) Assessing executive abilities following acute stroke with the trail making test and digit span. Behav Neurol 24:177–185
Towles JD, Kamper DG, Rymer WZ (2010) Lack of hypertonia in thumb muscles after stroke. J Neurophysiol 104:2139–2146
Wei JW, Heeley EL, Wang JG, Huang Y, Wong LK, Li Z, Heritier S, Arima H, Anderson CS (2010) ChinaQUEST Investigators. Comparison of recovery patterns and prognostic indicators for ischemic and hemorrhagic stroke in China: the ChinaQUEST (QUality Evaluation of Stroke Care and Treatment) Registry study. Stroke 41:1877–1883
Westling G, Johansson RS (1984) Factors influencing the force control during precision grip. Exp Brain Res 53:277–284
Yamada T, Taki T, Yamada M, Funahashi Y, Yamamoto H (2011) Static stability analysis of spatial grasps including contact surface geometry. Adv Robot 25:447–472
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kurihara, J., Lee, B., Hara, D. et al. Increased center of pressure trajectory of the finger during precision grip task in stroke patients. Exp Brain Res 237, 327–333 (2019). https://doi.org/10.1007/s00221-018-5425-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-018-5425-x