Abstract
Tinnitus is an auditory phantom percept with a tone, hissing or buzzing sound in the absence of any objective physical sound source. Tinnitus is considered to be an auditory phantom phenomenon analogous to somatosensory phantom pain. Controllable versus uncontrollable pain is characterized by an increased activity in the ventrolateral prefrontal cortex (VLPFC), and activation in the VLPFC correlating with perceived control over pain results in a decrease in subjective pain intensity. Depressed individuals show less activation than healthy controls in the left VLPFC in response to sad autobiographical scripts, and greater relative left prefrontal activation is related to a greater disposition to approach-related, positive affect with a greater ability to regulate negative affect. Based on the theory that non-pulsatile tinnitus can be considered the auditory analogue for deafferentation pain, we hypothesize that the left VLPFC might also be involved in control of tinnitus. We conducted a transcranial magnetic stimulation (TMS) study verifying whether modulating the left VLPFC by TMS can modulate the loudness of tinnitus. We studied 60 patients with chronic tinnitus of which 21 patients received in random order sham and 1-Hz stimulation, while 39 patients received in random order sham and 10-Hz stimulation. Our results show that 10-Hz stimulation can modulate tinnitus loudness, while 1-Hz stimulation does not seem to exert the same effect. Our findings give further support to the fact that non-auditory areas are involved in tinnitus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tinnitus is an auditory phantom percept with a tone, hissing or buzzing sound in the absence of any objective physical sound source. The American Tinnitus Association estimates 50 million Americans perceive tinnitus, and that 12 million of these people have chronic tinnitus that prompts them to seek medical attention. Up to 2 million have such a severe tinnitus that it becomes disabling, interfering with sleep and concentration, social interaction and work and results in major depressions.
Tinnitus is considered to be an auditory phantom phenomenon (Jastreboff 1990) similar to deafferentation pain seen in the somatosensory system (Tonndorf 1987; Moller 2000; De Ridder et al. 2007a, 2011). It is related to both map plasticity (Muhlnickel et al. 1998) and synchronized gamma band activity (Llinas et al. 1999; Weisz et al. 2007; van der Loo et al. 2009; Vanneste et al. 2010b) of the auditory central nervous system. Indeed, electrophysiological studies indicate an excessive spontaneous activity in the central auditory nervous system and changes in the tonotopic map of the auditory cortex as the neurobiological basis of tinnitus.
Consistent with the hypothesis that tinnitus is related to overactivation of the auditory cortex, transcranial magnetic stimulation (TMS) can transiently reduce this cortical hyperactivity by directly stimulating temporal cortex (De Ridder et al. 2005), effects that can persist for a longer time when performing the stimulation repetitively (Kleinjung et al. 2005; Langguth et al. 2008; Khedr et al. 2009). New insights into the neurobiology of tinnitus suggest that neuronal changes are not limited to the classical auditory pathways (Lockwood et al. 1999; Landgrebe et al. 2009; Lanting et al. 2009; Rauschecker et al. 2010). Current studies using transcranial direct current stimulation and TMS have furthermore shown that modulating respectively the right and left dorsolateral prefrontal cortex can interfere with both the tinnitus intensity and distress (Kleinjung et al. 2008; Vanneste et al. 2010a). Depressed individuals show less activation than healthy controls in the left ventrolateral prefrontal cortex (VLPFC) in response to sad autobiographical scripts (Keedwell et al. 2005), and greater relative left prefrontal activation is related to a greater disposition to approach-related, positive affect (Tomarken et al. 1992) with a greater ability to regulate negative affect (Davidson 1995). It has recently been shown that the prefrontal cortex is a key player in emotion regulation. (Ochsner and Gross 2005). The ventrolateral, dorsolateral and dorsomedial prefrontal cortices are important in cognitive strategies that reduce negative emotional experience (Ochsner and Gross 2005). Successful reappraisal of negative experiences is associated with increased activity within the left VLPFC (Wager et al. 2008). Also, controllable versus uncontrollable pain is characterized by an increased activity in the VLPFC (Wiech et al. 2008), and activation in the VLPFC correlating with perceived control over pain results in a decrease in subjective pain intensity (Salomons et al. 2007).
Based on the theory that non-pulsatile tinnitus can be considered the auditory analogue for deafferentation pain (De Ridder et al. 2011), we hypothesize that the left VLPFC might also be involved in control of tinnitus. Previous research revealed that low (1 Hz)- and high-frequency (>5 Hz) TMS of the prefrontal cortex exerts opposing effects (Speer et al. 2000), with low-frequency TMS being predominantly inhibitory, decreasing metabolism, while high-frequency TMS has an excitatory effect increasing metabolism (Kimbrell et al. 1999; Speer et al. 2000). Hence, we conducted a TMS study verifying whether potentially inhibitory or excitatory modulation of the left VLPFC by respectively using low- and high-frequency TMS can modulate the loudness of tinnitus.
Methods
Patients
We studied 60 patients (male: 36, female: 24) with chronic tinnitus (>1 year). The mean age was 50.05 years (SD = 11.77). Twenty-two patients had unilateral tinnitus, and 38 patients had bilateral tinnitus. Twenty-two patients had a pure tone tinnitus, and 38 patients had narrow band noise tinnitus. The mean tinnitus duration was 8.33 years (SD = 9.47).
All participants underwent a complete audiological, ENT and neurological investigation to rule out possible treatable causes for their tinnitus. All patients had a reduction in their hearing, but no patient had hyperacusis.
The study has been approved by the Antwerp University Hospital IRB (‘Comité voor medische ethiek’). Patients gave an informed consent.
TMS
TMS is performed as a routine neuromodulation technique for the diagnosis of tinnitus in the multidisciplinary TRI tinnitus clinic of the University of Antwerp, Belgium.
The motor threshold to TMS is first determined by placing the coil over the motor cortex using EMG. The coil was positioned tangentially to the scalp and oriented so that the induced electrical currents would flow approximately perpendicular to the central sulcus, at 45° angle from the mid-sagittal line. TMS is performed using a super rapid stimulator (Magstim Inc, Wales, UK) with a figure eight coil placed over the left ventrolateral prefrontal cortex (the middle between F3 and FP1 determined by the International 10/20 Electroencephalogram System) (see Fig. 1). To validate the coil positioning, we applied a neuronavigated TMS on two volunteers. Based on this procedure, it can be concluded that the coil positioning indeed targets the VLPFC.
The intensity of the stimulation is set at 80 % of the motor threshold (MT), because 80 % MT is the lowest intensity known to elicit metabolic changes when stimulating the adjacent dorsolateral prefrontal cortex (Speer et al. 2003). This threshold at the dorsolateral prefrontal cortex modulates the ipsilateral auditory cortex, whereas 100 % MT has contralateral auditory cortex activation and 120 % bifrontal activation (Nahas et al. 2001). Thus, the minimal intensity known to still modulate the auditory cortex is 80 % MT. In other words, using a higher stimulation threshold might exert effects on multiple different pathways and be theoretically less specific.
Twenty-one patients received in random order sham and 1-Hz stimulation, while thirty-nine patients received in random order sham and 10-Hz stimulation. Patients were assigned randomly to the 1- or 10-Hz condition, without a predefined number of how many patients needed to be assigned to one of the two conditions. Each stimulation session consisted of 200 pulses. When tinnitus loudness is back to its initial score, the next TMS stimulation type was applied. The presence of a control procedure (i.e. placebo effect) is tested by placing the coil perpendicular to the frontal area for the same frequency. All patients were wearing earplugs during the TMS session.
Evaluation
A visual analogue scale (VAS) for tinnitus loudness (‘How loud do you perceive your tinnitus?: 0 = no tinnitus and 10 = as loud as imaginable’) was asked before (pre) and directly after both sham and real TMS stimulation.
Statistical analysis
Calculations were performed using SPSS software package. Repeated measures ANOVA was conducted with tinnitus loudness (baseline, sham and real treatment) as within-subjects variable and stimulation frequency (1 vs. 10 Hz) as stimulation design as between-subjects variable. A similar analysis was conducted with tinnitus loudness (baseline, sham and real treatment) as within-subjects variable and stimulation order (first sham versus first real stimulation) as between-subjects variable.
The sample size for the patients who received 10 Hz was larger than the patient group who received 1-Hz stimulation. This unbalanced design may lead to an overpowering for the 10-Hz group. Hence, we conducted a resampling analysis (i.e. bootstrapping) in which we draw 22 participants from the 10-Hz group and tested whether the same results are obtained in this randomly selected smaller group. This process is repeated 1,000 times.
A linear regression analysis was conducted with tinnitus type, tinnitus laterality and tinnitus duration as independent variables and tinnitus loudness as dependent variables for the stimulation parameters (1, 10 Hz and total). The dependent variables were computed by making the subtraction between ‘tinnitus loudness for each stimulation parameter’ minus sham scores. These scores give an indication of the net effect of the stimulation. The independent variables tinnitus type and tinnitus laterality were recorded in contrast variables, tinnitus type (narrow band noise and pure tone) and tinnitus laterality (bilateral and unilateral).
Responders are defined as patients who improve after the TMS session on their tinnitus loudness, while non-responders are defined as patients who had no improvement after TMS treatment on tinnitus loudness.
Results
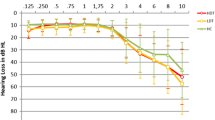
Patients report a mean tinnitus loudness of 6.72/10 (SD = 1.63/10) on a VAS before the TMS treatment. A repeated measures ANOVA revealed a significant main effect for tinnitus loudness (F = 9.14, p < .001). Multiple comparisons with Bonferonni correction indicated that after real stimulation, a significant (p < .05) lower score on the VAS tinnitus loudness was demonstrated in comparison with respectively baseline measurement and sham stimulation (See Table 1). In addition, also a significant difference was obtained between baseline measurement and sham stimulation, indicating that sham had a significantly lower VAS tinnitus loudness score than baseline measurement (See Table 1). No significant main effect was obtained for stimulation type (F = 1.68, p = .20). However, a significant interaction effect was revealed between measurement (baseline, sham and real) and stimulation type (F = 8.90, p < .001; see Fig. 2). Simple contrast analysis revealed that there was no significant difference between baseline VAS tinnitus loudness scores (F = 1.69, p = .20) in the 1- and 10-Hz stimulation group. A second simple contrast demonstrated that for the sham group, there was no significant difference between 1-Hz and 10-Hz stimulation (F = .02, p = .97). A third simple contrast, however, yielded a significant effect revealing that 10-Hz stimulation leads to a significantly lower mean VAS tinnitus loudness score in comparison with 1-Hz stimulation (F = 8.27, p < .01). Additional simple contrasts show that for the 10-Hz stimulation, real stimulation had a significantly lower mean VAS tinnitus loudness score than respectively baseline (F = 41.46, p < .001) and sham stimulation (F = 31.66, p < .001) (see Table 1).
In addition, a repeated measures ANOVA controlling for the stimulation order (first sham versus first reals stimulation) revealed no significant effect for order (F = .22, p = .64), indicating that the order of stimulation had no influence on the obtained effect.
To make sure that the obtained findings are not the result of an overpowering of the 10-Hz group (i.e. larger sample size in comparison with the 1-Hz group), we applied a resampling bootstrapping technique. Based on this technique, we also find a significant main effect for tinnitus loudness (range of F = 4.691–14.76, respectively p < .05 and p < .001) and a significant interaction effect (range of F = 5.621–12.672, respectively p < .05 and p < .001) indicating the same effects as with the unbalanced sample size and suggesting a robust effect.
A linear regression analysis demonstrated that the amount of suppression for tinnitus intensity and tinnitus-related distress was independent of tinnitus laterality, tinnitus type and tinnitus duration for both 1 Hz (F = .60, p = .62), 10 Hz (F = .81, p = .50) and total (1 + 10 Hz; F = .76, p = .52) (see Table 2).
For the 10-Hz stimulation, 35 tinnitus patients (89.74 %) have no response for the sham treatment and were further analysed. Exclusion of responders to the sham procedure is performed to exclude the possible influence of sound from the TMS masking the tinnitus as the TMS equipment generates a clicking sound on each pulse delivery. A significant suppression effect was obtained for tinnitus loudness indicating a suppression effect of 21.86 % for tinnitus loudness. However, of these 35 participants who did not respond to the sham procedure, 14 (40 %) showed no suppressive response to stimulation, and 21 patients (60 %) were TMS responders. For this latter group, mean transient tinnitus suppression was 36.66 % for tinnitus loudness.
Discussion
This is the first study to describe the effect of TMS on the left VLPFC for the modulation of tinnitus loudness. Our results show that 10-Hz stimulation can modulate tinnitus loudness, while 1-Hz stimulation does not seem to exert the same effect. The amount of suppression on tinnitus loudness was independent of tinnitus laterality, tinnitus type and tinnitus duration, suggesting a more general modulatory activity.
The results show that low- and high-frequency left VLFPC TMS yield different effects on tinnitus loudness. As high-frequency TMS (i.e. 10 Hz) leads to a temporary increase in cortical excitability and low-frequency TMS (i.e. 1 Hz) usually reduces cortical excitability (Chen 2000), it can be hypothesized that 10-Hz TMS might excite the left VLPFC, thereby reducing tinnitus loudness. The fact that tinnitus loudness is reduced by 10-Hz stimulation but not by 1-Hz rTMS should be further explored; however, a hypothesis can be proposed.
It is known that the VLPFC mediates the analgesic effect of expected and perceived control over pain (Wiech et al. 2006, 2008). As tinnitus can be considered analogous to deafferentation pain (Tonndorf 1987; Moller 2000; De Ridder et al. 2007a, 2011), it is possible that stimulating the left VLPFC gives patients more ability that they can control their tinnitus. One might expect that inhibiting the left VLPFC due to low-frequency TMS could also worsen the tinnitus. However, we did not find any worsening of the tinnitus. This might be due to the fact that patients received only one session, or that a decrease in metabolic activity does not parallel clinical changes. PET-scan studies have demonstrated that TMS not only modulates the directly stimulated cortical area, but that it has an effect on remote areas functionally connected to the stimulated area (Hallett 2000; Kimbrell et al. 2002). The VLPFC is involved in processing non-spatial acoustic information as evidenced by the fact that it receives afferents from physiologically and anatomically defined auditory cortical areas (Romanski and Goldman-Rakic 2002). Thus, stimulating the VLPFC can indirectly modulate the auditory cortex thereby changing the tinnitus percept. Furthermore, auditory cortex TMS at both low and high frequencies does not necessarily produce opposite effects (De Ridder et al. 2007c, b; Khedr et al. 2008).
One limitation of this study relates to the coil positioning. These were not performed under neuronavigated control and were only defined by anatomical landmarks. Yet, recent studies for TMS demonstrated that consistent results can be obtained with a probabilistic approach (i.e. non-neuronavigated) (Langguth et al. 2010), and that using the 10-20 EEG system as coordinates can be successfully applied in determining coil positioning (Langguth et al. 2006). In addition, a post hoc analysis indeed revealed that using the middle between F3 and FP1 targets the VLPFC. Nevertheless, even if fMRI-guided stimulation might be accurate within the range of millimetres for targeting purposes, the area of modulation might still be as large as 3 cm (Cohen et al. 1990), questioning the value of fMRI-guided TMS at least at the level of the auditory cortex (De Ridder et al. 2005). This pilot study does not provide any working mechanism of why and how left VLPFC stimulation influences tinnitus loudness. Thus, a control study should be performed associating TMS with functional imaging modalities.
In conclusion, 10-Hz TMS seems to influence the loudness of tinnitus. Our findings give further support to the fact that non-auditory areas are involved in tinnitus. Combining this stimulation method with functional imaging will refine our knowledge of the neural circuits involved in auditory phantom perceptions such as chronic tinnitus.
References
Chen R (2000) Studies of human motor physiology with transcranial magnetic stimulation. Muscle Nerve Suppl 9:S26–S32
Cohen LG, Roth BJ, Nilsson J et al (1990) Effects of coil design on delivery of focal magnetic stimulation. Technical considerations. Electroencephalogr Clin Neurophysiol 75:350–357
Davidson D (1995) Cerebral asymmetry, emotion and affective style. MIT, Cambridge
De Ridder D, Verstraeten E, Van der Kelen K et al (2005) Transcranial magnetic stimulation for tinnitus : influence of tinnitus duration on stimulation parameter choice and maximal tinnitus suppression. Otol Neurotol 26:616–619
De Ridder D, De Mulder G, Menovsky T, Sunaert S, Kovacs S (2007a) Electrical stimulation of auditory and somatosensory cortices for treatment of tinnitus and pain. Prog Brain Res 166:377–388
De Ridder D, van der Loo E, Van der Kelen K, Menovsky T, van de Heyning P, Moller A (2007b) Do tonic and burst TMS modulate the lemniscal and extralemniscal system differentially? Int J Med Sci 4:242–246
De Ridder D, van der Loo E, Van der Kelen K, Menovsky T, van de Heyning P, Moller A (2007c) Theta, alpha and beta burst transcranial magnetic stimulation: brain modulation in tinnitus. Int J Med Sci 4:237–241
De Ridder D, Elgoyhen AB, Romo R, Langguth B (2011) Phantom percepts: tinnitus and pain as persisting aversive memory networks. Proc Natl Acad Sci USA. doi:10.1073/pnas.1018466108
Hallett M (2000) Transcranial magnetic stimulation and the human brain. Nature 406:147–150. doi:10.1038/35018000
Jastreboff PJ (1990) Phantom auditory perception (tinnitus): mechanisms of generation and perception. Neurosci Res 8:221–254
Keedwell PA, Andrew C, Williams SC, Brammer MJ, Phillips ML (2005) A double dissociation of ventromedial prefrontal cortical responses to sad and happy stimuli in depressed and healthy individuals. Biol Psychiatry 58:495–503. doi:10.1016/j.biopsych.2005.04.035
Khedr EM, Rothwell JC, Ahmed MA, El-Atar A (2008) Effect of daily repetitive transcranial magnetic stimulation for treatment of tinnitus: comparison of different stimulus frequencies. J Neurol Neurosurg Psychiatry 79:212–215. doi:10.1136/jnnp.2007.127712
Khedr EM, Rothwell JC, El-Atar A (2009) One-year follow up of patients with chronic tinnitus treated with left temporoparietal rTMS. Eur J Neurol 16:404–408. doi:10.1111/j.1468-1331.2008.02522.x
Kimbrell TA, Little JT, Dunn RT et al (1999) Frequency dependence of antidepressant response to left prefrontal repetitive transcranial magnetic stimulation (rTMS) as a function of baseline cerebral glucose metabolism. Biol Psychiatry 46:1603–1613
Kimbrell TA, Dunn RT, George MS et al (2002) Left prefrontal-repetitive transcranial magnetic stimulation (rTMS) and regional cerebral glucose metabolism in normal volunteers. Psychiatry Res 115:101–113
Kleinjung T, Eichhammer P, Langguth B et al (2005) Long-term effects of repetitive transcranial magnetic stimulation (rTMS) in patients with chronic tinnitus. Otolaryngol Head Neck Surg 132:566–569. doi:10.1016/j.otohns.2004.09.134
Kleinjung T, Eichhammer P, Landgrebe M et al (2008) Combined temporal and prefrontal transcranial magnetic stimulation for tinnitus treatment: a pilot study. Otolaryngol Head Neck Surg 138:497–501. doi:10.1016/j.otohns.2007.12.022
Landgrebe M, Langguth B, Rosengarth K et al (2009) Structural brain changes in tinnitus: grey matter decrease in auditory and non-auditory brain areas. Neuroimage 46:213–218. doi:10.1016/j.neuroimage.2009.01.069
Langguth B, Zowe M, Landgrebe M et al (2006) Transcranial magnetic stimulation for the treatment of tinnitus: a new coil positioning method and first results. Brain Topogr 18:241–247. doi:10.1007/s10548-006-0002-1
Langguth B, de Ridder D, Dornhoffer JL et al (2008) Controversy: does repetitive transcranial magnetic stimulation/transcranial direct current stimulation show efficacy in treating tinnitus patients? Brain Stimul 1:192–205. doi:10.1016/j.brs.2008.06.003
Langguth B, Kleinjung T, Landgrebe M, de Ridder D, Hajak G (2010) rTMS for the treatment of tinnitus: the role of neuronavigation for coil positioning. Neurophysiol Clin 40:45–58. doi:10.1016/j.neucli.2009.03.001
Lanting CP, de Kleine E, van Dijk P (2009) Neural activity underlying tinnitus generation: results from PET and fMRI. Hear Res 255:1–13. doi:10.1016/j.heares.2009.06.009
Llinas RR, Ribary U, Jeanmonod D, Kronberg E, Mitra PP (1999) Thalamocortical dysrhythmia: a neurological and neuropsychiatric syndrome characterized by magnetoencephalography. Proc Natl Acad Sci USA 96:15222–15227
Lockwood AH, Salvi RJ, Burkard RF, Galantowicz PJ, Coad ML, Wack DS (1999) Neuroanatomy of tinnitus. Scand Audiol Suppl 51:47–52
Moller AR (2000) Similarities between severe tinnitus and chronic pain. J Am Acad Audiol 11:115–124
Muhlnickel W, Elbert T, Taub E, Flor H (1998) Reorganization of auditory cortex in tinnitus. Proc Natl Acad Sci USA 95:10340–10343
Nahas Z, Lomarev M, Roberts DR et al (2001) Unilateral left prefrontal transcranial magnetic stimulation (TMS) produces intensity-dependent bilateral effects as measured by interleaved BOLD fMRI. Biol Psychiatry 50:712–720
Ochsner KN, Gross JJ (2005) The cognitive control of emotion. Trends Cogn Sci 9:242–249. doi:10.1016/j.tics.2005.03.010
Rauschecker JP, Leaver AM, Muhlau M (2010) Tuning Out the Noise: limbic-Auditory Interactions in Tinnitus. Neuron 66:819–826
Romanski LM, Goldman-Rakic PS (2002) An auditory domain in primate prefrontal cortex. Nat Neurosci 5:15–16. doi:10.1038/nn781
Salomons TV, Johnstone T, Backonja MM, Shackman AJ, Davidson RJ (2007) Individual differences in the effects of perceived controllability on pain perception: critical role of the prefrontal cortex. J Cogn Neurosci 19:993–1003. doi:10.1162/jocn.2007.19.6.993
Speer AM, Kimbrell TA, Wassermann EM, Repell JD, Willis MW, Herscovitch P, Post RM (2000) Opposite effects of high and low frequency rTMS on regional brain activity in depressed patients. Biol Psychiatry 48:1133–1141
Speer AM, Willis MW, Herscovitch P et al (2003) Intensity-dependent regional cerebral blood flow during 1-Hz repetitive transcranial magnetic stimulation (rTMS) in healthy volunteers studied with H215O positron emission tomography: II. Effects of prefrontal cortex rTMS. Biol Psychiatry 54:826–832
Tomarken AJ, Davidson RJ, Wheeler RE, Doss RC (1992) Individual differences in anterior brain asymmetry and fundamental dimensions of emotion. J Pers Soc Psychol 62:676–687
Tonndorf J (1987) The analogy between tinnitus and pain: a suggestion for a physiological basis of chronic tinnitus. Hear Res 28:271–275
van der Loo E, Gais S, Congedo M et al (2009) Tinnitus intensity dependent gamma oscillations of the contralateral auditory cortex. PLoS One 4:e7396 (7391–7395). doi:10.1371/journal.pone.0007396
Vanneste S, Plazier M, Ost J, van der Loo E, Van de Heyning P, De Ridder D (2010a) Bilateral dorsolateral prefrontal cortex modulation for tinnitus by transcranial direct current stimulation: a preliminary clinical study. Exp Brain Res 202:779–785. doi:10.1007/s00221-010-2183-9
Vanneste S, Plazier M, van der Loo E, Van de Heyning P, De Ridder D (2010b) The difference between uni-and bilateral auditory phantom percept. Clin Neurophysiol. doi:10.1016/j.clinph.2010.07.022
Wager TD, Davidson ML, Hughes BL, Lindquist MA, Ochsner KN (2008) Prefrontal-subcortical pathways mediating successful emotion regulation. Neuron 59:1037–1050. doi:10.1016/j.neuron.2008.09.006
Weisz N, Muller S, Schlee W, Dohrmann K, Hartmann T, Elbert T (2007) The neural code of auditory phantom perception. J Neurosci 27:1479–1484
Wiech K, Kalisch R, Weiskopf N, Pleger B, Stephan KE, Dolan RJ (2006) Anterolateral prefrontal cortex mediates the analgesic effect of expected and perceived control over pain. J Neurosci 26:11501–11509. doi:10.1523/JNEUROSCI.2568-06.2006
Wiech K, Ploner M, Tracey I (2008) Neurocognitive aspects of pain perception. Trends Cogn Sci 12:306–313. doi:10.1016/j.tics.2008.05.005
Acknowledgments
The authors thank Jan Ost, Bram Van Achteren, Bjorn Devree and Pieter van Looy for their help in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vanneste, S., De Ridder, D. The involvement of the left ventrolateral prefrontal cortex in tinnitus: a TMS study. Exp Brain Res 221, 345–350 (2012). https://doi.org/10.1007/s00221-012-3177-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-012-3177-6