Abstract
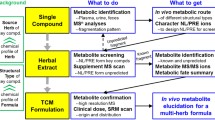
The toxicity assessment of herbal medicines is important for human health and appropriate utilization of these medicines. However, challenges have to be overcome because of the complexity of coexisting multiple components in herbal medicines and the highly interconnected organismal system. In this study, a target profiling approach was established by combining the characteristic fingerprint analysis of herbal chemicals with potential toxicity through a precursor ion scan-based mass spectroscopy and the target profiling analysis of biomarkers responsible for the toxicity. Through this newly developed approach, the comparative hepatotoxicity assessment of two herbal medicines from the same genus, Senecio vulgaris L. and Senecio scandens Buch.-Ham, was performed. Significant differences were found between the two species in their chemical markers (i.e., pyrrolizidine alkaloids) and biomarkers (i.e., bile acids) responsible for their toxicities. This result was consistent with the conventional toxicity assessment conducted by histopathological examination and clinical serum index assay on experimental animal models. In conclusion, this study provided a new approach for the hepatotoxicity assessment of herbal medicines containing pyrrolizidine alkaloids, which are widely distributed in various herbal medicines. The target profiling approach may shed light on the toxicity assessment of other herbal medicines with potential toxicity.

The comparative hepatotoxicity assessment of two herbal medicines, Senecio vulgaris L. (SV) and Senecio scandens Buch.-Ham (SS), was performed by combining the characteristic fingerprint analysis of toxic chemical markers (i.e. pyrrolizidine akaloids) through a precursor ion scan-based mass spectroscopy and the target profiling analysis of toxic biomarkers (i.e. bile acids). It was found that SV was highly hepatotoxic as they contained higher concentration of toxic chemicals, which induced significant changes in the bile acid profile by the transcriptional regulation of their synthesis, excretion, and uptake
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Herbal medicines are reputed for their efficacy and safety for the prevention and treatment of various diseases. However, international attention has focused on their potential toxicities [1, 2] because of the unfortunate medical disaster caused by the aristolochic acids from Aristolochia fangchi (Guang fangji), which was mistaken for the traditional Chinese medicine Stephania tetrandra (Fen fangji) [3]. Moreover, global interests in the safety of herbal medicines have grown [4–10]. However, compared with the safety of pharmaceutical medicines, the toxicity investigations for herbal medicines are considerably more difficult because of the three following aspects: First, it is definite that the authentication of herbal medicines is the first and key step for their toxicity investigation. The authentication of herbal medicines—misidentification, name confusion, and substitution or adulteration can occur, impacting on safety; second, the coexisting multiple components of herbal medicines may vary with numerous factors, such as seasonal changes, age, and cultural environment within one species [11, 12], that contribute to the various observations of the toxic effects; third, the complex and highly interconnected human body system is dynamically regulated within boundaries, the so-called homeostasis, which may be disturbed or compromised by certain stimuli and xenobiotics, such as the chemicals from herbal medicines. The later two aspects act together and make toxicity investigations more difficult.
Pyrrolizidine alkaloids (PAs) are a type of natural toxins. PAs are widely distributed in more than 6000 flowering plants, especially those from the family of Asteraceae, Boraginaceae, and Fabaceae [13–15]. PAs are hepatotoxic to humans and livestock by the ingestion of PA-containing plants and herbal medicinal products. PAs are esters with a necic acid and necine moieties, which could be either 1,2-unsaturated or saturated (Fig. 1). Based on the representative necine bases, PAs are generally classified into three types, namely, retronecine, otonecine, and platynecine. The retronecine PAs can be N-oxidized, thus, enlarging the PA family. With the combination of necines with necic acids, the family is now composed of about 660 members, which includes more than 350 retronecine PAs and their almost equally numbered N-oxidants, as well as lesser-numbered otonecine PAs. Although the structures of PAs vary, characteristic product ions can be generated for each type of PA in the MS/MS fragmentation, which is m/z 120 and 138 for retronecine, m/z 150 and 168 for otonecine, and m/z 122 and 140 for platynecine (Fig. 1) [16–18]. Precursor ion scan (PIS) is a typical target scanning of all compounds with similar molecular structures. For the high selectivity and high sensitivity of this technique for precursor ions and fragment ions, PIS has been used for the target profiling of certain active components of herbal materials recently [17, 19, 20]. Therefore, a selective, sensitive, and high-throughput profiling of the PA structures in herbs can be achieved through the PIS analysis of these characteristic product ions [17], which should be promising for the chemical illustration of the toxicity of herbal medicines containing PAs.
PAs produce irreversible chronic and acute hepatotoxic effects [15]. Over 8,000 PA-caused poisoning cases, with estimated 2,000 deaths, have been reported in numerous countries, such as Afghanistan, China, Ethiopia, Iraq, South Africa, and Uzbekistan [21–25]. With the threat PA imposes on human health, guidelines on the prevention of PA exposure have been enacted in several countries and organizations [21, 26, 27]. Considerable attention has been given for the toxicological research of PAs and herbal medicines containing PAs, in which disturbed homeostasis of endogenous signaling biomarkers, such as amino acids and bile acids, were found [28–31]. Moreover, increased serum bile acid is regarded as the most sensitive index of hepatic function caused by PAs [29, 30]. Our previous study showed that the bile acid homeostasis is compromised by senecionine treatment [32]. As the major endogenous metabolites of cholesterol, bile acids are commonly associated with liver injury. Apparent changes can be observed in the concentrations of the individual bile acids and the whole profile [33–36]. A study on progressive human non-alcoholic fatty liver disease revealed a transition from the classical pathway to the alternative pathway of bile acid synthesis in the liver of patients by analysis of the hepatic levels of bile acids and the expression of genes associated with bile acids metabolism [34]. Conclusively, bile acid profiling does not only reflect the different pathological changes, but it also provides insights for the underlying pathogenesis. Thus, the target profiling of bile acids might shed new light on the hepatotoxicity assessment of herbal medicines containing PAs.
PAs are reported to occur in many medicinal herbs in Europe and China [13, 14], especially those from Senecio genus, such as Senecio vulgaris L. (SV) and Senecio scandens Buch.-Ham. (SS). SV is used as an emmenagogue in Europe [13]. However, the consumption of herbal tea containing SV caused several deaths because of the high contents of several toxic PAs [13, 37, 38]. Therefore, SV was restricted for medical use. In contrast, SS is widely distributed in China, as well as India, Japan, Nepal, and other countries. SS is officially recorded in Chinese Pharmacopeia [27] and used in single or as an ingredient in more than 100 preparations, mainly for anti-inflammatory purposes. Although no study on its toxicity has been reported, several PAs have been found in SS [39, 40]. Thus, the toxicity assessment of SS is urgently needed for human health and better utilization of this herbal medicine. In this study, the two target profiling analyses, namely, PIS-based target profiling of PAs and metabolomic profiling of bile acids, were firstly integrated for the hepatotoxicity assessment of two herbal medicines from the same genus. The methodology established in this study might also be beneficial for illustrating the relationship of chemical markers and toxic biomarkers of other herbal medicines with potential toxicity.
Experimental
Chemicals and reagents
Senecionine, integerrimine, seneciphylline, spartiodine, and senkirkine were isolated from the aerial part of SV (collected from Jilin, China). Retrorsine was purchased from Sigma-Aldrich. Co. (St. Louis, MO, USA). Adonifoline was isolated from the aerial part of SS (collected form Yunnan, China) and used as standard reference for semi-quantification of PAs. All PAs were identified by comparing their 1H and 13C NMR data with Refs. [41–45] (see Electronic Supplementary Material (ESM), Fig. S1, Table S1 and S2). The purity of adonifoline was determined to be more than 98 % by normalization of the peak areas detected by HPLC-DAD as well as HPLC-MS. N-oxides of adonifoline, senecionine, and retrorsine were prepared by oxidation of adonifoline, senecionine, and retrorsine, respectively, according to Ref. [16]. Bile acids standards are purchased from Sigma-Aldrich. Co. (St. Louis, MO, USA), including cholic acid (CA), lithocholic acid (LCA), deoxycholic acid (DCA), chenodeoxycholic acid (CDCA), ursodeoxycholic acid (UDCA), hyodeoxycholic acid (HDCA), glycocholic acid (GCA), glycodeoxycholic acid (GDCA), glycochenodeoxycholic acid (GCDCA), glycoursodeoxycholic acid (GUDCA), glycolithocholic acid (GLCA), taurocholic acid (TCA), taurodeoxycholic acid (TDCA), taurochenodeoxycholic acid (TCDCA), tauroursodeoxycholic acid (TUDCA), taurohyodeoxycholic acid (THDCA), and taurolithocholic acid (TLCA).
Acetonitrile was of HPLC grade and purchased from Fisher Scientific Co. (Santa Clara, CA, USA). Ammonium formate and ammonium acetate were of HPLC grade and purchased from Sigma-Aldrich Co. (St. Louis, MO, USA). Formic acid (98 %), ammonia solution (25 %) and methanol were of analytical grade and purchased from Shanghai Reagent Co. (Shanghai, P.R. China). Water was purified with a Milli-Q system (Millipore, Bedford, MA, USA).
Herbal materials
SS and SV were collected in their flowering season, i.e., early summer to late autumn, from typical sources both in China and abroad (Table 1). All the samples were authenticated by Professor Zhengtao Wang and naturally dried in air. The voucher specimens were deposited in the herbarium of the Institute of Chinese Materia Medica, SHUTCM. The herbal materials were dried at 60 °C overnight and powdered.
For chromatographic fingerprint analysis, samples were prepared following our reported method [46]: 0.5 g of powder was extracted with 50 mL of 0.5 % formic acid solution (v/v) by ultrasonication. For toxicity evaluation on experimental animals, herbal extracts were prepared using the following procedure: 500 g of herbal crude powders were boiled twice with water (10 volumes) for 2 h. The extracts were pooled and vacuum concentrated to 10 g crude herb/ml.
Bio-samples
Animal experiments
Male Sprague-Dawley rats (n = 30, 200–220 g, at 6–8 weeks of age) were obtained from the Laboratory Animal Center of SHUTCM. The animal welfare practices and the animal experimental protocols were strictly consistent with the Guide for the Care and Use of Laboratory Animals and the related ethics regulations of SHUTCM. The rats were maintained in a controlled environment with a temperature of 22 ± 2 °C and a relative humidity of 55 ± 5 % under a 12-h light/dark cycle. The rats were fed with a commercial pellet diet and tap water ad libitum and acclimatized for 1 week before experimentation. Prior to treatment, animals were divided randomly into three groups (10 for each group) and fasted overnight. Group I (VEH group), group II (SS group), and group III (SV group) were orally treated with the same volume of sodium chloride, SS extract, and SV extract, respectively, equivalent to 80 g crude drug/kg. Each animal was anesthetized with sodium pentobarbital for sample collection 36 h after dosage.
Serum
Blood samples were collected and left to coagulate for 2 h at room temperature and then centrifuged at 800 g for 10 min at 4 °C. The serum samples were then collected for serum clinical biochemistry indexes examination and bile acid profiling analyses. Alanine aminotransferase (ALT) activity, aspartate aminotransferase (AST) activity, and total bilirubin (TBIL) level were measured using a Hitachi Automatic Analyzer 7080 (Hitachi High-Tech Science Systems Corp., Ibaraki, Japan). An aliquot of 200 μl of serum was mixed with 600 μl of methanol, followed by 1 min of vortex mixing; after centrifugation at 15,000 g for 15 min at 4 °C, the supernatant was separated and applied for bile acid profiling.
Liver tissues
The liver samples were collected for histological analysis by hematoxylin and eosin staining and quantitative real-time polymerase chain reaction analysis (RT-PCR) following the method provided in supporting information (see ESM, Table S3).
Target profiling analyses
Chromatographic fingerprint of pyrrolizidine alkaloids
Chromatographic separation of herbal samples were following our reported method [50] via a Waters ACQUITY UPLC TQD™ system (Waters Corporation, Milford, USA) with gradient elution of acetonitrile and 10 mM ammonium formic modified by the addition of 0.1 % (v/v) ammonia solution (25 %). For screening of PAs by PIS approach, MS parameters were set as follows: detection mode, positive ion mode; capillary voltage, 3.5 kV; cone voltage, 45 V; source temperature, 150 °C; desolvation temperature, 450 °C; desolvation gas (nitrogen), 900 L/h; cone gas (nitrogen), 50 L/h; mass scan range, m/z 150–650; parent ion scan channel, m/z 120 and 138 for retronecine and their N-oxides, m/z 122 and 140 for platynecine, m/z 150 and 168 for otonecine (Fig. 1) [14, 16–18]; collision energy, 30 eV. For semi-quantification of main hepatotoxic PAs (HPAs), full scan (at positive ion mode) method was introduced and parameters were set as reported [46]. Extracted ion chromatogram (EIC) of each target compound was integrated and the peak area was used for calculating its contents in herbal samples.
Metabolomic profiling of bile acids
Bile acid profiling analysis was performed with modification of our reported method [35] via a Waters ACQUITY UPLC ZQ2000 system (Waters Corporation, Milford, USA) with gradient elution of methanol and 5 mM ammonium acetate modified by the addition of 0.1 % (v/v) ammonia solution (25 %).
Statistical analysis
Target profiling data were acquired and processed using MassLynx 4.1 software (Waters Corp., Milford, MA, USA). SIMCA-P 12.0 (Umetrics, Umea, Sweden) and SPSS 16.0 software (SPSS, Inc., Chicago, IL, USA) were used for principal component analysis (PCA), orthogonal projection to latent structures-discriminant analysis (OPLS-DA), and correlation analysis. All quantitative data, including contents of PAs, serum indexes (ALT activity, AST activity, and TBIL level), serum concentrations of each single bile acid, hepatic mRNA levels of genes by quantitative RT-PCR, were expressed as mean ± standard error of mean (mean ± SEM) and statistically analyzed using two-tailed unpaired Student’s t test.
Results and discussion
Conventional hepatotoxicity evaluation of herbal medicines
The liver sections stained by hematoxylin and eosin were histopathologically assessed for the extent of the acute liver injury induced by SS and SV (Fig. 2). Compared with the VEH group, animals exposed to SS showed no significant changes. However, those exposed to SV showed blood stasis and significant inflammation, which suggest severe liver injury.
Histological and biochemical findings of toxicity caused by Senecio vulgaris and S. scandens on rats. Rats were treated with herbal extracts equal to 80 g crude drug/kg body weight. a, b, and c show histological examination results of liver sections of rats in the control group, SS treatment group, and SV treatment group, respectively. The bar represents 200 μm. d, e, and f show serum ALT activity, AST activity, and TBIL level, respectively. Values are expressed as mean ± SEM (n = 10 for each group); significant differences between the control group and SV or SS treatment group are based on two-tailed unpaired Student’s t test (* p < 0.05, ** p < 0.01 and *** p < 0.001)
The serum ALT and AST activities, and TBIL level are common indexes used in clinical medicine to evaluate hepatotoxicity. These indexes are significantly elevated after exposure to PAs [23–25]. In this study, the serum ALT and AST activities in SV group increased 24-fold (1046 IU/L in SV group vs. 43 IU/L in VEH group) and 10-fold (2956 IU/L in SV group vs. 286 IU/L in VEH group), respectively. In addition, serum TBIL level in SV group increased four fold (3.2 μmol/L in SV group vs. 0.8 μmol/L in VEH group). However, no obvious changes were observed in SS group. Significant differences among these indexes were found between SV and SS groups, with elevated ALT and AST activities, and TBIL level in SV group. These results indicated that evident differences were present in the hepatotoxicities of these two Senecio species, and that SV exposure could induce severe hepatic injury.
Chromatographic fingerprint analysis
Screening of PAs in herbal materials
The total ion chromatogram (TIC) of each PIS channel was obtained (Fig. 3). Compared with the full scanning of all existing components in herbal material, the PIS chromatogram can evidently mitigate endogenous interferences, which significantly increased the sensitivity for detecting PAs in herbal materials [17]. As a result, 44 PAs were screened, including 32 retronecine PAs, one otonecine PA, and 11 platynecine PAs (Table 2). In addition, 11 retronecine PAs were further specified as N-oxidative through their characterized ion clusters at m/z 118–120 and 136–138 [16, 18]. Moreover, SV consisted of 35 PA structures, wherein 27 structures were with hepatotoxic potential. Meanwhile, SS consisted of 17 PA structures with 10 HPAs.
Multivariate statistical analysis
PCA was performed with the mass spectrometry intensities of the 44 PAs screened. The PCA scores plot (Fig. 4a) shows that two Senecio species were clearly separated by the first principal component. An OPLS-DA model [46, 47] was generated to determine the most significant compounds between SS and SV (Fig. 4b). The S-plot combines the covariance (the contribution of variations to the model, as X-axis) and correlation (the reliability of variations to the model, as Y-axis). Variations in the significant covariance and correlation values are most likely to be considered as the potential markers that can discriminate between groups. In this study, PAs in the right-up phase were abundant in SV, while PAs in the left-bottom phase were abundant in SS (Fig. 4c). The results show that SV contained substantially more PAs. R03 (m/z 334.1, 6.4 min), R04 (m/z 334.1, 6.5 min), R05 (m/z 336.1, 6.9 min), R06 (m/z 336.1, 7.0 min), R11 (m/z 350.2, 3.4 min), R12 (m/z 350.2, 3.5 min), R15 (m/z 352.2, 4.2 min), R16 (m/z 352.2, 4.4 min), R18 (m/z 352.2, 6.2 min), and R29 (m/z 368.2, 3.2 min) were important for SV. In contrast, R25 (m/z 366.2, 3.3 min), R31 (m/z 382.2, 1.8 min), and O01 (m/z 366.2, 4.6 min) were specific for SS.
Multivariate statistical analysis for chromatographic profiling of pyrrolizidine alkaloids in Senecio vulgaris and S. scandens. a shows the PCA score plot; b shows the OPLS-DA score plot; c shows the OPLS-DA S-plot. open circle represents SS group, while filled circle represents SV group. All data were generated by the intensity of PAs detected by UPLC-MS analysis
Among these PAs, 10 PAs, including R03, R04, R05, R06, R16, R18, R25, R29, R31, and O01, showed the same fragments and retention times as with spartioidine, seneciphylline, integerrinine, senecionine, senecionine N-oxide, retrorsine, adonifoline, retrorsine N-oxide, adonifoline N-oxide, and senkirkine, respectively. Thus, they were unequivocally identified. The other three PAs, namely, R11, R12, and R15, were tentatively identified to be spartioidine N-oxide, seneciphylline N-oxide, and integerrimine N-oxide, respectively, based on their MS/MS fragmentations and retention times compared with their isomers (see ESM, Fig. S2).
Semi-quantification of PAs in herbal materials
Most PAs exist in herbs at trace amounts and are not commercially available. Thus, a semi-quantification method can be used to better evaluate the PA contents in herbs. In the latest version of Chinese Pharmacopeia, adonifoline was selected as the standard for the limit detection of PAs in Senecionis Scandentis Herb [27], which is the aerial species of S. scandens Buch.-Ham. In this study, a semi-quantification method of 13 HPAs was established using adonifoline as the standard reference. Generally, a standard curve was obtained by plotting the areas (y) of the adonifoline standards (m/z 366.2, 3.3 min) against their concentrations (x) in the form of y = A + Bx, which was calculated using weighted (1/x) least squares of linear regression. Seven concentration levels, which ranged from 2 to 1000 ng/mL, were prepared in triplicate and used for analysis. Excellent linearity was obtained over the concentration range of 2–1000 ng/mL (r = 0.9995). The limit of quantitation (LOQ) was 2 ng/mL (single to noise ratio (S/N) > 10) with a peak relative standard deviation (RSD) of <5 % (n = 6). The limit of detection (LOD) was 0.5 ng/mL (S/N > 3). The method reproducibility was assessed by analyzing multiple samples (n = 6) of SV01 and SS01. Firstly, the EIC of each PA, i.e. m/z 334.1 for spartioidine and seneciphylline, m/z 336.1 for integerrimine and senecionine, m/z 350.2 for spartioidine N-oxide and seneciphylline N-oxide, m/z 352.2 for integerrimine N-oxide, senecionine N-oxide and retrorsine, m/z 366.2 for adonifoline and senkirkine, m/z 368.2 for retrorsine N-oxide, and m/z 382.2 for adonifoline N-oxide, was recorded and integrated. It was found that the RSDs of the retention time (t R) for each single PA were not more than 0.31 % (see ESM, Table S4). Then, the concentration (Con.) for each single PA was calculated according to their peak area using the standard curve generated by adonifoline. And the RSDs of Con. for each single PA in different herbal samples were not more than 8.15 % (see ESM, Table S4), indicating the method was reproducible. Similarly, the method precision was measured through the intra- and interday variabilities for PAs in multiple samples (n = 5) of SV01 and SS01. Overall, the intraday variabilities for t R and Con. of each single PA were less than 0.31 and 4.76 %, respectively. Meanwhile, the intraday variabilities for t R and Con. of each single PA were less than 0.35 and 9.66 %, respectively (see ESM, Table S5).
The contents of major HPAs in different batches of the two species of herbs were calculated (Table 3). SV generally contained higher contents of HPAs and the contents of the total main HPAs were 0.06–0.14 %. Meanwhile, SS contained lower concentrations of HPAs and adonifoline and its N-oxide are the main HPAs in SS. The average contents of HPAs in SS were 0.0001–0.01 %. SV and SS are two herbs from the same genus, but they reportedly show different toxicities. The differences in the toxicities of the two herbs might be connected with the differences in the constituent PAs. In this study, more kinds of PAs, especially HPAs, were found in SV through PIS approach (27 HPAs in SV vs. 10 HPAs in SS). In addition, the concentrations of the main HPAs were significantly higher in SV than in SS (625.20–1454.72 μg/g in SV vs. 1.20–98.57 μg/g in SS). The recommended dose for SS is 15–30 g/day for adults [27], which is equivalent to 1.35–2.7 g/kg for rats.
In this study, 80 g crude herb/kg of SV01 and SS01 (approximately 30-fold of recommended dose) were administrated to rats to investigate the acute toxicity of these two herbs. The contents of the total HPAs were calculated to be 1284.02 and 98.57 μg/g in SV01 and SS01, respectively, resulting in doses of 1027.22 mg HPAs/kg for the rats in SV group and 7.89 mg HPAs/kg for the rats in SS group. As a result, the rats in SV group evidently showed blood stasis and inflammation, together with significantly high ALT and AST activities (p < 0.001), and serum TBIL levels (p < 0.01) (Fig. 2). However, no evident changes were seen in SS group. These results successfully proved that the differences in the structures and contents of PAs in herbal medicines are positively related to the apparent toxicities of herbal medicines. Furthermore, although PAs are definitely present in SS, their contents are significantly low such that no evident toxicity can be induced by this herbal medicine even at 30-fold of the recommended dose.
Bile acid profiling of serum samples
A total of 15 bile acids were analyzed through our reported method [35, 36] and the bile acid contents of the serum samples from VEH, SS, and SV groups were presented (Fig. 5). The results showed that bile acid concentrations significantly varied among the three groups. Compared with the VEH group, the serum concentrations of the conjugated and free bile acids were greatly elevated in SV group. Three free bile acids, which include DCA, HDCA, and LCA, significantly increased about 3.1-, 2.7-, and 2.0-fold, respectively, in SV group. Moreover, several glycine-conjugated bile acids (such as GCA, GDCA, and GUDCA) and taurine-conjugated bile acids (such as TCA, TDCA, and TUDCA) were also elevated at least 2.0-fold. Among these acids, TCA, TDCA, and TUDCA, were the top three increased bile acids, which increased 6.5-, 5.6-, and 4.0-fold, respectively. In addition, the total glycine-conjugated and taurine-conjugated bile acids significantly increased 3.1- and 5.1-fold, respectively. However, no significant differences were observed in bile acid levels between the VEH group and SS group (Fig. 5).
Contents of serum bile acids significantly changed after exposure to herbal medicines. Values were expressed as mean ± SEM (n = 10); significant differences between the control group and treated group are based on two-tailed unpaired Student’s t test (*p < 0.05 and **p < 0.01). All data were generated through UPLC-MS analysis
The relationship of bile acids homeostasis and hepatotoxicity
A correlation analysis was performed between bile acid groups (DCA, HDCA, LCA, GCA, GDCA, GUDCA, TCA, TDCA, and TUDCA) and conventional clinical biochemical indicators (ALT, AST, and TBIL) (Table 4). The results show that the profiles of the nine bile acids were closely correlated with the ALT and AST activities, and TBIL level, suggesting that the bile acids are important biomarkers for the evaluation of hepatotoxicity caused by exposure to PA-containing herbs.
Bile acids are modulated at the transcriptional level by several nuclear receptors and their downstream genes [48–50]. Therefore, the hepatic mRNA levels of several genes involved in bile acid metabolism of rats in SV-treated group were analyzed and compared with those in the control group (Fig. 6). The genes encoded with two nuclear receptors related to bile acid synthesis, namely, farnesoid X receptor (FXR) and short heterodimer partner (SHP), were significantly inhibited, suggesting severe liver injury and cholestasis [51–53]. These findings were consistent with the highly elevated TBIL level (Fig. 2), which is conventionally used as the chemical indicator for cholestasis in clinical settings. Moreover, the bile acid-CoA:amino acid N-acyltransferase (BAAT) expression decreased, suggesting a reduced conversion of bile acids from their toxic free forms to their less toxic conjugated forms. BAAT is one of the target genes of FXR [54] and deficiency of it could cause intrahepatic cholestasis [55]. This phenomenon was also proven by the elevated serum levels of several free bile acids, which include LCA, DCA, and HDCA, in SV-treated group (Fig. 5). Under normal conditions, bile acids are excreted into bile by bile salt export pump (BSEP) in the canaliculus membrane [56, 57]. However, a basolateral excretion into the blood by multidrug resistance-associated protein (MRP) 3 occurs during cholestasis [58, 59]. After exposure to SV, the BSEP expression decreased, whereas MRP 3 expression significantly increased 3.7-fold (p < 0.05) (Fig. 6). This enhanced basolateral excretion of bile acids coincided with the significantly elevated serum levels of the bile acids, which should be substantially low under normal conditions (Fig. 5). The reabsorption of bile acids into the liver through the portal vein has an important role in bile acid homeostasis. Na+-taurocholate cotransporting proteins (NTCPs), organic anion transporters (OATs), and organic anion-transporting polypeptides (OATPs) are the main transporters responsible for this phenomenon and their deficiencies are observed in rat cholestasis models and patients with cholestasis liver disease [60, 61]. After SV treatment, the NTCP, OAT 3, and OATP 3 expression decreased (Fig. 6), suggesting a dramatically reduced reabsorption of the bile acids, which coincided with the elevated concentrations of the bile acids in the SV-treated rats (Fig. 5).
Hepatic mRNA expression of genes related to bile acid metabolism after exposure to Senecio vulgaris. Hepatic mRNA levels were determined through quantitative RT-PCR, with GAPDH as the internal standard. Relative gene expression was calculated as the ratio of mRNA level in the treated group to that in the control group; this value is expressed as mean ± SEM (n = 3); significant differences between the control group and treated group are based on two-tailed unpaired Student’s t test (* p < 0.05, ** p < 0.01, and *** p < 0.001)
The homeostasis of bile acids was previously proven to have an important function in the SV-induced hepatotoxicity. After SV treatment, the serum profile of the bile acids changed, along with transcriptional factors. The free and conjugated bile acids increased, and the organism showed adaptive modulation of bile acids to prevent bile acid overload by suppressing bile acid during de novo synthesis, thereby limiting bile acid reabsorption and reducing bile acid accumulation in the hepatocytes by basolateral excretion. These findings might also contribute to the survival of experimental animals and patients, which are severely poisoned by PAs and herbs containing PAs [29, 62, 63].
Conclusions
A target profiling approach was developed for the hepatotoxicity assessment of PA-containing herbal medicines by combining the PIS-based characteristic fingerprint analysis of PAs and target profiling of bile acids. In addition, the established methodology was successfully applied in the comparative assessment of two herbal medicines from the same genus, namely, S. vulgaris L. (SV) and S. scandens Buch.-Ham. (SS). Significant differences are found between the two herbal medicines in the chemical markers and biomarkers responsible for their toxicities, which was consistent with conventional toxicity assessment by histopathological examination and clinical serum index assays for experimental animal models. SV contained more PA structures, particularly HPAs. Furthermore, the average contents of the main HPAs in SV were 26-fold higher than in SS. Moreover, the SV treatment induced significant changes in the bile acid profile by the transcriptional regulation of their synthesis, excretion, and uptake. This study definitely revealed the existence of several toxic PAs in SS. However, SS did not show apparent acute toxicity at a single dose level of approximately 30-fold of the officially recommended dose [41], indicating that herbs containing toxic components might also be used with careful assessment and proper dosage for the treatment of diseases. Thus, the toxicity assessment of herbal medicines through a proper approach is important for human health and better utilization of herbal medicines.
References
Lv W, Piao JH, Jiang JG (2012) Expert Opin Drug Saf 11:985–1002
Abdualmjid RJ, Sergi C (2013) J Pharm Pharm Sci 16:376–404
Vanherwegham JL, Depierreux M, Tielemans C, Abramowicz D, Dratwa M, Jadoul M, Richard C, Vandervelde D, Verbeelen D, Vanhaelen-Fastre R (1993) Lancet 341:387–391
Ernst E (2003) Can J Cardiol 19:818–827
Chan TYK, Tam HP, Lai CK, Chan AYW (2005) Ther Drug Monit 27:53–57
Seeff LB (2007) Clin Liver Dis 11:577–596
Jordan SA, Cunningham DG, Marles RJ (2010) Toxicol Appl Pharmacol 243:198–216
Shaw D (2010) Planta Med 76:2012–2018
Efferth T, Kaina B (2011) Curr Drug Metab 12:989–996
Ma B, Li N, Lin G (2012) Curr Drug Metab 13:652–658
Chang WT, Thissen U, Ehlert KA, Koek MM, Jellema RJ, Hankemeier T, Van der Greef J, Wang M (2006) Planta Med 72:458–467
Zhang Y, Li F, Huang F, Xie G, Wei R, Chen T, Liu J, Zhao A, Jia W (2014) J Sep Sci 37:731–737
Roeder E (1995) Pharmazie 50:83–98
Roeder E (2000) Pharmazie 55:711–726
International Programme on Chemical Safety (1988) Pyrrolizidine alkaloids. Environmental health criteria 80.WHO, Geneva
Xiong AZ, Yang L, He YQ, Zhang F, Wang J, Han H, Wang CH, Bligh SWA, Wang ZT (2009) Rapid Commun Mass Spectrom 23:3907–3916
Zhou Y, Li N, Choi FF, Qiao CF, Song JZ, Li SL, Liu X, Cai ZW, Fu PP, Lin G, Xu HX (2010) Anal Chim Acta 681:33–40
Ruan J, Li N, Xia Q, Fu PP, Peng S, Ye Y, Lin G (2012) J Mass Spectrom 47:331–337
Qi M, Xiong AZ, Geng F, Yang L, Wang ZT (2012) J Sep Sci 35:1470–1478
Ji S, Wang Q, Qiao X, Guo HC, Yang YF, Bo T, Xiang C, Guo DA, Ye M (2014) J Pharm Biomed Anal 90:15–26
International Programme on Chemical Safety (1989) Pyrrolizidine alkaloids health and safety guide. Health and safety guide no. 26. WHO, Geneva
Dai N, Yu YC, Ren TH, Wu JG, Jiang Y, Shen LG, Zhang J (2007) World J Gastroenterol 13:1628–1631
Altaee MY, Mahmood MH (1998) East Mediterr Health J 4:142–148
Kakar F, Akbarian Z, Leslie T, Mustafa ML, Watson J, van Egmond HP, Omar MF, Mofleh J (2010) J Toxicol 2010:313280
Bane A, Seboxa T, Mesfin G, Ali A, Tsegaye YW, Tensae MG, Selassie S, Haile T (2012) Eth Med J 50:9–16
Lewis CJ (2001) U.S. Food and Drug Administration Web site. http://www.fda.gov/Food/RecallsOutbreaksEmergencies/SafetyAlertsAdvisories/ucm111219.htm. Accessed 6 July 6 2001
State Pharmacopoeia Commission of the P. R. China (2010) Pharmacopoeia of the People’s Republic of China 2010. China Medicinal Science and Technology Press, Beijing
Lessard P, Wilson WD, Olander HJ, Rogers QR, Mendel VE (1986) Am J Vet Res 47:1776–1780
Mendel VE, Witt MR, Gitchell BS, Gribble DN, Rogers QR, Segall HJ, Knight HD (1988) Am J Vet Res 49:572–578
Sutherland RJ, Deol HS, Hood PJ (1992) Vet Clin Pathol 21:51–56
Yan CC, Huxtable RJ (1995) Toxicol Appl Pharmacol 130:132–139
Xiong AZ, Yang F, Fang LX, Yang L, He YQ, Wan YY, Xu Y, Qi M, Wang XL, Yu K, Tsim KW, Wang ZT (2014) Chem Res Toxicol 27(5):775–786
Chen J, Deng W, Wang J, Shao Y, Ou M, Ding M (2013) Int J Gynaecol Obstet 1:5–8
Lake AD, Novak P, Shipkova P, Aranibar N, Robertson D, Reily MD, Lu Z, Lehman-McKeeman LD, Cherrington NJ (2013) Toxicol Appl Pharmacol 2:132–140
Yang L, Xiong AZ, He YQ, Wang ZY, Wang CH, Wang ZT, Li W, Yang L, Hu ZB (2008) Chem Res Toxicol 21:2280–2288
Yang F, Xu Y, Xiong AZ, He YQ, Yang L, Wan YJY, Wang ZT (2012) J Ethnopharmacol 144:599–604
Ortiz Cansado A, Crespo Valadés E, Morales Blanco P, Sáenz de Santamaría J, González Campillejo JM, Ruiz Téllez T (1995) Gastroenterol Hepatol 18:413–416
Vilar JH, García M, Cabrera P (2000) Gastroenterol Hepatol 23:285–286
Li SL, Lin G, Fu PP, Chan CL, Li M, Jiang ZH, Zhao ZZ (2008) Rapid Commun Mass Spectrom 22:591–602
Zhang F, Wang CH, Wang W, Chen LX, Ma HY, Zhang CF, Zhang M, Bligh SW, Wang ZT (2008) Phytochem Anal 19:25–31
Jones AJ, Culvenor CCJ, Smith LW (1982) Aust J Chem 35(6):1173–1178
Segall HJ, Dallas TL (1983) Phytochemistry 22(5):1271–1273
Zalkow LH, Asibal CF, Glinski JA, Bonetti SJ, Gelbaum LT, VanDerveer D, Powis G (1988) J Nat Prod 51(4):690–702
Witte L, Ernsta L, Wrayb V, Hartmann T (1992) Phytochemistry 31(3):1027–1028
Noorwala M, Mohammad F, Ahmad V, Sener B, Ergun F, Deliorman D (2000) Fitoterapia 71(5):618–620
Xiong AZ, Yang L, Ji LL, Wang ZY, Yang XJ, Chen Y, Wang XL, Wang CH, Wang ZT (2012) Metabolomics 8:614–623
Wiklund S, Johansson E, Sjöström L, Mellerowicz EJ, Edlund U, Shockcor JP, Gottfries J, Moritz T, Trygg J (2008) Anal Chem 80:115–122
Claudel R, Steals B, Kuipers F (2005) Arterioscler, Thromb, Vasc Biol 25:2020–2030
Calkin AC, Tontonoz P (2012) Nat Rev Mol Cell Biol 13:213–224
Nicolaou M, Andress EJ, Zolnerciks JK, Dixon PH, Williamson C, Linton KJ (2012) J Pathol 226:300–315
Wu XP, Chai J, Chen WS (2009) Acad J Sec Mil Med Univ 30:1398–1401
Abu-Hayyeh S, Papacleovoulou G, Lövgren-Sandblom A, Tahir M, Oduwole O, Jamaludin NA, Ravat S, Nikolova V, Chambers J, Selden C, Rees M, Marschall HU, Parker MG, Williamson C (2013) Hepatology 57:716–726
Yang F, Huang X, Yi TS, Yen Y, Moore DD, Huang WD (2007) Cancer Res 67:863–867
Pircher PC, Kitto JL, Petrowski ML, Tangirala RK, Bischoff ED, Schulman IG, Westin SK (2003) J Biol Chem 278(30):27703–27711
Hadžić N, Bull LN, Clayton PT, Knisely AS (2012) World J Gastroenterol 18(25):3322–3326
Stieger B, Fattinger K, Madon J, Kullak-Ublick GA, Meier PJ (2000) Gastroenterology 118:422–430
Cao J, Huang L, Liu Y, Hoffman T, Stieger B, Meier PJ, Vore M (2001) Hepatology 33:140–147
Soroka CJ, Lee JM, Azzaroli F, Boyer JL (2001) Hepatology 33:783–791
Teng S, Piquette-Miller M (2007) Br J Pharmacol 151:367–376
Zollner G, Fickert P, Zenz R, Fuchsbichler A, Stumptner C, Kenner L, Ferenci P, Stauber RE, Krejs GJ, Denk H, Zatloukal K, Trauner M (2004) Hepatology 33:633–646
Geier A, Dietrich CG, Gerloff T, Haendly J, Kullak-Ublick GA, Stieger B, Meier PJ, Matern S, Gartung C (2003) Biochim Biophys Acta 1609:87–94
DeLeve LD, McCuskey RS, Wang X, Hu L, McCuskey MK, Epstein RB, Kanel GC (1999) Hepatology 29:1779–1791
Lin G, Wang JY, Li N, Li M, Gao H, Ji Y, Zhang F, Wang H, Zhou Y, Ye Y, Xu HX, Zheng J (2011) J Hepatol 54:666–673
Acknowledgments
This work was supported by the Program for Changjiang Scholars and Innovative Research Team in University (IRT1071), the National Nature Science Foundation of China (81222053), the Program for New Century Excellent Talents in University (NCET-12-1056), the Shanghai Nature Science Foundation (12ZR1450300), the Rising-Star Scholar Project of Shanghai Municipal Science and Technology Commission (12QH1402200), the Foundation for University Key Teacher of Shanghai Municipal Science and Technology (12CG50), the Foundation for University Young Teachers of Shanghai Municipal Education Commission (ZZSZY12014), the Hong Kong Scholars Program (XJ2012031), and the China Postdoctoral Science Foundation funded project (2012 T50451).
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 171 kb)
Rights and permissions
About this article
Cite this article
Xiong, A., Fang, L., Yang, X. et al. An application of target profiling analyses in the hepatotoxicity assessment of herbal medicines: comparative characteristic fingerprint and bile acid profiling of Senecio vulgaris L. and Senecio scandens Buch.-Ham. Anal Bioanal Chem 406, 7715–7727 (2014). https://doi.org/10.1007/s00216-014-8175-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-014-8175-z