Abstract
We report for the first time the excretion kinetics of the percentage dose of 13C recovered/h (13C-PDR %/h) and cumulative PDR, i.e. c-PDR (%) to accomplish the highest diagnostic accuracy of the 13C-urea breath test (13C-UBT) for the detection of Helicobacter pylori infection without any risk of diagnostic errors using an optical cavity-enhanced integrated cavity output spectroscopy (ICOS) method. An optimal diagnostic cut-off point for the presence of H. pylori infection was determined to be c-PDR (%) = 1.47 % at 60 min, using the receiver operating characteristic curve (ROC) analysis to overcome the “grey zone” containing false-positive and false-negative results of the 13C-UBT. The present 13C-UBT exhibited 100 % diagnostic sensitivity (true-positive rate) and 100 % specificity (true-negative rate) with an accuracy of 100 % compared with invasive endoscopy and biopsy tests. Our c-PDR (%) methodology also manifested both diagnostic positive and negative predictive values of 100 %, demonstrating excellent diagnostic accuracy. We also observed that the effect of endogenous CO2 production related to basal metabolic rates in individuals was statistically insignificant (p = 0.78) on the diagnostic accuracy. However, the presence of H. pylori infection was indicated by the profound effect of urea hydrolysis rate (UHR). Our findings suggest that the current c-PDR (%) is a valid and sufficiently robust novel approach for an accurate, specific, fast and noninvasive diagnosis of H. pylori infection, which could routinely be used for large-scale screening purposes and diagnostic assessment, i.e. for early detection and follow-up of patients.

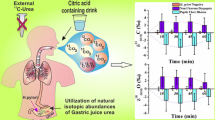
The excretion kinetics of the 13C-urea breath test with an ICOS system is demonstrated for accurate, specific, fast and noninvasive diagnosis of H. pylori infection in the human stomach
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Helicobacter pylori (H. pylori) infection is the primary cause of gastritis and peptic ulcer diseases and has been linked to the onset of various critical diseases such as stomach cancer, gastric lymphoma, and adenocarcinoma [1, 2]. It is estimated that more than half of the world’s populations harbour H. pylori infection, with a prevalence of 80 % or more in the Indian subcontinent [3, 4]. The infection is usually acquired early in life and may remain in the stomach for the rest of the person’s life if it is not properly treated [5, 6]. Most individuals harbouring H. pylori, however, are usually asymptomatic, and hence, they remain undiagnosed. Therefore, an accurate and early detection of H. pylori infection is vital for initiation of proper treatment.
Currently, the 13C-urea breath test (13C-UBT) is considered to be an effective noninvasive method for detecting H. pylori infection by contrast with the direct invasive “gold standard” endoscopy and biopsy-based rapid urease test (RUT) [7, 8]. The 13C-UBT is usually performed by ingestion of a test meal containing 75 mg of 13C-enriched urea with 4 g of citric acid dissolved in 200 mL of water. Initially, a baseline breath (fasting breath) sample is collected, and subsequently, a further breath sample is collected at 30 min following the administration of the substrate. The 13CO2 isotopic enrichments in breath samples are usually measured with a high-precision gas chromatography coupled with an isotope ratio mass spectrometer (GC-IRMS). However, the 13C-UBT exploits the large amount of urease enzyme, secreted by H. pylori in the stomach, to hydrolyse the orally administered 13C-labelled urea into ammonia and 13C-labelled carbon dioxide. The 13C-urea-derived 13CO2 is then transported to the lungs through the bloodstream and is exhaled as 13CO2 in the breath samples. The difference of 13CO2 concentrations before and after ingestion of the labelled urea, which is reported as the delta-over-baseline (DOB) relative to a standard in per mil (‰), i.e. δDOB 13C‰ (δDOB 13C ‰ = (δ13C ‰) t = t min − (δ13C ‰) t = 0 min), will be exploited to detect the presence of H. pylori infection. Therefore, H. pylori-infected individuals will exhibit an increase of 13CO2 in their breath after a certain time following ingestion of 13C-enriched urea. However, to our knowledge, the time-dependent excretion patterns of the 13C-UBT and the percentage dose of 13C recovered per hour, i.e. 13C-PDR (%/h) along with cumulative PDR, i.e. c-PDR (%) in exhaled breath samples have not been investigated in detail. The 13C-PDR describes the rate of 13C-enriched substrate that has been exhaled as 13CO2 in the exhaled breath, whereas the c-PDR (%) accounts for the total amount of 13C-enriched substrate metabolised at any given time. A complete evaluation of the excretion kinetic profiles, 13C-PDR (%/h) and c-PDR (%) of the 13C-UBT is important to understand the real emptying processes, determine the optimal sampling point, elucidate the effects of urea hydrolysis rate (UHR) and accomplish the highest diagnostic accuracy as well as the best diagnostic cut-off level for broad clinical applicability of the 13C-UBT method for large-scale screening purposes.
Moreover, the effect of endogenous CO2 production associated with basal metabolic rates (BMR) may have an influence on the diagnostic accuracy of the 13C-UBT. It is expected that endogenous CO2 production varies along with age (adults > children), weight, height and sex (male > female) [9], and consequently, the DOB values are also expected to vary in accordance with these factors. Yang et al. [5] have recently demonstrated a significant effect of endogenous CO2 production rates on the 13C-UBT even after the application of urea hydrolysis rate (UHR) in children aged between 7 months and 18 years. However, to our knowledge, no investigations of the effect of endogenous CO2 production on 13C-UBT have been performed in adults aged 20–75 years until now.
Furthermore, the determination of a precise cut-off value for discriminating between H. pylori-positive and H. pylori-negative results is still the subject of debate, and subsequently, a wide range of diagnostic cut-off values between 1.3 and 11 ‰ have been suggested in several reports [7, 8]. Sometimes, it is very critical to accurately diagnose if the DOB values are very close to the selected cut-off point or at the borderline, and consequently, the results of 13C-UBT remain questionable and affect the diagnostic accuracy. Some authors have also suggested a narrow spectrum of the DOB values called “grey zone” (2.0 to 5.0 ‰) of the 13C-UBT in which the 13C-UBT results are inconclusive [8]. Therefore, a DOB value within this region should be cautiously interpreted. This grey zone containing unreliable results accounts for intuitive variations of 13CO2 in exhaled breath samples, patient’s metabolism and the limits of the analytical precision of 13CO2 measurements. Therefore, a comprehensive revaluation of the optimal diagnostic cut-off point is required to validate the widespread clinical implementation of the 13C-UBT in the diagnosis of H. pylori infection.
In this article, we first report the time-dependent evaluation of δDOB 13C‰ and 13C-PDR (%/h) along with c-PDR in exhaled breath samples after ingestion of 13C-labelled urea for the detection of H. pylori infection by means of an optical cavity-enhanced integrated cavity output spectroscopy (ICOS) system. We have employed the cavity-enhanced optical spectroscopy method in the present study because of its fast analysis time (about 30 s) compared to the MS-based method (typically 2 min) [10]. We also investigated the influences of endogenous CO2 production and urea hydrolysis rate on the diagnostic accuracy of 13C-UBT. Finally, we determined statistically sound several diagnostic parameters such as the optimal diagnostic cut-off value, sensitivity, specificity, accuracy, the risk of false-positive and false-negative results of the 13C-UBT using the ICOS system against the defined gold-standard endoscopic biopsy tests.
Materials and methods
Subjects
Eighty-three subjects (61 male, 22 female, aged 21–72 years with mean age 38.33 ± 11.69 years) with a variety of gastrointestinal disorders such as chronic gastritis, duodenal and gastric ulcer, and non-ulcer dyspepsia were included in the present study (Electronic Supplementary Material (ESM) Table S1). On the basis of gold-standard reports, such as gastrointestinal endoscopy and biopsy-based rapid urease tests (RUTs), subjects were classified into two different groups, as either H. pylori positive or H. pylori negative. For this purpose, 34 controls negative for H. pylori and 49 patients positive for H. pylori were considered for the 13C-UBTs. Subjects who had taken antibiotics, proton-pump inhibitors or bismuth-containing compound prior to 4 weeks of study and subjects having previous gastric surgery were excluded from the study. The current protocol was approved by the Ethics Committee Review Board of AMRI Hospital, Salt Lake, India (Study No. AMRI/ETHICS/2013/1). Informed consent was obtained from each patient prior to enrolment in the study.
Breath sample collection and 13C-UBT
After an overnight fast, subjects performed the 13C-UBT within 1–2 days after endoscopy according to the standard procedure as previously mentioned in several articles [5, 7, 8, 11]. A baseline breath sample was collected in a 750-mL breath collection bag (QT00892, QuinTron Instrument Co., USA). Subjects were first instructed to ingest 200 mL of citric acid solution (4.0-g citric acid in 200-mL water), and then a drink containing 75-mg 13C-labelled Urea (CLM-311-GMP, Cambridge Isotope Laboratories, Inc., USA) dissolved in 50-mL water was orally administered as per the standard procedure. Post-dose breath samples were collected subsequently at 15-min intervals up to 90 min. During breath sample collection, subjects were instructed to hold their breath for 3 s and blow smoothly through a mouth piece directly into the breath collection bag provided. All breath samples were repeated and analysed by the ICOS system as described in the following section. Figure 1 depicts a diagram presenting the steps of the procedure and analytical protocol used in the study.
Calibration and validation of 13C-UBT by integrated cavity output spectrometer
We have used a high-precision isotopic CO2 integrated cavity output spectrometer (LGR, Los Gatos Research, CA, USA) to measure simultaneously 12C16O16O and 13C16O16O in exhaled breath samples for H. pylori detection. The details of the instrument and the capability of measuring high-precision 13C/12C isotope ratios in CO2 samples have been described elsewhere [12, 13]. In brief, a high-finesse optical cavity (59 cm long) comprised of two high-reflectivity mirrors (R ~ 99.98 %) serves as an absorption measurement cell for breath sample analysis. A temperature-controlled continuous-wave distributed feedback diode laser (cw-DFB) operating at ~2.05 μm was coupled into the optical cavity that provided an effective optical path length of 3 km. The laser frequency of the instrument was repeatedly tuned over 20 GHz to scan over the absorption features of 12C16O16O and 13C16O16O at the wavenumbers of 4,874.448 and 4,874.086 cm−1, respectively, every second. The two absorption features, i.e. R(28) rotational line of the 12C16O16O (2,0°,13) ← (0,0°,0) band and P(16) rotational line of the 13C16O16O (2,0°,12) ← (0,0°,0) band used to determine the 13C/12C isotope ratio, arise from the (2ν1 + ν3) vibrational combination band of the CO2 molecule.
The 13CO2 enrichment in samples is usually expressed by δ13C notation in parts per thousand (or per mil, ‰) where, δ13C‰ = (R sample / R standard − 1) × 1,000, where R sample is the 13C/12C isotope ratio of the sample and R standard is the international standard Pee Dee Belemnite (PDB) value, i.e. 0.0112372. The accuracy and precision of the ICOS instrument for the δ13C‰ measurements of the 13CO2-enriched breath samples were determined by measuring three calibration standards containing 5 % CO2 in air analysed by IRMS (Cambridge Isotope Laboratory, USA). The δ13C values of the calibration standards ranged from baseline level (−22.8 ‰) to high level (−7.33 ‰) including the mid level (−13.22 ‰). The measured δ13C values by ICOS instrument were in excellent quantitative agreement with the values of calibration standards with a precision of ±0.2 ‰ (ESM Table S2). During measurements, a 25 -mL volume of breath sample was injected into the ICOS cell with a syringe/stopcock. High-purity dry nitrogen (HPNG10-1, F-DGSi SAS, France, purity > 99.99 %) was used as the carrier gas for purging the cavity and dilution of breath samples.
Statistical analysis
One-way ANOVA test for parametric variables and the Mann–Whitney test for nonparametric variables were applied to our analysis. A two-sided p value <0.05 was considered statistically significant. A box and whiskers plot was used to illustrate the distribution of δDOB 13C‰ in H. pylori-positive and H. pylori-negative subjects. Finally, a receiver operating characteristic curve (ROC) [14] was generated by plotting the true-positive rate against false-positive rate to determine the optimal diagnostic cut-off value for H. pylori infection. All statistical analysis was performed with Origin Pro 8.0 and Analyse-it Method Evaluation version 2.30 (Analyse-it Software Ltd., UK).
Results and discussion
Figure 2 depicts the typical excretion kinetic patterns of δDOB 13C‰ values in exhaled breath samples for three H. pylori-positive and three H. pylori-negative individuals after ingestion of 13C-enriched substrate. It was observed that in H. pylori-positive patients, the δDOB 13C‰ values in breath samples reached a maximum at around 30 min and then slowly decreased, whereas no significant differences of δDOB 13C‰ values in breath samples were observed for the H. pylori-negative individuals.
It was previously reported by in vitro biopsies analysis that the internal urease activity of H. pylori strongly depends on the medium pH values, and the activity is maximum at a low pH of 3.0 and is minimum at pH 7.0 or 8.0 [15]. When 13C-enriched urea is administered with citric acid, the internal urease activity is stimulated [16] at a pH of <6.5. The activity is increased with acidifications of the medium owing to increased 13C-urea permeability through the urea channel in the inner membrane of H. pylori, allowing a large increase in 13C-urea access to intra-bacterial urease enzyme [15, 17]. It was also shown before that the major effect of acidification of the medium occurs within 30 min [15]. Consequently, an increase in the rate and quantity of δDOB 13C‰ values in exhaled breath within 30 min is most likely to be the result of increased urease activity, i.e. urease-catalysed hydrolysis of 13C-urea increases and thus results in enrichment of 13CO2. The gradual decrease in δDOB 13C‰ values in exhaled breath samples later on is a sign of lower urease activity because of alkalinisation of the bacterial environment by production of NH3. Consequently, the large difference in the δDOB 13C‰ values in breath samples demonstrated a clear distinction between H. pylori-infected and H. pylori-uninfected individuals.
A box and whisker plot of δDOB 13C‰ to illustrate the distribution of 13CO2 enrichment at 30 min in H. pylori-positive and H. pylori-negative individuals is shown in Fig. 3. The mean, median and interquartile ranges (IQRs) (i.e. mid-spread of statistical dispersion) for positive and negative patients were 22.66, 12.64 and 4.32 ‰ to 31.71 ‰, respectively and 1.44, 1.24 and 0.56 ‰ to 2.06 ‰, respectively. It was observed that the median values of δDOB 13C‰ increased significantly for the group with H. pylori-positive individuals compared to that of the group with H. pylori-negative individuals. There was a statistically significant difference between the δDOB 13C‰ values (p < 0.0001) obtained for the two different types of groups, and therefore, they can be distinguished.
Box and whiskers plot of δDOB 13C‰ illustrating the statistical distribution of 13CO2 enrichment at 30 min in H. pylori-positive and H. pylori-negative individuals. The scattered points represented by open circle and open diamond symbols correspond to experimental data points obtained by the ICOS instrument
However, to investigate the diagnostic accuracy of the present 13C-UBT for distinguishing H. pylori-positive and H. pylori-negative individuals, a ROC was constructed by plotting the true-positive rate (sensitivity) against the false-positive rate, i.e. (1-specificity) at 30 min according to the standard procedure as shown in Fig. 4. The sensitivity, specificity and false-positive and false-negative results of 13C-UBT were calculated at various cut-off values (ESM Table S3). An optimal cut-off point for 13C-UBT was defined as the point with the highest sensitivity, specificity and diagnostic accuracy to identify individuals with and without H. pylori infection.
The optimal diagnostic cut-off value was determined to be δDOB 13C‰ (cut-off) = 3.14 ‰, exhibiting 87.8 % sensitivity (95 % confidence interval (CI) 75.2–95.4) and 91.2 % specificity (95 % CI 76.3–98.1) with an accuracy of 89.16 %. The calculated cut-off value as determined by the ROC analysis correlated well with cut-off values of between 2 and 5 ‰ mentioned in the grey zone [7, 8]. The area under the ROC curve referred to as AUC was also determined to be 0.95 (95 % CI 91.0–99.0). At a cut-off value of 3.14 ‰, it was therefore possible to correctly diagnose 43 of 49 patients as positive (i.e. 6 false-negative patients) and 31 of 34 patients as negative (i.e. 3 false-positive patients). It is noted that when the DOB value is close to the cut-off point and the cut-off point is within the grey zone, the risk of a false-positive or false-negative response of the 13C-UBT is extremely high. It should be emphasised here that the grey zone of the 13C-UBT was not hitherto well addressed. The evaluation of the grey zone is very important for the early diagnosis of H. pylori infection because many individuals harbouring the infection fall in this region. In this study, we therefore, have explored a possible way to overcome the grey zone by exploiting the time-dependent evaluation of δDOB 13C‰ values in the exhaled breath samples.
However, there are several possibilities which can affect the results of 13C-UBT within the grey zone. One such possibility is to investigate the effect of endogenous CO2 production associated with basal metabolic rates (BMR) in individuals. To study this effect, we applied the Mifflin–St Jeor equations to calculate the BMR based on age, weight and height of either sex [18]. The effect of the endogenous CO2 production rates between the two groups of H. pylori-positive and H. pylori-negative individuals (10.57 vs 10.66 mmol/min) was statistically insignificant (p = 0.78). However, the effect of urea hydrolysis rate (UHR) at 30 min on 13C-UBT between H. pylori-positive and H. pylori-negative individuals (81.49 vs 5.30 μg/min) was statistically significant (p < 0.0001) which thus showed the presence of H. pylori infection (ESM Fig. S1a, b). To study the UHR, we applied the Schofield equations [19] and used the experimentally determined δDOB 13C‰ values as shown below [5]:
We subsequently investigated the optimal diagnostic cut-off value of 10.48 μg/min by means of UHR at 30 min, but no significant improvement in the results of diagnostic sensitivity, specificity and accuracy was observed (ESM Table S4), demonstrating the insignificant effect of endogenous CO2 production on 13C-UBT.
Figure 5 depicts the excretion patterns of δDOB 13C‰ values within the grey zone for the two groups (20 H. pylori-positive and 17 H. pylori-negative individuals) of patients. It was observed that the δDOB 13C‰ values at each time point for the two groups were very close or sometimes overlap each other, demonstrating that the accurate detection of H. pylori infection in the grey zone is often incorrect and uncertain. We also observed that there were sudden rises or abrupt falls of δDOB 13C‰ values at 30 min in the individual excretion kinetic patterns, which have essentially reflected in the outcomes of 13C-UBT for producing false-positive and false-negative results. The detailed results are shown in the Electronic Supplementary Material (ESM Tables S5, S6 and S7).
Therefore, to avoid the risk of diagnostic errors in the grey zone and consequently to achieve the highest diagnostic accuracy of the 13C-UBT, we have explored the percentage dose of 13C recovered per hour, i.e. 13C-PDR (%/h), and cumulative percentage dose of 13C recovered, i.e. c-PDR (%), in exhaled breath samples for the present 13C-UBT.
To investigate the 13C-PDR, we applied the following formula of Wu and colleagues [20]:
where δDOB 13C is the DOB values, R PDB is equal to 0.0112372, D is the dose of substrate administered, M t is molecular weight of the substrate, p is 13C atom % excess, n is the number of labelled carbon positions and \( {V}_{{\mathrm{CO}}_2} \) is the CO2 production rate per hour. The c-PDR (%) values were calculated using a trapezoidal rule [21] from the 13C-PDR values. Figure 6 shows the time profiles of c-PDR (%) for the two groups of patients within the grey zone. A clear distinction between the groups of H. pylori-positive and H. pylori-negative individuals was observed after 45 min (0.75 h) in the kinetic profiles. Thus, the measurement of c-PDR (%) is more advantageous compared to a single-point δDOB 13C measurement because it accounts for the cumulative effect of δDOB 13C‰ at any given time.
However, a clear disadvantage of the c-PDR (%) methodology compared to the standard single-point δDOB 13C‰ measurement is that at least five to six breath samples need to be measured. In several reports [8], many authors have also suggested that a repeat 13C-UBT or invasive endoscopy and biopsy tests would be an appropriate choice to have a conclusive result for the grey-zone patients. Nevertheless, this is much more expensive and time consuming than a single test regardless of requiring breath samples at multiple time points.
We subsequently explored the diagnostic accuracy of the 13C-UBT by constructing another ROC curve using the c-PDR (%) values, and Fig. 7 depicts the ROC curve. An optimal diagnostic cut-off level was estimated to be c-PDR = 1.47 % at 60 min, exhibiting 100 % diagnostic sensitivity (95 % CI 92.7–100), 100 % specificity (95 % CI 89.7–100) and 100 % accuracy of the 13C-UBT for the detection of H. pylori infection (ESM Tables S8 and S9).
We also investigated whether the current c-PDR (%) methodology is statistically robust compared to the standard one for the grey-zone patients. Figure 8 illustrates a simple statistical test, demonstrating that the optimal cut-off point of the standard δDOB 13C‰ test, i.e. 3.14 ‰ lies within the overlapping areas between the two groups of patients, considering only 1 standard deviation (SD) of the mean values, whereas in the case of c-PDR (%) methodology, the cut-off point (1.47 %) is quite far away from the overlapping areas of both types of patients even by considering 2 SD. It is also noted that the cut-off value of the c-PDR (%) could be decreased to 1.29 % without compromising the sensitivity and specificity of this methodology.
A statistical comparison between single-point δDOB 13C‰ measurement and c-PDR (%) methodology for grey-zone individuals. The error bar corresponds to 1 SD and 2 SD respectively for δDOB 13C‰ and c-PDR (%) measurements. Hp(+) and Hp(−) stand for H. pylori-positive and H. pylori-negative individuals, respectively, and SD is the standard deviation
Thus, the c-PDR (%) methodology appears to be sufficiently robust for an accurate diagnosis of H. pylori infection, avoiding a repeat endoscopic biopsy test, as some authors have previously suggested this invasive test [8] when the DOB values are inconclusive within the grey zone. Moreover, we determined the positive and negative predictive values (i.e. PPV and NPV) of the present 13C-UBT. The PPV and NPV essentially indicate the probabilities that the infection is truly positive and negative, respectively, among the total test outcome positives and test outcome negatives, respectively [22]. The present 13C-UBT demonstrated both PPV and NPV of 100 %, manifesting excellent diagnostic accuracy for large-scale screening purposes. Table 1 shows the comparison of various diagnostic parameters for 13C-UBT in three different methodologies.
Finally, we have investigated the real emptying process of the present 13C-UBT for H. pylori-infected individuals. Figure 9 illustrates the time profiles of 13C-PDR (%/h) and c-PDR (%) of H. pylori-infected individuals. The median data for the 13C-PDR (%/h) of 49 H. pylori-positive patients were fitted by the following mathematical formula for the determination of the time of maximal emptying rate [15]:
Time profiles of percentage dose of 13C recovered per hour, 13C-PDR (%/h) and cumulative percentage dose of 13C recovered, c-PDR (%). Median values of 49 H. pylori-positive patients are used to plot. Red lines are the fitted curves. t max and t 1/2 indicate the time of maximal emptying rate and half emptying time, respectively
where y is the percentage of 13CO2 excretion per hour, t is the time, and a, b and c are constants. From the fitting constants, the time of maximal emptying rate of the current 13C-UBT was calculated to be t max = (b/c) = 0.60 h (36 min) as shown in Fig. 9.
The calculated value also supported the maximum δDOB 13C‰ values at 30 min as previously observed in Fig. 2 for H. pylori-positive patients. The c-PDR (%) data were also fitted to another three-parameter model with
where m, k and β are constants to determine the half emptying time [15] of the current protocol, and it was estimated to be t 1/2 = (−1/k)ln(1 − 2− 1/β) = 0.75 h(45 min). From Fig. 9, it was also observed that about 8 % of the total 13C dose recovered over 1.5 h which in turn exhibited the existence of H. pylori infection.
Conclusion
We have demonstrated for the first time the excretion kinetic patterns of δDOB 13C‰, 13C-PDR (%/h) as well as c-PDR (%) for the 13C-UBT in the diagnosis of H. pylori infection. We subsequently investigated the effect of endogenous CO2 production and urea hydrolysis rates on the excretion kinetic curves. The present study clearly demonstrates how to overcome the grey zone in the 13C-UBT for the accurate determination of the infection without any risk of diagnostic errors and consequently introduces a new diagnostic cut-off value of c-PDR (%) = 1.47 % at 60 min. Moreover, the current c-PDR methodology exhibited both sensitivity (true-positive rates) and specificity (true-negative rates) of 100 % and a diagnostic accuracy of 100 % compared with endoscopic biopsy tests, thus making it a sufficiently robust and novel method for an accurate and fast noninvasive diagnosis of H. pylori infection for large-scale screening purposes. However, it should be emphasised that we have investigated the c-PDR (%) methodology only on limited number of samples as a preliminary test, and a much larger study would be required to confirm the general rule that c-PDR (%) = 1.47 % at 60 min is always the best choices.
References
Imrie C, Rowland M, Bourke B, Drumm B (2001) Is Helicobacter pylori infection in childhood a risk factor for gastric cancer? Pediatrics 107:373–380
Suzuki H, Marshall BJ, Hibi T (2006) Overview: Helicobacter pylori and extragastric disease. Int J Hematol 84:291–300
Crowe SE (2005) Helicobacter infection, chronic inflammation and the development of malignancy. Curr Opin Gastroenterol 21:32–38
Thirumurthi S, Graham DY (2012) Helicobacter pylori infection in India from a western perspective. Indian J Med Res 136:549–562
Yang HR, Ko JS, Seo JK (2008) Does the diagnostic accuracy of the 13C-urea breath test vary with age even after the application of urea hydrolysis rate? Helicobacter 13:239–244
Perry S, Parsonnet J (2005) Commentry: H. pylori infection in early and the problem of imperfect tests. Int J Epidemiol 34:1356–1358
Goddard AF, Logan RPH (1997) Review article: urea breath tests for detecting Helicobacter pylori. Aliment Pharmacol Ther 11:641–649
Gisbert JP, Pajares JM (2004) Review article: 13C-urea breath test in the diagnosis of Helicobacter pylori infection—a critical review. Aliment Pharmacol Ther 20:1001–1017
Klein PD, Malaty HM, Czinn SJ, Emmons SJ, Martin RF, Graham DY (1999) Normalizing results of 13C-Urea breath testing for CO2 production rates in children. J Pediatr Gastroenterol Nutr 29:297–301
Savarino V, Vigneri S, Celle G (1999) The 13C urea breath test in the diagnosis of Helicobacter pylori infection. Gut 45(Suppl I):18–I22
Dominguez-Munoz JE, Leodolter A, Sauerbruch T, Malfertheiner P (1997) A citric acid solution is an optimal test drink in the 13C-urea breath test for the diagnosis of Helicobacter pylori infection. Gut 40:459–462
McAlexander I, Rau GH, Liem J, Owano T, Fellers R, Bear D, Gupta M (2011) Deployment of a carbon isotope ratiometer for the monitoring of CO2 sequestration leakage. Anal Chem 83:6223–6229
Creedon CT, Verhulst PJ, Choi KM, Mason JE, Linden DR, Szurszewski JH, Gibbons SJ, Farrugia G (2013) Assessment of gastric emptying in non-obese diabetic mice using a [13C]-octanoic acid breath test. J Vis Exp 73:e50301
Grzybowski M, Younger JG (1997) Statistical methodology: III. Receiver operating characteristic (ROC) curves. Acad Emerg Med 4:818–826
Pantoflickova D, Scott DR, Sachs G, Dorta G, Blum AL (2003) 13C urea breath test (UBT) in the diagnosis of Helicobacter pylori; why does it work better with acid test meals? Gut 52:933–937
Scott DR, Weeks D, Hong C, Postitus S, Melchers K, Sachs G (1998) The role of internal urease in acid resistance of Helicobacter pylori. Gastroenterology 114:58–70
Rektorschek M, Weeks D, Sachs G, Melchers K (1998) Influence of pH on metabolism and urease activity of Helicobacter pylori. Gastroenterology 115:628–641
Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO (1990) A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr 51:241–247
Schofield WN (1985) Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 39:S5–S41
Wu IC, Ohsawa I, Fuku N, Tanaka M (2010) Metabolic analysis of 13C-labeled pyruvate for noninvasive assessment of mitochondrial function. Ann N Y Acad Sci 1201:111–120
Evenepoel P, Hiele M, Geypens B, Geboes KP, Rutgeerts P, Ghoos Y (2000) 13C-egg white breath test: a non-invasive test of pancreatic trypsin activity in the small intestine. Gut 46:52–57
Akobeng AK (2006) Understanding diagnostic tests 1: sensitivity, specificity and predictive values. Acta Paediatr 96:338–341
Acknowledgments
This work was supported by the S.N. Bose National Centre for Basic Sciences (Grant No. SNB/MP/11-12/69). The authors further acknowledge the financial support from Thematic Unit (Ref. No. DST-SR/NM/NS-09/2011). The Department of Science & Technology (DST, India) Inspire Fellowships (A. Maity and G.D. Banik) and JRF studentships from S.N. Bose Centre (S. Som and C. Ghosh) are gratefully acknowledged. M. Pradhan thanks the Department of Biotechnology (DBT, India) for the award of Rapid Grant for Young Investigators (RGYI) which was helpful at the initial stage of the breath analysis research work. The authors also thank Prof. A. K. Raychaudhuri and Dr. G. Gangopadhyay for useful discussions. We are also grateful to all volunteers who willingly participated in the present study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Suman Som and Abhijit Maity contributed equally to this work and are considered as joint first authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 3117 kb)
Rights and permissions
About this article
Cite this article
Som, S., Maity, A., Banik, G.D. et al. Excretion kinetics of 13C-urea breath test: influences of endogenous CO2 production and dose recovery on the diagnostic accuracy of Helicobacter pylori infection. Anal Bioanal Chem 406, 5405–5412 (2014). https://doi.org/10.1007/s00216-014-7951-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-014-7951-0