Abstract
The 13C-urea breath test (13C-UBT), developed a few decades ago, is widely used as a non-invasive diagnostic method to detect only the presence of the gastric pathogen Helicobacter pylori infection; however, the actual disease state, i.e. whether the person harbouring H. pylori has peptic ulcer disease (PUD) or non-ulcerous dyspepsia (NUD), is still poorly understood. Nevertheless, the present 13C-UBT has numerous limitations, drawbacks and pitfalls owing to the ingestion of 13C-labelled external urea. Here, we show that H. pylori is able to utilize the natural 13C and 18O-urea inherently present in the gastric juice in humans for its urease activity which has never been explored before. In vitro measurements of isotopic fractionations of gastric juice urea provide new insights into the actual state of the infection of PUD or NUD. We also provide evidence of the unusual 13C and 18O-isotopic fractionations of breath CO2 that are distinctively altered in individuals with PUD encompassing both gastric and duodenal ulcers as well as with NUD by the enzymatic activity of H. pylori in the gastric niche without oral administration of any 13C-enriched external urea. This deepens our understanding of the UBT exploiting the natural 13C and 18O-gastric juice urea in the pathogenesis of H. pylori infection, reveals the actual disease state of PUD or NUD and thus offers novel opportunities for a simple, robust, cost-effective and non-toxic global strategy devoid of any 13C-enriched urea for treating these common diseases by a single breath test.

Urea breath test without any external urea
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Helicobacter pylori, one of the most common gastric pathogens in the human stomach, is strongly associated with chronic gastritis and peptic ulcer disease [1–6]. This microorganism has high urease activity which enables it to hydrolyse gastric juice urea with the production of CO2 and NH3, thus elevating the pH to neutral as required for the survival of the pathogen in a highly acidic environment [7, 8]. However, despite the vital role of urease enzyme in H. pylori pathogenesis, the relationship between non-ulcerous dyspepsia, peptic ulcer (encompassing both gastric and duodenal ulcers) and H. pylori infection still remains poorly understood.
Over the last few decades, the 13C-urea breath test (13C-UBT) based on the urease activity of the organism has widely been used as a non-invasive diagnostic method to detect exclusively the presence of H. pylori infection in the stomach [9, 10]. But thus far the current 13C-UBT has not allowed one to accurately assess the actual disease state i.e. whether the person harbouring H. pylori infection has peptic ulcer or non-ulcerous dyspepsia. One salient disadvantage of the 13C-UBT is the influence of urease-positive non-H. pylori bacteria in the oral cavity on the results of 13C-UBT [11–13]. Numerous false positive results are thus still observed in the present 13C-UBT because of the consumption of orally administered 13C-enriched urea. Moreover, there are several other drawbacks and pitfalls in the existing 13C-UBT. For example, the optimal diagnostic cut-off point discriminating positive and negative 13C-UBT results is still a controversial issue [10]. The results of 13C-UBT remain questionable and affect the diagnostic accuracy when the cut-off values are very close to the borderline at the onset of the infection or when the cut-off level lies in the so-called grey zone [10]. Therefore there is a pressing need to explore a new-generation strategy which can circumvent all these issues in the existing 13C-UBT and consequently make the diagnosis more sensitive, precise and disease specific.
Studies in the past decade have also demonstrated that 16O in 12C16O2 and 18O of H2 18O are rapidly exchanged in the gastric juice catalysed by the metalloenzyme carbonic anhydrase (CA) of H. pylori to maintain the urease activity in its environment [14–16]. But the potential role of 18O-isotopic fractionations in the gastric environment influenced by the enzymatic activity of H. pylori especially in the pathogenesis of peptic ulcer or non-ulcerous dyspepsia has not yet been fully explored.
Several lines of evidence [17, 18] also suggest that gastric juice contains urea in the range of 3–5 mM but its potential link to the infection remains controversial. Moreover, the natural isotopic abundances of 13C-urea [13C16O(NH2)2] as well as 18O-urea [12C18O(NH2)2] in the gastric juice of positive and negative H. pylori-infected persons are also largely unknown. It therefore suggests a tantalizing hypothesis that utilization of natural isotopic urea in the gastric juice by the H. pylori and subsequently monitoring of 18O and 13C of breath CO2 levels in response to the enzymatic activity may distinctively track the pathogenesis of peptic ulcer, non-ulcerous dyspepsia and H. pylori infection. Hence this may afford a new-generation and cost-effective UBT strategy without any orally administered 13C-labelled external urea for treating the risk of developing ulcer or ulcer-related complications associated with H. pylori infection. But until now there has been no study to support such a hypothesis. Moreover, without oral ingestion of any 13C-labelled urea, how the accurate diagnosis of H. pylori infection along with the actual disease state (i.e. peptic ulcer or non-ulcerous dyspepsia) might be possible has never been explored before. The reason for the missing information is mainly due to the lack of knowledge of the actual isotopic abundances of the 18O and 13C-urea in human gastric juice. New insight into the role of natural 13C and 18O-isotopic urea in gastric juice is therefore essential to elucidate the pathophysiology of H. pylori infection and to distinctively track the pathogenesis of peptic ulcer or functional dyspepsia.
In this study, we first report the natural isotopic abundances of 18O and 13C-urea in the gastric juice of H. pylori positive and negative patients together with the potential links between both 18O and 13C isotopes of breath CO2 and the gastric pathogen H. pylori. We subsequently assessed the clinical validity and robustness of the new UBT without ingestion of any external isotopic urea in response to the standard eradication therapies of the infection and finally also determined several novel diagnostic parameters such as diagnostic cut-off values, sensitivity, specificity of 18O and 13C of breath CO2 to gain a better insight into the diagnostic efficacy for the non-invasive assessment of peptic ulcer, non-ulcerous dyspepsia and H. pylori.
Materials and methods
Subjects
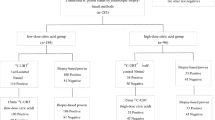
In this study, 145 individuals (83 male, 62 female; age 18–67 years), with different gastrointestinal disorders like gastritis, non-ulcer dyspepsia, and peptic ulcer, were enrolled after the initial screening. We categorized the enrolled individuals into the three distinct groups: non-ulcer dyspepsia (H. pylori positive, n = 53), peptic ulcer (H. pylori positive, n = 57) and H. pylori negative (n = 35) based on the reports of both invasive and non-invasive “gold-standard” tests i.e. endoscopy, biopsy-based rapid urease (RUT) and 13C-urea breath test (13C-UBT), respectively. For all the enrolled individuals, there was no contradiction between the test reports of H. pylori infection of both tests. In 13C-UBT, individuals with the value of δDOB 13C (‰) ≥ 3 ‰ at 30 min were considered to be H. pylori positive [9, 10, 19]. Patients receiving antibiotics, proton pump inhibitors or H2 receptor antagonists 4 weeks prior to the study were excluded at the initial screening. The Ethics Committee Review Board of AMRI Hospital, Salt Lake, Kolkata, India, approved the protocol of the current study (Study no.: AMRI/ETHICS/2013/1). The administration of S. N. Bose Centre, Kolkata, India, also approved the current study (Ref. no.: SNB/PER-2-6001/13-14/1769). All the patients gave their written consent prior to the study.
Collection of gastric juice
During the endoscopic examinations, ca. 10 mL of gastric juice from each enrolled subject was aspirated through the suction channel of the endoscope and collected in a mucus extractor inserted in the suction line. The gastric juice samples were then stored under −20 °C to maintain protein stability until analysis. Before analysis, the gastric juice samples were centrifuged at 10,000 rpm for 10 min to further remove the mucus and subsequently the filtrate parts were used for the Fourier transform infrared (FTIR) spectroscopy and integrated cavity output spectroscopy (ICOS) studies.
Preparations of chemical solutions
The protein, jack bean urease (Sigma Aldrich; EC 3.5.1.5), was purchased from Sigma Aldrich with the highest available purity. The 13C-enriched urea was acquired from Cambridge Isotope Laboratory (CLM-311-GMP, Cambridge Isotopic Laboratories, Inc., USA) whereas all the other chemicals were procured from Sigma Aldrich. All the chemicals were used without further purification. Milli-Q water was used to prepare the salt solutions. The aqueous solution (0.01 nM) of urease was prepared in citrate buffer (10 mM) at pH 7.0. The wide functionality range of citrate buffer was exploited to deal with the different pH (1–7.6) of the gastric juice samples. The standard solutions (5 mM) of both 12C and 13C-enriched urea were prepared in the same citrate buffer at pH 7.0. The pH measurements of different samples were made utilizing a standard pH meter (ecphtutor-ds).
FTIR study
FTIR spectroscopic measurements were carried out in a JASCO FTIR-6300 spectrophotometer using CaF2 windows and a spacer thickness of 100 μm/200 μm in the mid-infrared region (1400–1500 cm−1). For each measurement, 50 scans were acquired at 2 cm−1 resolution. All the spectra were collected taking the buffer solution as a background reference.
Isotopic determination of gastric juice urea
A portion of the filtrate gastric juice was equally divided into two closed round-bottom flasks filled with an inert atmosphere (N2). The jack bean urease solution (0.01 nM) was then added into the gastric juice of one of the flasks, and the other flask contained only the gastric juice sample. After 10 min, an adequate amount of H3PO4 acid was injected into both flasks to remove the dissolved CO2 from the sample to its headspace. The headspace CO2 was thereafter collected from the individual flasks and analysed separately for the measurements of isotopic mole fractions of CO2 using an isotope-sensitive high-precision off-axis ICOS as described in the following section. The actual isotopic mole fractions of CO2, generated from the in vitro chemical hydrolysis of gastric juice urea in response to the external jack bean urease, were calculated after subtracting the CO2 mole fractions of the other flask that originated from the bicarbonate which was initially present in the gastric juice sample. This eliminated the contributions from bicarbonates, and the isotopic mole fractions of CO2 were utilized for the measurements of isotopic abundances of gastric juice urea. It is noteworthy that an adequate amount of NaOH solution was additionally mixed with the gastric juice samples of pH 1–3 to increase the pH to 7 before the addition of external urease and as a result the functionality of the urease remained intact in the gastric juice samples.
Integrated cavity output spectroscopy (ICOS)
A CO2 isotope analyser (CCIA 36-EP, LGR, USA) exploiting off-axis ICOS was utilized for extremely precise measurements of 12CO2, 13CO2 and 12C16O18O isotopes of CO2 in a gas sample. The details of the ICOS system and its capability for high precision isotope measurements were described elsewhere [19–21]. Here we briefly described its salient features. It consists of a high finesse optical cavity comprising two high reflectivity mirrors (R ~ 99.98 %) yielding an optical path length of ca. 3 km. A laser operating at ca. 2.05 μm scans over a range of 20 GHz and records the absorption spectra of 12C16O16O, 13C16O16O and 12C18O16O at the wavenumbers of 4874.448 cm−1, 4874.086 cm−1 and 4874.178 cm−1, respectively. The aforementioned wavenumbers correspond to R(28), P(16) and P(36) ro-vibrational lines in the (2,00,1)←(0,00,0) vibrational combination band of the CO2 molecule. The isotopic ratios were expressed in the typical δ13C ‰ and δ18O ‰ notation relative to the standard Vienna Pee Dee Belemnite (PDB) values of (13C/12C)Standard = 0.0112372 and (18O/16O)Standard = 0.0020672 as described by Eqs. (1) and (2), respectively:
The accuracy and precision of the CO2 spectrometer were determined by utilizing three calibration standards from CIL (Cambridge Isotope Laboratory, USA) with known δ13C values (−22.71 ‰, −15.5 ‰ and −9.69 ‰) and a standard NOAA air tank with known δ18O value (−1 ‰) (Electronic Supplementary Material (ESM) Tables S1 and S2).
Breath sample collection
The patients enrolled in the study underwent 13C-UBT within 1–2 days of the endoscopic examination. Prior to the breath test, every patient was instructed to wash his mouth repeatedly to avoid any kind of contamination arising from the oral cavity bacteria. In 13C-UBT, after an overnight fasting (10–12 h) a baseline breath sample was collected in a breath bag (QUINTRON, USA, SL No.QT00892) 10 min after administration of 4 g citric acid dissolved in 200 mL of water. The test meal consisting of 75 mg 13C-labeled urea (CLM-311-GMP, Cambridge Isotopic Laboratories, Inc., USA) in 50 mL of water was then administered and subsequently breath samples were taken at 15-min intervals for a period of 1 h. The design of the breath collection bags was such that the oral breath was first passed through a dead space and then the end tidal breath was captured in the 750-mL reservoir bags utilizing a one-way valve. In this study, we collected an empty stomach breath sample additionally prior to the 13C-UBT.
The next day, to exploit the natural isotopic urea present in the gastric juice, an empty stomach breath was taken after the overnight fasting (10–12 h) and 4 g citric acid dissolved in 200 mL of water was then administered. Consequently, breath samples were collected at 15-min intervals for 1 h. The isotope ratios of 13C/12C and 18O/16O in the exhaled breath samples were analysed using the ICOS technique as mentioned before.
Statistical analysis
To analyse the results, one-way ANOVA test was used for the normally distributed data whereas Mann–Whitney test and Kruskal–Wallis test were utilized for non-normally distributed data. A two-sided p value less than 0.05 was considered to be statistically significant. All data are presented as mean ± standard deviation (SD) except in Figs. 2a, b and 4c, d where mean ± standard error (SEM) are plotted. The receiver operating characteristics curve (ROC), drawn by plotting the sensitivity against (1 − specificity), was utilized to demonstrate different diagnostic cut-off values. The optimal diagnostic cut-off value represents the maximum sensitivity and specificity. All the statistical analyses were performed using Origin Pro 8.0 and Analyse-it method evaluation software (Analyse-it software Ltd, UK, version 2.30).
Results and discussion
To investigate the natural isotopic abundances of 12C and 13C-urea present in human gastric juice, we first studied the in vitro chemical reactions of human gastric juice in response to an external jack bean urease enzyme (Sigma Aldrich; EC 3.5.1.5) using FTIR spectroscopy. In the FTIR analyses, CN stretching vibrational frequencies at 1465 cm−1 and 1434 cm−1 [22, 23] were assigned to qualitatively examine the presence of 12C and 13C-urea, respectively, in the human gastric juice samples. The selected vibrational frequencies were also confirmed by utilizing the solutions of 12C and 13C-enriched pure urea substrates (ESM Fig. S1). In this in vitro investigation (Fig. 1a, b), we observed a significant decrease in peak intensity at different time intervals, demonstrating the possible chemical hydrolysis of urea present in gastric juice catalysed by external jack bean urease and thereby confirming the existence of the different isotopes of urea in the human gastric juice in a qualitative way.
FTIR study of gastric juice urea: a, b show reduction in peak intensity of urea with time in response to the external jack bean urease enzyme for 12C and 13C isotopes, respectively, exploiting C–N stretching vibrational frequencies. The decrease in peak intensity likely indicates the manifestation of the urea hydrolysis reaction. Larger volume of gastric juice has been exploited for 13C isotope to achieve the reasonable peak intensity
To evaluate the precise abundances of individual isotopes, i.e. 12C, 13C and 18O, of urea along with the total amount of urea present in the gastric juice, we analysed the gastric juice of positive and negative H. pylori-infected individuals by an isotope-selective high-resolution optical ICOS technique. In this unique approach, headspace CO2, generated from the chemical breakdown of urea present in human gastric juice in response to the external jack bean urease, was exploited for the isotope specific measurements of gastric juice urea. In this study (Fig. 2a), we found statistically insignificant difference (p > 0.05) of total gastric juice urea between H. pylori positive (1.78 ± 0.3(SE) mM) and negative (2.68 ± 0.44(SE) mM) individuals. But, interestingly, a statistically significant difference (p < 0.01) of total gastric juice urea was observed between the subgroups of H. pylori positive individuals, i.e. between NUD (2.17 ± 0.37(SE) mM) and PUD (0.65 ± 0.20(SE) mM), whereas NUD was found to be statistically insignificant (p > 0.05) from H. pylori negative individuals (Fig. 2b). This result signifies that higher urease activity of PUD individuals eventually lowered the total gastric juice urea on average. Our study also sheds light on the contradictory results of previous reports [17, 18] in which specific disease states of the H. pylori infection had not been studied properly. However, the isotopic analyses (Fig. 2c, d) showed that there was statistically insignificant difference (p > 0.05) of isotopic abundances (%) between H. pylori positive and negative individuals irrespective of the isotopic nature of the gastric juice urea. Nevertheless, the main conclusive outcome of the isotopic analyses was that the abundances of the individual isotopes, i.e. 12C (~98.4 %), 13C (~1.11 %) and 18O (~0.45 %), of gastric juice urea were found to be sufficiently high enough to be utilized for non-invasive detection of H. pylori infection in conjunction with its urease activity.
Urea concentration and isotopic fractionations in gastric juice of NUD, PUD and H. pylori negative patients. a Total urea concentration in gastric juice of H. pylori positive and negative individuals. p > 0.05 indicates statistically insignificant difference between both the groups. b Total urea concentration in gastric juice of PUD can be statistically differentiated from NUD and H. pylori negative patients. c, d 12C, 13C and 18O isotopic fractionations ( %) of total urea content in gastric juice of PUD, NUD and H. pylori negative individuals. The abundances of 13C and 18O isotopes in gastric juice are comparable to those of the enriched international standard Pee Dee Belemnite (PDB)
To investigate how the 13C and 18O-isotopic fractionations of breath CO2 changes without ingestion of any external 13C-enriched urea but exploitation of natural isotopic urea present in the gastric juice by H. pylori, we studied the time-dependent excretion dynamics of both the isotopes in exhaled breath following ingestion of a citric acid-containing test meal for H. pylori negative (n = 35) and positive (n = 110) individuals with different gastrointestinal disorders such as peptic ulcers (n = 57) and non-ulcerous dyspepsia (n = 53). We monitored simultaneously 13C16O2/12C16O2 and 12C18O16O/12C16O16O isotope ratios in exhaled breath samples associated with the enzymatic activities of urease in the citric acid-mediated bacterial environment using a laser-based high-resolution ICOS technique. The isotopic fractionations in breath were expressed as usual by the delta-over-baseline (DOB) with respect to the VPDB standard, i.e. δDOB 13C‰ = [(δ13C‰) t = t − (δ13C‰) t = basal] and δDOB 18O‰ = [(δ18O‰) t = t − (δ18O‰) t = basal]. In this investigation (Fig. 3a, b), H. pylori positive subjects exhibited two notably distinct excretion kinetic profiles of both 18O and 13C in breath CO2 depending on the state of the infection i.e. NUD and PUD during the 1-h breath excretion studies, while no significant enrichments of both the isotopic species were manifested for H. pylori negative individuals.
Alterations in δDOB values for 13C and 18O in exhaled breath due to utilization of gastric juice urea by H. pylori in response to citric acid. a Change in δDOB 13C (‰) values in exhaled breath for NUD, PUD and H. pylori negative individuals. A significant enrichment and depletion is observed for NUD and PUD, respectively, while no significant change is observed for H. pylori negative patients. b Change in δDOB 18O (‰) values in exhaled breath for NUD, PUD and H. pylori negative individuals follows a similar trend as for δDOB 13C(‰) values. c, d Statistical comparisons of δDOB 13C(‰) and δDOB 18O (‰) values between the H. pylori positive and the H. pylori negative individuals. Cut-off ranges for the distinct diagnosis of H. pylori infection are demonstrated both for δDOB 13C (‰) and δDOB 18O (‰) values
We observed a statistically significant differences of δDOB 18O‰ and δDOB 13C‰ values (p < 0.001) among the two subgroups i.e. NUD and PUD of H. pylori-infected positive individuals (Fig. 3c, d). In case of NUD patients, the higher amount of gastric juice urea as we experimentally observed (see Fig. 2b) in response to the urease enzyme secreted by H. pylori was possibly attributed to the isotopic enrichments of both δDOB 13C‰ and δDOB 18O‰ values, whereas for PUD patients a much lower amount of gastric juice urea was supposed to be responsible for the depletion of δDOB 13C‰ and δDOB 18O‰ values. In view of these results, cut-off ranges of −0.95 ‰ ≥ δDOB 13C ≥ 1.04 ‰ and −0.96 ‰ ≥ δDOB 18O ≥ 1.01 ‰ were calculated with 100 % sensitivity and specificity to diagnose the presence of H. pylori infection in this new UBT methodology. Taken together, these findings suggest that H. pylori has the ability to utilize the natural 13C and 18O-urea in the gastric juice and consequently the precise distinction between H. pylori infected and non-infected individuals is possible by monitoring 13C and 18O of breath CO2; this reveals a missing link between H. pylori infection and 13C and 18O-istopic exchange in exhaled breath without oral administration of 13C-labelled urea and hence may open a new UBT strategy to diagnose H. pylori infection. We have also confirmed the earlier hypothesis that the urease-catalysed hydrolysis of natural 13C-urea and 18O-urea in the gastric juice is strongly associated with the alteration of 13C16O2 and C18O16O in breath samples.
On the basis of the two distinct excretion dynamics profiles of both δDOB 13C‰ and δDOB 18O‰ in individuals with H. pylori infection (Fig. 3a, b), we next explored whether the new UBT without the utilization of any external 13C-labelled urea has sufficient efficacy to selectively track the actual disease state i.e. whether the subject has PUD or NUD associated with the H. pylori infection. We used ROC analysis to determine the optimal diagnostic cut-off values of δDOB 13C‰ and δDOB 18O‰ of the new UBT to selectively track the PUD and NUD. In the new UBT not including any 13C-labelled urea, individuals with δDOB 13C‰ ≥ 1.04 and δDOB 18O‰ ≥ 1.01 were considered to be NUD and these afforded a diagnostic sensitivity and specificity of 100 % (Fig. 4a, b). In contrast, δDOB 13C‰ ≤ −0.95 and δDOB 18O‰ ≤ −0.96 indicated PUD with ca. 96 % sensitivity and 100 % specificity and two false negative outcomes (Fig. 4a, b). We then critically assessed the false negative results and found significant enhancements (>1.5 ‰) of both δDOB 13C‰ and δDOB 18O‰ values in the exhaled breath as a direct consequence of high urea concentrations in the gastric juices of these PUD individuals (ESM Fig. S2). Furthermore, the detailed characteristic study of the specific state of the infection revealed that these individuals were suffering from peptic ulcer bleeding. We therefore speculate that blood urea may play a vital role in the enhancement of urea concentration in the gastric juice of these two PUD individuals. We further assessed clinical validity and widespread efficacy of the new UBT for eradication purposes. Figure 4c, d demonstrate the clinical feasibility of the new UBT to monitor the response to the standard antibiotic therapies and thus provide a new-generation methodology for the early detection and follow-up of patients after eradication of H. pylori infection. In view of these results, our findings point to new perspectives into the pathogenesis of the disease and the potential mechanisms linking breath 13C and 18O-isotopes to ulcer and non-ulcerous dyspepsia.
Receiver operating characteristics (ROC) curve for determining diagnostic cut-off values. Viability of the new UBT before and after the eradication of the disease. a, b ROC analysis for the determination of cut-off values for the specific discrimination of PUD, NUD and H. pylori negative patients for δDOB 13C(‰) and δDOB 18O(‰), respectively. NUD patients could be well distinguished with 100 % sensitivity and specificity while PUD showed ca. 96 % sensitivity and 100 % specificity. c, d Comparison of the values of δDOB 13C(‰) and δDOB 18O(‰) before and after the eradication therapy depicting the absence of the infection after the therapy with no significant difference to the H. pylori negative group
Finally, we addressed the missing link of the grey-zone problem in standard 13C-UBT and the efficacy of the new UBT not including any 13C-labelled urea to overcome this problem. After incorporating the empty stomach breath sample into the standard 13C-UBT protocol where 13C-enriched urea was administered 10 min after ingestion of citric acid, we observed (Fig. 5) a significant enrichment of δDOB 13C‰ value for NUD within the 10 min of acidification of the bacterial environment through the administration of citric acid and thereby indicating that H. pylori already started to utilize the gastric juice urea to alkalize the medium. Now, administration of 13C-labelled urea thereafter may eventually show less enrichment of δDOB 13C‰ value for the on-set of the infection and thus give an inconclusive result or grey-zone problem. Therefore, the new UBT, exploiting only gastric juice urea, provides great promise for a better, more robust and non-toxic global methodology compared with the existing 13C-UBT for precise detection of the H. pylori infection. Moreover, several earlier pieces of evidence [11–13] demonstrated that numerous urease-containing microorganisms other than H. pylori are present in the human oral cavity possessing strong urease activity. Therefore the observations of the false positive results of the existing 13C-UBT are likely to be the effects of the urease activity by the urease-positive non-H. pylori bacteria in response to the orally administered 13C-enriched external urea.
Effect of gastric juice urea in the standard 13C-UBT protocol. The figure shows the increment in the δDOB 13C(‰) value for NUD within 10 min of ingestion of citric acid where the endogenous urea in gastric juice is utilized by the H. pylori and therefore causes the grey-zone problem for the onset of the infection. 0 min denotes the empty stomach breath sample i.e. before the ingestion of citric acid. The entire excretion dynamics of 13C-UBT is divided into two regions with region I demonstrating the effect of citric acid and region II illustrating the effect of 13C-labelled urea, whereas the grey region (III) indicates the grey zone of 13C-UBT
Conclusion
Our findings suggest that devoid of any external 13C-enchried urea, the new UBT strategy exploiting the natural 18O and 13C-urea in human gastric juice selectively reveals the specific disease state (i.e. whether it is a peptic ulcer or non-ulcer) and allows the correct diagnosis of the H. pylori infection with unprecedented diagnostic sensitivity and specificity. Consequently, our new UBT overcomes all the existing issues that the existing 13C-UBT often fails to do. Nonetheless, the direct exploitation of gastric juice urea in the new UBT methodology should enhance our ability to devise new and better approaches to treat the deleterious effects of all these common diseases. The new knowledge is also fostering exploration in our understanding of the relationship between peptic ulcer disease, non-ulcerous dyspepsia and H. pylori infection.
References
Covacci A, Telford JL, Del Giudice G, Parsonnet J, Rappuoli R. Helicobacter pylori virulence and genetic geography. Science. 1999;284:1328–33.
Smoot DT, Mobley HL, Chippendale GR, Lewison JF, Resau JH. Helicobacter pylori urease activity is toxic to human gastric epithelial cells. Infect Immun. 1990;58:1992–4.
El-Omar EM, Carrington M, Chow WH, McColl KE, Bream JH, Young HA, et al. Interleukin-1 polymorphisms associated with increased risk of gastric cancer. Nature. 2000;404:398–402.
Pietroiusti A, Forlini A, Magrini A, Galante A, Bergamaschi A. Isolated H. pylori duodenal colonization and idiopathic duodenal ulcers. Am J Gastroenterol. 2008;103:55–61.
Peterson WL. Helicobacter pylori and peptic ulcer disease. N Engl J Med. 1991;324:1043–8.
Chan FKL, Leung WK. Peptic-ulcer disease. Lancet. 2002;360:933–41.
Marshall BJ, Langton SR. Urea hydrolysis in patients with campylobacter pyloridis infection. Lancet. 1986;327:965–6.
Marshall BJ, Barrett LJ, Prakash C, McCallum RW, Guerrant RL. Urea protects Helicobacter (Campylobacter) pylori from the bactericidal effect of acid. Gastroenterology. 1990;99:697–702.
Goddard AF, Logan RPH. Review article: urea breath tests for detecting Helicobacter pylori. Aliment Pharmacol Ther. 1997;11:641–9.
Gisbert JP, Pajares JM. Review article: 13C-urea breath test in the diagnosis of Helicobacter pylori infection-a critical review. Aliment Pharmacol Ther. 2004;20:1001–17.
Osaki T, Mabe K, Hanawa T, Kamiya S. Urease-positive bacteria in the stomach induce a false-positive reaction in a urea breath test for diagnosis of Helicobacter pylori infection. J Med Microbiol. 2008;57:814–9.
Peng NJ, Lai KH, Liu RS, Lee SC, Tsay DG, Lo CC, et al. Clinical significance of oral urease in diagnosis of Helicobacter pylori infection by [13C]urea breath test. Dig Dis Sci. 2001;46:1772–8.
Brandi G, Biavati B, Calabrese C, Granata M, Nannetti A, Mattarelli P, et al. Urease-positive bacteria other than Helicobacter pylori in human gastric juice and mucosa. Am J Gastroenterol. 2006;101:1756–61.
Chirica LC, Petersson C, Hurtig M, Jonsson BH, Borén T, Lindskog S. Expression and localization of α- and β-carbonic anhydrase in Helicobacter pylori. Biochim Biophys Acta. 2002;1601:192–9.
Marcus EA, Moshfegh AP, Sachs G, Scott DR. The periplasmic α-carbonic anhydrase activity of Helicobacter pylori is essential for acid acclimation. J Bacteriol. 2005;187:729–38.
Maity A, Som S, Ghosh C, Banik GD, Daschakraborty SB, Ghosh S, et al. Oxygen-18 stable isotope of exhaled breath CO2 as a non-invasive marker of Helicobacter pylori infection. J Anal At Spectrom. 2014;29:2251–5.
Neithercut WD, el Nujumi AM, McColl KEL. Measurement of urea and ammonium concentrations in gastric juice. J Clin Pathol. 1993;46:462–4.
Neithercut WD, Milne A, Chittajallu RS, el Nujumi AM, McColl KE. Detection of Helicobacter pylori infection of the gastric mucosa by measurement of gastric aspirate ammonium and urea concentrations. Gut. 1991;32:973–6.
Maity A, Banik GD, Ghosh C, Som S, Chaudhuri S, Daschakraborty SB, et al. Residual gas analyzer mass spectrometry for human breath analysis: a new tool for the non-invasive diagnosis of Helicobacter pylori infection. J Breath Res. 2014;8(1):016005. doi:10.1088/1752-7155/8/1/016005.
Crosson ER, Ricci KN, Richman BA, Chilese FC, Owano TG, Provencal RA, et al. Stable isotope ratios using cavity-ring-down spectroscopy: determination of 13C/12C for carbon dioxide in human breath. Anal Chem. 2002;74:2003–7.
Som S, Maity A, Banik GD, Ghosh C, Chaudhuri S, Daschakraborty SB, et al. Excretion kinetics of 13C-urea breath test: influences of endogenous CO2 production and dose recovery on the diagnostic accuracy of Helicobacter pylori infection. Anal Bioanal Chem. 2014;406:5405–12.
Keuleers R, Desseyn HO, Rousseau B, Van Alsenoy C. Vibrational analysis of urea. J Phys Chem A. 1999;103:4621–30.
Grdadolnika J, Maréchalb Y. Urea and urea–water solutions—an infrared study. J Mol Struct. 2002;615:177–89.
Acknowledgments
M. Pradhan acknowledges the ‘Rapid Grant for Young Investigators (No. BT/PR6683/GBD/27/477/2012)’ from the Department of Biotechnology (DBT, India) for this work. A. Maity, M. Pal and S. Maithani acknowledge the Department of Science & Technology (DST, India) for Inspire Fellowships, whereas S. Som acknowledges Bose Centre for PhD fellowship. We also thank all the volunteers who participated in this study.
Author contributions
Manik Pradhan arranged the funding; Manik Pradhan and Abhijit Maity conceived the study; Manik Pradhan, Sujit Chaudhuri supervised the whole study; Manik Pradhan and Abhijit Maity designed the study; Abhijit Maity, Mithun Pal, Suman Som and Sanchi Maithani collected and analysed the samples; all authors drafted the manuscript and critically reviewed it.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The present study has been approved by the Ethics Committee Review Board of AMRI Hospital, Salt Lake, Kolkata, India (Study no.: AMRI/ETHICS/2013/1). All the patients provided their written consent prior to the study.
Conflict of interest
The authors declare no conflict of interests.
Additional information
Abhijit Maity and Mithun Pal contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 722 kb)
Rights and permissions
About this article
Cite this article
Maity, A., Pal, M., Som, S. et al. Natural 18O and 13C-urea in gastric juice: a new route for non-invasive detection of ulcers. Anal Bioanal Chem 409, 193–200 (2017). https://doi.org/10.1007/s00216-016-9985-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-016-9985-y