Abstract
Rationale
Several second-generation antipsychotics are characterised by a significant antagonistic effect at serotonin 5-HT2A receptors (5-HT2AR), a feature that has been associated with lower incidence of extra-pyramidal symptoms and a putative amelioration of positive and negative symptoms experienced by schizophrenic patients. However, the neurofunctional substrate of 5-HT2A antagonism and its exact contribution to the complex pharmacological profile of these drugs remain to be elucidated.
Objectives
Here, we used pharmacological magnetic resonance imaging to map the modulatory effects of the selective 5-HT2AR antagonist Ml00907 on the spatiotemporal patterns of brain activity elicited by acute phencyclidine (PCP) challenge in the rat. PCP is a non-competitive NMDA receptor antagonist that induces dysregulation of corticolimbic glutamatergic neurotransmission and produces cognitive impairment and psychotic-like symptoms reminiscent of those observed in schizophrenia.
Results
Pre-administration of M100907 produced focal and region-dependent attenuation of PCP-induced response in frontoseptohippocampal areas. As early studies highlighted a permissive role of 5-HT2AR on frontal dopamine release, the role of post-synaptic dopamine D1 receptors on PCP-induced response was examined by using the potent antagonist SCH23390. Interestingly, SCH23390 did not affect PCP’s response in any of the regions examined. This finding rules out a significant contribution of dopamine in the functional changes mapped and, indirectly, the inhibitory effect of M100907, in favour of a glutamatergic origin.
Conclusions
Our data expand recent evidence suggesting a key role of 5-HT2AR in modulating glutamate-mediated cognitive performance in the prefrontal cortex and highlight the whole frontoseptohippocampal circuit as a key functional substrate of 5-HT2AR antagonism in normal and disease states.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia is a disabling psychiatric disorder characterised by complex and severe symptoms, including psychosis, hallucinations, cognitive deficits and mood alterations. Whilst the first antipsychotic agents targeted selectively the dopamine system through dopamine D2 receptors, second-generation antipsychotics (SGA; e.g. clozapine) are characterised by a multifaceted pharmacological profile, including multiple antagonist or inverse agonist properties at several neuroreceptor systems including serotonin, noradrenaline and histamine (Seeman 2002). This complexity makes it difficult to unravel the role and pharmacological contribution of individual target receptors, and despite almost two decades of active research since the identification of the first atypical antipsychotic clozapine, the precise mechanism responsible for the therapeutic effect of these molecules remains elusive.
The observation that several SGA present relatively low dopamine D2 receptors affinity but high affinity for serotonin (5-HT) receptors has stimulated great interest in the neurophysiological role of this neurotransmitter in schizophrenia (Meltzer 1996). In particular, it has been suggested that the relatively high affinity of clozapine for the 5-HT2A receptor (5-HT2AR) may contribute to its reduced side effect liability and to its greater efficacy in therapy-resistant schizophrenia (Tandon and Fleischhacker 2005; Ichikawa and Meltzer 1999; Meltzer et al. 1989).
Pre-clinical experimental evidence indicates the possibility of a significant role for 5HT2A receptors in modulating specific effects of SGA. Early studies showed that systemic or local administration of selective 5-HT2AR antagonists in the rat medial prefrontal cortex stimulates dopamine efflux (Schmidt and Fadayel 1995). This finding has led to the hypothesis of a permissive role of 5-HT2AR on frontal dopamine release as a contributory factor for a potentially superior cognitive effect of novel generation antipsychotics over classic dopamine D2 receptor antagonists (Kuroki et al. 1999; Ichikawa and Meltzer 1999). This hypothesis, however, has not been consistently confirmed in clinical studies, and the benefit exerted by SGA medications on cognitive performance remains questionable (Davidson et al. 1999). Recent studies have revealed an additional contribution of 5-HT2AR as modulators of glutamatergic neurotransmission in frontocortical areas (Scruggs et al. 2000, 2003; Zhai et al. 2002), an effect that seems to be relevant for the control of attentional and cognitive performance of rat prefrontal cortex (Carli et al. 2005; Mirjana et al. 2004) and could exert a direct anti-psychotic effect in disease states involving hyper-glutamatergic neurotransmission (Coyle 2006). However, most of the studies that investigated the neurobehavioural correlates of frontal 5-HT2AR antagonism have employed local impairment of NMDA and/or 5-HT2AR activity through in situ administration of pharmacological agents (Mirjana et al. 2004; Martin-Ruiz et al. 2001; Ceglia et al. 2004). Whilst this approach is valuable in linking discrete receptor populations with the cellular determinants of behaviour, its pharmacological significance is severely limited by the local nature of the manipulations employed, which neglects potentially important afferent and efferent contributions of a complex receptor system like 5-HT2A. Moreover, the wide distribution of 5-HT2AR in the brain (Hoyer et al. 1986) and its pre- and post-synaptic location at different neuronal sub-types (Meltzer et al. 2003) make it difficult to predict the overall functional effect and exact neuronal substrates of 5HT2AR antagonism in the living brain. As most of the pre-clinical research so far has focused on the role of the receptor in frontal areas, the function and possible contributions of the wide extra-frontal 5-HT2AR pool has remained virtually unexplored.
Non-invasive neuroimaging techniques such as pharmacological magnetic resonance imaging (phMRI) simultaneously integrate multiple functional contributions from widely distributed receptor populations, providing a spatially resolved description of pharmacological activity that is not straightforwardly related to receptor distribution and density (Jenkins et al. 2003; Gozzi et al. 2006; Honey and Bullmore 2004). In an attempt to identify the circuits modulated by 5-HT2AR antagonism in the living brain, we used a rat phMRI protocol to map the modulatory effect of the selective 5-HT2AR antagonist M100907 (Kehne et al. 1996) on the spatiotemporal pattern of response to an acute challenge with the N-methyl-d-aspartic acid receptor (NMDAR) antagonist phencyclidine (PCP). NMDAR antagonists like ketamine and PCP induce perceptual abnormalities, psychosis-like symptoms and mood changes in healthy humans and patients with schizophrenia (Malhotra et al. 1997; Adler et al. 1999; Allen and Young 1978), a finding that has led to the hypothesis that a decreased NMDAR function may be a pre-disposing or even causative factor in schizophrenia (Kristiansen et al. 2007; Krystal et al. 2002). The behavioural and functional effects of NMDAR antagonists are thought to arise primarily from a dose-dependent disinhibition of thalamocortical glutamatergic neurotransmission (Greene 2001; Large 2007), an event that cascades to involve several neurotransmitter systems including serotonin and dopamine (Greene 2001; Large 2007; Moghaddam et al. 1997). Recent neuroimaging studies have demonstrated the ability of NMDAR antagonists to elicit focal corticolimbothalamic activation in pre-clinical species (Gozzi et al. 2008b; Littlewood et al. 2006) and humans (Langsjo et al. 2003; Deakin et al. 2008), an effect totally suppressed by agents that modulate glutamate neurotransmission and regionally attenuated by atypical antipsychotics like clozapine (Gozzi et al. 2008a, b). In the present study, we explored the modulatory effect of the selective 5-HT2AR antagonist M100907 on the functional response to PCP as a means to identify and spatially resolve the circuital substrate of 5-HT2AR antagonism in the living brain. This approach allowed us to identify a focal and region-dependent attenuation of PCP-induced response by M100907 in frontoseptohippocampal areas.
Moreover, in an attempt to elucidate the neurochemical determinants of the changes mapped, we examined the role of dopamine D1 antagonism on the pattern of activation of PCP using the potent antagonist SCH22390 (Neisewander et al. 1998). Dopamine D1 receptors are crucially involved in the control of cognitive functions processed at a prefrontal level (Robbins 2005). Since M100907 has been reported to stimulate dopamine release in frontal areas (Schmidt and Fadayel 1995), the effect of this drug may involve post-synaptic activation of D1 dopamine receptors. Given the prevalent role of dopamine D1 receptors in mediating the fMRI response to dopamine-releasing agents (reviewed by Knutson and Gibbs 2007), by assessing the effect SCH22390, we sought to determine whether the functional response to PCP in our model presents significant contributions of dopaminergic nature. When considered with previous evidence of a negligible role of dopamine D2 receptors in the same experimental setup (Gozzi et al. 2008b), a lack of modulatory effect by SCH233990 would strongly argue against a predominant contribution of dopamine in the functional response to PCP mapped and, in turn, in the inhibitory effect of M100907. In the light of the established facilitatory role of 5-HT2AR on pyramidal glutamate neurotransmission (Scruggs et al. 2000, 2003; Zhai et al. 2002), this finding would thus provide important indirect evidence supporting a glutamatergic origin of the effects mapped with M100907.
Materials and methods
Animal preparation
The studies were performed on male Sprague–Dawley rats (250–350 g, Charles River, Como, Italy). Animal preparation/monitoring and MRI acquisition have been previously described in greater detail (Gozzi et al. 2008b). Briefly, rats were anaesthetised with 3% halothane, tracheotomised and artificially ventilated with a mechanical respirator. The left femoral artery and vein were cannulated and animal paralysed with a 0.25-mg/kg i.v. bolus of d-tubocurarine followed by a continuous infusion of 0.25 mg/kg/h through the artery. After surgery, halothane level was set to 0.8%. Arterial blood samples (0.5 ml) were taken immediately prior to and at the end of the fMRI time series acquisition, and paCO2 and paO2 were measured using a blood gas analyser (Table SI). No statistically significant difference in mean pre- and post-acquisition paCO2 values for each pair of PCP-challenged groups was found (p > 0.33, all groups; ANOVA, followed by Fisher’s least significant difference (LSD) test for multiple comparisons). The body temperature of all subjects was maintained within physiological range (37 ± 0.8°C) throughout the experiment by using a water heating system. Mean arterial blood pressure (MABP) was monitored continually through a transducer placed in the femoral artery.
rCBV measurement
MRI acquisition parameters have been previously described in greater detail (Gozzi et al. 2008a). Images were acquired using a Bruker Avance 4.7-T system. The MR acquisition for each subject comprised T2-weighted anatomical images using the rapid acquisition relaxation enhanced (RARE) sequence (Hennig et al. 1986; TR = 5,000 ms, TEeff = 76 ms, RARE factor 8, FOV 40 mm, 256 × 256 matrix, 16 contiguous 1 mm slices) followed by a time series acquisition with same spatial coverage (TReff = 2,700 ms, TEeff = 110 ms, RARE factor 32, 128 × 128 matrix, NA = 2, dt = 40).
Total MRI time-series acquisition time was 77 min (110 repetitions) for all groups. Following six reference images, 2.67 ml/kg of the blood pool contrast agent Endorem (Guerbet, France) was injected so that subsequent signal changes would reflect alterations in relative cerebral blood volume (rCBV; Mandeville et al. 1998).
Compounds, doses and experimental design
In order to allow for a better randomisation and keep the study manageable, drugs were tested in two separate studies. PCP challenge was administered 30 or 20 min after i.p. or s.c. pre-treatment (see below), and MRI data were acquired over a period of 30 min following the administration of the PCP challenge. Male SD rats were randomly assigned to one of the groups below.
M100907 1.5 mg/kg study
-
1.
Intraperitoneal pre-treatment with vehicle (water 1 ml/kg) followed by intravenous challenge with PCP (0.5 mg/kg, 1 ml/rat) 30 min later (n = 5)
-
2.
Intraperitoneal pre-treatment with M100907 (1.5 mg/kg) and intravenous challenge with PCP (0.5 mg/kg, 1 ml/rat) 30 min later (n = 6)
M100907 0.5 mg/kg study
-
3.
Intraperitoneal pre-treatment with vehicle (saline, 1 ml/kg), followed by intravenous challenge with PCP (0.5 mg/kg, 1 ml/rat) 30 min later (n = 8)
-
4.
Intraperitoneal pre-treatment with M100907 (0.5 mg/kg) followed by intravenous administration of PCP (0.5 mg/kg, 1 ml/rat) 30 min later (n = 6)
SCH23390 0.5 mg/kg study
-
5.
Subcutaneous pre-treatment with vehicle (water, 1 ml/kg) followed by intravenous challenge with PCP (0.5 mg/kg, 1 ml/rat) 20 min later (n = 6)
-
6.
Subcutaneous pre-treatment with SCH23390 (0.1 mg/kg; 1 ml/kg) followed by intravenous challenge with PCP (0.5 mg/kg, 1 ml/rat) 20 min later (n = 8)
-
7.
Intraperitoneal pre-treatment with water (1 ml/kg) followed by intravenous challenge with saline (1 ml/rat) 30 min later (n = 6). This group served as reference rCBV baseline for PCP in all studies
Phencyclidine hydrochloride was purchased from Tocris (Bristol, UK). M100907 was synthesised by the GSK department of Medicinal Chemistry. All compounds were dissolved in saline and injected at a rate of 1 ml/min. The doses chosen for the different drugs were based on previously published in vivo studies. PCP was tested at a sub-anaesthetic dose (0.5 mg/kg i.v.) that produces robust corticolimbothalamic activation in halothane-anesthetised rat (Gozzi et al. 2008c). The same dose of PCP has also been reported to elicit robust behavioural and metabolic (2-deoxyglucose) effects in conscious and freely-moving rats (Weissman et al. 1987; Gozzi et al. 2008b).
The doses of M100907 used in the present study showed robust effects in multiple behavioural readouts in rodents (reviewed by Kehne et al. 1996). The compound exhibits high potency and excellent selectivity (>100-fold separation at 26 receptors) and has been shown to be devoid of ex vivo receptor binding at alpha1-adrenetrgic or D2-dopamine receptor at doses 7-fold higher than the maximal dose tested in our experiments (Kehne et al. 1996). SCH23390 is a potent dopamine D1 antagonist (Andersen et al. 1992). The pre-treatment regimen used with SCH23390 has been reported to produce rapid and sustained exposure in the rat brain (Hietala et al. 1992). The same dose of SCH223390 tested produced robust in vivo antagonism of acute and chronic effect of dopaminergic agents in numerous rat behavioural paradigms (Molloy and Waddington 1984; Garris et al. 1994; Wolf and Xue 1999; Zahrt et al. 1997) whilst minimising the cataleptic and cognitive-impairing effects reported at higher doses (Wadenberg 1992).
Data analysis
rCBV time series image data for each experiment were analysed within the framework of the general linear model as described in greater detail elsewhere (Worsley et al. 1992; Schwarz et al. 2006b). The maps thus obtained were used to guide the selection of activated/deactivated regions for subsequent volume of interest (VOI)-based quantification and comparison of efficacy of pre-treatments.
Signal intensity changes in the time series were converted into fractional rCBV on a pixel-wise basis, using a constrained exponential model of the gradual elimination of contrast agent from the blood pool (Schwarz et al. 2003, 2006b). Individual subjects in each study were spatially normalised by a 9 degree-of-freedom affine transformation mapping their T2-weighted anatomical images to a stereotaxic rat brain MRI template set (Schwarz et al. 2006a) and applying the resulting transformation matrix to the accompanying rCBV time series. rCBV time series for the PCP or vehicle challenge were calculated covering 8 min (12 time points) pre-challenge baseline and 25 min (38 time points) post-challenge window, normalised to a common injection time point. Image-based time series analysis was carried out using FMRI Expert Analysis Tool Version 5.63, part of FMRIB’s Software Library (www.fmrib.ox.ac.uk/fsl) with 0.8 mm spatial smoothing (≈2.5 × in-plane voxel dimension) and using a model function identified by Wavelet Cluster Analysis across all animals in the cohort, capturing the temporal profile of the signal change induced by PCP challenge (Whitcher et al. 2005; Schwarz et al. 2006b). As no substantial differences in the temporal profile of PCP-induced changes were observed across PCP-challenged groups (see “Results” section), a common regressor was used (Supplementary Figure 1). Consistent with previous studies, PCP did not produce any significant short-lived or negative signal changes in any of the regions analysed (Gozzi et al. 2008a, b).
The design matrix also included the temporal derivative of this regressor and a linear ramp (both orthogonalised to the regressor of interest) with the aim to capture additional variance due to slight deviations in individual subjects or brain regions from the signal model time course as described in more detail in Schwarz et al. (2006b). The coefficients of the model function thus provided a map of rCBV response amplitude for each injection in each subject. Higher-level group comparisons were carried out using FMRIB’s Local Analysis of Mixed Effects; Z (Gaussianised T/F) statistic images were thresholded using clusters determined by Z > 2.3 and a corrected cluster significance threshold of p = 0.01 (Worsley et al. 1992; Friston et al. 1994). Volumetric three-dimensional reconstructions of activation maps were generated using custom in-house software written in IDL (Research Systems Inc., Boulder, CO, USA).
VOI time courses for the PCP challenge were extracted from unsmoothed rCBV time series data using a 3D digital reconstruction of a rat brain atlas (Paxinos and Watson 1998) co-registered with the MRI template (Schwarz et al. 2006a), using custom in-house software written in IDL (Research Systems Inc., Boulder, CO, USA). A list of the VOIs examined and their anatomical definitions can be found in (Gozzi et al. 2008b). For each VOI time course, the average rCBV over a 16-min time window covering the peak response to PCP (4–20 min post-injection) was used as a summary statistic of the relative change. The effect of pre-treatment on the magnitude of average rCBV in different VOIs was assessed by a one-way ANOVA followed by Fisher’s LSD test for multiple comparisons.
VOI time courses pre- and post-M100907 administration were also examined to assess potential effects of pre-treatment per se on basal CBV. To this end, rCBV time courses were also calculated for the pre-treatment over a time window covering 6 min (8 time points) pre-injection baseline and 22 min (32 time points, groups 1–4 and 7) or 17 min (24 time points, groups 5 and 6) post-injection window normalised to a common injection time point. VOI time courses were extracted from unsmoothed rCBV time series in the same regions examined for the PCP challenge.
Administration of vehicle, SCH23390 or PCP was accompanied by small and transient alterations of MABP. M100907 produced a sustained decrease in MABP that lasted throughout PCP’s pre-injection time window (mean MABP ≈ 65 mmHg). In all cases, peak magnitude of the MABP observed was within the cerebral blood flow auto-regulation range measured under the same anaesthetic conditions used in the present study (Gozzi et al. 2007). As shown by us and other groups, positive or negative pharmacologically evoked MABP changes within the auto-regulation range mentioned above do not result in significant central rCBV response when spin-echo MRI sequences are used (Zaharchuk et al. 1999; Gozzi et al. 2006).
Results
Vehicle-pre-treated animals (groups 1 and 3 and 5) showed a robust and sustained rCBV response to PCP in several corticolimbothalamic structures (Figs. 1, 2, 3, 4 and 5), consistent with previous observations (Gozzi et al. 2008b, c). Statistically significant activation was observed in limbic cortical regions with extension into the motor, visual, parietal- and temporal association and rhinal cortices. Additional foci of subcortical activation were observed in the medial and lateral habenula, amygdala, anterodorsal, dorsolateral and ventromedial thalamus, posterodorsal, anterodorsal and ventral and posterior hippocampus, the striatum and the nucleus accumbens. The overall temporal profile of PCP-induced activation was comparable in all the activated regions (Fig. 4; Supplementary Figures 2 and 3). Despite differences in the peak magnitude of PCP response across studies, the spatial distribution and relative amplitude of the regional response to PCP were very consistent and conserved across the different control groups (groups 1, 3 and 5; Figs. 3 and 5).
a Anatomical distribution of the rCBV response following acute challenge with PCP (0.5 mg/kg i.v., group 1) with respect to baseline (vehicle–vehicle, group 5). b Anatomical distribution of the rCBV response following acute challenge with PCP (0.5 mg/kg i.v., group 1) in animals pre-treated with M100907 with respect to baseline (vehicle–vehicle, group 5). Orange/yellow indicates increased rCBV versus baseline (vehicle–vehicle). c Map of the regions showing an attenuated PCP response in animals pre-treated with M100907 (1.5 mg/kg i.p., group 1 vs. group 2). Blue indicates decreased rCBV versus baseline. Z statistics threshold levels are reported beside each map. Maps were cluster-corrected using a p = 0.01 significance level. mPFC medial prefrontal cortex, Sp septum, VHc ventral hippocampus
a Volumetric reconstruction of the pattern of rCBV activation produced by acute challenge with PCP with respect to vehicle and b attenuating effect of pre-treatment with the selective 5-HT2A antagonist M100907 (1.5 mg/kg i.p.) in frontoseptohippocampal regions. PFC medial prefrontal cortex, VHc ventral hippocampus, Sp septum
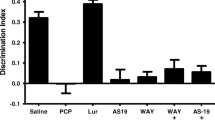
Magnitude of mean rCBV response (AUC4–20 min) to PCP in representative regions of interest. Left Veh-PCP (group 3); Veh-PCP (group 4). Right Veh-PCP (group 1), M100907 1.5 mg/kg–PCP (group 2); *p < 0.05 versus Veh-PCP (group 1), ANOVA followed by Fisher LSD test for multiple comparison. Acb nucleus accumbens, Cpu caudate putamen, DL dorsolateral thalamus, VM ventromedial thalamus, AD anterodorsal hippocampus, V ventral hippocampus, PDG posterior dentate gyrus, PD posterodorsal hippocampus, S1 primary somatosensory cortex, V1 primary visual cortex, Cg cingulate cortex, PFC medial prefrontal cortex
rCBV time course following PCP injection in representative brain structures. PCP was administered at time 0. Baseline data were obtained in animals pre-treated and challenged with vehicle (saline, group 5). Data are plotted as mean ± SEM within each group. Veh-PCP: group 1, M100907 (1.5 mg/kg i.p.)–PCP: group 2, Veh-Veh: group 7. PFC medial prefrontal cortex, VHc ventral hippocampus, DLTh dorsolateral thalamus, S1Ctx primary somatosensory cortex
Magnitude of mean rCBV response (AUC4–20 min) to PCP in representative regions of interest. Veh-PCP (group 5), SCH23390 0.1 mg/kg (group 6). Acb nucleus accumbens, Cpu caudate putamen, DL dorsolateral thalamus, VM ventromedial thalamus, AD anterodorsal hippocampus, V ventral hippocampus, PDG posterior dentate gyrus, PD posterodorsal hippocampus, S1 primary somatosensory cortex, V1 primary visual cortex, Cg cingulate cortex, PFC medial prefrontal cortex
Pre-administration of M100907 (1.5 mg/kg i.p.) produced region-dependent and sustained attenuation of PCP-induced rCBV response (Figs. 1, 2, 3 and 4). Foci of significant inhibition were observed in the medial prefrontal cortex, diagonal band, septal nuclei and in ventral hippocampal and peri-hippocampal areas, including the rhinal cortex (p < 0.05, ANOVA; Figs. 1, 2, 3 and 4). Three-dimensional reconstruction of the areas of attenuation highlighted the involvement of contiguous septofrontal and hippocampal structures (Fig. 2). No areas of increased response to PCP were observed. The lower dose of M100907 (0.5 mg/kg i.p.) did not produce statistically significant attenuation of PCP response in any of the regions examined (p > 0.28 all regions; Fig. 3), although a trend was evident in the medial prefrontal cortex (p < 0.09). This effect was best seen on rCBV time courses (Supplementary Figure 2). Pre-administration of SCH23390 (0.1 mg/kg i.p.) did not produce any significant alteration of PCP response in any of the regions examined (p > 0.24, all regions; Fig. 5; Supplementary Figure 3).
Administration of M100907 per se (0.5 or 1.5 mg/kg i.p.) produced small (2–8%) and short-lived (4–9 min) rCBV increases in various brain regions, including the medial prefrontal cortex and ventral hippocampus (Supplementary Figures 4 and 5). At the time of PCP challenge, no apparent basal rCBV alteration with respect to vehicle was present in any of the regions examined. Intraperitoneal administration of SCH23390 did not produce visible alteration of basal rCBV with respect to vehicle in any of the regions examined (Supplementary Figure 6).
Discussion
In the present study, we show that selective antagonism of 5-HT2AR induces focal attenuation of PCP-induced activation in frontoseptohippocampal areas of the rat brain. Our results extend previous findings of a role of 5-HT2AR in modulating frontocortical activity (Ceglia et al. 2004; Mirjana et al. 2004) by highlighting the additional involvement of septal and ventral–hippocampal structures as integrated substrate of the action of 5-HT2AR antagonism in the living brain. This finding is of particular interest in the light of clinical evidence suggesting a correlation between frontohippocampal hyperactivity and cognitive and perceptual alterations observed in unmedicated schizophrenia patients (Silbersweig et al. 1995; Liddle et al. 2000; Parellada et al. 1994; Ngan et al. 2002; Soyka et al. 2005; Medoff et al. 2001)
The observation that 5-HT2AR antagonism affects brain activity in frontohippocampal areas is consistent with previous pre-clinical research. 5-HT2A receptor density in these regions is high (Cornea-Hebert et al. 1999), and immunofluorescence studies have demonstrated marked 5-HT2AR immunoreactivity in GABAergic and cholinergic septohippocampal terminals, as well as in pyramidal and granule cells of the hippocampus (Luttgen et al. 2004). These findings suggest that 5-HT2AR can regulate hippocampal activity both via local pre-synaptic mechanisms and upstream modulation of septal outputs. In agreement with this, electrophysiology studies showed that M100907 and atypical antipsychotic can potently inhibit the excitatory action of serotonin on various septohippocampal neuronal populations (Alreja 1996; Liu and Alreja 1997; Piguet and Galvan 1994; Shen and Andrade 1998). However, the effect does not trivially reflect 5-HT2AR receptor distribution. Indeed, high 5-HT2AR density has been reported in large brain structures such as basal ganglia, thalamus and neocortex (Cornea-Hebert et al. 1999) which did not show significant modulation by M100907. This finding is of interest, as it highlights a discrete circuit whose activity is focally modulated by a widely distributed receptor population, and underscores the possibility to use functional neuroimaging methods to describe specific psychopharmacological contributions in terms of modulation of focal neural circuits.
The functional imaging technique used for this study does not provide direct information on the specific cellular or neurochemical determinants of the modulatory action of M100907. However, multiple lines of evidence support a glutamatergic origin of the effect mapped. Firstly, 5-HT2AR can positively modulate glutamatergic neurotransmission in frontocortical areas (Ceglia et al. 2004; Scruggs et al. 2000; Aghajanian and Marek 1997), through blockade of 5-HT2A pre-synaptic heteroreceptors (Aghajanian and Marek 2000; Martin-Ruiz et al. 2001). Consistent with this hypothesis, NMDAR antagonists have been shown to induce a dose- and use-dependent hyper-glutamatergic state through deregulation of pyramidal glutamatergic activity by selectively impairing recurrent feedback from GABAergic inter-neurons (Gozzi et al. 2008a; Greene 2001; Homayoun and Moghaddam 2007). Secondly, compounds that modulate pyramidal glutamate release have been shown to markedly attenuate the functional and behavioural cascade triggered by NMDAR antagonism (Gozzi et al. 2008a, b; Cartmell et al. 1999). In agreement with this, Ceglia et al. (2004) reported the ability of M100907 to prevent the increase in frontocortical glutamate induced by the NMDAR antagonist 3-(R)-2-carboxypiperazin-4-propyl-1-phosphonic acid (CPP), an effect that also produced an improvement of CPP-induced impairment in attentional performance. Conversely, little or no inhibitory effect has been observed with drugs that target neurotransmitter systems secondarily activated by the effect of NMDAR antagonism such as dopamine D2 antagonists (Idris et al. 2005; Gozzi et al. 2008b; Large 2007).
Alternatively, since M100907 has been reported to stimulate dopamine release in frontal areas (Schmidt and Fadayel 1995), the inhibitory effect observed could reflect post-synaptic activation of D1 dopamine receptors. However, this effect, however, cannot be straightforwardly investigated by using dopamine-mimetic drugs, as these compounds produce robust and widespread haemodynamic alterations that could saturate the subsequent response to a PCP challenge (Choi et al. 2006; Schwarz et al. 2004, 2007). We therefore examined the role of post-synaptic dopamine D1 receptors on PCP-induced fMRI response examined using a potent D1 antagonist (SCH23390, 0.1 mg/kg; Andersen et al. 1992). Acute administration of PCP generates disinhibition of corticothalamic glutamatergic neurotransmission, an event that cascades to involve several neurotransmitter systems including serotonin and dopamine (Greene 2001; Large 2007; Moghaddam et al. 1997). Increased dopamine release upon acute administration of NMDAR antagonists has been observed in mesolimbic areas and in frontal regions of the rat (Moghaddam et al. 1997; Javitt et al. 1999). Given the prevalent role of dopamine D1 receptors in mediating the fMRI response to dopamine-releasing agents (Knutson and Gibbs 2007), by assessing the effect of selective DA antagonists, we sought to determine whether the functional response to PCP in our model presents significant contributions of dopaminergic nature. Interestingly, pre-administration of SCH23390 did not produce any significant alteration of PCP response in any of the regions examined. When considered with previous evidence of a negligible role of dopamine D2 receptors in the same experimental setup (Gozzi et al. 2008b), this finding strongly argues against a predominant role of dopamine in the functional changes mapped and, in turn, in the inhibitory action observed with M100907. In the light of the established facilitatory role of 5-HT2AR on pyramidal glutamate neurotransmission discussed above, it seems thus likely that that the effect of M100907 reflects a local reduction in glutamatergic neurotransmission. However, whilst this is by far the most plausible neurochemical mechanism, our data do not permit to rule out contributions of PCP-induced serotonergic neurotransmission independent of the neuromodulatory role of the 5-HT2AR on glutamate release
Although a comprehensive discussion of the role of dopamine in the cascade elicited by NMDAR antagonism is beyond the scope of the manuscript, the lack of effect of SCH22390 is of interest per se as it provides additional evidence of a subsidiary role of this neurotransmitter in mediating the neurobehavioural effects of these drugs, a finding observed by numerous investigators using dopamine D2 antagonists in different experimental models and readouts (Idris et al. 2005; Gozzi et al. 2008b; Krystal et al. 1999; Linn et al. 2003). Our finding extends these results to the D1 receptor subtype, suggesting that dopaminergic mechanisms are engaged far downstream in the neurofunctional cascade triggered by psychotogenic doses of NMDAR antagonists.
M100907 produced significant attenuation of PCP only at the highest dose (1.5 mg/kg), although a trend in the mPFC was apparent at the lower dose tested (0.5 mg/kg; Fig. 3). As pharmacodynamic studies reported complete inhibition of behavioural response to serotonergic agents at doses of 0.1 mg/kg (Schreiber et al. 1995; Kehne et al. 1996), the presence of significant attenuation only at the higher dose may call into question putative contributions from other receptor types, namely alpha1-adrenergic, dopamine D2 or 5-HT2c. However, multiple lines of evidence make this hypothesis very unlikely. Firstly, M100907’s affinity for D2 receptors is >2,500-fold lower than 5-HT2A (Kehne et al. 1996). Consistent with this, the drug failed to reduce apomorphine induced climbing in rats, an index of D2 receptor antagonism, at a dose as high as 8 mg/kg (Kehne et al. 1996; Sorensen et al. 1993). Although the selectivity at alpha1-adrenergic receptor is slightly lower (>100-fold), the drug did not show significant ex vivo receptor binding at alpha1-adrenergic receptors at doses up to 10 mg/kg (Kehne et al. 1996). Moreover, a dose of 16 mg/kg of M100907 (i.e. 10-fold higher than the effective dose of our study) failed to antagonise the acute cardiovascular effects of the alpha1-adrenergic agonist phenylephrine (Kehne et al. 1996) in a widely used behavioural assay index of alpha1-receptor antagonism (Peroutka et al. 1977). Finally, 1 mg/kg of M100907 did not show significant antagonism of the pre-pulse inhibition-disruptive effect of the potent alpha1-adrenergic agonist cirazoline in two different rat strains (Varty et al. 1999). In the light of these findings, a significant contribution of dopamine D2 or alpha1-adrenergic receptors appears extremely unlikely.
Secondly, although receptor binding data indicate a >100-fold selectivity over 5-HT2C receptors (Kehne et al. 1996; Palfreyman et al. 1993), in vitro antagonism assays of functional selectivity highlighted a >1,000-fold separation between the two receptors (Kehne et al. 1996). In agreement with this, a number of in vivo studies showed that M100907, at the same or higher doses tested here, did not produce detectable effects in behavioural paradigms sensitive to the action of selective 5-HT2C antagonism (Fletcher et al. 2002; Zaniewska et al. 2007; Hajos et al. 2003), or produced significant effects that were not paralleled by the action of selective 5-HT2C antagonists (Varty et al. 1999). Thirdly, the nature of the behavioural alterations produced by 5-HT2C antagonism in models of NMDAR hypo-function cannot be easily be reconciled with our findings, as several reports showed that 5-HT2C antagonism does not inhibit, but rather exacerbates, the acute effects of NMDAR antagonists (Higgins et al. 2003; Hutson et al. 2000; O’Neill et al. 1999; Wood et al. 2001). These effects have been linked to an increased dopaminergic tone consequent to the blockade of 5- HT2C receptors in several mesocortical areas, including the medial prefrontal cortex (Gobert et al. 2000). However, as discussed above, our data with the dopamine D1 antagonists SCH23390 argue against a significant contribution of dopaminergic neurotransmission in the functional effect mapped. Moreover, consistent with the hypothesis of an opposing functional role of 5-HT2A and 5-HT2C receptors (Ichikawa and Meltzer 1999), electrophysiology studies demonstrated that 5-HT2C antagonism do not decreases, but rather increases the activity of septohippocampal circuit (expressed as theta waves recordings), an effect reversed by selective 5-HT2C agonists (Hajos et al. 2003). In agreement with this, selective 5-HT2C agonists have been recently shown to be highly efficacious in inhibiting the behavioural effects of NMDAR antagonism (Marquis et al. 2007).When considered together, these data strongly argue against a significant contribution of 5-HT2C or other spurious receptor systems in the inhibitory effect of M100907 observed in this study.
Based on recent ex vivo receptor occupancy data in the rat frontal cortex, the doses of M100907 used in the present manuscript (1.5 and 0.5 mg/kg i.p.) would be expected to have an estimated receptor occupancy of approximately 100% and 80% at the end 30-min post-PCP time window examined (Knauer et al. 2008). Although the different receptor occupancy alone could explain the lack of response at the low dose, other experimental factors could have contributed to stretch or right-shift the effective dose–efficacy curve. For example, pharmacokinetic studies of M100907 in the rat showed that the compound reaches peak brain concentrations (T max) 32 ± 11 min after its intravenous administration (5 mg/kg; Scott and Heath 1998). Assuming similar parameters following use of intraperitoneal route, the relatively long-time window used to quantify its effect in the present manuscript (30–60 min post-administration) may not be optimally suited to maximise the sensitivity of the measurements. Furthermore, molecular interactions between M100907, PCP and the anaesthetic used (halothane) could also play a significant contribution in vivo. Recent work from (Kapur and Seeman 2002) showed the ability of PCP and ketamine to bind to the high-affinity state of 5-HT2A receptor with micromolar affinity, a value consistent with brain exposure of PCP at the dose used in the present work (Proksch et al. 2000). Moreover, the same authors recently demonstrated that low doses of volatile anaesthetics such as halothane or isoflurane can also bind to (and stimulate) the activity of 5-HT2A receptors (Seeman and Kapur 2003). Thus, simultaneous interactions of PCP and anaesthetic with 5-HT2A receptors may produce significant functional antagonisation or pharmacological displacement of M100907, resulting in the need of higher doses to exert pharmacologically significant effects. Interestingly, a number of studies of 5-HT2A antagonism in PCP models of NMDAR hypo-function showed significant effects only at doses similar to those used in our study (Varty et al. 1999; Habara et al. 2001), whilst studies performed at lower doses do not consistently show effects (Rodefer et al. 2008; Winter et al. 2004; Adams and Moghaddam 2001). This suggests that PCP-5-HT2A receptor interactions might be non-negligible even in absence of anaesthesia. Future experiments using NMDAR antagonist devoid of significant 5-HT2A affinity (i.e. CPP; Lehmann et al. 1987) may be performed to investigate this hypothesis. Nonetheless, it should be emphasised that if these interactions do occur in vivo, they are expected to affect the effectiveness, but not the outcome, of 5-HT2A antagonism in the brain, thus leaving unaltered the functional significance of the effects described in our manuscript.
Whilst the transient state produced by the acute administration of PCP cannot possibly mimic the entire syndrome and course of a multi-factorial disease like schizophrenia, the ability of NMDAR antagonists to produce behavioural effects akin to positive and negative symptoms of the disorder in human volunteers (Krystal et al. 2003; Adler et al. 1999) suggests that the hyper-glutamatergic state produced by these drugs alters neural function in circuits that are relevant for this condition. Importantly, the circuits activated by NMDAR antagonists in rodents and humans as seen with various functional imaging modalities (Deakin et al. 2008; Gozzi et al. 2008c; Langsjo et al. 2003; Vollenweider, personal communication) show a high degree of homology between species and do not appear to be qualitatively affected by the anaesthesia (Gozzi et al. 2008c). Several neuroimaging studies have provided evidence for localised anatomical and functional abnormalities in frontohippocampal areas of schizophrenia patients. Imaging studies of haemodynamic parameters have highlighted increased blood flow and abnormal hippocampal activity at rest and during the performance of memory retrieval tasks (Heckers 2001; Medoff et al. 2001). Similarly, neurometabolic studies in unmedicated schizophrenic patients have highlighted increased tonic frontocortical activity, a feature that has been linked to the sensory flooding, cognitive fragmentation and ego-dissolution seen in both drug-induced and disorder-based psychosis (Parellada et al. 1994; Soyka et al. 2005; Geyer and Vollenweider 2008; Volkow et al. 1986). Thus, the ability of 5-HT2AR antagonism to produce region-selective attenuation of aberrant frontohippocampal states suggests that this pharmacological mechanism might contribute to some of the therapeutic effect of clozapine and other second generation anti-psychotics that possess significant 5-HT2AR affinity (Ichikawa and Meltzer 1999). A few clinical studies have recently addressed the role of selective 5-HT2AR antagonism in schizophrenia patients. In a two multicenter, placebo and haloperidol-controlled studies in USA, M100907 showed statistically significant efficacy on total score versus placebo of positive and negative symptoms (De Paulis 2001; Marder 1999), although the drug was less effective than haloperidol. The effect was not confirmed in a European study involving patients with predominantly negative symptoms, although M100907-treated schizophrenic subjects showed significantly fewer preservative errors in the Wisconsin Card Sorting Test (Roth et al. 2004). A recent placebo-controlled study using a the 5-HT2A/2CR antagonist SR46349B produced significant reductions in the positive and negative syndrome scale total and negative scores versus placebo (Meltzer et al. 2004). Likewise, the 5-HT2A/2CR antagonist mianserin produced significant improvement in measures of cognitive function (learning, memory and sustained attention) when the drug was tested as add-on therapy in schizophrenic patients (Poyurovsky et al. 2003). Collectively, the limited clinical data available suggest that 5-HT2A antagonism per se may produce mild, but clinically significant antipsychotic effects, involving a moderate improvement of both positive and negative symptoms. This is in agreement with our observation that the 5-HT2AR antagonist M100907, unlike glutamatergic compounds (Gozzi et al. 2008a, b), is unable to entirely suppress the functional cascade produced by PCP in the rat brain, but selectively reduces PCP-induced activation in the frontoseptohippocampal circuit, a key substrate of higher cognitive functions that appears to be tonically hyper-activated in drug-induced and disorder-based psychosis. Consistent findings have been reproduced in pre-clinical behavioural models, where 5-HT2AR receptor antagonists do not consistently antagonise the entire spectrum of behavioural and neurochemical responses produced by NMDAR antagonists in the rat (Large 2007; Adams and Moghaddam 2001) but have been shown to improve frontocortical functions (Mirjana et al. 2004; Winstanley et al. 2003). Of interest, glucose metabolism studies using positron emission tomography highlighted a tight correlation between depression of corticohippocampal activity and antipsychotic action elicited by a single dose of the atypical anti-psychotics risperidone (Liddle et al. 2000). Whilst multiple receptor contributions are likely to contribute to this effect, this finding is important as it suggests that the circuital mechanism identified in our study may be of clinical significance.
In conclusion, we have shown that 5-HT2AR antagonist reduces PCP-induced activation in discrete brain regions, including frontal cortex, septum and ventral–hippocampal areas. These results are consistent with pre-clinical studies highlighting a key role of 5-HT2AR in modulating glutamate-mediated cognitive performance in the rodent prefrontal cortex and extend those findings by highlighting a role of the frontoseptohippocampal circuit as an integrated substrate of the action of 5HT2A antagonism in the living brain. Collectively, pre-clinical and clinical research provide converging evidence that 5-HT2AR antagonism can exert a region-selective modulation of frontoseptohippocampal activity that might be of clinical benefit when the circuit is functionally hyperactive.
References
Adams BW, Moghaddam B (2001) Effect of clozapine, haloperidol, or M100907 on phencyclidine-activated glutamate efflux in the prefrontal cortex. Biol Psychiatry 50:750–757
Adler CM, Malhotra AK, Elman I, Goldberg T, Egan M, Pickar D, Breier A (1999) Comparison of ketamine-induced thought disorder in healthy volunteers and thought disorder in schizophrenia. Am J Psychiatry 156:1646–1649
Aghajanian GK, Marek GJ (1997) Serotonin induces excitatory postsynaptic potentials in apical dendrites of neocortical pyramidal cells. Neuropharmacology 36:589–599
Aghajanian GK, Marek GJ (2000) Serotonin model of schizophrenia: emerging role of glutamate mechanisms. Brain Res Rev 31:302–312
Allen RM, Young SJ (1978) Phencyclidine-induced psychosis. Am J Psychiatry 135:1081–1084
Alreja M (1996) Excitatory actions of serotonin on GABAergic neurons of the medial septum and diagonal band of Broca. Synapse 22:15–27
Andersen PH, Gronvald FC, Hohlweg R, Hansen LB, Guddal E, Braestrup C, Nielsen EB (1992) NNC-112, NNC-687 and NNC-756, new selective and highly potent dopamine D1 receptor antagonists. Eur J Pharmacol 219:45–52
Carli M, Baviera M, Invernizzi RW, Balducci C (2005) Dissociable contribution of 5-HT1A and 5-HT2A receptors in the medial prefrontal cortex to different aspects of executive control such as impulsivity and compulsive perseveration in rats. Neuropsychopharmacology 31:757–767
Cartmell J, Monn JA, Schoepp DD (1999) The metabotropic glutamate 2/3 receptor agonists LY354740 and LY379268 selectively attenuate phencyclidine versus d-amphetamine motor behaviors in rats. J Pharmacol Exp Ther 291:161–170
Ceglia I, Carli M, Baviera M, Renoldi G, Calcagno E, Invernizzi RW (2004) The 5-HT2A receptor antagonist M100, 907 prevents extracellular glutamate rising in response to NMDA receptor blockade in the mPFC. J Neurochem 91:189–199
Choi JK, Chen YI, Hamel E, Jenkins BG (2006) Brain hemodynamic changes mediated by dopamine receptors: role of the cerebral microvasculature in dopamine-mediated neurovascular coupling. NeuroImage 30:700–712
Cornea-Hebert V, Riad M, Wu C, Singh SK, Descarries L (1999) Cellular and subcellular distribution of the serotonin 5-HT2A receptor in the central nervous system of adult rat. J Comp Neurol 409:187–209
Coyle J (2006) Glutamate and schizophrenia: beyond the dopamine hypothesis. Cell Mol Neurobiol 26:363–382
Davidson RJ, Abercrombie H, Nitschke JB, Putnam K (1999) Regional brain function, emotion and disorders of emotion. Curr Opin Neurobiol 9:228–234
De Paulis T (2001) M-100907 (Aventis). Curr Opin Investig Drugs 2:123–132
Deakin JFW, Lees J, McKie S, Hallak JEC, Williams SR, Dursun SM (2008) Glutamate and the neural basis of the subjective effects of ketamine: a pharmaco-magnetic resonance imaging study. Arch Gen Psychiatry 65:154–164
Fletcher PJ, Grottick AJ, Higgins GA (2002) Differential effects of the 5-HT(2A) receptor antagonist M100907 and the 5-HT(2C) receptor antagonist SB242084 on cocaine-induced locomotor activity, cocaine self-administration and cocaine-induced reinstatement of responding. Neuropsychopharmacology 27:576–586
Friston KJ, Jezzard P, Turner R (1994) Analysis of functional MRI time-series. Hum Brain Mapp 1:153–171
Garris PA, Ciolkowski EL, Pastore P, Wightman RM (1994) Efflux of dopamine from the synaptic cleft in the nucleus accumbens of the rat brain. J Neurosci 14:6084–6093
Geyer MA, Vollenweider FX (2008) Serotonin research: contributions to understanding psychoses. Trends Pharmacol Sci 29:445–453
Gobert A, Rivet JM, Lejeune F, Newman-Tancredi A, dhumeau-Auclair A, Nicolas JP, Cistarelli L, Melon C, Millan MJ (2000) Serotonin(2C) receptors tonically suppress the activity of mesocortical dopaminergic and adrenergic, but not serotonergic, pathways: a combined dialysis and electrophysiological analysis in the rat. Synapse 36:205–221
Gozzi A, Schwarz A, Reese T, Bertani S, Crestan V, Bifone A (2006) Region-specific effects of nicotine on brain activity: a pharmacological MRI study in the drug-naïve rat. Neuropsychopharmacology 31:1690–1703
Gozzi A, Ceolin L, Schwarz A, Reese T, Bertani S, Bifone A (2007) A multimodality investigation of cerebral haemodynamics and autoregulation in phMRI. Magn Reson Imaging 25:826–833
Gozzi A, Herdon H, Schwarz A, Bertani S, Crestan V, Turrini G, Bifone A (2008a) Pharmacological stimulation of NMDA receptors via co-agonist site suppresses fMRI response to phencyclidine in the rat. Psychopharmacology 201:273–284
Gozzi A, Large C, Schwarz A, Bertani S, Crestan V, Bifone A (2008b) Differential effects of antipsychotic and glutamatergic agents on the phMRI response to phencyclidine. Neuropsychopharmacology 33:1690–1703
Gozzi A, Schwarz AJ, Reese T, Crestan V, Bifone A (2008c) Drug-anaesthetic interaction in phMRI: the case of the pyschotomimetic agent phencyclidine. Magn Reson Imag 26:999–1006
Greene R (2001) Circuit analysis of NMDAR hypofunction in the hippocampus, in vitro, and psychosis of schizophrenia. Hippocampus 11:569–577
Habara T, Hamamura T, Miki M, Ohashi K, Kuroda S (2001) M100907, a selective 5-HT(2A) receptor antagonist, attenuates phencyclidine-induced Fos expression in discrete regions of rat brain. Eur J Pharmacol 417:189–194
Hajos M, Hoffmann WE, Weaver RJ (2003) Regulation of septo-hippocampal activity by 5-hydroxytryptamine2C receptors. J Pharmacol Exp Ther 306:605–615
Heckers S (2001) Neuroimaging studies of the hippocampus in schizophrenia. Hippocampus 11:520–528
Hennig J, Nauerth A, Friedburg H (1986) RARE imaging: a fast imaging method for clinical MR. Magn Reson Med 3:823–833
Hietala J, Sepp T, Lappalainen J, Syvlahti E (1992) Quantification of SCH 39166, a novel selective D1 dopamine receptor antagonist, in rat brain and blood. Psychopharmacology 106:455–458
Higgins GA, Enderlin M, Haman M, Fletcher PJ (2003) The 5-HT2A receptor antagonist M100, 907 attenuates motor and ‘impulsive-type’ behaviours produced by NMDA receptor antagonism. Psychopharmacology 170:309–319
Homayoun H, Moghaddam B (2007) NMDA receptor hypofunction produces opposite effects on prefrontal cortex interneurons and pyramidal neurons. J Neurosci 27:11496–11500
Honey G, Bullmore E (2004) Human pharmacological MRI. Trends Pharmacol Sci 25:366–374
Hoyer D, Pazos A, Probst A, Palacios JM (1986) Serotonin receptors in the human brain. II. Characterization and autoradiographic localization of 5-HT1C and 5-HT2 recognition sites. Brain Res 376:97–107
Hutson PH, Barton CL, Jay M, Blurton P, Burkamp F, Clarkson R, Bristow LJ (2000) Activation of mesolimbic dopamine function by phencyclidine is enhanced by 5-HT2C/2B receptor antagonists: neurochemical and behavioural studies. Neuropharmacology 39:2318–2328
Ichikawa J, Meltzer HY (1999) Relationship between dopaminergic and serotonergic neuronal activity in the frontal cortex and the action of typical and atypical antipsychotic drugs. Eur Arch Psychiatry Clin Neurosci 249:S90–S98
Idris NF, Repeto P, Neill JC, Large CH (2005) Investigation of the effects of lamotrigine and clozapine in improving reversal-learning impairments induced by acute phencyclidine and D-amphetamine in the rat. Psychopharmacology (Berl) 179:336–348
Javitt DC, Balla A, Sershen H, Lajtha A (1999) Reversal of phencyclidine-induced effects by glycine and glycine transport inhibitors. Biol Psychiatry 45:668–679
Jenkins BG, Chen Y-CI, Mandeville JB (2003) Pharmacological magnetic resonance imaging (phMRI). In: van Bruggen N, Roberts T (eds) Biomedical imaging in experimental neuroscience. CRC, New York, pp 155–209
Kapur S, Seeman P (2002) NMDA receptor antagonists ketamine and PCP have direct effects on the dopamine D(2) and serotonin 5-HT(2)receptors-implications for models of schizophrenia. Mol Psychiatry 7:837–844
Kehne JH, Baron BM, Carr AA, Chaney SF, Elands J, Feldman DJ, Frank RA, van Giersbergen PL, McCloskey TC, Johnson MP, McCarty DR, Poirot M, Senyah Y, Siegel BW, Widmaier C (1996) Preclinical characterization of the potential of the putative atypical antipsychotic MDL 100, 907 as a potent 5-HT2A antagonist with a favorable CNS safety profile. J Pharmacol Exp Ther 277:968–981
Knauer CS, Campbell JE, Galvan B, Bowman C, Osgood S, Buist S, Buchholz L, Henry B, Wong EHF, Shahid M, Grimwood S (2008) Validation of a rat in vivo [3H]M100907 binding assay to determine a translatable measure of 5-HT2A receptor occupancy. Eur J Pharmacol 591:136–141
Knutson B, Gibbs S (2007) Linking nucleus accumbens dopamine and blood oxygenation. Psychopharmacology 191:813–822
Kristiansen LV, Huerta I, Beneyto M, Meador-Woodruff JH (2007) NMDA receptors and schizophrenia. Curr Opin Pharmacol 7:48–55
Krystal JH, D’Souza DC, Karper LP, Bennett A, Abi-Dargham A, Abi-Saab D, Cassello K, Bowers MB Jr, Vegso S, Heninger GR, Charney DS (1999) Interactive effects of subanesthetic ketamine and haloperidol in healthy humans. Psychopharmacology (Berl) 145:193–204
Krystal JH, Anand A, Moghaddam B (2002) Effects of NMDA receptor antagonists: implications for the pathophysiology of schizophrenia. Arch Gen Psychiatry 59:663–664
Krystal JH, D’Souza DC, Mathalon D, Perry E, Belger A, Hoffman R (2003) NMDA receptor antagonist effects, cortical glutamatergic function, and schizophrenia: toward a paradigm shift in medication development. Psychopharmacology (Berl) 169:215–233
Kuroki T, Meltzer HY, Ichikawa J (1999) Effects of antipsychotic drugs on extracellular dopamine levels in rat medial prefrontal cortex and nucleus accumbens. J Pharmacol Exp Ther 288:774–781
Langsjo JW, Kaisti KK, Aalto S, Hinkka S, Aantaa R, Oikonen V, Sipila H, Kurki T, Silvanto M, Scheinin H (2003) Effects of subanesthetic doses of ketamine on regional cerebral blood flow, oxygen consumption, and blood volume in humans. Anesthesiology 99:614–623
Large CH (2007) Do NMDA receptor antagonist models of schizophrenia predict the clinical efficacy of antipsychotic drugs? J Psychopharmacol 21:283–301
Lehmann J, Schneider J, McPherson S, Murphy DE, Bernard P, Tsai C, Bennett DA, Pastor G, Steel DJ, Boehm C (1987) CPP, a selective N-methyl-D-aspartate (NMDA)-type receptor antagonist: characterization in vitro and in vivo. J Pharmacol Exp Ther 240:737–746
Liddle PF, Lane CJ, Ngan E (2000) Immediate effects of risperidone on cortico-striato-thalamic loops and the hippocampus. Br J Psychiatry 177:402–407
Linn S, Negi S, Gerum V, Javitt C (2003) Reversal of phencyclidine-induced prepulse inhibition deficits by clozapine in monkeys. Psychopharmacology V169:234–239
Littlewood CL, Jones N, O’Neil MJ, Mitchell SN, Tricklebank M, Williams MS (2006) Mapping the central effects of ketamine in the rat using pharmacological MRI. Psychopharmacology V186:64–81
Liu W, Alreja M (1997) Atypical antipsychotics block the excitatory effects of serotonin in septohippocampal neurons in the rat. Neuroscience 79:369–382
Luttgen M, Ove Ígren S, Br M (2004) Chemical identity of 5-HT2A receptor immunoreactive neurons of the rat septal complex and dorsal hippocampus. Brain Res 1010:156–165
Malhotra AK, Pinals DA, Adler CM, Elman I, Clifton A, Pickar D, Breier A (1997) Ketamine-induced exacerbation of psychotic symptoms and cognitive impairment in neuroleptic-free schizophrenics. Neuropsychopharmacology 17:141–150
Mandeville JB, Marota JJA, Kosofsky BE, Keltner JR, Weissleder R, Rosen B, Weisskoff R (1998) Dynamic functional imaging of relative cerebral blood volume during rat forepaw stimulation. Magn Reson Med 39:615–624
Marder SR (1999) Limitations of dopamine-D2 antagonists and the search for novel antipsychotic strategies. Neuropsychopharmacology 21:S117–S121
Marquis KL, Sabb AL, Logue SF, Brennan JA, Piesla MJ, Comery TA, Grauer SM, Ashby CR Jr, Nguyen HQ, Dawson LA, Barrett JE, Stack G, Meltzer HY, Harrison BL, Rosenzweig-Lipson S (2007) WAY-163909 [(7bR, 10aR)-1, 2, 3, 4, 8, 9, 10, 10a-octahydro-7bH-cyclopenta-[b][1, 4]diazepino[6, 7, 1hi]indole]: a novel 5-hydroxytryptamine 2C receptor-selective agonist with preclinical antipsychotic-like activity. J Pharmacol Exp Ther 320:486–496
Martin-Ruiz R, Puig MV, Celada P, Shapiro DA, Roth BL, Mengod G, Artigas F (2001) Control of serotonergic function in medial prefrontal cortex by serotonin-2A receptors through a glutamate-dependent mechanism. J Neurosci 21:9856–9866
Medoff DR, Holcomb HH, Lahti AC, Tamminga CA (2001) Probing the human hippocampus using rCBF: contrasts in schizophrenia. Hippocampus 11:543–550
Meltzer HY (1996) Pre-clinical pharmacology of atypical antipsychotic drugs: a selective review. Br J Psychiatry 168(Suppl 29):23–31
Meltzer HY, Matsubara S, Lee JC (1989) Classification of typical and atypical antipsychotic drugs on the basis of dopamine D-1, D-2 and serotonin2 pKi values. J Pharmacol Exp Ther 251:238–246
Meltzer HY, Li Z, Kaneda Y, Ichikawa J (2003) Serotonin receptors: their key role in drugs to treat schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 27:1159–1172
Meltzer HY, Arvanitis L, Bauer D, Rein W (2004) Placebo-controlled evaluation of four novel compounds for the treatment of schizophrenia and schizoaffective disorder. Am J Psychiatry 161:975–984
Mirjana C, Baviera M, Invernizzi RW, Balducci C (2004) The serotonin 5-HT2A receptors antagonist M100907 prevents impairment in attentional performance by NMDA receptor blockade in the rat prefrontal cortex. Neuropsychopharmacology 29:1637–1647
Moghaddam B, Adams B, Verma A, Daly D (1997) Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience 17:2921–2927
Molloy AG, Waddington JL (1984) Dopaminergic behaviour stereospecifically promoted by the D1 agonist R-SK & F 38393 and selectively blocked by the D1 antagonist SCH 23390. Psychopharmacology 82:409–410
Neisewander JL, Fuchs RA, O’Dell LE, Khroyan TV (1998) Effects of SCH-23390 on dopamine D1 receptor occupancy and locomotion produced by intraaccumbens cocaine infusion. Synapse 30:194–204
Ngan ETC, Lane CJ, Ruth TJ, Liddle PF (2002) Immediate and delayed effects of risperidone on cerebral metabolism in neuroleptic naive schizophrenic patients: correlations with symptom change. J Neurol Neurosurg Psychiatry 72:106–110
O’Neill MF, Heron-Maxwell CL, Shaw G (1999) 5-HT2 receptor antagonism reduces hyperactivity induced by amphetamine, cocaine, and MK-801 but not D1 agonist C-APB. Pharmacol Biochem Behav 63:237–243
Palfreyman MG, Schmidt CJ, Sorensen SM, Dudley MW, Kehne JH, Moser P, Gittos MW, Carr AA (1993) Electrophysiological, biochemical and behavioral evidence for 5-HT2 and 5-HT3 mediated control of dopaminergic function. Psychopharmacology (Berl) 112:S60–S67
Parellada E, Catafau AM, Bernardo M, Lomena F, Gonzalez-Monclus E, Setoain J (1994) Prefrontal dysfunction in young acute neuroleptic-naive schizophrenic patients: a resting and activation SPECT study. Psychiatry Res 55:131–139
Paxinos G, Watson C (1998) The rat brain in stereotactic coordinates. Academic, San Diego
Peroutka SJ, U’Prichard DC, Greenberg DA, Snyder SH (1977) Neuroleptic drug interactions with norepinephrine alpha receptor binding sites in rat brain. Neuropharmacology 16:549–556
Piguet P, Galvan M (1994) Transient and long-lasting actions of 5-HT on rat dentate gyrus neurones in vitro. J Physiol 481(Pt 3):629–639
Poyurovsky M, Koren D, Gonopolsky I, Schneidman M, Fuchs C, Weizman A, Weizman R (2003) Effect of the 5-HT2 antagonist mianserin on cognitive dysfunction in chronic schizophrenia patients: an add-on, double-blind placebo-controlled study. Eur Neuropsychopharmacol 13:123–128
Proksch JW, Gentry WB, Owens SM (2000) The effect of rate of drug administration on the extent and time course of phencyclidine distribution in rat brain, testis, and serum. Drug Metab Dispos 28:742–747
Robbins TW (2005) Chemistry of the mind: neurochemical modulation of prefrontal cortical function. J Comp Neurol 493:140–146
Rodefer JS, Nguyen TN, Karlsson JJ, Arnt J (2008) Reversal of subchronic PCP-induced deficits in attentional set shifting in rats by sertindole and a 5-HT6 receptor antagonist: comparison among antipsychotics. Neuropsychopharmacology 33:2657–2666
Roth BL, Hanizavareh SM, Blum AE (2004) Serotonin receptors represent highly favorable molecular targets for cognitive enhancement in schizophrenia and other disorders. Psychopharmacology 174:17–24
Schmidt CJ, Fadayel GM (1995) The selective 5-HT2A receptor antagonist, MDL 100, 907, increases dopamine efflux in the prefrontal cortex of the rat. Eur J Pharmacol 273:273–279
Schreiber R, Brocco M, de Lefebvre LB, Monneyron S, Millan MJ (1995) A drug discrimination analysis of the actions of novel serotonin1A receptor ligands in the rat using the 5-HT1A receptor agonist, 8-hydroxy-2-(di-n-propylamino)tetralin. J Pharmacol Exp Ther 275:822–831
Schwarz AJ, Reese T, Gozzi A, Bifone A (2003) Functional MRI using intravascular contrast agents: detrending of the relative cerebrovascular (rCBV) time course. Magn Reson Imaging 21:1191–1200
Schwarz AJ, Zocchi A, Reese T, Gozzi A, Varnier G, Girlanda E, Biscaro B, Bertani S, Crestan V, Heidbreder CA, Bifone A (2004) The relationship between local dopamine changes and phMRI response to acute cocaine challenge in the rat revealed by concurrent in situ microdialysis. In: Book of abstracts: Twelfth Annual Meeting of the International Society of Magnetic Resonance in Medicine 12
Schwarz AJ, Danckaert A, Reese T, Gozzi A, Paxinos G, Watson C, Merlo-Pich EV, Bifone A (2006a) A stereotaxic MRI template set for the rat brain with tissue class distribution maps and co-registered anatomical atlas: application to pharmacological MRI. NeuroImage 32:538–550
Schwarz AJ, Whitcher B, Gozzi A, Reese T, Bifone A (2006b) Study-level wavelet cluster analysis and data-driven signal models in pharmacological MRI. J Neurosci Methods 159:346–360
Schwarz AJ, Gozzi A, Reese T, Heidbreder CA, Bifone A (2007) Pharmacological modulation of functional connectivity: the correlation structure underlying the phMRI response to d-amphetamine modified by selective dopamine D3receptor antagonist SB277011A. Magn Reson Imag 25:811–820
Scott DO, Heath TG (1998) Investigation of the CNS penetration of a potent 5-HT2a receptor antagonist (MDL 100, 907) and an active metabolite (MDL 105, 725) using in vivo microdialysis sampling in the rat. J Pharm Biomed Anal 17:17–25
Scruggs JL, Patel S, Bubser M, Deutch AY (2000) DOI-induced activation of the cortex: dependence on 5-HT2A heteroceptors on thalamocortical glutamatergic neurons. J Neurosci 20:8846–8852
Scruggs JL, Schmidt D, Deutch AY (2003) The hallucinogen 1-[2, 5-dimethoxy-4-iodophenyl]-2-aminopropane (DOI) increases cortical extracellular glutamate levels in rats. Neurosci Lett 346:137–140
Seeman P (2002) Atypical antipsychotics: mechanism of action. Can J Psychiatry 47:27–38
Seeman P, Kapur S (2003) Anesthetics inhibit high-affinity states of dopamine D2 and other G-linked receptors. Synapse 50:35–40
Shen RY, Andrade R (1998) 5-Hydroxytryptamine2 receptor facilitates GABAergic neurotransmission in rat hippocampus. J Pharmacol Exp Ther 285:805–812
Silbersweig DA, Stern E, Frith C, Cahill C, Holmes A, Grootoonk S, Seaward J, McKenna P, Chua SE, Schnorr L (1995) A functional neuroanatomy of hallucinations in schizophrenia. Nature 378:176–179
Sorensen SM, Kehne JH, Fadayel GM, Humphreys TM, Ketteler HJ, Sullivan CK, Taylor VL, Schmidt CJ (1993) Characterization of the 5-HT2 receptor antagonist MDL 100907 as a putative atypical antipsychotic: behavioral, electrophysiological and neurochemical studies. J Pharmacol Exp Ther 266:684–691
Soyka M, Koch W, Möller H, Rüther T, Tatsch K (2005) Hypermetabolic pattern in frontal cortex and other brain regions in unmedicated schizophrenia patients. Eur Arch Psychiatry Clin Neurosci 255:308–312
Tandon R, Fleischhacker W (2005) Comparative efficacy of antipsychotics in the treatment of schizophrenia: a critical assessment. Schizophr Res 79:145–155
Varty GB, Bakshi VP, Geyer MA (1999) M100907, a serotonin 5-HT2A receptor antagonist and putative antipsychotic, blocks dizocilpine-induced prepulse inhibition deficits in Sprague–Dawley and Wistar rats. Neuropsychopharmacology 20:311–321
Volkow ND, Brodie JD, Wolf AP, Angrist B, Russell J, Cancro R (1986) Brain metabolism in patients with schizophrenia before and after acute neuroleptic administration. J Neurol Neurosurg Psychiatry 49:1199–1202
Wadenberg M-L (1992) Antagonism by 8-OH-DPAT, but not ritanserin, of catalepsy induced by SCH 23390 in the rat. J Neural Transm 89:49–59
Weissman AD, Dam M, London ED (1987) Alterations in local cerebral glucose utilization induced by phencyclidine. Brain Res 435:29–40
Whitcher B, Schwarz AJ, Barjat H, Smart SC, Grundy RI, James MF (2005) Wavelet-based cluster analysis: data-driven grouping of voxel time courses with application to perfusion-weighted and pharmacological MRI of the rat brain. Neuroimage 24:281–295
Winstanley CA, Chudasama Y, Dalley JW, Theobald DEH, Glennon JC, Robbins TW (2003) Intra-prefrontal 8-OH-DPAT and M100907 improve visuospatial attention and decrease impulsivity on the five-choice serial reaction time task in rats. Psychopharmacology 167:304–314
Winter JC, Eckler JR, Rabin RA (2004) Serotonergic/glutamatergic interactions: the effects of mGlu2/3 receptor ligands in rats trained with LSD and PCP as discriminative stimuli. Psychopharmacology (Berl) 172:233–240
Wolf ME, Xue CJ (1999) Amphetamine-induced glutamate efflux in the rat ventral tegmental area is prevented by MK-801, SCH 23390, and ibotenic acid lesions of the prefrontal cortex. J Neurochem 73:1529–1538
Wood MD, Reavill C, Trail B, Wilson A, Stean T, Kennett GA, Lightowler S, Blackburn TP, Thomas D, Gager TL, Riley G, Holland V, Bromidge SM, Forbes IT, Middlemiss DN (2001) SB-243213; a selective 5-HT2C receptor inverse agonist with improved anxiolytic profile: lack of tolerance and withdrawal anxiety. Neuropharmacology 41:186–199
Worsley KJ, Evans AC, Marrett S, Neelin P (1992) A three-dimensional statistical analysis for CBF activation studies in human brain. J Cereb Blood Flow Metab 12:900–918
Zaharchuk G, Mandeville JB, Bogdanov AA Jr, Weissleder R, Rosen BR, Marota JJ (1999) Cerebrovascular dynamics of autoregulation and hypoperfusion. An MRI study of CBF and changes in total and microvascular cerebral blood volume during hemorrhagic hypotension. Stroke 30:2197–2204
Zahrt J, Taylor JR, Mathew RG, Arnsten AF (1997) Supranormal stimulation of D1 dopamine receptors in the rodent prefrontal cortex impairs spatial working memory performance. J Neurosci 17:8528–8535
Zaniewska M, McCreary AC, Przegalinski E, Filip M (2007) Effects of the serotonin 5-HT2A and 5-HT2C receptor ligands on the discriminative stimulus effects of nicotine in rats. Eur J Pharmacol 571:156–165
Zhai Y, George CA, Zhai J, Nisenbaum ES, Johnson MP, Nisenbaum LK (2002) Group II metabotropic glutamate receptor modulation of DOI-induced c-fos mRNA and excitatory responses in the cerebral cortex. Neuropsychopharmacology 28:45–52
Acknowledgements
The author would like to thank Dr. Mauro Corsi for critically reviewing the manuscript.
Disclosure/conflict of interest
The author(s) declare that, except for income received from my primary employer, no financial support or compensation has been received from any individual or corporate entity over the past 3 years for research or professional service and there are no personal financial holdings that could be perceived as constituting a potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
All in vivo studies were conducted in accordance with the Italian laws (DL 116, 1992 Ministero della Sanità, Roma). Animal research protocols were also reviewed and consented to by the GSK animal care committee, in accordance with the guidelines of the Principles of Laboratory Animal Care (NIH publication 86-23, revised 1985).
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 394kb)
Rights and permissions
About this article
Cite this article
Gozzi, A., Crestan, V., Turrini, G. et al. Antagonism at serotonin 5-HT2A receptors modulates functional activity of frontohippocampal circuit. Psychopharmacology 209, 37–50 (2010). https://doi.org/10.1007/s00213-009-1772-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-009-1772-4