Abstract
Rationale
Quetiapine, an atypical neuroleptic, has beneficial antipsychotic effects in schizophrenic patients, but with a lower incidence of extrapyramidal symptoms (EPS) compared with typical antipsychotics. While typical antipsychotics are often switched to atypical agents when adverse effects become limiting, there is little preclinical information to support this strategy, both in terms of efficacy and side effects.
Objectives
The antipsychotic effects and EPS during concomitant administration of quetiapine with haloperidol, a typical antipsychotic agent, were evaluated in mice and compared with chlorpromazine and risperidone.
Methods
We first investigated the antipsychotic effects and EPS liability of quetiapine, risperidone, chlorpromazine, and haloperidol when administered alone to select optimal doses for subsequent combination studies. The second study was designed to evaluate the antipsychotic efficacy and EPS profile of concomitant administration of quetiapine, risperidone, or chlorpromazine with haloperidol. Antipsychotic effects were evaluated with the methamphetamine-induced hyperlocomotion test, and EPS liability was evaluated in a catalepsy-induction model.
Results
Quetiapine, risperidone, chlorpromazine, and haloperidol dose-dependently reduced methamphetamine-induced hyperlocomotion, with ED50 values of 5.6, 0.020, 1.8, 0.035 mg/kg, respectively. In the catalepsy test, quetiapine only weakly induced catalepsy at the highest dose of 100 mg/kg, whereas risperidone, chlorpromazine, and haloperidol dose-dependently induced catalepsy with ED50 values of 0.25, 4.6, and 0.10 mg/kg, respectively. While the combination of quetiapine (6 mg/kg) and haloperidol (0.04 mg/kg) significantly reduced methamphetamine-induced hyperlocomotion in comparison with haloperidol alone, quetiapine (10, 32 mg/kg) plus haloperidol did not potentiate the cataleptogenic activity of haloperidol. In contrast, risperidone (0.1, 0.32 mg/kg) or chlorpromazine (3.2 mg/kg) significantly augmented catalepsy induced by haloperidol. Catalepsy induced by co-administration of quetiapine (10 mg/kg) and haloperidol (0.1 mg/kg) was significantly potentiated by WAY100635, a 5-HT1A antagonist, and catalepsy induced by co-administration of risperidone (0.1 mg/kg) and haloperidol (0.1 mg/kg) was significantly antagonized by 8-OH-DPAT, a 5-HT1A agonist.
Conclusion
The present study demonstrated that the combined administration of quetiapine with haloperidol did not aggravate EPS, possibly because of its affinity for 5-HT1A receptors. This finding may have the clinical implication that quetiapine could provide a successful regimen in switching from typical antipsychotic agents in the symptom management of schizophrenia, or even in adjunctive therapy with other antipsychotic agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Quetiapine, a dibenzothiazepine derivative with atypical antipsychotic properties, effectively treats positive symptoms in schizophrenic patients with similar efficacy to typical antipsychotics such as haloperidol (Arvanitis et al. 1997), as well as demonstrating efficacy in treating negative symptoms and cognitive impairment in these patients (Purdon et al. 2001; Velligan et al. 2002). In addition, quetiapine shows a lower incidence of extrapyramidal symptoms (EPS) (Meats 1997) and other adverse events such as increases in serum prolactin levels, compared with typical antipsychotics (Hamner et al. 1996; Arvanitis et al. 1997; Peuskens and Link 1997; Copolov et al. 2000). In experimental animals, quetiapine only weakly induces catalepsy in rats and dystonic liability in haloperidol-sensitized monkeys, and only transiently elevates serum prolactin levels in rats (Migler et al. 1993; Saller and Salama 1993). Similarly, quetiapine alleviates negative symptoms in an animal model of schizophrenia (Guan et al. 2000). Quetiapine binds with higher affinity to α1-adrenergic and α2-adrenergic, histamine H1, 5-HT1A, and 5-HT2A receptors than to dopamine D2 receptors (Richelson and Souder 2000), which potentially contributes to its unique pharmacological actions.
Most antipsychotic drugs induce frequent EPS in schizophrenic patients, and they often require concomitant medication with anti-Parkinson’s agents. Furthermore, the presence of EPS is predictive of patients who will later exhibit tardive dyskinesia, an extremely serious side effect associated with long-term antipsychotic therapy (Casey 1999). Treatment with typical antipsychotics is often switched to atypical antipsychotics, such as quetiapine, when the typical agents produce intolerable adverse effects (Weiden et al. 1997; Kinon et al. 2000). In this regard, it is common clinical practice to switch to the new drug after first adding the atypical antipsychotic agent to prevent aggravation of psychotic symptoms. Recent clinical studies have suggested that switching to quetiapine is clinically beneficial for patients showing a poor response or intolerable side effects on their previous antipsychotic medications and does not exacerbate patients’ symptoms (Cutler et al. 2002; Nayer et al. 2003). In spite of accumulating clinical demands for such a switching strategy, however, there is limited preclinical information to support this combination strategy of atypical and typical antipsychotic agents, both in terms of efficacy and side effects.
The present study was designed to investigate the influence of combined administration of quetiapine with haloperidol in animal models of schizophrenia (Weiss and Kilts 1995): its antipsychotic efficacy (using a methamphetamine-induced hyperlocomotion model) and side-effect profile (using a mouse catalepsy model). We also tested a second atypical antipsychotic agent, risperidone, and a typical antipsychotic agent, chlorpromazine, in the same experimental paradigms. Finally, we expanded our study to clarify the possible mechanism by which atypical antipsychotic agents interact with a typical agent to alter their propensity of inducing extrapyramidal side effects in the light of the possible involvement of 5-HT1A receptors, one of the putative mechanisms contributing to the unique features of atypical antipsychotic drugs including quetiapine (Bantick et al. 2001).
Materials and methods
Animals
Adult male ddY mice were purchased from Japan SLC Co. Ltd (Hikisa, Shizuoka, Japan) at the age of 6 weeks old and were used at 7 weeks old. They were housed in groups of eight to nine in polycarbonate cages with clean paper tips as bedding, under controlled conditions of light (12 h light–dark cycle, light on at 7:00 a.m.) and temperature (23±1°C). Mice had free access to water and food throughout the experiment. All animal experimental procedures were performed under the guidelines of the Animal Experiment Committee of Fujisawa Pharmaceutical Co. Ltd.
Methamphetamine-induced hyperlocomotion
Mice were placed in the experimental chamber (L30×W36×H17 cm) 30 min after injection of methamphetamine (1 mg/kg, IP) and locomotor activity was immediately recorded for 30 min using ANIMEX AUTO (MK-110; Muromachi Kikai Co. Ltd, Tokyo, Japan).
Catalepsy
The mouse’s forepaws were placed on a horizontal steel bar (diameter 0.3 cm), elevated 3 cm above the tabletop, and the duration of cataleptic time was recorded for up to 30 s. If the catalepsy time was 30 s in at least one trial out of two, it was regarded as the drug-induced catalepsy and scored as “+”, otherwise it was scored as “−”. The incidence of catalepsy was expressed as the percentage of mice scored as “+” in the total mouse group.
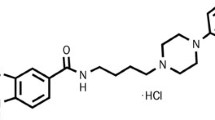
Drugs
Quetiapine was provided from AstraZeneca (Cheshire, UK). Risperidone was synthesized at Fujisawa Pharmaceutical Co. Ltd (Osaka, Japan). Chlorpromazine, WAY100635, and 8-OH-DPAT were purchased from Sigma-Aldrich Co. (St Louis, Mo., USA). Haloperidol and methamphetamine were purchased from Dainippon Pharmaceutical (Osaka, Japan). Quetiapine was suspended in 0.5% methylcellulose, and risperidone and haloperidol were dissolved in saline. Chlorpromazine, WAY100635, and 8-OH-DPAT were dissolved in distilled water. All drugs were freshly prepared and administered in a volume of 10 ml/kg. Quetiapine, risperidone, and chlorpromazine were administered orally 1 h before the measurement. Haloperidol, WAY100635, and 8-OH-DPAT were injected intraperitoneally 30 min before the measurement.
Data analysis
In methamphetamine-induced hyperlocomotion, the data are expressed as mean±SEM. Statistical analysis for the changes in locomotor activity between groups was made using Student’s t-test (for vehicle-treated normal versus methamphetamine control) and one-way ANOVA followed by Dunnett’s multiple comparisons (for multiple drug-treated groups). ED50 value was calculated from linear regression analysis. Statistically significant changes in the incidence of catalepsy were calculated using Chi-square test (for comparison of two groups) and Dunnett’s multiple comparison test (for multiple groups). The ED50 value was calculated using linear regression analysis.
Results
Effect of quetiapine, risperidone, chlorpromazine, or haloperidol alone
In the first study, we investigated the antipsychotic effects and EPS liability of quetiapine, risperidone, chlorpromazine, or haloperidol alone in an attempt to compare the spectrum of each drug and to provide rationale for choosing optimal doses for subsequent combination studies.
Methamphetamine-induced hyperlocomotion
Methamphetamine treatment (0.1, 0.32, 1, 3.2 mg/kg, IP) dose-dependently increased locomotor activity (data not shown). Hyperlocomotion induced by methamphetamine (1 mg/kg) was dose-dependently reduced by single injections of quetiapine, risperidone, chlorpromazine, or haloperidol, with ED50 values of 5.6, 0.020, 1.8, 0.035 mg/kg, respectively (Table 1).
Catalepsy
Risperidone, chlorpromazine, and haloperidol dose-dependently induced catalepsy at low doses (Table 1), whereas quetiapine only minimally induced catalepsy at only the highest dose (100 mg/kg). ED50 values of quetiapine, risperidone, chlorpromazine, and haloperidol were 95, 0.25, 4.6, and 0.10 mg/kg, respectively (Table 1). The therapeutic index of each compound was calculated using ED50 values for inhibiting methamphetamine-induced hyperlocomotion versus those of eliciting catalepsy: quetiapine and risperidone showed wider therapeutic windows than did chlorpromazine and haloperidol (Table 1).
Effect of combined administration of quetiapine, risperidone or chlorpromazine with haloperidol
The second study was designed to determine the antipsychotic efficacy and side-effect profile of concomitant administration of quetiapine, risperidone, or chlorpromazine with haloperidol.
Methamphetamine-induced hyperlocomotion
Doses of quetiapine, risperidone, chlorpromazine, and haloperidol were administered at their ED50 values for inhibiting methamphetamine-induced hyperlocomotion when used alone (Table 1): 6 mg/kg for quetiapine, 0.02 mg/kg for risperidone, 2 mg/kg for chlorpromazine, and 0.04 mg/kg for haloperidol. Both the combination of quetiapine and haloperidol and the combination of chlorpromazine and haloperidol significantly reduced methamphetamine-induced hyperlocomotion compared with haloperidol alone (Fig. 1). Risperidone plus haloperidol similarly protected methamphetamine-induced hyperlocomotion compared with the risperidone-alone group (Fig. 1).
Effects of concomitant administration of quetiapine (QTP), risperidone (RIS) or chlorpromazine (CPZ), and haloperidol (HPD) on methamphetamine-induced hyperlocomotion in mice. Each column represents the average counts of locomotor activity±SEM measured for 30 min using the Animex system. Dosage of each drug used was based on the ED50 value for each compound determined in the first study (Table 1); quetiapine 6 mg/kg, risperidone 0.02 mg/kg, chlorpromazine 2 mg/kg, haloperidol 0.04 mg/kg. Methamphetamine (1 mg/kg) was intraperitoneally administered 30 min before measurement. Quetiapine, risperidone, and chlorpromazine were orally administered 1 h before measurement, and haloperidol was intraperitoneally administered 30 min before the measurement. Number of animals was 15 for each treatment group. ## P<0.01, statistically significant compared with vehicle-treated group (by Student’s t-test). **P<0.01, statistically significant compared with methamphetamine-alone group (by ANOVA followed by Dunnett’s multiple comparison test). *P<0.05 statistically significant compared with haloperidol alone group (by ANOVA followed by Dunnett’s multiple comparison test). ‡ P<0.01, statistically significant compared risperidone-alone group (by Student’s t-test)
Catalepsy
Quetiapine (10 and 32 mg/kg) plus haloperidol (0.032, 0.1, and 0.32 mg/kg) did not enhance the cataleptogenic effects of haloperidol (Fig. 2). Furthermore, the combination of quetiapine (100 mg/kg) and haloperidol did not affect the incidence of catalepsy compared with haloperidol alone. In contrast, the combination of risperidone (0.1 mg/kg) and haloperidol (0.1 mg/kg) markedly augmented haloperidol-induced catalepsy (Fig. 3). Risperidone (0.32 mg/kg) also enhanced the catalepsy induced by combination with haloperidol (0.032 and 0.1 mg/kg). Similarly, the combination of chlorpromazine (3.2 mg/kg) and haloperidol (0.1 mg/kg) showed greater cataleptic effects than haloperidol alone (Fig. 4).
Effect of quetiapine on haloperidol-induced catalepsy in mice. Each column represents the incidence of catalepsy. Quetiapine (10, 32, 100 mg/kg) was orally administered 1 h before measurement, and haloperidol (0.032, 0.1, 0.32 mg/kg) was intraperitoneally administered 30 min before measurement. Number of animals was 20 for each treatment group. **P<0.01, statistically significant compared with quetiapine 0 mg/kg treated group in each haloperidol treated group (by Dunnett’s multiple comparison test)
Effect of risperidone on haloperidol-induced catalepsy in mice. Each column represents the incidence of catalepsy. Risperidone (0.1, 0.32, 1 mg/kg) was orally administered 1 h before measurement, and haloperidol (0.032, 0.1, 0.32 mg/kg) was intraperitoneally administered 30 min before the measurement. Number of animals was 20 for each treatment group. *P<0.05, **P<0.01, statistically significant compared with risperidone 0 mg/kg treated group in each haloperidol treated group (by Dunnett’s multiple comparison test)
Effect of chlorpromazine on haloperidol-induced catalepsy in mice. Each column represents the incidence of catalepsy. Chlorpromazine (1, 3.2, 10 mg/kg) was orally administered 1 h before measurement, and haloperidol (0.032, 0.1, 0.32 mg/kg) was intraperitoneally administered 30 min before measurement. Number of animals was 20 for each treatment group. **P<0.01, statistically significant compared with chlorpromazine 0 mg/kg treated group in each haloperidol treated group (by Dunnett’s multiple comparison test)
Involvement of 5-HT1A receptors in catalepsy produced by combining either quetiapine or risperidone with haloperidol
We next wanted to clarify the role of 5-HT1A receptors in the mechanism by which risperidone, but not quetiapine, augmented haloperidol-induced catalepsy. WAY100635, a 5-HT1A antagonist, was investigated for its effects on the catalepsy observed following co-administration of quetiapine and haloperidol. In accordance with our previous results (see Fig. 2), co-administration of quetiapine (10 mg/kg) and haloperidol (0.1 mg/kg) significantly induced catalepsy, but this was exactly comparable with that produced by haloperidol alone and quetiapine did not enhance the catalepsy by haloperidol. Co-administration of WAY100635 (0.1 and 1 mg/kg) with quetiapine and haloperidol dose-dependently enhanced the catalepsy, with statistical significance at 1 mg/kg (Fig. 5). WAY100635 had no effects on the catalepsy induced by haloperidol alone at the doses used here (Fig. 5), and did not produce any cataleptic behaviors when administered alone (data not shown).
Effect of treatment with WAY100635 on catalepsy induced by co-administration of quetiapine and haloperidol in mice. Each column represents the incidence of catalepsy. Quetiapine (10 mg/kg) was orally administered 1 h before measurement, and haloperidol (0.1 mg/kg) and WAY100635 (0.1, 1 mg/kg) was intraperitoneally administered 30 min before the measurement. Number of animals was 18 for each treatment group. ## P<0.01, statistically significant compared with quetiapine-alone group (by Chi-square test). **P<0.01, statistically significant compared with quetiapine plus haloperidol treated group (by Dunnett’s multiple comparison test)
We finally evaluated the effect of 8-OH-DPAT, a 5-HT1A agonist, on catalepsy enhanced by co-administration of risperidone and haloperidol. As with the previous experiment (Fig. 3), catalepsy induced by haloperidol (0.1 mg/kg) was significantly aggravated by risperidone (0.1 mg/kg). The enhanced catalepsy induced by co-administration of risperidone and haloperidol was significantly antagonized dose-dependently by 8-OH-DPAT (0.001 and 0.01 mg/kg; Fig. 6). 8-OH-DPAT had no significant effects on haloperidol-induced catalepsy (Fig. 6), and 8-OH-DPAT alone had no effect in this catalepsy model (data not shown).
Effect of 8-OH-DPAT on co-administration of risperidone and haloperidol on catalepsy in mice. Each column represents the incidence of catalepsy. Risperidone (0.1 mg/kg) was orally administered 1 h before measurement, and haloperidol (0.1 mg/kg) and 8-OH-DPAT (0.001, 0.01 mg/kg) was intraperitoneally administered 30 min before measurement. Number of animals was 18 for each treatment group. ## P<0.01, statistically significant compared with risperidone-alone group (by Chi-square test). ‡ P<0.01, statistically significant compared with haloperidol alone group (by Chi-square test). **P<0.01, statistically significant compared with risperidone plus haloperidol treated group (by Dunnett’s multiple comparison test)
Discussion
In the present study, quetiapine was evaluated for its ability to potentiate the antipsychotic effects and EPS of haloperidol, and it was compared with two other antipsychotic agents, risperidone, and chlorpromazine. In the first study, which evaluated the antipsychotic effects and EPS liability of each drug when treated alone, most agents significantly inhibited methamphetamine-induced hypermotility, a model of antipsychotic efficacy, and induced catalepsy, a predictive measure of EPS (Weiss and Kilts 1995), at similar doses. However, in the case of quetiapine, the dose that produced antipsychotic effects (10 mg/kg) was much lower than the dose required to weakly induce catalepsy (100 mg/kg). Based on the ratio between ED50 values for inhibiting methamphetamine-induced hyper-locomotor activity and ED50 values for producing catalepsy, quetiapine and risperidone behaved as atypical antipsychotic agents with higher therapeutic indices compared with those of typical antipsychotic drugs such as chlorpromazine and haloperidol. The results are in accordance with previous observations by others in animal models (Migler et al. 1993) and also in clinical studies showing that atypical antipsychotic agents show wider margins in comparison with typical antipsychotic agents (Jibson and Tandon 1998). Therefore, these results suggest that these mice models used here mirror the clinical observations in terms of their sensitivity in distinguishing the profile of atypical from typical antipsychotic agents.
Quetiapine, risperidone, and chlorpromazine were evaluated for their antipsychotic effects in combination with haloperidol in a methamphetamine-induced hyperlocomotion model. The combination of quetiapine and haloperidol significantly inhibited methamphetamine-induced hyperlocomotion compared with haloperidol alone, and both risperidone and chlorpromazine similarly enhanced haloperidol-induced inhibition of methamphetamine-induced hyperlocomotion. This enhancement of haloperidol activity putatively occurred via a common mechanism, since the inhibitory activity of these drugs were additive (not synergistic) and there were no meaningful differences in the magnitude of the protection by any of three drugs combined with haloperidol. Alternatively, a ceiling effect of inhibition in the drug combinations might mask further changes even if quetiapine, risperidone, and chlorpromazine interacted with haloperidol through different modes of action.
The most important finding in the present study is that quetiapine did not enhance haloperidol-induced catalepsy, suggesting that quetiapine and haloperidol differentially modulate the neuronal systems responsible for expression of antipsychotic activity and EPS. In contrast, risperidone and chlorpromazine significantly enhanced haloperidol-induced catalepsy, even with a suboptimal dose of haloperidol (0.1 mg/kg). Although quetiapine and risperidone are both classified as atypicals, it is conceivable that these compounds have different modes of actions. The lack of catalepsy potentiation by the combination of quetiapine with haloperidol might be consistent with recent clinical observation that patients with schizophrenia who switched from typical agents to quetiapine experienced improvements in symptoms as well as a reduction in EPS (Cutler et al. 2002; Nayer et al. 2003), and also supports the further clinical use of such combination (at least quetiapine plus haloperidol) in schizophrenic patients.
Atypical antipsychotic agents have binding affinities for many neurotransmitter receptors in the brain. Quetiapine reportedly has a low affinity for D2 receptors but instead has higher affinity for the 5-HT2A and 5-HT1A than D2 receptors (Richelson and Souder 2000). On the other hand, risperidone has higher affinity for 5-HT2A than D2 receptors, with low affinity for 5-HT1A receptors (Richelson and Souder 2000). It is also reported that quetiapine exhibits a partial agonist activity at the 5-HT1A receptor (Newman-Tancredi et al. 1998; Ichikawa et al. 2002). In contrast, risperidone is known to behave as a 5-HT1A antagonist at higher dosages (Newman-Tancredi et al. 1998). In the present study, we demonstrated that catalepsy induced by co-administration of quetiapine and haloperidol was dose-dependently enhanced by low doses of WAY100635, a 5-HT1A antagonist that did not alter haloperidol-induced catalepsy. This finding suggests that the 5-HT1A agonistic property of quetiapine contributes to its low liability for inducing EPS, and that a normally hidden propensity masked by 5-HT1A receptor agonism was reversed by WAY100635, consequently resulting in an apparent increase in EPS. In contrast, the fact that the enhanced catalepsy following co-administration of risperidone and haloperidol could be significantly inhibited by low dosages of 5-HT1A agonist 8-OH-DPAT that failed to affect haloperidol-induced catalepsy, indicates that risperidone’s property as a 5-HT1A receptor antagonist could partly contribute to a high incidence of EPS after concomitant administration with haloperidol.
The present study clearly highlights the difference in the action of quetiapine and risperidone, but the study does not per se clarify how this phenomenon is observed in combination with haloperidol, peculiar for quetiapine among diverse atypical antipsychotics. Biochemical and behavioral pharmacological tests in animals have proven that quetiapine resembles clozapine, another atypical antipsychotic agent, in the profiles sharing partial agonist activity at the 5-HT1A receptor (Meltzer et al. 1975; Casey 1989; Meltzer 1992). However, Ahlqvist et al. (2003) recently demonstrated that clozapine but not quetiapine or olanzapine blocked the catalepsy induced by dopamine antagonists, suggesting that clozapine has anticataleptic activity differing from quetiapine, possibly via other mechanisms rather than 5-HT1A receptor agonism. As their finding is not fully compatible with our study that focused on the possible potentiation of catalepsy, it would be fascinating to evaluate combination effects using other diverse antipsychotic drugs in our experimental paradigms.
Serotonergic drugs are known to modulate EPS associated with antipsychotics through the interaction between serotonin and dopamine in the substantia nigra and the striatum (Kapur and Remington 1996). The serotonergic pathway from the dorsal raphe (Fibiger and Miller 1977; Olpe and Koella 1977) projects directly to the substantia nigra, and inhibits the firing of the nigral dopaminergic neurons (Nedergaard et al. 1988). The raphe-nigral neurons arise as collateral of the raphe-striatal neurons, thus providing a neural basis for coordinated modulation of midbrain and terminal dopaminergic functions (Kooy and Hattori 1980). Therefore, inhibition of serotonin function (for instance; activation of somatodendritic 5-HT1A receptors in the nigra, or blockade of terminal 5-HT2A receptors in the striatum) is expected to disinhibit the dopamine system and decrease blockade of D2 receptors in the striatum, therefore inhibiting EPS (Kapur and Remington 1996). Thus, the 5-HT1A partial agonist activity of quetiapine might prevent enhancement of catalepsy when co-administrated with haloperidol. 5-HT1A partial agonists not only inhibit antipsychotic-induced EPS but also improve cognitive symptoms in schizophrenic patients and exert antidepressant and anxiolytic effects in humans (Millan 2000). Furthermore, biochemical studies using post-mortem schizophrenic brain have identified a reproducible elevation in 5-HT1A receptor density in the frontal cortex (Burnet et al. 1997). Therefore, it is tempting to speculate that the 5-HT1A partial agonist activity of quetiapine is involved, in part, in its therapeutic efficacy.
In conclusion, the present study provides compelling evidence that combined administration of quetiapine and haloperidol does not exacerbate EPS but still enhances the antipsychotic efficacy in animal models, suggesting that quetiapine could contribute to a successful regimen for switching from symptomatic management using typical antipsychotic agents, or adjunctive therapy with other antipsychotic agents.
References
Ahlqvist J, Isacson R, Wahlestedt C, Salmi P (2003) Anti-cataleptic effects of clozapine, but not olanzapine and quetiapine, on SCH 23390- or raclopride-induced catalepsy in rats. Eur Neuropsychopharmacol 13:177–182
Arvanitis LA, Miller BG, The Seroquel Trial 13 Study Group (1997) Multiple fixed doses of “Seroquel” (quetiapine) in patients with acute exacerbation of schizophrenia: a comparison with haloperidol and placebo. Biol Psychiatry 42:233–246
Bantick RA, Deakin JF, Grasby PM (2001) The 5-HT1A receptor in schizophrenia: a promising target for novel atypical neuroleptics? J Psychopharmacol 15:37–46
Burnet PW, Eastwood SL, Harrisson PJ (1997) [3H]WAY-100635 for 5-HT1A receptor autoradiography in human brain: a comparison with [3H]8-OH-DPAT and demonstration of increased binding in the frontal cortex in schizophrenia. Neurochem Int 30:565–574
Casey DE (1989) Clozapine: neuroleptic-induced EPS and tardive dyskinesia. Psychopharmacology 99:S47–S53
Casey DE (1999) Tardive dyskinesia and atypical antipsychotic drugs. Schizophr Res 35:S61–S66
Copolov DL, Link CGG, Kowalcyk B (2000) A multicentre, double-blind, randomized comparison of quetiapine (ICI 204,636, ‘Seroquel’) and haloperidol in schizophrenia. Psychol Med 30:95–105
Cutler AJ, Goldstein JM, Tumas JA (2002) Dosing and switching strategies for quetiapine fumarate. Clin Ther 24:209–222
De Nayer A, Windhager E, Irmansyam, Larmo I, Linderbauer B, Rittmannsberger H, Platz T, Jones AM, Whiteford JL, Altman CA, On behalf of the SPECTRUM study group (2003) Efficacy and tolerability of quetiapine in patients with schizophrenia switched from other antipsychotics. Int J Psychiatr Clin Pract 7:59–66
Fibiger HC, Miller JJ (1977) An anatomical and electrophysiological investigation of the serotonergic projection from the dorsal raphe nucleus to the substantia nigra in the rat. Neuroscience 2:975–987
Guan HJ, Dai J, Zhu XZ (2000) Atypical antipsychotic effects of quetiapine fumarate in animal models. Acta Pharmacol Sin 21:205–210
Hamner MB, Arvanitis LA, Miller BG, Link CGG, Hong WW (1996) Plasma prolactin in schizophrenia subjects treated with Seroquel (ICI204,636). Psychopharmacol Bull 32:107–110
Ichikawa J, Li Z, Dai J, Meltzer HY (2002) Atypical antipsychotic drugs, quetiapine, iloperidone, and melperone, preferentially increase dopamine and acetylcholine release in rat medial prefrontal cortex: role of 5-HT1A receptor agonism. Brain Res 956:349–357
Jibson MD, Tandon R (1998) New atypical antipsychotic medications. J Psychiatr Res 32:215–228
Kapur S, Remington G (1996) Serotonin-dopamine interaction and its relevance to schizophrenia. Am J Psychiatry 153:466–476
Kinon BJ, Basson BR, Gilmore JA, Malcolm S, Stauffer VL (2000) Strategies for switching from conventional antipsychotic drugs or risperidone to olanzapine. J Clin Psychiatry 61:833–840
Kooy DV, Hattori T (1980) Dorsal raphe cells with collateral projections to the caudate-putamen and substantia nigra: a fluorescent retrograde double labeling study in the rat. Brain Res 186:1–7
Meats P (1997) Quetiapine (‘Seroquel’); an effective and well-tolerated atypical antipsychotic. Int J Psychiatr Clin Pract 1:231–239
Meltzer HY (1992) The importance of serotonin-dopamine interactions in the action of clozapine. Br J Psychiatry 160:22–29
Meltzer HY, Daniels S, Fang VS (1975) Clozapine increases rat serum prolactin levels. Life Sci 17:339–342
Migler BM, Warawa EJ, Malick JB (1993) Seroquel: behavioral effects in conventional and novel tests for atypical antipsychotic drug. Psychopharmacology 112:299–307
Millan MJ (2000) Improving the treatment of schizophrenia: focus on serotonin (5-HT)1A receptors. J Pharmacol Exp Ther 295:853–861
Nedergaard S, Bolam JP, Greenfield SA (1988) Facilitation of a dendritic calcium conductance by 5-hydroxytryptamine in the substantia nigra. Nature 333:174–177
Newman-Tancredi A, Gavaudan S, Conte C, Chaput C, Touzard M, Verriele L, Audinot V, Millan MJ (1998) Agonist and antagonist actions of antipsychotic agents at 5-HT1A receptors: a [35S]GTPγS binding study. Eur J Pharmacol 355:245–256
Olpe HR, Koella WP (1977) The response of striatal cells upon stimulation of the dorsal and median raphe nuclei. Brain Res 122:357–360
Peuskens J, Link CGG (1997) A comparison of quetiapine and chlorpromazine in the treatment of schizophrenia. Acta Psychiatr Scand 96:265–273
Purdon SE, Malla A, Labelle A, Lit W (2001) Neuropsychological change in patients with schizophrenia after treatment with quetiapine or haloperidol. J Psychiatry Neurosci 26:137–149
Richelson E, Souder T (2000) Binding of antipsychotic drugs to human brain receptors. Focus on newer generation compounds. Life Sci 68:29–39
Saller CF, Salama AI (1993) Seroquel: biochemical profile of a potential atypical antipsychotic. Psychopharmacology 112:285–292
Velligan DI, Newcomer J, Pultz J, Csernansky J, Hoff AL, Mahurin R, Miller AL (2002) Does cognitive function improve with quetiapine in comparison to haloperidol? Schizophr Res 53:239–248
Weiden PJ, Aquila R, Dalheim L, Standard JM (1997) Switching antipsychotic medications. J Clin Psychiatry 58:63–72
Weiss JM, Kilts CD (1995) Animal models of depression and schizophrenia. In: Schatzberg AF, Nemeroff CB (eds) Textbook of psychopharmacology. American Psychiatric Association, USA, pp 81–123
Acknowledgements
The authors would like to thank Drs. Raymond D. Price (Fujisawa Pharmaceutical Co. Ltd) and Rod Sayce (AstraZeneca) for their helpful comments in preparing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tada, M., Shirakawa, K., Matsuoka, N. et al. Combined treatment of quetiapine with haloperidol in animal models of antipsychotic effect and extrapyramidal side effects: comparison with risperidone and chlorpromazine. Psychopharmacology 176, 94–100 (2004). https://doi.org/10.1007/s00213-004-1866-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-004-1866-y