Abstract
Epidemiological studies show that a positive correlation exists between the consumption of strongly heated meat and fish and the development of colorectal tumours. In this context, it has been postulated that the uptake of toxic substances formed during meat and fish processing such as heterocyclic aromatic amines (HCAs) may be causally related to colon carcinogenesis. In a previous study, we have shown that 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP), the most abundantly formed HCA in the above-mentioned food items, is mainly absorbed in the small intestine (i.e. proximal jejunum) of the rat. In the present study, we analysed whether PhIP can actively be secreted by enterocytes in the rat proximal jejunum and distal colon. Unidirectional PhIP flux rates from the mucosal-to-the serosal compartment (J ms ) and in the opposite direction (J sm ) were examined in Ussing chambers with 14C-PhIP as radiotracer and in the absence of electrochemical gradients. Under these experimental conditions, significant negative net flux rates (J net = J ms − J sm ) can only be explained by an active secretion of PhIP into the luminal compartment, and such an effect was observed in the rat distal colon, but not in the proximal jejunum. Moreover, the data obtained suggest that the breast cancer resistance protein, the multidrug resistance protein 4 and P-glycoprotein are not involved in the active secretion of PhIP in the rat distal colon. The potential role of PhIP transport in colon carcinogenesis is discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colon cancer is one of the most frequent cancers in the industrialized nations. The consumption of strongly heated meat correlates with certain cancer types, among others with colorectal tumours (Scheppach et al. 1999; Chao et al. 2005; Norat et al. 2005; Sinha et al. 2005; Wu et al. 2006; Rohrmann et al. 2007). Heterocyclic aromatic amines (HCAs) are formed in meat and fish during the cooking procedure at high temperatures for a long time or over an open fire. 2-Amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) is the most abundantly formed HCA and therefore may have a great impact on colon cancer development (Layton et al. 1995). PhIP is known to form DNA adducts after its metabolic activation and is mutagenic in bacterial as well as mammalian cell-based genotoxicity assays (Thompson et al. 1987; Frandsen et al. 1992; Schut and Herzog 1992; Friesen et al. 1994; Dragsted et al. 1995). Its carcinogenicity in the large intestine of the rat was demonstrated by Ito et al. (1991) and Hasegawa et al. (1993). In these carcinogenicity studies, extremely high (i.e. for humans totally irrelevant) concentrations of PhIP (100–400 ppm) were used. When PhIP was fed at concentrations below 50 ppm, the number of aberrant crypt foci or tumours in the colon of rats did not increase when compared to the corresponding control groups (Fukushima et al. 2004; Doi et al. 2005; Kühnel et al. 2009).
The necessity to feed extremely high concentrations of PhIP to induce preneoplastic or neoplastic lesions in the colon of the rat actually suggests that PhIP is only absorbed to a minor extent in the gut. This suggestion was verified by applying the Ussing chamber technique (Dietrich et al. 2001a; Nicken et al. 2010). In both studies, it was shown that approximately a thousandth part of PhIP added to the mucosal compartment of the Ussing chambers reached the serosal compartment. This effect could in part be due to the presence of efflux transporters pumping PhIP out of the intestinal mucosa. Dietrich et al. (2001a, 2001b) showed that the multidrug resistance protein 2 (MRP2), which transports a wide range of compounds conjugated with glucuronic acid, sulphate or glutathione (Oude Elferink et al. 1995) and is expressed in the apical domain of enterocytes present in the small intestine of the rat (Mottino et al. 2000; Rost et al. 2002; MacLean et al. 2008), may act as an efflux pump for PhIP and decreases its bioavailability (i.e. its concentration in systemic blood) in Wistar rats. Moreover, the breast cancer resistance protein (BCRP), whose expression increases within the small intestine from proximal to distal and thereafter strongly decreases in the colon of the male rat (MacLean et al. 2008), has also been shown to reduce the bioavailability of PhIP (van Herwaarden et al. 2003; Pavek et al. 2005). Very recently, Dietrich et al. (2011) reported that down-regulation of BCRP expression in murine colon adenomas leads to an accumulation of PhIP in the above-mentioned lesions (Dietrich et al. 2011), thus reinforcing the view that BCRP is an important PhIP efflux transporter.
We hypothesized that PhIP is taken up by the small intestine and reaches the distal colon via the systemic blood circulation, where it is actively secreted into the gut lumen. Earlier Ussing chamber studies (Dietrich et al. 2001a; Nicken et al. 2010) have clearly shown that segments of the small intestine (e.g. the proximal jejunum) take up PhIP and that PhIP migrates from the tissue into the serosal compartment of the chambers. In the present study, we have analysed whether PhIP can be actively secreted into the gut lumen in the proximal jejunum and/or the distal colon and which transport proteins may be involved in the secretion process. The relevance of PhIP transport (intestinal absorption as well as secretion) in colon carcinogenesis is discussed with regard to previously published results and those obtained in the present study.
Materials and methods
Chemicals
PhIP was synthesized by Albrecht Seidel (Biochemisches Institut für Umweltcarcinogene, Großhansdorf, Germany). Its purity (>98 %) was checked by HPLC. A 10 mmol l−1 stock solution of PhIP in dimethyl sulfoxide (Carl Roth, Karlsruhe, Germany) was used for the Ussing chamber experiments. 14C-PhIP (Toronto Research Chemicals, North York, Canada) was dissolved in dimethyl sulfoxide, and 2 μCi (74 kBq) were used to label either the mucosal or the serosal compartment of the Ussing chambers. In those experiments, in which mannitol was used as a specific marker of the paracellular pathway, 3 μCi (111 kBq) ³H-mannitol (PerkinElmer, Boston, USA) were added to the mucosal or serosal buffer (buffer constituents listed in the section “Ussing chamber experiments”). Verapamil and forskolin were purchased from Sigma Aldrich (Munich, Germany) and dissolved in water. Ko143 (Sigma Aldrich) was dissolved in dimethyl sulfoxide.
Animals
Male Fischer 344 rats were obtained from Charles River Laboratories International Inc. (Sulzfeld, Germany) and housed for a minimum of 8 days in our animal facility. During this period of time, the animals had free access to water and standard feed. Rats were killed at an age of 8–10 weeks (body weight 200 ± 40 g). The study protocol was approved by the Animal Welfare Service of the Lower Saxony State Office for Consumer Protection and Food Safety (Oldenburg, Germany).
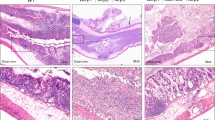
Preparation of the intestinal segments
Rats were killed by cervical dislocation and subsequent exsanguination. The whole gut was removed from the abdomen within the first 5 min after killing the animals and kept in the ice-cold buffer used for the serosal compartment (described in the section “Ussing chamber experiments”), which was continuously gassed with carbogen (95 % O2:5 % CO2), until the tissues were stripped and mounted into the Ussing chambers or cut into small pieces for gene expression analyses. The following gut segments were used: the duodenal sample was taken 1 cm below the pylorus, the proximal jejunal sample 15 cm distal to the duodenum, the distal jejunal sample 10 cm proximal to the ileum, the ileal sample directly proximal to the caecum and the caecal sample from the corpus ceci. The tissue excised up to 3 cm distal to the junction of the caecum and the colon was defined as “proximal colon”, the tissue proximal to the rectum as “distal colon” and the tissue immediately proximal to the anus as “rectum”. For the gene expression analyses, the samples were incubated overnight at 4 °C in RNAlater reagent (Qiagen, Hilden, Germany) and stored at −20 °C until RNA isolation was performed.
Ussing chamber experiments
The experiments were basically performed as previously described (Nicken et al. 2010) with slight modifications. Briefly, from each animal and location, two tissue segments of about 2 cm length were used. The tissues consisted of the mucosal layer, which had been stripped from the muscle, and the serosal layers on ice and mounted into the Ussing chambers with an exposed serosal area of 0.5 cm2. The tissue samples were stabilized by allowing them to recover from the preparation procedure for 30 min at the experimental temperature of 37 °C (Polentarutti et al. 1999). The buffer solution in the mucosal compartment of the Ussing chambers consisted of 113.6 mmol l−1 NaCl, 5.4 mmol l−1 KCl, 0.2 mmol l−1 HCl, 1.2 mmol l−1 MgCl2, 2 mmol l−1 NaHCO3, 0.4 mmol l−1 Na2HPO4, 1.1 mmol l−1 NaH2PO4, 2 mmol l−1 mannitol, 19.8 mmol l−1 sodium gluconate and 0.01 mmol l−1 indomethacin, while the buffer solution in the serosal compartment of the Ussing chambers consisted of 113.6 mmol l−1 NaCl, 5.4 mmol l−1 KCl, 0.4 mmol l−1 HCl, 1.2 mmol l−1 MgCl2, 21 mmol l−1 NaHCO3, 1.2 mmol l−1 Na2HPO4, 0.3 mmol l−1 NaH2PO4, 2 mmol l−1 mannitol and 0.01 mmol l−1 indomethacin. The lack of glucose at the luminal side avoided alterations in mucosal transport due to active glucose absorption. The osmolalities were measured at pH 7.4 in the serosal buffer solution and at pH 6.4 in the mucosal buffer (both at 37 °C after gassing with carbogen) and resulted in 283 and 273 mosm kg−1, respectively.
The tissues were incubated under short-circuited conditions, the electrophysiological parameters tissue conductance (G t ) and short-circuit current (I sc ) being continuously recorded throughout the entire experimental period. A 10 mmol l−1 PhIP stock solution was added to each compartment to yield a final PhIP concentration of 10 μmol l−1. The radiotracers 14C-PhIP and ³H-mannitol were then added to the mucosal or serosal compartments. After 30 min equilibration in the presence of radiotracers, 500 μl samples were collected every 15 min. Unidirectional flux rates became stable after another 30 min. After each sampling, the respective chamber was refilled with the corresponding amount of buffer. To determine which transport protein was involved in PhIP transport across the intestinal mucosa 100 μmol l−1 verapamil as a P-glycoprotein inhibitor (Iida et al. 2005) or 5 μmol l−1 Ko143 as a BCRP inhibitor (Allen et al. 2002) were added after 75 min to both the mucosal and the serosal compartments of the Ussing chambers and the sampling was continued for three further intervals. At the end of the experiments, 10 μmol l−1 forskolin was added to the serosal compartment of the Ussing chambers to prove the viability of the tissues. Forskolin leads to the stimulation of adenylate cyclase activity, which in turn normally induces a marked electrogenic chloride secretion via the cAMP pathway and is accompanied by a marked I sc increase (Bleich et al. 2007). The difference of the I sc value before application of forskolin and the maximal I sc response as a measure of electrogenic net ion secretion (maximal ΔI sc ) was used to test the viability of the tissue samples and to eliminate inappropriate tissues. For this purpose, Grubbs’ test (GraphPad Prism version 5.00 for Windows, GraphPad Software, San Diego, CA, USA) was applied to test the forskolin-induced maximal I sc data of the animals. The mean maximal ΔI sc ± standard deviation was 6.32 ± 1.42 (n = 22) with a critical Z value of 2.76. Z values in the experiments ranged between 0.06 and 1.92. However, no significant outlier was detected (level of significance 0.05, two-sided).
The radioactivity of the samples was measured using a conventional liquid scintillation counter (Wallac 1410; Wallac Oy, Turku, Finland). The standard double label DPM (decays per min) program of the Wallac counter was used for counting respective 14C and 3H radioactivities in the same sample. The tracers were discriminated on the basis of the corresponding quench standard libraries. Unidirectional flux rates (J ms , J sm ) were calculated from the rate of tracer appearance at the observed side using standard equations (Schultz and Zalusky 1964). Since mannitol has been suggested to be exclusively transported paracellularly, its flux rates can be used to estimate the corresponding water fluxes (Karbach 1992). For example, at a concentration of 2 mmol l−1 mannitol in the buffer as used here, a flux rate of 100 nmol cm−2 h−1 could be generated by the paracellular translocation of 50 μl of water. Since 0.01 mmol l−1 PhIP was homogenously dissolved in the buffer solution, this implies a theoretical PhIP flux rate of 0.5 nmol cm−2 h−1 in the same volume. Thus, this procedure enables the comparison of the calculated transepithelial flux rates of PhIP (“radiotracer method”) with the estimated paracellular flux rates (“mannitol method”, Fig. 1) and provides an approach to differentiate between transcellular and paracellular transport of PhIP.
Comparison of overall transepithelial flux rates of PhIP (data taken from Table 3) and paracellular flux rates (data calculated from mannitol flux rates as presented in Table 3; calculation exemplified in Materials and methods, section “Ussing chamber experiments”) in rat jejunum and colon. Results are expressed as mean ± SEM of ten independent experiments (Student’s t test for paired observations; n.s., not significant)
RNA isolation and quantitative real-time PCR
RNA was isolated with the RNeasy Plus Mini Kit (Qiagen) according to the instructions of the manufacturer. The columns were eluted twice with 30 μl water. The reverse transcription was performed by using 200 U Moloney murine leukaemia virus reverse transcriptase, 40 U RNAsin Plus and an oligo(dT)15 primer (all from Promega, Mannheim, Germany), and 6 μl of the isolated RNA in a 20 μl reaction. Expression levels of the rat target genes abcb1a (coding for Mdr1a), abcb1b (coding for Mdr1b), abcc4 (coding for Mrp4) and abcg2 (coding for BCRP) as well as the β-actin gene (as an internal control) were determined with the following primer pairs: forward β-actin (5′-CTG AAC CCT AAG GCC AAC C-3′) and reverse β-actin (5′-AAC ACA GCC TGG ATG GCT AC-3′); forward abcb1a (5′-CTG GAG GAC GAA ATG ACC AC-3′) and reverse abcb1a (5′-TGG AGA CGT CAT CTG TGA GC-3′); forward abcb1b (5′-TGC TCA TCG TTG CCT ACA TC-3′) and reverse abcb1b (5′-TCC AAG TTT GTC ACC AAT TCC-3`); forward abcg2 (5′-TCA CTG ACC CTT CCA TCC TC-3′) and reverse abcg2 (5′-TGT TGT AGG GCT CAC AGT GG-3′); forward abcc4 (5′-AAG TTC TGC GAG CCA AGA AG-3′) and reverse abcc4 (5′-GCC GAG TCG TCA GAG TCA TAC-3′). The quantitative PCR was carried out with a Mx3000P sequence detection system (Agilent Technologies, Waldbronn, Germany) in a 20 μL reaction containing KAPA SYBR® FAST qPCR Universal Mix (Peqlab Biotechnologie GmbH, Erlangen, Germany), 100 nmol l−1 forward primer, 100 nmol l−1 reverse primer, and 2 μl of a 1:10 diluted cDNA sample using an annealing and elongation temperature of 60 °C. The melting curves were analysed after 40 amplification cycles. The quantification was performed by making use of a standard curve of pooled proximal jejunum and ileum samples over 5 log levels of dilution in each plate. The target gene expression levels were normalized by dividing them by the rat β-actin expression level. All assays were performed at least in duplicates.
Statistical analyses
The data of the Ussing chamber experiments are presented as arithmetic mean ± SEM. Statistical analyses (Grubbs’ outlier test, paired t test) were performed with the number of animals (n) as indicated in the respective text, tables and figures with GraphPad Prism 5.0 (GraphPad Software, San Diego, CA, USA) and values of p < 0.05 were considered statistically significant.
Results
Electrophysiological parameters and unidirectional flux rates of PhIP and mannitol in proximal jejunum and distal colon under baseline conditions
To reduce prostaglandin-mediated secretory activities that potentially could interfere with tissue viability and particularly with PhIP flux rates in jejunum and colon indomethacin was added to the buffer solutions. Therefore, in a first step, the effect of indomethacin on the electrophysiological parameters determined in the Ussing chamber experiments was analysed. As in the case of pig and dog (Schröder et al. 1991; Omori et al. 2011), basal I sc values were higher in the absence of indomethacin than in the presence of it. Furthermore, in the presence of indomethacin, tissue permeabilities as a function of time were more stable and the forskolin response was more prominent, thus indicating greater viability over time (Table 1). In a few experiments (n = 4), secretory PhIP flux rates in distal colon were determined in the presence or absence of indomethacin. It was shown that indomethacin has no influence on the secretory PhIP flux rates (data not shown).
Mean basal I sc and G t values of jejunal and colonic preparations after a 60 min incubation in the presence of indomethacin are presented in Table 2. Whereas I sc values as a measure of total electrogenic net ion transport were not significantly different between jejunum and colon, G t values as a measure of tissue permeability were higher (by about 20 %) in jejunum than in colon (p < 0.05). The forskolin-induced I sc response was significantly higher (by almost 40 %) in colon when compared to jejunum.
Equilibrated mean unidirectional flux rates of PhIP and mannitol occurred at 60 min of incubation (Table 3). In jejunum, the PhIP flux rate in the mucosa-to-serosa direction (J ms ) was not significantly different from J sm , thereby resulting in a J net (J net = J ms − J sm ) that was not different from zero. In contrast, J sm of PhIP in colon was significantly higher (by 138 %) than in the opposite direction, thus leading to a net secretion of PhIP. Irrespective of the direction, mannitol flux rates were not significantly different in jejunum and colon and resulted in J net values that were not significantly different from zero.
Unidirectional flux rates of mannitol were used to calculate paracellular water fluxes, which can be used to estimate the corresponding theoretical paracellular PhIP flux rates. These in turn can be compared with transepithelial flux rates of PhIP obtained from radiotracer measurements (Fig. 1). Interestingly, in the jejunum, the estimated paracellular flux rates of PhIP were significantly higher than the transepithelial fluxes. In contrast, in the colon, the J ms values for the transepithelial and paracellular pathways were similar, while the transepithelial transport of PhIP in the opposite direction was significantly higher than the estimated paracellular transport (Fig. 1).
Unidirectional flux rates of PhIP in distal colon in the presence of transport inhibitors
To identify which transport proteins could be involved in the actively driven PhIP secretion in rat distal colon, the P-glycoprotein inhibitor verapamil and the BCRP inhibitor Ko143 were used. Neither 100 μmol l−1 verapamil nor 5 μmol l−1 Ko143 had a significant inhibitory effect on J sm of PhIP (Fig. 2). Even after adding 25 μmol l−1 Ko143, no effect on J sm of PhIP was observed (data not shown).
Transporter gene expression in different sections of the gut
The expression of the genes coding for the transport proteins BCRP, Mdr1a and Mdr1b was measured by real-time quantitative PCR experiments in different segments of the rat gut. The three gene transcripts were expressed in all gut segments (Fig. 3), and no statistical significant differences in the expression levels of the three genes were observed among the different segments. In contrast, Mrp4 was expressed at 1010 times lower levels than β-actin (data not shown).
Discussion
In an early study by Watkins et al. (1991), it was shown that Fischer 344 rats excrete about 80 % of an oral dose of 14C-marked PhIP within the first 24 h via faeces. In accordance with this observation, Ussing chamber experiments by Dietrich et al. (2001a) and our group (Nicken et al. 2010) demonstrated that PhIP is taken up to a limited extent in the small intestine (e.g. the proximal jejunum). In a follow-up study, we now show that PhIP is secreted into the luminal compartment of Ussing chambers when rat distal colon samples are used as a transport site. To differentiate between paracellular (passive) and transcellular (active) transport, mannitol flux rates were examined and compared with those of PhIP. The fact that PhIP flux rates significantly differed from mannitol flux rates suggests that PhIP is actively secreted into the luminal compartment in rat colon. These results are in agreement with a previous study by Walle and Walle (1999) in Caco-2 cells, in which the basolateral to apical PHIP efflux was 3.6 times greater than the apical to basolateral PhIP influx and in which equilibrium exchange experiments demonstrated the PhIP efflux in Caco-2 cells to be mediated by an active process.
MRP2 as well as MRP4 can be discarded as protein(s) involved in the transport of PhIP across the gut mucosa in Fischer 344 rats, since they are almost not detectable in the tissue samples analysed (Nicken et al. 2010; this study). P-glycoprotein has previously been reported to transport PhIP (Walle and Walle 1999), but this seems not to be the case in the distal colon of Fischer 344 rats, since verapamil had no effect on the PhIP efflux. This is in accordance with the observation by Iida et al. (2005) that P-glycoprotein only played a minor role in the clearance of the P-glycoprotein substrate rhodamine 123 in the colon when compared to the jejunum and ileum of rats. BCRP acts as an efflux pump for PhIP and is able to reduce the bioavailability of PhIP in mice by increasing its faecal elimination (van Herwaarden et al. 2003; Pavek et al. 2005). However, the expression of BCRP was very low in the rat colon samples, an observation that is in accordance with a study by MacLean et al. (2008). Furthermore, the highly specific BCRP inhibitor Ko143 (van Loevezijn et al. 2001; Allen et al. 2002) had no effect on PhIP efflux. Although one could argue that Ko143 did not reach the BCRP molecules during the incubation period chosen, these results rather show that BCRP is not involved in PhIP efflux in the distal colon of Fischer 244 rats. Future experiments will be conducted to identify the transport protein(s) responsible for pumping PhIP out of the rat colon epithelial cells. Another open question remaining unanswered at present is whether N-hydroxy-PhIP (N-OH-PhIP), an important metabolite of PhIP (see below), is also actively pumped out of rat colon epithelial cells. Since no radioactively marked N-OH-PhIP was available, it could not be tested in the Ussing chamber experiments.
In order to discuss the relevance of the above-mentioned PhIP movements across the rat gut mucosa in PhIP-induced colon carcinogenesis, one has to take into account how and where PhIP is activated in the rat. The first step in the activation of PhIP is its N-oxidation to N-OH-PhIP, a reaction that primarily occurs in the rat liver and is catalysed by cytochrome P450 1A2 (Wallin et al. 1990; Alexander et al. 1994; Lin et al. 1995; Turesky et al. 1998), while it does not take place in the rat colon (Malfatti et al. 1996). N-OH-PhIP is metabolized in a second step by N-acetyltransferase 2 and sulfotransferases to the corresponding N-acetoxy and N-sulfonyloxy esters. These are unstable, spontaneously decompose and give rise to the nitrenium ion, which in turn binds to DNA (Frandsen et al. 1992; Lin et al. 1992; Nagaoka et al. 1992).
By combining the knowledge on PhIP transport and metabolism mentioned above, the way how HCAs lead to the formation of malignant tumours in the rat colon, first suggested by Kaderlik et al. (1994) and now complemented with transport studies (Nicken et al. 2010; this study), becomes more and more concrete and is schematically presented in Fig. 4. A limited amount of PhIP is absorbed in the small intestine and transported via the portal vein into the liver. In the liver, PhIP is converted into N-OH-PhIP in a cytochrome P450-mediated reaction, and the esterified form of N-OH-PhIP and/or free N-OH-PhIP is/are transported via the bloodstream to the distal colon, where the metabolite(s) is/are secreted into the gut lumen. During the passage of the active metabolite(s) through the colon mucosa, the compound(s) enter(s) the stem cell compartment, in which the nitrenium ion is released. If stem cell DNA is damaged by the nitremium ions, initiated cells might be formed and with time give rise to a malignant tumour. In the case that N-OH-PhIP is taken up by the stem cells in the colon crypts, it must first be esterified (most probably acetylated) as a precondition for nitrenium ion formation within these cells.
Hypothetical scheme describing the fate of PhIP following its uptake in the small intestine. Details regarding the scheme are included in the section “Discussion”
As to the target cell population hit by the PhIP metabolite(s) Takahashi et al. (1998) administered a single dose of PhIP to rats, killed the animals 1, 2 or 7 days later and analysed the distribution of PhIP-DNA adducts in various organs including the colon by making use of a polyclonal antibody against PhIP-DNA adducts. The authors reported that PhIP-DNA adducts were uniformly detected in surface epithelial cells and crypt cells of the colon. If one takes into account that surface epithelial cells in the rat colon have a very short lifespan (Qi et al. 2009), these cells most probably cannot serve as precursor cells for the tumours arising later. Based on the fact that antibodies against PhIP-DNA adducts are available (Takahashi et al. 1998) and that markers for cancer stem cells in rat colonic crypts have been described (Levi et al. 2009), it should be possible to define in the near future which cells within the colonic crypts of the rat are indeed involved in the formation of colon tumours in PhIP-treated rats.
If it is considered that a large amount of PhIP administered to rats p.o. is eliminated with faeces (Watkins et al. 1991), the possibility that bacteria in the colon metabolize PhIP to a mutagenic metabolite has to be discussed. In fact, Vanhaecke et al. (2008a) detected the PhIP metabolite 7-hydroxy-5-methyl-3-phenyl-6,7,8,9-tetrahydropyrido[3′,2′:4,5]imidazo[1,2-a]pyrimidin-5-ium chloride (PhIP-M1) in faecal samples of human volunteers having eaten cooked chicken containing PhIP and identified the bacterial strains in human faeces that are able to catalyse the conversion of PhIP to PhIP-M1 (Vanhaecke et al. 2008b). Moreover, alkaline comet assay experiments revealed that PhIP-M1 led to a concentration-dependent increase in DNA damage in Caco-2 cells (Vanhaecke et al. 2008c), whereby the genotoxic effect was observed in a concentration range of 50-200 μmol l−1. Since humans take up less than 1 μg HCAs per day (SKLM 1998), even if one supposed that 100 % of the daily amount of PhIP ingested by a human being is converted into PhIP-M1 in the colon, the concentration needed to induce DNA damage in the epithelial cells of the colonic mucosa is definitely not reached.
A number of epidemiological studies have pointed out that a positive association between the consumption of red and processed meat and colorectal cancer risk exists (Scheppach et al. 1999; Chao et al. 2005; Norat et al. 2005; Sinha et al. 2005; Wu et al. 2006; Rohrmann et al. 2007). Furthermore, it has been postulated that haem iron, nitrate/nitrite as well as HCAs present in red and processed meat might explain the above-mentioned association (Cross et al. 2010). However, the fact that the amounts of HCAs actually consumed by humans are very low (<1μg/person/day) and that only a limited fraction of the HCAs ingested are taken up in the small intestine (Watkins et al. 1991; Dietrich et al. 2001a; Nicken et al. 2010) and later activation supports the view that HCAs alone cannot account for the increased red and processed meat-associated colorectal cancer risk. Most probably, the continuous or discontinuous exposure of the gastrointestinal tract to a number of compounds present in red and processed meat (e.g. haem iron, nitrate/nitrite as well as HCAs) in combination with toxic intermediates endogenously formed in the gut (e.g. endogenously formed N-nitroso compounds) (Bingham et al. 1996; Hughes et al. 2001; Bingham et al. 2002; Cross et al. 2003; Lewin et al. 2006; Kuhnle et al. 2007) and other risk factors (ethanol, tobacco and/or obesity among others) are responsible for the high colorectal cancer incidence observed in industrialized nations.
References
Alexander J, Fossum BH, Holme JA (1994) Metabolism of the food mutagen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) in isolated liver cells from guinea pig, hamster, mouse, and rat. Environ Health Perspect 102(Suppl 6):109–114
Allen JD, van Loevezijn A, Lakhai JM, van der Valk M, van Tellingen O, Reid G, Schellens JH, Koomen GJ, Schinkel AH (2002) Potent and specific inhibition of the breast cancer resistance protein multidrug transporter in vitro and in mouse intestine by a novel analogue of fumitremorgin C. Mol Cancer Ther 1:417–425
Bingham SA, Pignatelli B, Pollock JR, Ellul A, Malaveille C, Gross G, Runswick S, Cummings JH, O’Neill IK (1996) Does increased endogenous formation of N-nitroso compounds in the human colon explain the association between red meat and colon cancer? Carcinogenesis 17:515–523
Bingham SA, Hughes R, Cross AJ (2002) Effect of white versus red meat on endogenous N-nitrosation in the human colon and further evidence of a dose response. J Nutr 132:3522S–3525S
Bleich A, Leonhard-Marek S, Beyerbach M, Breves G (2007) Characterisation of chloride currents across the proximal colon in CftrTgH(neoim)1Hgu congenic mice. J Comp Physiol B 177:61–73
Chao A, Thun MJ, Connell CJ, McCullough ML, Jacobs EJ, Flanders WD, Rodriguez C, Sinha R, Calle EE (2005) Meat consumption and risk of colorectal cancer. JAMA 293:172–182
Cross AJ, Pollock JR, Bingham SA (2003) Haem, not protein or inorganic iron, is responsible for endogenous intestinal N-nitrosation arising from red meat. Cancer Res 63:2358–2360
Cross AJ, Ferrucci LM, Risch A, Graubard RI, Ward MH, Park Y, Hollenbeck AR, Schatzkin A, Sinha R (2010) A large prospective study of meat consumption and colorectal cancer risk: an investigation of potential mechanisms underlying this association. Cancer Res 70:2406–2414
Dietrich CG, de Waart DR, Ottenhoff R, Schoots IG, Elferink RP (2001a) Increased bioavailability of the food-derived carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine in MRP2-deficient rats. Mol Pharmacol 59:974–980
Dietrich CG, de Waart DR, Ottenhoff R, Bootsma AH, van Gennip AH, Elferink RP (2001b) Mrp2-deficiency in the rat impairs biliary and intestinal excretion and influences metabolism and disposition of the food-derived carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine. Carcinogenesis 22:805–811
Dietrich CG, Vehr AK, Martin IV, Gassler N, Rath T, Roeb E, Schmitt J, Trautwein C, Geier A (2011) Downregulation of breast cancer resistance protein in colon adenomas reduces cellular xenobiotic resistance and leads to accumulation of a food-derived carcinogen. Int J Cancer 129:546–552
Doi K, Wanibuchi H, Salim EI, Morimura K, Kinoshita A, Kudoh S, Hirata K, Yoshikawa J, Fukushima S (2005) Lack of large intestinal carcinogenicity of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine at low doses in rats initiated with azoxymethane. Int J Cancer 115:870–878
Dragsted LO, Frandsen H, Reistad R, Alexander J, Larsen JC (1995) DNA-binding and disposition of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) in the rat. Carcinogenesis 16:2785–2793
Frandsen H, Grivas S, Andersson R, Dragsted L, Larsen JC (1992) Reaction of the N 2-acetoxy derivative of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) with 2′-deoxyguanosine and DNA. Synthesis and identification of N 2-(2′-deoxyguanosin-8-yl)-PhIP. Carcinogenesis 13:629–635
Friesen MD, Kaderlik K, Lin D, Garren L, Bartsch H, Lang NP, Kadlubar FF (1994) Analysis of DNA adducts of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine in rat and human tissues by alkaline hydrolysis and gas chromatography/electron capture mass spectrometry: validation by comparison with 32P-postlabeling. Chem Res Toxicol 7:733–739
Fukushima S, Wanibuchi H, Morimura K, Iwai S, Nakae D, Kishida H, Tsuda H, Uehara N, Imaida K, Shirai T, Tatematsu M, Tsukamoto T, Hirose M, Furukawa F (2004) Existence of a threshold for induction of aberrant crypt foci in the rat colon with low doses of 2-amino-1-methyl-6-phenolimidazo[4,5-b]pyridine. Toxicol Sci 80:109–114
Hasegawa R, Sano M, Tamano S, Imaida K, Shirai T, Nagao M, Sugimura T, Ito N (1993) Dose-dependence of 2-amino-1-methyl-6-phenylimidazo[4,5-b]-pyridine (PhIP) carcinogenicity in rats. Carcinogenesis 14:2553–2557
Hughes R, Cross AJ, Pollock JR, Bingham S (2001) Dose-dependent effect of dietary meat on endogenous colonic N-nitrosation. Carcinogenesis 22:199–202
Iida A, Tomita M, Hayashi M (2005) Regional difference in P-glycoprotein function in rat intestine. Drug Metab Pharmacokinet 20:100–106
Ito N, Hasegawa R, Sano M, Tamano S, Esumi H, Takayama S, Sugimura T (1991) A new colon and mammary carcinogen in cooked food, 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP). Carcinogenesis 12:1503–1506
Kaderlik KR, Minchin RF, Mulder GJ, Ilett KF, Daugaard-Jenson M, Teitel CH, Kadlubar FF (1994) Metabolic activation pathway for the formation of DNA adducts of the carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) in rat extrahepatic tissues. Carcinogenesis 15:1703–1709
Karbach U (1992) Paracellular calcium transport across the small intestine. J Nutr 122:672–677
Kühnel D, Taugner F, Scholtka B, Steinberg P (2009) Inflammation does not precede or accompany the induction of preneoplastic lesions in the colon of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine-fed rats. Arch Toxicol 83:763–768
Kuhnle GG, Story GW, Reda T, Mani AR, Moore KP, Lunn JC, Bingham SA (2007) Diet-induced endogenous formation of nitroso compounds in the GI tract. Free Radic Biol Med 43:1040–1047
Layton DW, Bogen KT, Knize MG, Hatch FT, Johnson VM, Felton JS (1995) Cancer risk of heterocyclic amines in cooked foods: an analysis and implications for research. Carcinogenesis 16:39–52
Levi E, Misra S, Du J, Patel BB, Majumdar AP (2009) Combination of aging and dimethylhydrazine treatment causes an increase in cancer-stem cell population of rat colonic crypts. Biochem Biophys Res Commun 385:430–433
Lewin MH, Bailey N, Bandaletova T, Bowman R, Cross AJ, Pollock J, Shuker DE, Bingham SA (2006) Red meat enhances the colonic formation of the DNA adduct O 6-carboxymethyl guanine: implications for colorectal cancer risk. Cancer Res 66:1859–1865
Lin D, Kaderlik KR, Turesky RJ, Miller DW, Lay JO, Kadlubar FF (1992) Identification of N-(deoxyguanosine-8-yl)-2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine as the major adduct formed by the food-borne carcinogen, 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine, with DNA. Chem Res Toxicol 5:691–697
Lin DX, Lang NP, Kadlubar FF (1995) Species differences in the biotransformation of the food-borne carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine by hepatic microsomes and cytosols from humans, rats, and mice. Drug Metab Dispos 23:518–524
MacLean C, Moenning U, Reichel A, Fricker G (2008) Closing the gaps: a full scan of the intestinal expression of p-glycoprotein, breast cancer resistance protein, and multidrug resistance-associated protein 2 in male and female rats. Drug Metab Dispos 36:1249–1254
Malfatti MA, Connors MS, Mauthe RJ, Felton JS (1996) The capability of rat colon tissue slices to metabolize the cooked-food carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine. Cancer Res 56:2550–2555
Mottino AD, Hoffman T, Jennes L, Vore M (2000) Expression and localization of multidrug resistant protein mrp2 in rat small intestine. J Pharmacol Exp Ther 293:717–723
Nagaoka H, Wakabayashi K, Kim S-B, Kim I-S, Tanaka Y, Ochiai M, Tada A, Nukuya H, Sugimura T, Nagao M (1992) Adduct formation at C-8 of guanine on in vitro reaction of the ultimate form of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine with 2′-deoxyguanosine and its phosphate esters. Jpn J Cancer Res 83:1025–1029
Nicken P, Hamscher G, Breves G, Steinberg P (2010) Uptake of the colon carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine by different segments of the rat gastrointestinal tract: its implication in colorectal carcinogenesis. Toxicol Lett 196:60–66
Norat T, Bingham S, Ferrari P, Slimani N, Jenab M, Mazuir M, Overvad K, Olsen A, Tjonneland A, Clavel F, Boutron-Ruault MC, Kesse E, Boeing H, Bergmann MM, Nieters A, Linseisen J, Trichopoulou A, Trichopoulos D, Tountas Y, Berrino F, Palli D, Panico S, Tumino R, Vineis P, Bueno-de-Mesquita HB, Peeters PH, Engeset D, Lund E, Skeie G, Ardanaz E, Gonzalez C, Navarro C, Quiros JR, Sanchez MJ, Berglund G, Mattisson I, Hallmans G, Palmqvist R, Day NE, Khaw KT, Key TJ, San JM, Hemon B, Saracci R, Kaaks R, Riboli E (2005) Meat, fish, and colorectal cancer risk: the European Prospective Investigation into cancer and nutrition. J Natl Cancer Inst 97:906–916
Omori M, Hill RC, Scott KC, Lester GD (2011) Evaluation of the secretory response to endogenous and exogenous prostaglandins in mucosa from the proximal and distal portions of the colon of dogs. Am J Vet Res 72:404–409
Oude Elferink RP, Meijer DK, Kuipers F, Jansen PL, Groen AK, Groothuis GM (1995) Hepatobiliary secretion of organic compounds; molecular mechanisms of membrane transport. Biochim Biophys Acta 1241:215–268
Pavek P, Merino G, Wagenaar E, Bolscher E, Novotna M, Jonker JW, Schinkel AH (2005) Human breast cancer resistance protein: interactions with steroid drugs, hormones, the dietary carcinogen 2-amino-1-methyl-6-phenylimidazo(4,5-b)pyridine, and transport of cimetidine. J Pharmacol Exp Ther 312:144–152
Polentarutti BI, Peterson AL, Sjöberg ÅK, Anderberg EKI, Utter LM, Ungell A-LB (1999) Evaluation of viability of excised rat intestinal segments in Ussing chamber: investigation of morphology, electrical parameters, and permeability characteristics. Pharm Res 16:446–454
Qi WM, Yamamoto K, Yokoo Y, Miyata H, Udayanga KG, Kawano J, Yokoyama T, Hoshi N, Kitagawa H (2009) Histoplanimetrical study on the relationship between cellular kinetics of epithelial cells and proliferation of indigenous bacteria in the rat colon. J Vet Med Sci 71:745–752
Rohrmann S, Zoller D, Hermann S, Linseisen J (2007) Intake of heterocyclic aromatic amines from meat in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Heidelberg cohort. Br J Nutr 98:1112–1115
Rost D, Mahner S, Sugiyama Y, Stremmel W (2002) Expression and localization of the multidrug resistance-associated protein 3 in rat small and large intestine. Am J Physiol Gastrointest Liver Physiol 282:G720–G726
Scheppach W, Bingham S, Boutron-Ruault MC, Gerhardsson de Verdier M, Moreno V, Nagengast FM, Reifen R, Riboli E, Seitz HK, Wahrendorf J (1999) WHO consensus statement on the role of nutrition in colorectal cancer. Eur J Cancer Prev 8:57–62
Schröder B, Kaune R, Harmeyer J (1991) Effects of calcitriol on stimulation of ion transport in pig jejunal mucosa. J Physiol 433:461–465
Schultz SG, Zalusky R (1964) Ion transport in isolated rabbit ileum. I. Short-circuit current and Na fluxes. J Gen Physiol 47:567–584
Schut HA, Herzog CR (1992) Formation of DNA adducts of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) in male Fischer-344 rats. Cancer Lett 67:117–124
Sinha R, Peters U, Cross AJ, Kulldorff M, Weissfeld JL, Pinsky PF, Rothman N, Hayes RB (2005) Meat, meat cooking methods and preservation, and risk for colorectal adenoma. Cancer Res 65:8034–8041
SKLM (1998) Heterocyclische aromatische Amine. Statement of the Permanent Senate Commission on Food Safety of the German Research Foundation, 14./15.12.1998
Takahashi S, Tamano S, Hirose M, Kimoto N, Ikeda Y, Sakakibara M, Tada M, Kadlubar FF, Ito N, Shirai T (1998) Immunohistochemical demonstration of carcinogen-DNA adducts in tissues of rats given 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP): detection in paraffin-embedded sections and tissue distribution. Cancer Res 58:4307–4313
Thompson LH, Tucker JD, Stewart SA, Christensen ML, Salazar EP, Carrano AV, Felton JS (1987) Genotoxicity of compounds from cooked beef in repair-deficient CHO cells versus Salmonella mutagenicity. Mutagenesis 2:483–487
Turesky RJ, Constable A, Richoz J, Varga N, Markovic J, Martin MV, Guengerich FP (1998) Activation of heterocyclic aromatic amines by rat and human liver microsomes and by purified rat and human cytochrome P450 1A2. Chem Res Toxicol 11:925–936
van Herwaarden AE, Jonker JW, Wagenaar E, Brinkhuis RF, Schellens JH, Beijnen JH, Schinkel AH (2003) The breast cancer resistance protein (Bcrp1/Abcg2) restricts exposure to the dietary carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine. Cancer Res 63:6447–6452
van Loevezijn A, Allen JD, Schinkel AH, Koomen GJ (2001) Inhibition of BCRP-mediated drug efflux by fumitremorgin-type indolyl diketopiperazines. Bioorg Med Chem Lett 11:29–32
Vanhaecke L, Knize MG, Noppe H, De Brabander H, Verstraete W, Van de Wiele T (2008a) Intestinal bacteria metabolize the dietary carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine following consumption of a single cooked chicken meal in humans. Food Chem Toxicol 46:140–148
Vanhaecke L, Vercruysse F, Boon N, Verstraete W, Cleenwerck I, De Wachter M, De Vos P, van de Wiele T (2008b) Isolation and characterization of human intestinal bacteria capable of transforming the dietary carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine. Appl Environ Microbiol 74:1469–1477
Vanhaecke L, Derycke L, Le Curieux F, Lust S, Marzin D, Verstraete W, Bracke M (2008c) The microbial PhIP metabolite 7-hydroxy-5-methyl-3-phenyl-6,7,8,9-tetrahydropyrido[3′,2′:4,5]imidazo[1,2-a]pyrimidin-5-ium chloride (PhIP-M1) induces DNA damage, apoptosis and cell cycle arrest towards Caco-2 cells. Toxicol Lett 178:61–69
Walle UK, Walle T (1999) Transport of the cooked-food mutagen 2-amino-1-methyl-6-phenylimidazo-[4,5-b]pyridine (PhIP) across the human intestinal Caco-2 cell monolayer: role of efflux pumps. Carcinogenesis 20:2153–2157
Wallin H, Mikalsen A, Guengerich FP, Ingelman-Sundberg M, Solberg KE, Rossland OR, Alexander J (1990) Differential rates of metabolic activation and detoxication of the food mutagen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine by different cytochrome P450 enzymes. Carcinogenesis 11:489–492
Watkins BE, Esumi H, Wakayabashi K, Nagao M, Sugimura T (1991) Fate and distribution of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) in rats. Carcinogenesis 12:1073–1078
Wu K, Giovannucci E, Byrne C, Platz EA, Fuchs C, Willett WC, Sinha R (2006) Meat mutagens and risk of distal colon adenoma in a cohort of U.S. men. Cancer Epidemiol Biomarkers Prev 15:1120–1125
Acknowledgments
We thank Marion Burmester, Marion Loh, Kerstin Kiri, Yvonne Armbrecht and Michael Rohde for their excellent technical assistance.
Conflict of interest
The authors state that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Petra Nicken, Bernd Schröder and Anne von Keutz contributed equally to the study.
Rights and permissions
About this article
Cite this article
Nicken, P., Schröder, B., von Keutz, A. et al. The colon carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) is actively secreted in the distal colon of the rat: an integrated view on the role of PhIP transport and metabolism in PhIP-induced colon carcinogenesis. Arch Toxicol 87, 895–904 (2013). https://doi.org/10.1007/s00204-012-1006-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-012-1006-0