Abstract
Summary
We investigated whether bone microstructure assessed by high-resolution peripheral quantitative tomography (HR-pQCT) could be altered in children and teenagers with cystic fibrosis (CF). In comparison to their healthy counterparts, bone microstructure was mildly affected at the tibial level only.
Introduction
Cystic fibrosis-related bone disease (CFBD) may alter bone health, ultimately predisposing patients to bone fractures. Our aim was to assess bone microstructure using high-resolution peripheral quantitative tomography (HR-pQCT) in a cohort of children and teenagers with CF in comparison to age-, puberty-, and gender-matched healthy volunteers (HVs).
Methods
In this single-center, prospective, cross-sectional study, we evaluated the HR-pQCT bone parameters of CF patients and compared them to those of the healthy volunteers.
Results
At a median age of 15.4 [range, 10.5–17.9] years, 37 CF patients (21 boys) with 91% [range, 46–138%] median forced expiratory volume in 1 s were included. At the ultradistal tibia, CF patients had a smaller bone cross-sectional area (579 [range, 399–1087] mm2) than HVs (655 [range, 445–981] mm2) (p = 0.027), related to a decreased trabecular area, without any significant differences for height. No other differences were found (trabecular number, separation, thickness, or distribution) at the radial or tibial levels. Bone structure was different in patients receiving ursodeoxycholic acid and those bearing two F508del mutations.
Conclusion
In our cohort of children and teenagers with good nutritional and lung function status, bone microstructure evaluated with HR-pQCT was not severely affected. Minimal microstructure abnormalities observed at the tibial level may be related to the cystic fibrosis transmembrane conductance regulator defect alone; the long-term consequences of such impairment will require further evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Improved management of patients with cystic fibrosis (CF) has dramatically increased their life expectancy over the last few decades. Consequently, the prevalence of late complications such as CF-related bone disease (CFBD), known as osteoporosis or osteopenia as defined by the World Health Organization, has increased and reached up to 24% of adult patients in the most recent publications [1].
CFBD results from the complex combination of primary (i.e., primary cystic fibrosis transmembrane conductance regulator (CFTR) defect in the osteoblasts [2, 3]) and secondary (i.e., pancreatic insufficiency, denutrition, corticosteroids) factors that contribute to bone loss (reviewed in [4]). We and others have previously reported that CFBD can start early, in patients younger than 6 years with preserved respiratory health and nutritional status [4,5,6]. As such, recent cross-sectional data indicate that teenagers with CF had an almost tenfold higher risk of bone fractures in comparison to their healthy peers and that 60% of them will experience bone fractures by 25 years of age [7].
The European and North American guidelines recommend CFBD to be monitored beginning as early as 8 years of age, using dual X-ray absorptiometry (DXA) [8, 9]. Although DXA has several advantages and remains the gold standard for CFBD monitoring, it nevertheless fails to accurately assess bone quality (e.g., bone strength and bone trabecular microstructure), whose alteration was included in the definition of osteoporosis by the National Institutes of Health (NIH) in 2000. This lack of bone quality assessment may explain why a single-center study failed to find a correlation between vertebral BMD and bone fracture risk in adults with CF [10].
High-resolution peripheral quantitative computed tomography (HR-pQCT) may be valuable to assess bone quality in pediatric patients with CF. In contrast to peripheral quantitative computed tomography (pQCT), HR-pQCT evaluates not only all compartmental volumetric BMDs (total, cortical, and trabecular) but also trabecular microarchitecture and cortical thickness with a 82-μm3 voxel [11]. It requires absolute immobility for 3 min. The effective doses of HR-pQCT are among the lowest, similar to a DXA [12]. As a research tool, currently only limited data have been published in the CF adult population using HR-pQCT [13,14,15]. Gensburger et al. reported bone DXA and HR-pQCT evaluation in a cohort of 56 adults with CF. Abnormal bone microstructure, albeit of moderate importance with lower total and cortical vBMDs, and trabecular thickness (respectively, − 9.9, − 3.0, and − 5%, p < 0.05) were found to be significant only at the tibia, after age, gender, body weight, and height adjustments [13]. In the other two cohorts of 30 adults each, both tibial and radial microstructures were impaired, again with greater abnormalities at the tibia [14, 15]. In pediatrics, bone microstructure has been assessed in other populations with chronic disease [16, 17]. A study exploring bone microstructure using peripheral QCT (pQCT) in children with CF was recently published, demonstrating bone alteration especially at the tibia [18]. Another recent study found bone architecture abnormalities explored by pQCT at the radius level (bone mineral content and density, strength strain index at the proximal forearm) that differentiated teenagers who had no or one fracture and those having more than one fracture [7]. However, to the best of our knowledge, there are currently no published data on the use of HR-pQCT in children with CF.
Our primary goal was therefore to evaluate bone compartmental density, trabecular microstructure, and cortical geometry at the ultradistal radius and tibia in children and teenagers with CF, in comparison to age-, gender-, and puberty-matched local healthy controls, assuming that bone quantity and quality would be impaired in this young population with CF.
Patients and methods
We conducted a single-center prospective cross-sectional study between April 2014 and April 2015. Patients with CF were recruited from our pediatric CF center. The inclusion criteria were the following: being aged between 10 and 18 years and being clinically stable (absence of increased cough, sputum production, fatigue, breathlessness, hemoptysis for more than three consecutive days over a period of 3 weeks). The exclusion criteria were the following: patients unable to keep the arm or the leg completely still for 3 min, patients having undergone transplantation, patients participating in another investigational research protocol during the same period, pregnancy and any situation that might prevent consent of persons exercising parental authority. Patients who met the inclusion criteria were approached and participation in the study was proposed. A total of 41 patients were contacted. Two patients declined to participate. In the time between the protocol enrollment and the patient’s evaluation for radiological assessment, two patients became clinically unstable (pulmonary exacerbation). They were then excluded, leading to a total of 37 patients. The study was approved by the local institutional review board (Comité de Protection des Personnes Lyon Sud Est II, #2012-029-2). Written informed consent was obtained from all parents and patients before enrollment.
Clinical, functional, and biological outcomes
Medical records were reviewed to collect pertinent medical or therapeutic data that may impact bone health, namely the CFTR genotype, exocrine pancreatic insufficiency, allergic bronchopulmonary aspergillosis, Pseudomonas aeruginosa colonization status, vitamin D, K, and A supplementations, ursodeoxycholic acid (UDAC), diabetes mellitus, and history of fracture (as defined by the International Society of Clinical Densitometry [19]). Given that a precise lifelong evaluation of corticosteroid exposure was at high risk of error given its retrospective nature and dependence on the patient’s compliance (recall bias), we chose to collect only recent oral or inhaled steroid exposure in the year preceding the investigations. The proportion of patients that had received at least 3 days of oral steroids and/or at least three consecutive months of inhaled steroids in the year preceding bone assessment was recorded. Since liver disease may impair bone health [20], we recorded patients who were receiving UDAC for confirmed CF-related liver disease and those with confirmed biliary cirrhosis. Patients were classified as having CF liver disease when they met two out of the four diagnostic criteria (1—hepatomegaly and/or splenomegaly on physical examination; 2—abnormal liver function tests at three consecutive times over at least 12 months after excluding other causes of liver disease; 3—ultrasonographic evidence of liver involvement or portal hypertension or biliary abnormalities; 4—evidence of CF liver disease on liver biopsy when indicated) [21]. Most of our patients had had UDAC prescribed for a long time before entering this study and usually before the guidelines were published in 2011, so that the definition of whether or not each patient had liver disease was made based on retrospective data. We found two out of 21 (9.5%) patients had persistent abnormal liver tests plus hepatomegaly, and ten had an abnormal ultrasonographic liver aspect plus hepatomegaly or liver test abnormalities. In nine patients, it was retrospectively not possible to identify the reason(s) why they were put on UDAC.
For patients with CF, on the same day as the bone assessment, a clinical examination was performed, including measurement of anthropometrical parameters (body weight, height, arm and leg lengths, body mass index (BMI)), Tanner staging by an experienced pediatrician, and a lung function test with a spirometer (Masterscreen PFT, Jaeger, Germany) assessing forced expiratory volume in 1 s (FEV1) expressed as Z-scores [22] and as a percent predicted using the Zapletal reference equations [23]. Height and weight were expressed as Z-scores. Physical activity was not recorded. Morning fasting blood samples were drawn to measure C-reactive protein (CRP), bone markers (alkaline phosphatase [ALP], serum calcium and phosphorus, 25(OH)vitamin D, parathyroid hormone [PTH] and osteocalcin [OC]), and endocrine markers (insulin-like growth factor-1 [IGF-1], IGF-binding protein 3 [IGF-BP 3], and adiponectin (Adiponectin Elisa Kit, Thermo Fisher Scientific, Frederick, MD, USA)). Renal function was measured using the 2009 Schwartz formula.
Healthy volunteers
Each patient with CF participating in this study was matched in this hierarchical order by gender, age (± 1 year) and pubertal status (Tanner stage) to healthy volunteers (HVs) recruited concomitantly and locally in the VITADOS cohort (NTC01832623); all patients and controls were Caucasian. Briefly, this prospective study aimed to assess cardiovascular, nutritional, and bone status in healthy children and teenagers aged 10–18 years depending on their 25(OH)vitamin D levels. Since this study was not designed to evaluate adipose tissue biomarkers and lung function, they were not measured.
Bone assessment using HR-pQCT and parameter analysis
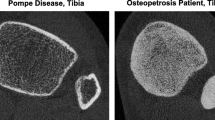
HR-pQCT (Scanco Medical AG, Brüttisellen, Switzerland) was performed on the nondominant arm and leg. Volumetric BMD (vBMD) and microstructure (see below) were measured at the distal radius and tibia using a scanner that acquires a stack of 110 parallel CT slices with an 82-μm isotropic voxel size, 9.5 and 22.5 mm from a reference line manually placed at the endplate of the radius and tibia, respectively, as previously described in teenagers whose growth plates are fused [13]. In children with open tibial and radial growth plates, the reference line was placed on the scan image at the proximal end of the growth plate [16, 17]. The outcome variables used in our analyses included vBMD (mg HA/cm3) for total (Total vBMD), trabecular (Tb.vBMD), and cortical (Ct.vBMD) areas; geometry of bone: total, trabecular, and cortical areas (Total, Tb, and Ct Areas, mm2); trabecular and cortical thickness (Tb Thickness and Ct Thickness, μm); and trabecular microstructure: trabecular number (Tb Number, /mm), thickness (Tb Thickness, μm), separation (Tb Separation, μm), and intraindividual distribution of separation (Tb Distribution, μm). HR-pQCT measurements were taken at the nondominant limb unless there was a history of fracture. HR-pQCT raw data were used for comparison between patients with CF and HVs.
Statistical analysis
Based on data published in patients suffering from chronic kidney disease [17], the sample size calculation indicated that 36 subjects per group would be required to demonstrate a 10% difference between HVs and patients for total tibial vBMD, with an 80% power and a 5% α risk.
The demographic, clinical, and biological characteristics of the CF patients and HVs were described using absolute and relative frequencies for categorical variables and median [range] for quantitative variables. Because the number of patients was low for some Tanner stages, we choose to group Tanner stages I with II and III (which corresponds to the ascendant phases of bone mass acquisition velocity), and Tanner stages IV and V (which corresponds to bone mass acquisition velocity decrease) [24].
Statistical analyses were performed with the SPSS 17.0 software. The Wilcoxon test was used to perform between-group (CF patients versus HVs) median comparisons. Within the CF group of patients, nonparametric Mann–Whitney tests were performed in subgroups of patients with CF to assess gender, steroid intake, fracture history, genotype, and the impact of comorbidities on HR-pQCT outcomes. Eventually, Spearman bivariate analysis was used to evaluate correlations between bone microstructure parameters and demographic, clinical, and biological characteristics. Multivariable analyses were performed using a backward stepwise analysis whenever needed.
Results
Characteristics of patients with CF versus HVs (Table 1)
Thirty-seven patients with CF (21 boys) and 37 HVs (21 boys), with a median age of 15.4 [10.4–17.9] years and 14.4 [10.9–17.6] years, respectively, were enrolled. The following characteristics were not statistically significantly different between CF patients and HVs: body mass index Z-scores and arm and leg lengths. However, CF patients were smaller than HVs (respective height Z-scores for age − 0.6 [− 3 to 4.4] versus 0 [− 2 to 11.4], p = 0.04) and thinner (respective weight Z-scores for age − 1.1 [− 2.6 to 2.3] versus − 0.1 [− 2.7 to 5.3], p = 0.02). Both CF patients and HVs had 25(OH)vitamin D blood levels within normal ranges: 26 out of 37 (70%) patients with CF and 26 out of 37 (70%) HVs had 25(OH)vitamin D blood levels above 30 nmol/L. Although 25(OH)vitamin D levels were similar, patients with CF displayed significantly greater PTH levels. Eight CF patients (22%) had a past history of fracture (collarbone, humeral head, wrist, kneecaps, ankle, foot, and toes), including two patients at multiple sites, while 13 HVs (35%) had fracture including seven at multiple sites.
Main characteristics of patients with CF (Table 2)
Almost all patients displayed pancreatic insufficiency. Their median FEV1 value was above 90% predicted (91% [46–138]), 17 patients (46%) had used inhaled corticoids for at least three consecutive months during the 12 months preceding bone assessment, and 15 patients (40%) had used oral corticoids for at least three consecutive days during the 12 months preceding bone assessment; moreover, six patients (17%) were chronically colonized by P. aeruginosa. Twenty-one patients (57%) received ursodeoxycholic acid (UDAC), including three patients (8%) with liver cirrhosis. All patients received a mean vitamin D supplementation of 2747 [751–4753] IU/day using different modalities. None received calcium supplementation.
HR-pQCT results in patients with CF compared to HVs
Overall, bone microstructure and bone volumetric densities were not statistically different between CF patients and HVs at the distal radius (Table 3). However, at the tibia, the total bone cross-sectional area (Total Area) was 11.6% lower in patients with CF in comparison to HVs (respectively, 579 [400–1087] versus 655 [445–981]; difference, − 11.6%; p = 0.03). Bone geometry was mostly affected in its trabecular component, with the trabecular area lower in CF patients (474 [320–968]) than in HVs (570 [360–898]; difference, − 16.8%; p = 0.01). However, no other significant differences were found on tibial parameters, namely for cortical thickness and density, trabecular number, separation, thickness, or distribution. We compared HR-pQCT parameters between early (Tanner I–III) and late (IV and V) puberty stages within the CF group and between CF patients and HVs. We found a trend for a better cortical vBMD at the tibial level in late Tanner stages (698 [438–868]) in comparison to early Tanner stages (579 [508–715]) (p = 0.005). Furthermore, comparing cortical vBMD between early and late Tanner stages of CF patients and HVs, no statistical differences were found.
Correlation between total tibial bone cross-sectional area and outcomes in CF patients
Since total tibial bone cross-sectional area (Total Area) was the sole HR-pQCT parameter to differ between CF patients and HVs, we wondered whether any clinical or biological parameters could predict a low tibial cross-sectional area. Using bivariate analyses, we found that age (r = 0.479), BMI (r = 0.417), adiponectin (r = − 0.355), renal function (r = 0.618), and CRP (r = 0.378) were all associated with low tibial total bone area (all p < 0.05). Backward multivariable analysis including these parameters demonstrated that only age remained a significant predictor of total tibial bone area. However, FEV1, osteocalcin, and IGF1 were not significantly correlated with tibial bone cross-sectional area.
Influence of gender, steroid intake, fracture history, genotype, and comorbidities on HR-pQCT results within the CF group
We found that there was no difference between boys and girls for the HR-pQCT results. When comparing CF patients who had received inhaled or oral glucocorticoids in the year preceding bone assessment, no significant differences were found either.
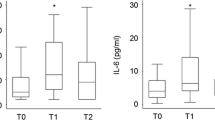
We then compared CF patients treated with UDAC (n = 21) to patients without. Three patients had liver cirrhosis and were not analyzed separately. Patients treated with UDAC surprisingly displayed significantly better tibial parameters (cortical area, total and cortical vBMD, cortical and trabecular thickness) in comparison to patients without (Fig. 1). We found a similar trend, although not statistically significant, at the radius (data not shown).
We finally explored the potential influence of the CFTR genotype on bone microstructure by comparing patients bearing two F508del mutations (n = 18) to those bearing other genotypes. Out of the nonhomozygous F508del genotype, 14 of 19 (73%) genotypes were associated with no CFTR activity, and five of 19 (27%) with a residual CFTR activity. As shown in Fig. 2, we found that at the radius, patients bearing two F508del mutations had a lower cortical BMD (621 [493–785]) than patients bearing other genotypes (715 [438–868] mg HA/cm3) (p = 0.045).
Discussion
Despite the improvement in patient care and better overall health status over the past few decades, CFBD still remains a source of concern, particularly in late adolescence and adulthood. We conducted this study to investigate bone microstructure in a cohort of well-nourished children and teenagers with CF using a high-resolution radiological tool (HR-pQCT). To the best of our knowledge, there are no other similar data published to date in these patients with CF using this tool. The main results of the present study are the following: (1) the bone microstructure of patients with CF was rather reassuring in comparison to healthy controls, although the former had smaller weight-bearing bones; (2) the CFTR genotype and UDAC administration may impact bone microstructure while corticosteroid intake or 25(OH)vitamin D circulating levels do not.
Bone microstructure assessed with HR-pQCT in young patients with CF in comparison to healthy volunteers
We found an 11% significant difference in tibial area between CF patients and HVs. CF patients had smaller tibial bones, with significantly decreased total and trabecular areas in the tibia without total, trabecular, or cortical vBMD alterations. Furthermore, at the tibial level, there were no significant differences in cortical thickness and density, trabecular numbers, separation, thickness, or distribution. These results only shared a few similarities with those reported in a similar study conducted in a cohort of 30 adult patients [14]. They found smaller cross-sectional radial and tibial areas, as well as lower vBMD. Furthermore, the microstructure was compromised at both levels, albeit most importantly in its tibial trabecular component (similar to our results). The results were unchanged after adjustment for BMI. The authors concluded that the bone strength at the tibia may be lower in CF patients than in the general population. It is unlikely that these discrepancies between our studies are related to methodological or analysis issues. Indeed, in the present study, patients and HVs were well matched (albeit not perfectly) for age, Tanner stages, height, arm and leg length, and BMI. Furthermore, HVs were recruited locally and concomitantly. It is more likely that bone microarchitecture alterations in patients with CF worsen with age, as is known for the overall bone status during CF and reported in longitudinal studies using DXA [4, 6]. In this cross-sectional study, the limited differences found between HVs and CF patients are relatively reassuring. The observation of significantly decreased trabecular and total areas in CF patients (without any significant differences with HVs for absolute height) may nevertheless reflect moderate bone fragility in CF patients. However, determining whether or not this observation can increase the risk of fracture over the long term warrants further longitudinal studies.
Our patients were well nourished and had good lung function, making secondary worsening factors less plausible in explaining the smaller bones in our patients. We suggest that part of the alterations of bone microarchitecture observed could be directly related to the basic CFTR defect and that as a “second hit,” secondary factors such as increased inflammatory status or decreased physical activities could worsen the primary bone deficit. This has been evidenced through other HR-pQCT bone studies in CF adults [13, 15] and several experimental results [2, 6, 8, 25,26,27].
Factors that impact bone microstructure
Animal studies (mainly from murine models) have shown that bone microstructure abnormalities may be influenced by gender and more pronounced in males than in females [28, 29]. In contrast, a recent study using pQCT conducted in a cohort of 97 children and young adults with CF showed greater alteration of bone microstructure in females than in males [18]. We wondered whether this could also be the case in our young patients with CF, but we found no gender differences on any of the HR-pQCT parameters studied. We must acknowledge that the low number of patients in each gender may have been insufficient to reach the needed statistical power.
In the recently published study by Putman et al., a correlation was found between bone microarchitecture and percent predicted FEV1 in a cohort of young adult patients [14]. This was not found in the present study, but this discrepancy is easily explained by our overall healthier pediatric population. Their FEV1 was within a close range, with a normal median FEV1 (91%) that contrasted with the mean FEV1 of 73.2 ± 28.2% in Putman’s series.
Finally, we did not find that recent oral or inhaled corticosteroid administration altered bone microstructure. This result is in agreement with Putman et al.’s paper: although they recorded lifetime corticosteroid exposure, they did not find a worsened effect on bone microarchitecture [14].
Bone health and UDAC administration
More surprisingly and unexpectedly, our patients receiving UDAC displayed significantly better bone microstructure parameters. It is noteworthy that these patients were similar to those without UDAC treatment in terms of pubertal stages (results not shown). Liver disease and cirrhosis are well-known risk factors of low bone mineralization [30]. Although this study was not powered to specifically address the relationship between bone and liver (meaning that the statistical significance observed may be related to type 2 error due to the small sample size), we believe that this result may be of interest to physicians. In fact, patients were classified as having CF liver disease when they met two out of the four diagnostic criteria [21], but only three of them were cirrhotic. Liver disease may be heterogeneous in its clinical, biological, and radiological manifestations, ranging from chronic liver test abnormalities to liver cirrhosis. In this way, the impact on nutritional and bone status may be very different. The only common point within this group of patients was the UDAC treatment. These results will first need to be specifically addressed in an adequately powered study. If replicated, the pivotal question that will remain to be answered is whether the observed “bone benefit” is related to liver disease alone (unlikely) or to UDAC administration (more likely). In this setting, it is noteworthy that recent results described UDAC as an inhibitor of osteoblastic apoptosis in vitro [31]. This hypothesis deserves future investigation, from both basic and clinical research perspectives, to evaluate the potential therapeutic advantage of UDAC on bone homeostasis in patients with CF and in those with other pathological conditions associated with bone fragility.
CFTR genotype–bone phenotype correlation
This study is actually the only one to identify a genotype–bone phenotype correlation at the radius for certain bone microstructure parameters. Patients bearing homozygous F508del mutations had a significantly lower radial cortical BMD and thickness. It should be noted that patients bearing two F508del mutations had pubertal stages similar to the other mutations groups (results not shown). To our knowledge, only one previous study has shown a genotype–phenotype correlation between bone and CFTR genotype: lower femoral and vertebral BMD measured by DXA were found in CF patients with at least one F508del mutation, compared to CF patients with other mutations, regardless of pancreatic or vitamin D insufficiency [32]. Our results will of course need to be replicated in a larger population of patients with CF with a clear determination of the predicted CFTR residual activity and the primary objective to study the bone phenotype–genotype correlation.
Vitamin D–calcium–PTH axis homeostasis in patients with CF
We found that PTH levels were higher in CF patients as compared to the age-, gender-, and puberty-matched HVs. Hyperparathyroidism has already been described in CF. Vitamin D deficit is highly prevalent in the CF population and may explain high PTH levels as a physiological response to vitamin D deficiency [8, 33, 34]. In our study, despite similar and normal vitamin D levels, CF patients had higher (albeit within the normal range) PTH levels than HVs. The phosphorus level was normal in CF patients and HVs, the calcium level was higher in HVs (probably due to a nonsignificant increase of protein levels in HVs), but the interpretation was limited by the lack of urinary calcium and phosphorus results. In accordance with vitamin D-independent hyperparathyroidism, we did not find any relation between PTH and vitamin D levels in bivariate analysis but an inverse association between PTH and inflammation (data not shown). However, when performing multivariable analyses (of limited value because of the small number of patients), CRP and vitamin D were the only predictors of PTH levels in CF patients (data not shown).
One explanation for these higher PTH levels in patients with CF may be the consequence of the acid–base imbalance. Indeed, the calcium-sensing receptor (CaSR) is a well-known regulator of PTH secretion, whose three-dimensional structure and consequently function is dependent on extracellular pH. Metabolic acidosis rapidly inhibits the CaSR, which causes PTH release and “hyperparathyroidism” [35, 36]. Moreover, in animal osteoblast-like cells, metabolic acidosis upregulates PTH binding and PTH receptors [37]. In the present study, we did not specifically measure the acid–base balance. However, CF patients displayed lower plasma bicarbonate concentrations than controls, corresponding to a compensatory mechanism of metabolic acidosis. This will require further investigation, but such modifications in the CaSR may explain these differences in PTH levels observed between CF patients and HVs.
Strengths and limitations of the study
The major strength of this study is that it is the first to describe bone microstructure in a cohort of children and teenagers with CF matched to their healthy counterparts recruited concomitantly and living in nearby geographic areas. Limitations were related to the cross-sectional design of the study, the relatively small size of the sample of patients (thus limiting more detailed subgroup analysis), and the likelihood of being underpowered for comparisons within the CF patient subgroup. The present results may likely not be generalizable to the entire CF population, since these patients were relatively healthy children and teenagers. Moreover, even though there is no statistical difference for age between patients and controls, the matching between the two populations was not perfect (CF patients were older and smaller than HVs). However, we believe that this limitation is not clinically meaningful in view of the results observed, namely the absence of significant differences in bone microstructure between HVs and CF patients. Last, it would have been useful to evaluate the relationship between nutritional (fat and lean masses) and bone status more thoroughly; however, we are limited in this analysis because we do not have concomitant DXA data in both the healthy and CF subjects.
Conclusion
We found that the bone microstructure was rather reassuring in children and teenagers with CF, who displayed only mild lower tibial cross-sectional areas. The long-term clinical significance of this finding will need to be studied over time however. As a research tool, HR-pQCT offers valuable additional information to DXA on bone quality and strength.
References
Paccou J, Zeboulon N, Combescure C et al (2009) The prevalence of osteoporosis, osteopenia, and fractures among adults with cystic fibrosis: a systematic literature review with meta-analysis. Calcif Tissue Int 86:1–7. doi:10.1007/s00223−009−9316−9
Le Heron L, Guillaume C, Velard F et al (2010) Cystic fibrosis transmembrane conductance regulator (CFTR) regulates the production of osteoprotegerin (OPG) and prostaglandin (PG) E2 in human bone. J Cyst Fibros 9:69–72. doi:10.1016/j.jcf.2009.11.005
Stalvey MS, Clines GA (2013) Cystic fibrosis-related bone disease: insights into a growing problem. Curr Opin Endocrinol Diabetes Obes 20:547–552. doi:10.1097/01.med.0000436191.87727.ec
Sermet-Gaudelus I, Castanet M, Retsch-Bogart G, Aris RM (2009) Update on cystic fibrosis-related bone disease: a special focus on children. Paediatr Respir Rev 10:134–142. doi:10.1016/j.prrv.2009.05.001
Reix P, Bellon G, Braillon P (2009) Bone mineral and body composition alterations in paediatric cystic fibrosis patients. Pediatr Radiol 40:301–308. doi:10.1007/s00247−009−1446−8
Sermet-Gaudelus I, Souberbielle JC, Ruiz JC et al (2007) Low bone mineral density in young children with cystic fibrosis. Am J Respir Crit Care Med 175:951–957. doi:10.1164/rccm.200606−776OC
Stahl M, Holfelder C, Kneppo C et al (2016) Multiple prevalent fractures in relation to macroscopic bone architecture in patients with cystic fibrosis. J Cyst Fibros Off J Eur Cyst Fibros Soc. doi:10.1016/j.jcf.2016.06.004
Aris RM, Merkel PA, Bachrach LK et al (2005) Guide to bone health and disease in cystic fibrosis. J Clin Endocrinol Metab 90:1888–1896. doi:10.1210/jc.2004−1629
Sermet-Gaudelus I, Bianchi ML, Garabédian M et al (2011) European cystic fibrosis bone mineralisation guidelines. J Cyst Fibros 10(Supplement 2):S16–S23. doi:10.1016/S1569−1993(11)60004−0
Stephenson A, Jamal S, Dowdell T et al (2006) Prevalence of vertebral fractures in adults with cystic fibrosis and their relationship to bone mineral density. Chest 130:539–544. doi:10.1378/chest.130.2.539
Bacchetta J, Boutroy S, Delmas P-D, Cochat P (2009) Nouvelles techniques d’imagerie osseuse: application chez l’enfant atteint de maladie rénale chronique. Arch Pédiatrie 16:1482–1490. doi:10.1016/j.arcped.2009.08.004
De Schepper J, Roggen I, Van Biervliet S et al (2012) Comparative bone status assessment by dual energy X-ray absorptiometry, peripheral quantitative computed tomography and quantitative ultrasound in adolescents and young adults with cystic fibrosis. J Cyst Fibros 11:119–124. doi:10.1016/j.jcf.2011.10.004
Gensburger D, Boutroy S, Chapurlat R, et al (2016) Reduced bone volumetric density and weak correlation between infection and bone markers in cystic fibrosis adult patients. Osteoporos Int 1–11. doi: 10.1007/s00198-016-3612-9
Putman MS, Milliren CE, Derrico N et al (2014) Compromised bone microarchitecture and estimated bone strength in young adults with cystic fibrosis. J Clin Endocrinol Metab 99:3399–3407. doi:10.1210/jc.2014−1982
Putman MS, Greenblatt LB, Sicilian L, et al (2016) Young adults with cystic fibrosis have altered trabecular microstructure by ITS-based morphological analysis. Osteoporos Int 1–9. doi: 10.1007/s00198−016−3557-z
Bacchetta J, Fargue S, Boutroy S et al (2010) Bone metabolism in oxalosis: a single-center study using new imaging techniques and biomarkers. Pediatr Nephrol 25:1081–1089. doi:10.1007/s00467−010−1453-x
Bacchetta J, Boutroy S, Vilayphiou N et al (2011) Bone assessment in children with chronic kidney disease: data from two new bone imaging techniques in a single-center pilot study. Pediatr Nephrol 26:587–595. doi:10.1007/s00467−010−1745−1
Kelly A, Schall J, Stallings VA, Zemel BS (2016) Trabecular and cortical bone deficits are present in children and adolescents with cystic fibrosis. Bone 90:7–14. doi:10.1016/j.bone.2016.04.030
Bishop N, Arundel P, Clark E et al (2014) Fracture prediction and the definition of osteoporosis in children and adolescents: the ISCD 2013 Pediatric Official Positions. J Clin Densitom 17:275–280. doi:10.1016/j.jocd.2014.01.004
Guañabens N, Parés A (2010) Liver and bone. Arch Biochem Biophys 503:84–94. doi:10.1016/j.abb.2010.05.030
Debray D, Kelly D, Houwen R et al (2011) Best practice guidance for the diagnosis and management of cystic fibrosis-associated liver disease. J Cyst Fibros 10:S29–S36. doi:10.1016/S1569−1993(11)60006−4
Quanjer PH, Stanojevic S, Cole TJ et al (2012) Multi-ethnic reference values for spirometry for the 3–95 year age range: the global lung function 2012 equations. Eur Respir J 40:1324–1343. doi:10.1183/09031936.00080312
Zapletal A, Paul T, Samánek M (1977) Significance of contemporary methods of lung function testing for the detection of airway obstruction in children and adolescents (author’s transl). Z Für Erkrank Atmungsorgane 149:343–371
Hui SL, Perkins AJ, Harezlak J et al (2010) Velocities of bone mineral accrual in black and white American children. J Bone Miner Res 25:1527–1535. doi:10.1002/jbmr.43
Sands D, Mielus M, Umławska W et al (2015) Evaluation of factors related to bone disease in Polish children and adolescents with cystic fibrosis. Adv Med Sci 60:315–320. doi:10.1016/j.advms.2015.05.002
Velard F, Delion M, Le Henaff C et al (2014) Cystic fibrosis and bone disease: defective osteoblast maturation with the F508del mutation in cystic fibrosis transmembrane conductance regulator. Am J Respir Crit Care Med 189:746–748. doi:10.1164/rccm.201312−2144LE
Street ME, Spaggiari C, Ziveri MA et al (2006) Analysis of bone mineral density and turnover in patients with cystic fibrosis: associations between the IGF system and inflammatory cytokines. Horm Res 66:162–168. doi:10.1159/000094143
Pashuck TD, Franz SE, Altman MK et al (2009) Murine model for cystic fibrosis bone disease demonstrates osteopenia and sex-related differences in bone formation. Pediatr Res 65:311–316. doi:10.1203/PDR.0b013e3181961e80
Le Henaff C, Gimenez A, Haÿ E et al (2012) The F508del mutation in cystic fibrosis transmembrane conductance regulator gene impacts bone formation. Am J Pathol 180:2068–2075. doi:10.1016/j.ajpath.2012.01.039
Luxon BA (2011) Bone disorders in chronic liver diseases. Curr Gastroenterol Rep 13:40–48. doi:10.1007/s11894−010−0166−4
Ruiz-Gaspà S, Dubreuil M, Guañabens N et al (2014) Ursodeoxycholic acid decreases bilirubin-induced osteoblast apoptosis. Eur J Clin Investig 44:1206–1214. doi:10.1111/eci.12355
King SJ, Topliss DJ, Kotsimbos T et al (2005) Reduced bone density in cystic fibrosis: ΔF508 mutation is an independent risk factor. Eur Respir J 25:54–61. doi:10.1183/09031936.04.00050204
Greer RM, Buntain HM, Potter JM et al (2003) Abnormalities of the PTH-vitamin D axis and bone turnover markers in children, adolescents and adults with cystic fibrosis: comparison with healthy controls. Osteoporos Int 14:404–411. doi:10.1007/s00198−003−1388−1
West NE, Lechtzin N, Merlo CA et al (2011) Appropriate goal level for 25-hydroxyvitamin d in cystic fibrosis. Chest 140:469–474. doi:10.1378/chest.10−2114
Campion KL, McCormick WD, Warwicker J et al (2015) Pathophysiologic changes in extracellular pH modulate parathyroid calcium-sensing receptor activity and secretion via a histidine-independent mechanism. J Am Soc Nephrol JASN 26:2163–2171. doi:10.1681/ASN.2014070653
López I, Aguilera-Tejero E, Estepa JC et al (2004) Role of acidosis-induced increases in calcium on PTH secretion in acute metabolic and respiratory acidosis in the dog. Am J Physiol - Endocrinol Metab 286:E780–E785. doi:10.1152/ajpendo.00473.2003
Disthabanchong S, Martin KJ, McConkey CL, Gonzalez EA (2002) Metabolic acidosis up-regulates PTH/PTHrP receptors in UMR 106–01 osteoblast-like cells. Kidney Int 62:1171–1177
Acknowledgements
The authors would like to thank the patients and families for their enthusiastic and active participation in this study. We also thank Marie Perceval for setting up and managing the database and Véronique Delaup for managing the patients and families.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the local institutional review board (Comité de Protection des Personnes Lyon Sud Est II, #2012-029-2). Written informed consent was obtained from all parents and patients before enrollment.
Funding
Institutional funding for this study was provided by l’Appel D’Offre Jeune Chercheur des Hospices Civils de Lyon (P. Reix, 2011). Institutional funding for the VITADOS cohort was provided by the Programme Hospitalier de Recherche Clinique (PHRC) Interrégional (J. Bacchetta, 2011).
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Braun, C., Bacchetta, J., Braillon, P. et al. Children and adolescents with cystic fibrosis display moderate bone microarchitecture abnormalities: data from high-resolution peripheral quantitative computed tomography. Osteoporos Int 28, 3179–3188 (2017). https://doi.org/10.1007/s00198-017-4179-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4179-9