Abstract
Summary
This study showed that bisphosphonate was safe and effective for the treatment of bone disorders in stage 4 chronic kidney disease (CKD) rats. Intermittent teriparatide therapy showed an anabolic action on bone even under secondary hyperparathyroidism conditions without having an adverse effect on mineral metabolism in late-stage CKD.
Introduction
Patients with late-stage CKD are at high risk for fragility fractures. However, there are no consensus on the efficacy and safety of osteoporosis medications for patients with late-stage CKD. In the present study, we aimed to examine the efficacy and safety of alendronate (ALN) and teriparatide (TPD) for treating bone disorder in late-stage CKD with pre-existing secondary hyperparathyroidism using a rat model of CKD.
Methods
Male 10-week-old Sprague-Dawley rats were subjected to a 5/6 nephrectomy or sham surgery and randomized into the following four groups: sham, vehicle (saline subcutaneous (sc) daily), ALN (50 μg/kg sc daily), and TPD (40 μg/kg sc daily). Medications commenced at 24 weeks of age and continued for 4 weeks. Micro-computed tomography, histological analysis, infrared spectroscopic imaging, and serum assays were performed.
Results
Nephrectomized rats developed hyperphosphatemia, secondary hyperparathyroidism (SHPT), and high creatinine, equivalent to CKD stage 4 in humans. ALN suppressed the bone turnover and increased the degree of mineralization in cortical bone, resulting in an improvement in the mechanical properties. TPD further increased the bone turnover and significantly increased the degree of mineralization, micro-geometry, and bone volume, resulting in a significant improvement in the mechanical properties. Both ALN and TPD had no adverse effect on renal function and mineral metabolism.
Conclusions
BP is safe and effective for the treatment of bone disorders in stage 4 CKD rats. Intermittent TPD therapy showed an anabolic action on bone even under SHPT conditions without having an adverse effect on mineral metabolism in late-stage CKD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with chronic kidney disease (CKD) have a 2- to 14-fold higher fracture risk than that of the general population [1, 2], and the incidence of fracture increases as the CKD stage increases [3, 4]. Because patients with CKD experience fractures more frequently than expected from bone mineral density-based predictions [5–7], the increased fracture risk in patients with CKD is attributable to bone quality abnormalities in addition to bone loss. Previous studies demonstrated that the abnormal mineral metabolism caused by CKD, termed CKD-related mineral and bone disorder (CKD-MBD) [8], leads to secondary hyperparathyroidism (SHPT) with vitamin D insufficiency, increased fibroblast growth factor 23 (FGF-23), and hyperphosphatemia, resulting in abnormal bone turnover and mineralization.
A problem in the management of osteoporosis in CKD is that the information regarding the safety and efficacy of osteoporosis medications is lacking, especially for patients with CKD stages 4 and 5 (late stage) who are more susceptible than patients with CKD stages 1–3 to fragility fractures. Although anti-osteoporotic agents, such as bisphosphonate (BP) or teriparatide (TPD), reduce the fragility fracture risk among patients with mild CKD [9], the safety and efficacy of BP and TPD for late-stage CKD (stages 4 and 5) patients are not entirely clear because clinical trials have not been performed on patients with CKD stages 4 and 5 due to safety concerns. Therefore, the data obtained from an animal study examining the effects of these medications on CKD-MBD should provide important information that will help establish a treatment strategy for osteoporosis in patients with late-stage CKD.
In the current study, we investigated the efficacy and safety of BP and TPD for the treatment of hyperparathyroid bone disease in late-stage CKD using a rat 5/6 nephrectomy model and focused on how BP and TPD improve bone quality, including material properties and structural properties, and on whether intermittent TPD therapy shows an anabolic effect on bone under SHPT conditions.
Materials and methods
Animal model and experimental design
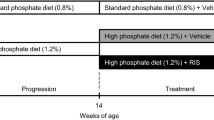
All animal studies were performed in accordance with protocols approved by the Hokkaido University Committee on Animal Resources. Male Sprague-Dawley rats (n = 24; 8 weeks of age; CLEA Japan Inc., Tokyo, Japan) were maintained at 20 °C on a 12-h light/dark cycle with free access to water and rat food containing 0.98% calcium (Ca) and 0.80% inorganic phosphorus (IP) (Labo MR Stock; Nosan Corporation Life-Tech Department, Yokohama, Japan). Following a 1-week adaptation period to the new environment, all rats were stratified according to body weight and underwent a two-third left nephrectomy. Two weeks after the first surgery, a right nephrectomy or sham operation (sham) was performed [10]. After the two-stage 5/6 nephrectomy surgeries, all rats were randomized into three groups within each stratum according to the following treatments: vehicle control group (n = 6), alendronate (ALN) group (n = 6), and TPD group (n = 6) (Fig. 1). ALN (LKT Laboratories Inc., MN) at a dosage of 50 μg/kg/day was administered to the animals by daily subcutaneous injection. Recombinant human TPD (Forteo®; Eli Lilly Ltd., Kobe, Japan) at a dosage of 20 μg/kg/day was administered to the animals by twice-daily subcutaneous injections (total 40 μg/kg/day). These doses were selected based on previous studies [11, 12]. Sham-operated controls also received vehicle treatment.
Serum chemistry tests
Serum chemistry tests were performed using the blood collected at 24 weeks of age (the onset of treatment) and at 28 weeks of age (the time of sacrifice). Serum was separated from the blood taken from fasted animals via centrifugation (30 min, 3000 rpm) at 4 °C and stored in single-use aliquots at −80 °C until analysis. Blood urea nitrogen (BUN), creatinine (CRE), and IP levels were measured using enzymatic methods. Ca levels were measured by the o-cresolphthalein complexone method. FGF-23 and intact-parathyroid hormone (i-PTH) levels were measured using an enzyme-linked immunosorbent assay (ELISA) kit.
Biomechanical testing
A three-point bending breakdown test was performed on the femoral shaft using a load mechanical universal testing machine (RTC-1310, AND Corp., Tokyo, Japan). The femur was placed with its anterior surface facing upward on the two lower support bars that were 14 mm apart. The load was applied at a rate of 0.2 mm/min until breakage. The ultimate load (N) and stiffness (N/mm) were calculated from the load-deformation curve. The load-displacement data were normalized to obtain intrinsic material properties, such as ultimate stress and elastic modulus, which are independent of cross-sectional size and shape [13, 14].
Micro-computed tomography analysis
The right femur and fifth lumbar vertebral body were scanned individually by micro-computed tomography (CT) (R_mCT2; Rigaku, Tokyo, Japan) at a 20-μm isotropic resolution. For the femur, a 2000-μm area of interest of 100 slices that encompassed the distal metaphysis, starting from 500-μm proximal to the growth plate, was used to assess the bone morphology. For the lumbar vertebral body, an area from the upper growth plate to the lower growth plate was used to assess the trabecular bone morphology.
Trabecular bone parameters of the distal femur and vertebral body, including the volumetric bone mineral density (vBMD), trabecular bone volume fraction (BV/TV), trabecular number (TbN), and trabecular thickness (TbTh), were determined using TRI/3D–BON software (Ratoc System Engineering Co., Tokyo, Japan) in accordance with the guidelines described by Bouxsein et al. For cortical bone analysis of the distal femur, the cortical thickness (CtTh) and polar moment of inertia (J) were determined [15].
Histology and histomorphometry
For dynamic bone formation analysis, calcein (20 mg/kg; Dojindo Laboratories, Kumamoto, Japan) was injected subcutaneously at 10 and 3 days before the rat was killed. The femora were fixed in 70% ethanol and stained with Villanueva bone stain. These specimens were then subjected to undecalcified tissue processing. The specimens were embedded in methyl methacrylate (MMA; Wako Chemicals, Kanagawa, Japan) and sectioned at 5 μm in the coronal plane. The distal femur was examined by fluorescence microscopy (BX53, Olympus, Tokyo, Japan) to evaluate the dynamic parameters of bone formation. Histomorphometric analysis was performed using ImageJ (NIH, Bethesda, MD). The measured parameters for trabecular bone of distal femur included total tissue volume (T. Ar), bone volume (B. Ar), osteoid volume (O. Ar), bone surface (B. Pm), osteoblast surface, eroded surface, single- and double-labeled surfaces (sL. Pm and dL. Pm, respectively), and inter-label width. These data were used to calculate the percent bone volume (B. Ar/T. Ar), percent osteoid volume (O. Ar/B. Ar), osteoblast number, osteoblast surface (Ob. Pm/B. Pm), eroded surface (E. Pm/B. Pm), mineral apposition rate (MAR), and bone formation rate (BFR/B. Pm) in accordance with the standard nomenclature proposed by Dempster et al. [16].
Fourier transform infrared spectroscopic imaging
The femora were fixed in 70% ethanol and were then subjected to undecalcified tissue processing. The specimens were embedded in MMA (Wako Chemicals, Kanagawa, Japan) and sectioned at 3 μm in the coronal plane. The sections were mounted on 1-mm thickness BaF2 window (Pier Optics, Japan) to assess bone quality by Fourier transform infrared spectroscopic (FTIR) imaging. Spectra were acquired with a Spectrum Spotlight 400 Imaging System (PerkinElmer, MA, USA), consisting of a FTIR spectrometer (Spectrum 400) and infrared (IR) microscope with a linear array mercury-cadmium-telluride (MCT) focal plane array detector. FTIR images were collected in the transmission mode at a spectral resolution of 4 cm−1 and 1 scan/pixel in the frequency region from 4000 to 680 cm−1 with an IR detector pixel size of 25 × 25 μm.
FTIR spectra were extracted from the FTIR images. After subtraction of a linear baseline and MMA spectrum, the FTIR spectrum was used to characterize the bone quality. A number of metrics related to bone biochemistry were calculated, including the mineral-to-matrix ratio [MTMR; PO4 3− (1183–985 cm−1)/amide I (1707–1599 cm−1)], which describes the degree of phosphate mineralization, and the carbonate-to-phosphate ratio [CTPR; CO3 2− (895–849 cm−1)/PO4 3− (1183–985 cm−1)], which describes the amount of carbonate substitution in the apatite crystal lattice [17].
Statistical analysis
Comparisons of data among the sham and CKD vehicle groups were performed using a Student’s t test. Comparisons of data among the CKD groups were performed using a one-way analysis of variance and Newman-Keuls tests. A significance level of P less than 0.05 was used for all comparisons. Data are represented as the mean ± standard deviation (SD). All statistical analyses were performed using GraphPad Prism version 5 (GraphPad Software, San Diego, CA, USA).
Results
Rat 5/6 nephrectomy led to CKD stage 4 in rats
When treatment commenced at 14 weeks after 5/6 nephrectomy, the serum BUN and CRE levels were significantly elevated in the CKD rats compared with the rats in the sham group. Although the serum Ca levels did not change in the CKD rats, the serum levels of IP, FGF-23, and i-PTH were significantly elevated among CKD rats compared with the rats in the sham group (Fig. 2a). These serologic data suggested that the 5/6 nephrectomized rats developed a condition equivalent to CKD stage 4 in humans in terms of renal function and mineral metabolism.
Effects of ALN and TPD treatments on renal function and mineral metabolism in 5/6 nephrectomized rats. a Serum chemistry tests for renal function (BUN, CRE) and mineral metabolism (Ca, IP, FGF-23, and i-PTH) 14 weeks after 5/6 nephrectomy showed that the nephrectomized rats developed CKD stage 4 at the start of treatment with the osteoporosis medication. b The effects of 4 weeks of treatment with ALN or TPD on renal function and mineral metabolism are shown. The ALN and TPD treatments did not worsen renal function. The ALN treatment normalized hyperphosphatemia and increased the serum levels of FGF-23 and i-PTH, albeit not in a statistically significant manner. TPD treatment showed a tendency to increase the IP levels and decrease the serum levels of FGF-23 and i-PTH, albeit not in a statistically significant manner. Values shown are the mean ± SD. *P < 0.05
Effects of BP and TPD on renal function and mineral metabolism in rats with CKD stage 4
Serum chemistry tests were performed 4 weeks after treatment with ALN or TPD to assess the effect of these medications on renal function and mineral metabolism (Fig. 2b). Neither ALN nor TPD further elevated the serum levels of BUN and CRE in the CKD rats, indicating that 4 weeks of treatment with BP or TPD did not worsen renal function. Regarding the mineral metabolism, the rats in the ALN group had decreased serum levels of Ca and IP compared with those in the vehicle group. The decrease in IP levels in the ALN group was not significant; however, the serum levels of IP in the ALN group were equivalent to those of the rats in the sham group, indicating that ALN normalized the serum IP levels. TPD did not significantly change the serum levels of Ca and IP. The FGF-23 levels tended to be increased by ALN treatment but decreased by TPD therapy (mean change of FGF-23 4 weeks after the treatment from the baseline −10.4 ± 10.6% in the vehicle group, 12.3 ± 24.3% in the ALN group, and −30.9 ± 10.5% in the TPD group). The i-PTH levels tended to increase in the ALN group but tended to decrease in the TPD group, albeit the changes were not statistically significant (mean change of i-PTH 4 weeks after the treatment from the baseline 49.3 ± 76.6% in the vehicle group, 150.2 ± 145.6% in the ALN group, and −28.6 ± 10.9% in the TPD group).
Effects of BP and TPD on biomechanical properties in rats with CKD stage 4
The biomechanical properties of the femoral shaft were evaluated by a three-point bending test (Fig. 3). The femora from the rats in the sham and vehicle groups did not exhibit any significant changes in ultimate load and in stiffness; in contrast, after the 5/6 nephrectomy, the intrinsic material properties of the femoral shaft deteriorated. Compared with the femora from the rats in the sham group, the femora from vehicle-treated CKD rats exhibited a significant decrease in elastic modulus and bending strength (P < 0.05). Treatment of the CKD rats with ALN tended to restore the intrinsic material properties, as well as the ultimate load and stiffness, albeit the improvement was not statistically significant. TPD therapy significantly increased the ultimate load, elastic modulus, and bending strength compared with those of the vehicle-treated CKD rats.
Effects of ALN and TPD treatments on the biomechanical properties of the femora in rats with CKD. Although nephrectomy did not have a significant negative impact on the ultimate load and stiffness, the intrinsic material properties, including elastic modulus and bending strength, worsened in the rats of the vehicle group compared with the rats of the sham group. Although BP showed only a tendency to increase biomechanical parameters, TPD caused a significant increase in the biomechanical parameters of CKD rats. Values shown are the mean ± SD. *P < 0.05
Effects of BP and TPD on bone volume and micro-structural properties in rats with CKD stage 4
We next evaluated the changes in bone volume and micro-structure of the distal femur and of the fifth lumber vertebral body (Fig. 4). Compared with the rats in the sham group, the nephrectomized rats had a statistically significant change in the BV/TV in the distal femur; however, there were no changes in the BV/TV in the L5 vertebral body and the vBMD and structural parameters of the trabecular and cortical bones in both the distal femur and L5 vertebral body. Compared with the rats in the vehicle group, the rats in the ALN treatment group had significantly higher BV/TV in the distal femur but did not have statistically significant changes in other bone volume and structural parameters. TPD treatment exerted a significant effect on the bone volume and structure in both the distal femur and L5 vertebral body. The rats in the TPD group had significantly higher bone density (vBMD), bone volume (BV/TV), trabecular structure (i.e., Tb. Th and Tb. N), and cortical bone structure (i.e., Ct. Th and J).
Effects of ALN and TPD treatments on the bone morphology of the femora and fifth lumbar vertebral bodies in rats with CKD. a Representative coronal cross-sectional views of micro-CT images of the distal femora 4 weeks after the treatments. b Representative coronal cross-sectional views of micro-CT images of the fifth lumbar vertebral bodies 4 weeks after the treatments. c, d The quantitative micro-CT morphometrical data of the trabecular bone and cortical bone in the distal femora and fifth lumbar vertebral bodies, respectively. The trabecular bone parameters included volumetric bone mineral density (vBMD), the trabecular bone volume fraction (BV/TV), trabecular number (TbN), and trabecular thickness (TbTh), and the cortical bone parameters included the cortical thickness (CtTh) and polar moment of inertia (J). Values shown are the mean ± SD. *P < 0.05
Effects of BP and TPD on bone metabolism in rats with CKD stage 4
To better understand the drug effects on bone metabolism in CKD rats, we performed dynamic bone histomorphometry using calcein-labeled undecalcified histological sections of the distal femur (Fig. 5). Compared with the sham rats, CKD rats did not have a significant change in B. Ar/T. Ar. ALN did not change the B. Ar/T. Ar in histology, whereas the rats in the TPD group had significantly increased B. Ar/T. Ar compared with that of the rats in the vehicle group. The osteoid, which is unmineralized bone matrix that becomes stained red-purple with Villanueva staining, was abundant in CKD rats in the vehicle group, suggesting high bone turnover in CKD rats. Although the rats in the TPD group did not have a significant change in O. Ar/B. Ar, the rats in the ALN group had significantly decreased O. Ar/B. Ar compared with the rats in the vehicle group. Analysis of bone formation and resorption parameters revealed that CKD tended to increase bone formation (i.e., Ob. Pm/B. Pm, MAR, and BFR/B. Pm) and significantly increased bone resorption (E. Pm/B. Pm) compared with the values in the sham group, indicating that CKD induces high bone turnover. Compared with the CKD rats in the vehicle group, the rats in the ALN group had significantly decreased bone formation (i.e., Ob. Pm/B. Pm, MAR, and BFR/B. Pm) and bone resorption (E. Pm/B. Pm). In contrast, the rats in the TPD group had further increased bone formation (i.e., Ob. Pm/B. Pm, MAR, and BFR/B. Pm) and decreased bone resorption (E. Pm/B. Pm) compared with those of the rats in the vehicle group.
Effects of ALN and TPD treatments on the bone metabolism in rats with CKD. a Micro-graphs showing representative coronal sections of the distal femora with Villanueva bone staining. Representative bright field micro-photographs (upper panels) and higher-magnification views (middle panels) show that osteoids, which are shown in the red-purple region, are abundant in the rats of the vehicle group. Representative fluorescence micro-graphs (lower panels) of trabecular bone obtained at 5-day intervals for double labeling with calcein green show that the rats in the vehicle group had more bone formation than the rats in the sham group; additionally, that TPD further promoted bone formation, while ALN attenuated it. b Bone histomorphometry data, including the bone volume of tissue volume (B. Ar/T. Ar), osteoid volume of bone volume (O. Ar/B. Ar), osteoblast surface (Ob. Pm/B. Pm), eroded surface (E. Pm/B. Pm), mineral apposition rate (MAR), and bone formation rate of bone surface (BFR/B. Pm), are shown. Bars = 100 μm. Values shown are the mean ± SD. *P < 0.05
Effects of BP and TPD on bone material properties in rats with CKD stage 4
To further investigate the drug effects on bone quality, we evaluated the material properties of bone using FTIR imaging (Fig. 6). CKD significantly decreased the MTMR of the center of the cortical bone in the distal femur, which indicates a reduction in the mineralization of cortical bone, and CKD decreased the CTPR of both the cortical and trabecular bone in the distal femur, which indicates the amount of carbonate substitution for phosphate or hydroxide in the mineral crystals. The decrease in the amount of carbonate substitution in the bone matrix indicates metabolic acidosis [18, 19]. The ALN treatment significantly increased the MTMR of the endosteal and periosteal regions of cortical bone. Compared with the rats in the vehicle group, the rats in the ALN group had a significantly increased CTPR of both trabecular and cortical bone, which indicates improvement of the metabolic acidosis in the rats treated with ALN. The TPD treatment significantly increased the MTMR of the cortical bone. Although the TPD treatment increased the CTPR of the trabecular bone, it did not have a significant effect on the CTPR of the cortical bone.
Effects of ALN and TPD treatments on the bone matrix quality in rats with CKD. Representative FTIR color mapping images of MTMR (PO4 3−/amide I) (a) and CTPR (CO3 2−/PO4 3−) (b) of the distal femur in the sham, vehicle, ALN, and TPD groups 4 weeks after the treatments. Comparisons of the values of MTMR (c) and CTPR (d) at the distal metaphysis of the femur are shown. The values of MTMR and CTPR were calculated separately according to the anatomical sites from the FTIR spectrum. The measured anatomical sites included the trabecular bone, center of the cortical bone, endosteal side of the cortical bone, and periosteal side of the cortical bone. Values shown are the mean ± SD. *P < 0.05
Discussion
The primary aim of this study was to elucidate the efficacy and safety of osteoporosis medications in late-stage CKD, which has not been tested in clinical trials due to safety concerns [20, 21]. In general, dietary phosphorus restriction and calcium binders are used as the initial treatments of CKD-MBD in stage 3 and 4 CKD, which were accompanied by moderately to severely reduced kidney function [22–24]. If these treatments fail to decrease i-PTH levels, active vitamin D analogs can be used as a second line of therapy [25]. Cinacalcet should be effective but is not approved for the treatment of SHPT in stage 3 and 4 CKD [26]. The problem is the uncertainty in the efficacy of these treatments for fracture prevention. In contrast, osteoporosis medications, including BP and TPD, are expected to be effective among patients with CKD stage 4 based on their proven effectiveness in fracture prevention for patients with CKD stages 1–3. If osteoporosis medications can safely be used by patients with late-stage CKD, then these should be effective treatment options, especially for the patients who have a high risk for fragility fracture due to coexisting illnesses, such as postmenopausal osteoporosis and glucocorticoid-induced osteoporosis [27].
Our data suggest that BP, which is a first-line therapy for most osteoporosis cases [28], is safe and effective for the treatment of osteoporosis in patients with CKD stage 4. Although 4 weeks of treatment with ALN only showed a tendency to have a positive impact on bone strength, FTIR imaging and micro-CT analyses demonstrated that ALN improved the material properties of cortical bone and increased the bone volume of the distal femur in the CKD rats. We believe that this improvement in bone quantity and quality reduces the fracture risk in patients with CKD and that longer-term treatment with BP may significantly increase bone strength. Regarding the safety of BP therapy, ALN did not worsen renal function to any extent. In contrast, hyperphosphatemia was improved by the ALN treatment. Furthermore, the rats in the ALN group had significantly increased CTPR of both trabecular and cortical bone compared with that of the rats in the vehicle group; thus, ALN might improve the metabolic acidosis in CKD. These results are consistent with the findings in some clinical studies showing that BP effectively reduces fracture risk without worsening renal function in patients with CKD stage 4 [29, 30].
A particularly important question addressed in this study is whether TPD therapy shows anabolic action on bone metabolism even under SHPT conditions. Our data demonstrated that intermittent TPD therapy did show an anabolic action on systemic bone metabolism even under SHPT conditions. Previous clinical studies reported that TPD therapy was effective for postmenopausal osteoporosis among patients with mild or moderate renal impairment (CKD stages 1–3) [31]; however, this is the first study to provide clear evidence of the anabolic action of TPD therapy in CKD stage 4 and under SHPT conditions. In addition to the remarkable increases in bone volume, the degree of mineralization, and micro-structure, the dynamic bone histomorphometric data support this idea.
Regarding the safety of TPD therapy, the serologic data obtained in this study showed that TPD therapy had neither a positive nor a negative effect on mineral metabolism as well as renal functions in late-stage CKD. Note, however, that 4 weeks of treatment with TPD tended to decrease serum FGF-23 levels, which may reduce phosphorus excretion, leading to exacerbation of hyperphosphatemia. As for the response of FGF-23 production to intermittent TPD therapy, however, it is inconclusive whether TPD therapy decreases serum FGF-23 levels or not. Sridharan M. et al. showed that FGF-23 increased after intermittent TPD therapy in 27 elderly women with postmenopausal osteoporosis and that there was a positive correlation between changes in bone formation maker procollagen-type 1 N-terminal propeptide (P1NP) and FGF-23 [32]. In contrast, it was demonstrated that increased bone formation down-regulates FGF-23 possibly through dentin matrix protein 1 (DMP-1) using mouse models manifesting differing degrees of coupled and uncoupled bone turnover [33]. Furthermore, transgenic expression of DMP-1 was demonstrated to reduce FGF-23 levels and to rescue the DMP-1-null animals from hypophosphatemia, suggesting that DMP-1 is likely to act as an inhibitor of FGF-23 expression [34].
There are several limitations of this study. First, we could not monitor the serum levels of vitamin D (1,25-dihydroxyvitamin D) and sclerostin, which are associated with CKD-MBD, because the amount of serum obtained from the living rats was limited. Serum concentrations of vitamin D should be decreased due to suppressed 1α-hydroxylase activity in a 5/6 nephrectomy rat model of CKD. However, changes in serum levels of vitamin D and sclerostin in response to BP or TPD treatment under the condition of CKD stages 4 and 5 should be investigated in the future study to better understand therapeutic action of these drugs on bone in patients with late-stage CKD. Second, the TPD dosage used in this study corresponds to tens or hundreds of multiples of the FDA-approved dosage of 20 μg/day for the treatment of osteoporosis. We selected the dosage of 40-μg/kg body weight TPD per day because a larger TPD dose is needed to observe significant effects in rodents, possibly due to the species difference. Finally, we did not evaluate the heterotopic mineralization of the vasculature although hyperphosphatemia induces it. It is of interest whether BP or TPD affects this mineralization. Therefore, how osteoporosis medications affect cardiovascular tissues in patients with CKD stage 4 must be evaluated in a future study.
It should be noted, however, that findings obtained in this study can be applicable to hyperparathyroid bone disease but not to other bone disorders induced by CKD-MBD. It is known that various pathologic patterns of bone remodeling are expressed in CKD including hyperparathyroid bone disease (high-turnover disease), adynamic bone disease and osteomalacia (low-turnover bone disease), and mixed uremic osteodystrophy (high-turnover plus a mineralization defect). However, a 5/6 nephrectomy rat model used in this study does simulate SHPT leading to high bone turnover condition but does not simulate other bone disorders induced by CKD-MBD. Very recently, Iwasaki et al. demonstrated that partial nephrectomy does not develop ABD but combination of partial nephrectomy and thyroparathyroidectomy induces ABD [35]. However, it is uncertain whether this model really mimics ABD or not because ABD is believed to be attributable to skeletal resistance to PTH and the pathogenesis of ABD has not been fully elucidated.
In conclusion, BP is safe and effective for the treatment of osteoporosis in stage 4 CKD rats. BP not only suppresses bone turnover but also may improve hyperphosphatemia and metabolic acidosis in CKD rats. Intermittent TPD therapy showed an anabolic action on bone even under SHPT conditions, thus resulting in remarkable increases in bone volume, the degree of calcification, and micro-geometry. Despite the excellent therapeutic efficacy of TPD in bone, the use of TPD in late-stage CKD might require careful attention because it possibly exacerbates hyperphosphatemia.
References
Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert SR, Wong C, Stehman-Breen C (2000) Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int 58:396–399
Nickolas TL, McMahon DJ, Shane E (2006) Relationship between moderate to severe kidney disease and hip fracture in the United States. J Am Soc Nephrol: JASN 17:3223–3232
Cummings SR, Black DM, Nevitt MC, Browner W, Cauley J, Ensrud K, Genant HK, Palermo L, Scott J, Vogt TM (1993) Bone density at various sites for prediction of hip fractures. The study of osteoporotic fractures research group. Lancet 341:72–75
Naylor KL, McArthur E, Leslie WD et al (2014) The three-year incidence of fracture in chronic kidney disease. Kidney Int 86:810–818
Jamal SA, Gilbert J, Gordon C, Bauer DC (2006) Cortical pQCT measures are associated with fractures in dialysis patients. J Bone Miner Res: Off J Am Soc Bone Miner Res 21:543–548
Ensrud KE, Lui LY, Taylor BC, Ishani A, Shlipak MG, Stone KL, Cauley JA, Jamal SA, Antoniucci DM, Cummings SR (2007) Renal function and risk of hip and vertebral fractures in older women. Arch Intern Med 167:133–139
Nickolas TL, Leonard MB, Shane E (2008) Chronic kidney disease and bone fracture: a growing concern. Kidney Int 74:721–731
Moe S, Drueke T, Cunningham J, Goodman W, Martin K, Olgaard K, Ott S, Sprague S, Lameire N, Eknoyan G (2006) Definition, evaluation, and classification of renal osteodystrophy: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int 69:1945–1953
Jiang Y, Zhao JJ, Mitlak BH, Wang O, Genant HK, Eriksen EF (2003) Recombinant human parathyroid hormone (1-34) [teriparatide] improves both cortical and cancellous bone structure. J Bone Miner Res: Off J Am Soc Bone Miner Res 18:1932–1941
Koyama H, Nishizawa Y, Inaba M, Hino M, Prahl JM, DeLuca HF, Morii H (1994) Impaired homologous upregulation of vitamin D receptor in rats with chronic renal failure. Am J Phys 266:F706–F712
Seedor JG, Quartuccio HA, Thompson DD (1991) The bisphosphonate alendronate (MK-217) inhibits bone loss due to ovariectomy in rats. J Bone Miner Res: Off J Am Soc Bone Miner Res 6:339–346
Xu J, Rong H, Ji H, Wang D, Wang J, Zhang W, Zhang Y (2013) Effects of different dosages of parathyroid hormone-related protein 1-34 on the bone metabolism of the ovariectomized rat model of osteoporosis. Calcif Tissue Int 93:276–287
Komatsubara S, Mori S, Mashiba T, Nonaka K, Seki A, Akiyama T, Miyamoto K, Cao Y, Manabe T, Norimatsu H (2005) Human parathyroid hormone (1-34) accelerates the fracture healing process of woven to lamellar bone replacement and new cortical shell formation in rat femora. Bone 36:678–687
Shimizu T, Takahata M, Kameda Y, Hamano H, Ito T, Kimura-Suda H, Todoh M, Tadano S, Iwasaki N (2014) Vitamin K-dependent carboxylation of osteocalcin affects the efficacy of teriparatide (PTH(1-34)) for skeletal repair. Bone 64:95–101
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Muller R (2010) Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res: Off J Am Soc Bone Miner Res 25:1468–1486
Dempster DW, Compston JE, Drezner MK, Glorieux FH, Kanis JA, Malluche H, Meunier PJ, Ott SM, Recker RR, Parfitt AM (2013) Standardized nomenclature, symbols, and units for bone histomorphometry: a 2012 update of the report of the ASBMR histomorphometry nomenclature committee. J Bone Miner Res: Off J Am Soc Bone Miner Res 28:2–17
Boskey A, Pleshko Camacho N (2007) FT-IR imaging of native and tissue-engineered bone and cartilage. Biomaterials 28:2465–2478
Green J, Kleeman CR (1991) Role of bone in regulation of systemic acid-base balance. Kidney Int 39:9–26
Yerramshetty JS, Lind C, Akkus O (2006) The compositional and physicochemical homogeneity of male femoral cortex increases after the sixth decade. Bone 39:1236–1243
Miller PD (2009) Diagnosis and treatment of osteoporosis in chronic renal disease. Semin Nephrol 29:144–155
Gordon PL, Frassetto LA (2010) Management of osteoporosis in CKD stages 3 to 5. Am J Kidney Dis: Off J Natl Kidney Found 55:941–956
Svara F (2009) Chronic kidney disease-mineral and bone disorder (CKD-MBD): a new term for a complex approach. J Renal Care 35(Suppl 1):3–6
(2009) KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney international Supplement S1–130
Ketteler M (2011) Phosphate metabolism in CKD stages 3-5: dietary and pharmacological control. Int J Nephrol 2011:970245
Melamed ML, Thadhani RI (2012) Vitamin D therapy in chronic kidney disease and end stage renal disease. Clin J Am Soc Nephrol: CJASN 7:358–365
Bolasco P (2009) Treatment options of secondary hyperparathyroidism (SHPT) in patients with chronic kidney disease stages 3 and 4: an historic review. Clin Cases Miner Bone Metab : Off J Ital Soc Osteoporos, Miner Metabol, Skelet Dis 6:210–219
Miller PD (2014) Chronic kidney disease and the skeleton. Bone Res 2:14044
Favus MJ (2010) Bisphosphonates for osteoporosis. N Engl J Med 363:2027–2035
Miller PD, Roux C, Boonen S, Barton IP, Dunlap LE, Burgio DE (2005) Safety and efficacy of risedronate in patients with age-related reduced renal function as estimated by the Cockcroft and gault method: a pooled analysis of nine clinical trials. J Bone Miner Res : Off J Am Soc Bone Miner Res 20:2105–2115
Jamal SA, Bauer DC, Ensrud KE, Cauley JA, Hochberg M, Ishani A, Cummings SR (2007) Alendronate treatment in women with normal to severely impaired renal function: an analysis of the fracture intervention trial. J Bone Miner Res : Off J Am Soc Bone Miner Res 22:503–508
Miller PD, Schwartz EN, Chen P, Misurski DA, Krege JH (2007) Teriparatide in postmenopausal women with osteoporosis and mild or moderate renal impairment. Osteoporos Int : J Established Result Cooperation Between Eur Found Osteoporos Natl Osteoporos Found USA 18:59–68
Sridharan M, Cheung J, Moore AE, Frost ML, Fraser WD, Fogelman I, Hampson G (2010) Circulating fibroblast growth factor-23 increases following intermittent parathyroid hormone (1-34) in postmenopausal osteoporosis: association with biomarker of bone formation. Calcif Tissue Int 87:398–405
Samadfam R, Richard C, Nguyen-Yamamoto L, Bolivar I, Goltzman D (2009) Bone formation regulates circulating concentrations of fibroblast growth factor 23. Endocrinology 150:4835–4845
Lu Y, Qin C, Xie Y, Bonewald LF, Feng JQ (2009) Studies of the DMP1 57-kDa functional domain both in vivo and in vitro. Cells Tissues Organs 189:175–185
Iwasaki-Ishizuka Y, Yamato H, Nii-Kono T, Kurokawa K, Fukagawa M (2005) Downregulation of parathyroid hormone receptor gene expression and osteoblastic dysfunction associated with skeletal resistance to parathyroid hormone in a rat model of renal failure with low turnover bone. Nephrol, Dial, Transplant : Off Publ Eur Dial Transplant Assoc – Eur Renal Assoc 20:1904–1911
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Ota, M., Takahata, M., Shimizu, T. et al. Efficacy and safety of osteoporosis medications in a rat model of late-stage chronic kidney disease accompanied by secondary hyperparathyroidism and hyperphosphatemia. Osteoporos Int 28, 1481–1490 (2017). https://doi.org/10.1007/s00198-016-3861-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3861-7