Abstract
Summary
Fracture liaison services often perform laboratory testing, but these results may be altered by surgery. In 40 hip arthroplasty patients, many laboratory parameters of bone health relevance were reduced by 8–22% on the first post-operative day. Laboratory results obtained in the immediate post-surgery interval do not reliably ascertain baseline status.
Introduction
As secondary causes of osteoporosis are common, fracture liaison services often perform laboratory testing in the immediate post-fracture interval. We hypothesized that laboratory results obtained shortly after surgery may not accurately ascertain baseline status. If true, such alterations might confound subsequent fracture prevention efforts.
Methods
Patients undergoing elective total hip arthroplasty were studied as a surrogate for hip fracture patients. Blood and urine were obtained 2 weeks before surgery, before anesthetic induction, on post-operative day one, and 6 weeks after surgery. Serum total and free 25-hydroxyvitamin D (25(OH)D), vitamin D-binding protein (DBP), calcium, creatinine, albumin (Alb), alkaline phosphatase (ALP), plasma hemoglobin (Hgb) and urinary DBP/creatinine ratio (UDBP/Cr) were measured.
Results
Forty volunteers (28 women; 12 men) with mean age of 65.7 [8.7] years were studied. Laboratory results were stable from 2 weeks before to the day of surgery. On the first day after surgery, total 25(OH)D, DBP, calcium, creatinine, ALP, and Alb declined 8–22% (p < 0.0001); free 25(OH)D and Hgb declined by 8 and 15% (p < 0.01), respectively; and UDBP/Cr increased 32% (p < 0.01). Using a 25(OH)D <30 ng/mL threshold, vitamin D inadequacy prevalence increased from 38% before surgery to 68% the day after (p < 0.001). All laboratory values returned to baseline at 6 weeks after surgery.
Conclusions
Laboratory values are reduced immediately following elective total hip arthroplasty. Testing at that time does not accurately ascertain baseline status and may lead to elevated estimates of vitamin D inadequacy, incorrect interventions, and misallocation of healthcare resources.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis, the loss of bone mass and microarchitectural integrity, becomes common with advancing age and heightens fragility fracture risk [1, 2]. As a result, ∼50% of women and ∼20% of men suffer an osteoporosis-related fracture in their lifetime. Fragility fractures reduce both the quality and quantity of life and account for major healthcare expenditures [3–5]. The occurrence of a fragility fracture is a strong predictor for a subsequent fracture [6], particularly in the succeeding 12 months [7]. Treatment of those who sustain fragility fractures with effective osteoporosis medications reduces future fracture risk and may decrease mortality [8, 9]. However, many persons with osteoporosis-related fractures remain untreated. Indeed, the proportion of people with a hip fracture that subsequently receive osteoporosis medications declined from ∼40% in 2002 to ∼20% in 2011 [10].
To address the osteoporosis treatment gap, the fracture liaison service (FLS) model is being implemented worldwide [11, 12]. The FLS model comprises a systematic approach that identifies fragility fracture patients, performs evaluations to diagnose and assess underlying causes of osteoporosis or fractures, and initiates appropriate treatment [13]. FLS programs are often directed by an orthopedic surgeon, teamed with a coordinator, who may be an advanced practice nurse practitioner, and other skilled staff [13, 14]. It is well established that the FLS approach reduces both fractures and healthcare expenditures [10, 14].
Many conditions are associated with bone loss and result in increased fracture risk. Individuals with such conditions are considered to have secondary osteoporosis [15]. Secondary osteoporosis is common in those who sustain fragility fracture [16]. Notably, more than half of the patients that sustained osteoporosis-related fracture may have vitamin D inadequacy and up to one third may have other secondary causes of osteoporosis [16]. As a result, FLS guidance includes post-fracture laboratory testing to identify secondary causes of bone loss [11]. In the USA, a pending Joint Commission quality measure (Osteoporosis-Associated Fracture Implementation Guide) [17] calls for performing a complete blood count, renal and hepatic function tests, serum calcium determination, and either administration of oral vitamin D or 25-hydroxyvitamin D (25(OH)D) measurement. However, physiologic changes that accompany anesthesia and surgery include blood loss, fluid shifts, autonomic imbalances, and hormonal responses that may confound interpretation of laboratory results acquired in the immediate post-surgery interval [18–20]. As a result, laboratory tests aimed at assessing potential secondary causes of osteoporosis may be altered by surgery. Nonetheless, the FLS recommendations noted above call for laboratory tests to be ordered or performed prior to discharge following hospitalization for primary repair of fragility fracture [17]. To test whether laboratory evaluations performed immediately after surgery in compliance with FLS program recommendations correspond to a patient’s true baseline status, individuals undergoing elective total hip arthroplasty were investigated as surrogates for hip fragility fracture patients, given their similar age and magnitude of surgical interventions.
Methods
Participants/study design
Adults age 50 and older with osteoarthritis scheduled for elective primary total hip arthroplasty were recruited to participate in this study. Exclusion criteria included hip arthritis from other causes, e.g., rheumatoid arthritis, surgery within the preceding 6 months, conditions/diseases known to affect vitamin D or vitamin D-binding protein (DBP) metabolism, and treatment with high-dose vitamin D.
This study was reviewed and approved by the University of Wisconsin Health Sciences Institutional Review Board (IRB). All participants signed an IRB-approved informed consent document prior to the conduct of any study procedure. Blood and urine samples were obtained 2 weeks before surgery at the time of pre-operative evaluation, the day of surgery just before anesthesia induction (pre-op), the day after surgery while still hospitalized (post-op day one), and at a scheduled clinic visit 6 weeks after surgery (post-op week six). Estimated intraoperative blood loss and intravenous (IV) fluid volume administered during surgery, in the recovery room, and over the first 24 h after surgery were obtained from electronic medical records.
Laboratory evaluation
Serum total 25(OH)D was measured by high-performance liquid chromatography (HPLC) using previously reported methods [21]. In our laboratory, this assay is traceable to the National Institutes of Standards and Technology (NIST) Standard Reference Materials as recommended [22]. The 25(OH)D intra-assay coefficient of variation (CV) ranges from 1.9% at a concentration of 61.5 ng/mL to 6.3% at a concentration of 14.3 ng/mL. The inter-assay CV is 3.2% at a 25(OH)D concentration of 59.8 ng/mL and 3.9% at a concentration of 14.3 ng/mL. Serum and urine DBP concentrations were measured by enzyme-linked immunoabsorbent assay (ELISA) (Alpco, Salem, NH) with inter- and intra-assay %CVs of 6.3 and 6.3%. Free 25(OH)D was measured by ELISA (DIAsource, Louvain-la-Neuve, Belgium). Plasma hemoglobin (Hgb) and serum creatinine, calcium, albumin and alkaline phosphatase (ALP), and urinary creatinine were measured by the UW Health clinical laboratory using Abbott Architect® (Abbott Park, IL) instrumentation.
Statistical analysis
Mixed linear model analysis was applied to evaluate the null hypothesis that there was no difference for each laboratory test among the four time points. In cases where a significant difference among time points was observed, a second test was used to compare the post-op value to the average of the other three values. The degree of association between observations at each pair of time points was described using the Pearson correlation coefficient. The significance level adopted for all comparisons was p < 0.05. This study had a >94% power to detect a difference in mean 25(OH)D of 4 ng/mL. Sample size calculations were performed using nQuery Advisor 1.0 (JD Elashoff, copyright 1995–2007).
Results
Subjects
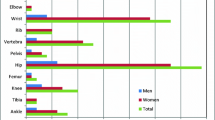
The mean (SD) age of the participants (28 female; 12 male) having elective, primary total hip arthroplasty for osteoarthritis was 65.7 (8.7) years, with a range from 53 to 83 years. Their mean (SD) body mass index (BMI) was 29.8 (6.1) kg/m2 with a range from 19.8 to 44.1 kg/m2. Thirty-four received regional anesthesia (i.e., spinal or epidural anesthesia) plus sedation (i.e., propofol), and six received general anesthesia without regional anesthesia (i.e., sevoflurane in oxygen/air, opiate, and non-depolarizing muscle relaxation). The mean (SD) operating room estimated blood loss was 296 (154) mL. The mean (SD) intravenous fluid volume administered in the operating room, post-anesthesia recovery room, and during post-operative day one was 1560 (707), 328 (320), and 834 (883) mL, respectively. Administered fluids were either normal saline or lactated Ringer’s solution. No participant received blood products. A minority (3/40) received a single unit of 5% albumin. No intraoperative or post-surgical complications were recorded, and all participants were discharged between post-operative days one to three.
Laboratory results
Laboratory values at four time intervals are noted in Table 1 and Fig. 1. Vitamin D-related laboratory values are noted in Table 2 and Fig. 2. All serum values were stable from 2 weeks before surgery to the day of surgery but declined by a mean of 7.9 to 22.4% from the day of surgery to post-op day one. The uniformity of change was noteworthy; Hgb declined in all participants, serum calcium declined in all but two, and ALP declined in all but three. The urinary DBP/creatinine ratio increased 32.0% at day one post-op (Fig. 2). No relationship between blood volume loss or IV fluid volume administered and change in laboratory parameters was observed (see Fig. 3) for the 25(OH)D data. Similarly, no significant relationship was observed between IV fluid volume administered or estimated blood loss with day one change in Hgb, creatinine, calcium, albumin, or DBP; all p values were >0.34. The small number of subjects that received general anesthesia (n = 6) limits the ability to draw conclusions regarding anesthesia approach and laboratory change. However, no difference in day one change in Hgb (p = 0.42), creatinine (p = 0.07), calcium (p = 0.16), 25(OH)D (p = 0.86), or DBP (p = 0.42) was observed. The mean (SD) serum 25(OH)D change from morning of surgery to 1 day post-operatively was −7.6 (5.2) ng/mL ranging from +0.8 to −25.4 ng/mL. As a result of these changes, if vitamin D inadequacy is defined as a serum total 25(OH)D of <30 ng/mL, ∼38% of the participants (15/40) would be classified as inadequate prior to surgery whereas ∼68% (27/40) would be identified as inadequate at day one after surgery. The prevalence of vitamin D inadequacy was 28% (11/40) at the 6-week post-operative visit. When the 6-week laboratory parameters were compared with screening values (Tables 1 and 2), no significant difference was observed for calcium (p = 0.10), creatinine (p = 0.31), albumin (p = 0.21), 25(OH)D (p = 0.95), DBP (p = 0.27), and free 25(OH)D (p = 0.77). Hgb was lower at 6 weeks than at screening, 13.1 vs. 13.8 g/dL; p < 0.0001.
Effect of hip arthroplasty on laboratory values. Serum calcium (a), hemoglobin (b), creatinine (c), and alkaline phosphatase (ALP; d) all declined at post-op day one (p < 0.01). Hgb declined in all participants, serum calcium declined in all but two, and ALP declined in all but three. Data as mean (SE)
Effect of hip arthroplasty on vitamin D-related laboratory indices. All laboratory values were significantly altered at post-operative day one. Serum total 25(OH)D (a) (p < 0.0001), vitamin D-binding protein (DBP) (b) (p < 0.0001), and serum free 25(OH)D (c) (p < 0.01) decreased. The urinary DBP/creatinine ratio (d) significantly increased (p < 0.01). Data as mean (SE)
Absence of a relationship between IV fluid volume administered estimated blood loss in operating room and change in 25(OH)D at day one post-op. The change in 25(OH)D from prior to surgery to 1 day post-operatively was unrelated to the amount of IV fluid administered in the operating room, post-operative recovery, and day following surgery (a). Similarly, change in 25(OH)D was unrelated to estimated blood loss in the operating room (b)
Discussion
Laboratory values that advocated for FLS quality metrics are uniformly and significantly reduced in the interval shortly after elective total hip arthroplasty and do not reliably reflect an individual’s baseline status. Thus, laboratory evaluation immediately following surgery to seek secondary causes of osteoporosis is likely an inappropriate use of limited healthcare resources and could lead to incorrect diagnoses and/or interventions. Decrements in laboratory values observed in this study returned to pre-operative levels at the 6-week post-surgical evaluation, suggesting that this visit may be preferred for collecting patient samples needed to identify secondary causes of osteoporosis.
Assessment of vitamin D status in fragility fracture patients is justified as up to 50% of women with hip fracture have 25(OH)D values ≤12 ng/mL, and 96% are below 32 ng/mL [23, 24]. However, recent reports of ∼20–40% decrements in serum 25(OH)D following surgery suggest that the reported prevalence of vitamin D inadequacy in post-surgical patients may not reflect their true baseline status [25, 26]. In our study, serum 25(OH)D is reduced from the pre-operative level by a mean of 21% the day after surgery (with a decrease ranging up to 34%). As a consequence, more participants, i.e., 68 vs. 38%, would be classified as vitamin D insufficient using a 25(OH)D threshold of 30 ng/mL. The reduction in total 25(OH)D observed is less than that reported after knee replacement (40%) [25] but very similar to the 18% reduction observed in 24 knee and 6 hip replacement patients [26]. Additionally, the approximate doubling of the urinary DBP/creatinine ratio is similar to that previously reported by Waldron et al. [26].
The present study differs in important ways from previous reports. No prior study documented stable laboratory values at two time points in advance of the surgery. Moreover, no prior study directly measured free 25(OH)D in the acute surgical setting. Reid et al. [25] reported calculated (not directly measured) free 25(OH)D values with ∼40% reduction on post-operative day one. However, the accuracy of calculated free 25(OH)D values has been questioned [27]. Importantly, in the present study, only participants undergoing total hip arthroplasty were enrolled, and the results were not pooled with patients undergoing a diversity of orthopedic surgeries as previously described.
The mechanism(s) of the observed changes in vitamin D-related analyte levels are unclear. Some have suggested that serum 25(OH)D is a “negative acute phase reactant” due to a correlation of increased circulating inflammatory marker levels with reduced 25(OH)D [25, 26, 28]. However, most studies report associations, i.e., a post-operative decrease in 25(OH)D correlates with the surgery-induced increase in inflammatory markers [29]. It has been hypothesized that proinflammatory cytokines could decrease 25(OH)D due to increased 1 alpha-hydroxylation [28, 30]. This possibility was not explored in this study but is worthy of further evaluation. Existing studies testing for a causal relationship between inflammation biomarkers and 25(OH)D changes are contradictory. Supporting a direct effect of inflammation is the report of a ∼30% 25(OH)D reduction in patients experiencing the acute phase response following intravenous bisphosphonate therapy [31]. Conversely, two studies of acute medical illness did not observe 25(OH)D changes but samples were obtained after illness onset [32, 33] while reduced 25(OH)D was observed in acute pancreatitis patients [34]. Such conflicting reports of decreased 25(OH) levels with medical illness (albeit limited) raise the possibility that the changes we observe are, at least in part, the consequence of surgery (e.g., blood loss) and anesthetic management rather than inflammation as the causal mechanism.
To summarize, it is unclear why 25(OH)D is reduced following surgery. Hypotheses include increased intracellular uptake and/or consumption of 25(OH)D in the immediate post-operative interval when demands for tissue regeneration are high. Additionally, increased volume of distribution, catabolism, and clearance of vitamin D-related analytes from the intravascular compartment, or increased urinary loss, are further non-exclusive potential mechanisms that await testing, particularly in view of reduced serum DBP and increased urinary DBP/creatinine ratio seen immediately after surgery. Further studies to define the mechanism(s) of the observed changes are needed [35].
Regardless of the mechanism(s) by which 25(OH)D is reduced, potential consequences of this decline are worthy of consideration. At a minimum, early post-operative 25(OH)D values should not be used as a basis upon which to initiate pharmacologic vitamin D treatment, i.e., a low value should not mandate prescription of high-dose vitamin D supplementation. Nonetheless, one could speculate that a low 25(OH)D level in the immediate post-operative interval might reflect a reduction in supply of a vitamin important in tissue repair and regeneration at a time of great demand. Consequently, we believe that this observation should not be dismissed as a laboratory phenomenon of no consequence. Indeed, a recent systematic review found that low vitamin D status is associated with adverse outcomes following surgery in 84% of 31 studies considered [36]. Of potential direct relevance to hip surgery/hip fracture patients is a report that low 25(OH)D correlated with higher rates of post-operative medical complications [37], greater duration of hospital stay [38], and, also, that low vitamin D status impairs strength recovery following orthopedic surgery [39]. One prospective study of ICU patients with 25(OH)D of ≤20 ng/mL found that high-dose vitamin D treatment did not reduce length of stay, hospital mortality, or 6-month mortality in those with less severe deficiency at baseline. However, this regimen reduced absolute risk of in-hospital mortality by 17.5% in patients with 25(OH)D levels of <12 ng/mL [40]. Whether vitamin D supplementation before, after, and even possibly during surgery has the capacity reduce complications is presently unknown; additional randomized trials to explore this possibility are clearly indicated. In the interim, as vitamin D inadequacy can promptly and safely be corrected [41], measurement of serum 25(OH)D and correction of vitamin D deficiency, when present, seem prudent prior to elective surgical procedures. Similarly, given the high prevalence of low vitamin D status among older adults, routine provision of vitamin D immediately prior to and/or following hip fracture repair is reasonable.
With regard to free 25(OH)D, the relative stability of its concentration, i.e., an ∼8% decrement vs. an ∼21% decline of total 25(OH)D, may indicate that its serum level is less affected by a reduction in circulating DBP concentration. If confirmed, and if free 25(OH)D is in fact the biologically active form of 25(OH)D, the observed increase in vitamin D inadequacy (as currently defined by measurement of total 25(OH)D) may lack profound physiologic consequences. However, such speculation is pre-mature as direct measurement of free 25(OH)D is in its infancy, and the physiologic significance of free 25(OH)D levels in plasma remains to be established.
Strengths of the present study include a prospective design that allows longitudinal documentation of laboratory results prior to surgery in the same participants, use of robust chromatographic total 25(OH)D measurements traceable to the NIST standards, ample power to detect small changes in 25(OH)D levels, and a uniform surgical procedure of comparable magnitude to that required for hip fracture repair. Several limitations are noteworthy. Patients undergoing acute hip fracture repairs were not enrolled, as it is impractical to prospectively investigate stable, baseline laboratory values before hip fracture surgical repair; thus, a surrogate surgical procedure is required. We believe that extrapolation of observations in patients undergoing elective total hip arthroplasty to post-hip fracture patients is reasonable in view of similar ages, presence of comorbidities, similar anesthetic management, and comparable magnitude of surgical intervention. Study of hip fracture patients is unlikely to add clarity as laboratory results obtained at the time of emergency department presentation are unlikely to reflect stable baseline status given variable amounts of time between fracture occurrence and initiation of medical care. Although it is unknown how well elective total hip arthroplasty for osteoarthritis models hip fracture repair, we suggest that disparities from baseline laboratory values might well be greater in hip fracture patients due to events following fracture, e.g., blood loss, dehydration, fluid shifts, pain, inflammatory changes, etc. The present investigation was not designed to resolve the time course of return of laboratory indices to baseline status in the interval between the first day after surgery and the 6-week post-operative visit. Whether levels return rapidly, slowly, or vary between patients, is amendable to further investigation and appears well warranted. Additionally, this study did not test for correlations between post-operative laboratory results and surgical outcomes. In a recent systematic review, low vitamin D status in the perioperative interval was found to be associated with multiple, severe outcomes including surgical site, periprosthetic and hospital acquired infections, decreased Harris hip scores after hip arthroplasty, and reduced quality of life scores [36].
In conclusion, multiple laboratory values decline immediately after total hip arthroplasty. In view of these data, and the data of others, we propose that laboratory evaluation for secondary causes of osteoporosis should not be performed in the immediate post-operative interval but rather should be done at a subsequent follow-up visit. We further report that serum total 25(OH) levels are at their lowest levels immediately following surgery when demands for bone, muscle, blood vessel, and skin regeneration are at their greatest. Whether or not such post-operative “vitamin D inadequacy” is compatible with optimal post-operative care is a testable hypothesis of high priority. Optimal serum 25(OH)D levels for daily life are controversial and intensely debated [42, 43]. Similarly, optimal serum 25(OH)D levels for recovery from surgery and trauma are unknown but knowable, thereby compelling prospective cohort investigation of the kinetics and dynamics of vitamin D-related analytes during surgical care.
References
Anonymous (2001) Osteoporosis prevention, diagnosis and therapy NIH consensus development panel on osteoporosis prevention, diagnosis and therapy. J Am Med Assoc 285:785–795
Leslie WD, Morin SN (2014) Osteoporosis epidemiology 2013: implications for diagnosis, risk assessment, and treatment. Curr Opin Rheumatol 26:440–446
Sattui SE, Saag KG (2014) Fracture mortality: associations with epidemiology and osteoporosis treatment. Nat Rev Endocrinol 10:592–602
Si L, Winzenberg TM, de Graaff B, Palmer AJ (2014) A systematic review and meta-analysis of utility-based quality of life for osteoporosis-related conditions. Osteoporos Int 25:1987–1997
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. Arch Osteoporos 8:136
Kanis JA, Johnell O, De Laet C et al (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int 15:175–179
Lyles KW, Colon-Emeric CS, Magaziner JS et al (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357:1799–1809
Cummings SR, San Martin J, McClung MR et al (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. [Erratum appears in N Engl J Med. 2009 Nov 5;361(19):1914] N Engl J Med 361:756–765
Solomon DH, Johnston SS, Boytsov NN, McMorrow D, Lane JM, Krohn KD (2014) Osteoporosis medication use after hip fracture in U.S. patients between 2002 and 2011. J Bone Miner Res 29:1929–1937
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24:2135–2152
Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE, McLellan A, Mitchel PJ, Silverman S, Singleton R, Siris E (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 27:2039–2046
Miller AN, Lake AF, Emory CL (2015) Establishing a fracture liaison service: an orthopaedic approach. J Bone Joint Surg Am 97:675–681
Dell R, Greene D, Schelkun SR, Williams K (2008) Osteoporosis disease management: the role of the orthopaedic surgeon. J Bone Joint Surg 90(suppl 4):188–194
Mirza F, Canalis E (2015) Management of endocrine disease: secondary osteoporosis: pathophysiology and management. Eur J Endocrinol 173:R131–R151
Bogoch ER, Elliot-Gibson V, Wang RY, Josse RG (2012) Secondary causes of osteoporosis in fracture patients. J Orthop Trauma 26:e145–e152
Commission TJ (2013) Osteoporosis-Associated Fracture Implemention Guide. The Joint Commission, Online, http://www.jointcommission.org/assets/1/6/Osteoporosis_Imp_Guide.pdf
Louw JA, Werbeck A, Louw ME, Kotze TJ, Cooper R, Labadarios D (1992) Blood vitamin concentrations during the acute-phase response. Crit Care Med 20:934–941
Navarro LH, Bloomstone JA, Auler JO Jr et al (2015) Perioperative fluid therapy: a statement from the international Fluid Optimization Group. Perioperative medicine (London, England) 4:3
Schricker T, Lattermann R (2015) Perioperative catabolism. Can J Anaesth 62:182–193
Lensmeyer GL, Wiebe DA, Binkley N, Drezner MK (2006) HPLC method for 25-hydroxyvitamin D measurement: comparison with contemporary assays. Clin Chem 52:1120–1126
Binkley N, Sempos CT (2014) Standardizing vitamin D assays: the way forward. J Bone Miner Res 29:1709–1714
LeBoff MS, Kohlmeier L, Hurwitz S, Franklin J, Wright J, Glowacki J (1999) Occult vitamin D deficiency in postmenopausal US women with acute hip fracture. J Am Med Assoc 281:1505–1511
LeBoff MS, Hawkes WG, Glowacki J, Yu-Yahiro J, Hurwitz S, Magaziner J (2008) Vitamin D-deficiency and post-fracture changes in lower extremity function and falls in women with hip fractures. Osteoporos Int 19:1283–1290
Reid D, Toole BJ, Knox S, Talwar D, Harten J, O’Reilly DS, Blackwell S, Kinsella J, McMillan DC, Wallace AM (2011) The relation between acute changes in the systemic inflammatory response and plasma 25-hydroxyvitamin D concentrations after elective knee arthroplasty. Am J Clin Nutr 93:1006–1011
Waldron JL, Ashby HL, Cornes MP, Bechervaise J, Razavi C, Thomas OL, Chugh S, Deshpande S, Ford C, Gama R (2013) Vitamin D: a negative acute phase reactant. J Clin Pathol 66:620–622
Schwartz JB, Lai J, Lizaola B, Kane L, Markova S, Weyland P, Terrault NA, Stotland N, Bikle D (2014) A comparison of measured and calculated free 25(OH) vitamin D levels in clinical populations. J Clin Endocrinol Metab 99:1631–1637
Henriksen VT, Rogers VE, Rasmussen GL, Trawick RH, Momberger NG, Aguirre D, Barker T (2014) Pro-inflammatory cytokines mediate the decrease in serum 25(OH)D concentrations after total knee arthroplasty? Med Hypotheses 82:134–137
Santonocito C, De Loecker I, Donadello K, Moussa MD, Markowicz S, Gullo A, Vincent JL (2014) C-reactive protein kinetics after major surgery. Anesth Analg 119:624–629
Barker T, Martins TB, Kjeldsberg CR, Trawick RH, Hill HR (2012) Circulating interferon-gamma correlates with 1,25(OH)D and the 1,25(OH)D-to-25(OH)D ratio. Cytokine 60:23–26
Bertoldo F, Pancheri S, Zenari S, Boldini S, Giovanazzi B, Zanatta M, Valenti MT, Dalle Carbonare L, Lo Cascio V (2010) Serum 25-hydroxyvitamin D levels modulate the acute-phase response associated with the first nitrogen-containing bisphosphonate infusion. J Bone Miner Res 25:447–454
Newens K, Filteau S, Tomkins A (2006) Plasma 25-hydroxyvitamin D does not vary over the course of a malarial infection. Trans R Soc Trop Med Hyg 100:41–44
Barth JH, Field HP, Mather AN, Plein S (2012) Serum 25 hydroxy-vitamin D does not exhibit an acute phase reaction after acute myocardial infarction. Ann Clin Biochem 49:399–401
Bang UC, Novovic S, Andersen AM, Fenger M, Hansen MB, Jensen JE (2011) Variations in serum 25-hydroxyvitamin D during acute pancreatitis: an exploratory longitudinal study. Endocr Res 36:135–141
Silva MC, Furlanetto TW (2015) Does serum 25-hydroxyvitamin D decrease during acute-phase response? A systematic review. Nutr Res 35:91–96
Iglar PJ, Hogan KJ (2015) Vitamin D status and surgical outcomes: a systematic review. Patient Saf Surg 9:14
Fakler JK, Grafe A, Dinger J, Josten C, Aust G (2016) Perioperative risk factors in patients with a femoral neck fracture - influence of 25-hydroxyvitamin D and C-reactive protein on postoperative medical complications and 1-year mortality. BMC Musculoskelet Disord 17:51
Maier GS, Maus U, Lazovic D, Horas K, Roth KE, Kurth AA (2016) Is there an association between low serum 25-OH-D levels and the length of hospital stay in orthopaedic patients after arthroplasty?. J Orthop Traumatol
Barker T, Martins TB, Hill HR, Kjeldsberg CR, Trawick RH, Weaver LK, Traber MG (2011) Low vitamin D impairs strength recovery after anterior cruciate ligament surgery. J Evid Based Complementary Altern Med 16:201–209
Amrein K, Schnedl C, Holl A et al (2014) Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. JAMA 312:1520–1530
Przybelski R, Agrawal S, Krueger D, Engelke JA, Walbrun F, Binkley N (2008) Rapid correction of low vitamin D status in nursing home residents. Osteoporos Int 19:1621–1628
Ross AC, Manson JE, Abrams SA et al (2011) The 2011 report on dietary reference intakes for calcium and vitamin D from the institute of medicine: what clinicians need to know. J Clin Endocrinol Metab 96:53–58
Holick MF, Binkley N, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 96:1911–1930
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was reviewed and approved by the University of Wisconsin Health Sciences Institutional Review Board.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Binkley, N., Coursin, D., Krueger, D. et al. Surgery alters parameters of vitamin D status and other laboratory results. Osteoporos Int 28, 1013–1020 (2017). https://doi.org/10.1007/s00198-016-3819-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3819-9