Abstract
Summary
No data on the pharmacological treatment of normocalcemic hyperparathyroidism (NPHPT) are available. We treated 30 NPHPT postmenopausal women with alendronate/cholecalciferol (treated group) or vitamin D alone (control group). Over 1 year, bone mineral density (BMD) increased significantly in treated group, but not in control group. Both treatments did not affect serum or urinary calcium.
Introduction
Normocalcemic primary hyperparathyroidism (NPHPT) is defined by normal serum calcium and consistently elevated PTH levels after ruling out the causes of secondary hyperparathyroidism. It is likely that subjects with NPHPT may develop kidney and bone disease. As no data on the pharmacological treatment of NPHPT are available, we aimed to investigate the effects of alendronate and cholecalciferol on both BMD and bone biochemical markers in postmenopausal women with NPHPT. Safety of vitamin D was evaluated as secondary endpoint.
Methods
The study was a prospective open label randomized trial comparing 15 postmenopausal women with NPHPT (PMW-NPHPT), treated with oral alendronate plus cholecalciferol (treated group) and 15 PMW-NPHPT treated only with cholecalciferol (control group). Blood samples were obtained at baseline and after 3, 6, and 12 months. Bone turnover markers (BTM) were measured at baseline, 3, and 6 months, respectively. BMD was assessed at baseline and after 12 months.
Results
After 1 year of treatment, BMD increased significantly at the lumbar, femoral neck, and hip level in the treated group, but not in the control group (p = 0.001). No differences were found between or within groups in serum calcium, PTH, and urinary calcium levels. BTM significantly decreased in the treated group but not in the control group, at 3 and 6 months (p < 0.001), respectively. No cases of hypercalcemia or hypercalciuria were detected during the study.
Conclusion
The results of this study indicate that alendronate/cholecalciferol increases BMD in postmenopausal women with NPHPT. Alendronate/cholecalciferol or vitamin D alone does not affect serum or urinary calcium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary hyperparathyroidism (PHPT) is a common endocrine disease characterized by an inappropriate elevation of the circulating parathyroid hormone (PTH) that provides stable hypercalcaemia [1]. Monoclonal parathyroid adenoma and multi-glandular hyperplasia represent the main causes of this endocrine condition [1]. The disease has been reported to affect the bone, kidney, and cardiovascular system health [2], but in recent years, its clinical scenario has completely changed. The widespread use of multi-channel biochemistry and the increasing attention paid to parathyroid pathologies are the reasons why it is increasingly frequent to find subclinical or asymptomatic forms of PHPT by accident during the biochemical screening of primarily middle-aged or elderly patient [3–5]. This subclinical form of hyperparathyroidism has been recently described as asymptomatic primary hyperparathyroidism. The Fourth International workshop for the management of asymptomatic PHPT stated that it is characterized by the lack of specific sign and/or symptoms that are traditionally associated with PTH excess or hypercalcaemia [6]. A new part of the spectrum of the asymptomatic primary hyperparathyroidism is represented by normocalcemic primary hyperparathyroidism (NPHPT). NPHPT is defined by normal total and ionized serum calcium concentrations and consistently elevated PTH levels after ruling out known causes for secondary elevations of PTH, such as renal disease or vitamin D deficiency [7–12]. It was first formally recognized at the time of the Third International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism in 2008 [7] but, due to the lack of evidence, the expert panel was not able to provide a clear guideline for its management. Although there is contrasting evidence about the metabolic consequences of NPHPT [13, 14], it is likely that subjects with NPHPT can develop kidney and bone involvement [15–20]. Charopoulos et al. demonstrated an impairment of cortical and cancellous skeleton sites in both normocalcemic and primary hyperparathyroidism even though the effect was accentuated in hypercalcemic patients [21].
In the last published guidelines for the management of PHPT, parathyroidectomy (PTX) is recommended for subjects with a BMD T-score at any of the three sites (lumbar spine, proximal femur, or forearm) of less than −2.5 SD [22]. Moreover, in subjects with mild primary hyperparathyroidism, PTX is followed by a decrease in bone turnover with an increase in bone mass, although the cortical compartment does not show any improvement in a short term [23, 24, 5].
No conclusive data are available about the treatment with vitamin D in subjects with PHPT. Although treatment with vitamin D3 [25–28] and vitamin D2 [29, 30] slightly decreases the level of PTH in patients with vitamin D deficiency, its effect on bone mineral density (BMD) and bone turnover markers (BMT) has not been well established. Only a randomized placebo controlled trial [28] together with an uncontrolled trial [31] have demonstrated a significant reduction of bone resorption markers with a parallel increase of lumbar spine BMD. Some concerns were raised on the safety of this treatment as other investigators have reported increased plasma and urine calcium levels after treatment with vitamin D [26, 29].
A few randomized controlled trials have investigated the role of anti-resorptive agents on the management of PHPT. In particular, estrogen therapy [32] and bisphosphonates [33–35, 23] were shown to increase femoral neck and lumbar spine BMD in subjects with mild primary hyperparathyroidism compared to untreated patients.
To date, no data on the pharmacological treatment of NPHPT are available.
Due to this lack of data, our study aimed to investigate the effects of oral treatment with alendronate and vitamin D on BMD and on the biochemical markers of both bone metabolism and turnover in postmenopausal women presenting with NPHPT. As a secondary endpoint we aimed to assess the safety and effects of vitamin D supplements in NPHPT patients.
Material and methods
Study design and population
The study was a prospective investigator-initiated, randomized, open parallel-group trial comparing weekly oral alendronate (70 mg) plus cholecalciferol (2800 IU) (Fosavance® 70 mg/28,000 IU, tablets) with only weekly cholecalciferol (Dibase® 10,000 IU:2800 IU = 11 drops). Thirty postmenopausal women (mean age 57 ± 4 years) with NPHPT, as defined by the Consensus Development Conference on the management of primary hyperparathyroidism [7], were enrolled (from January 2009 to March 2013). At baseline, blood samples and information on medical history, socioeconomic factors, and dietary habits (intake of milk and milk products, fish, and fruit) as well as the use of vitamin supplements were collected. In particular, dietary calcium intake was assessed by a questionnaire [36] that was completed after the first visit. Inclusion criteria were a menopausal state of at least 5 years, the presence of osteoporosis (defined by a BMD T-score at one or more skeletal sites lower than −2.5 SD), elevated serum PTH, normal values of calcium after adjustment for serum albumin, and normal vitamin serum levels (>30 ng/ml). Exclusion criteria were secondary hyperparathyroidism, concurrent systematic illness, thyroid disease, hepatic or renal dysfunction, and other disorders known to influence BMD. No patients had received estrogens, bisphosphonates, supplements of calcium and/or vitamin D or other drugs that could interfere with bone or mineral metabolism during the last 12 months. The subjects reported no personal or familial history of recurrent kidney stone disease.
Normocalcemia was defined as an adjusted plasma calcium level below the upper limit of reference range (in our lab, this is set at 10.5 mg/dl). A state of hyperparathyroidism was defined as PTH levels in the upper third of the reference interval or above (>65 pg/ml). Randomization was performed by the investigators using a computer-generated randomization code. The patients were randomized to treatment with Fosavance® (treated group, n = 15) or with cholecalciferol (control group, n = 15). To limit the potential difference in terms of bioavailability, all subjects were instructed to take either Fosavance® or cholecalciferol at the same time (in the morning 30 min before breakfast) in a fasting state. Overall dietary calcium intake was not adequate (treated group 685 mg ± 89 mg; control group 703 mg ± 12 mg, p = ns).
All patients were maintained on a controlled diet with a calcium intake of about 1000 mg/day. The study was performed in accordance with the Declaration of Helsinki II and guidelines on Good Clinical Practice. Informed consent was obtained from all the patients, and the study was approved by the local ethics committee.
Fasting blood samples for determination of serum PTH, calcium, phosphates, and 25-OH vitamin D were obtained at baseline and after 3, 6, and 12 months. Osteocalcin and urine samples for the measurement of CTX and 24-h calcium excretion were obtained at baseline and after 3 and 6 months. Serum PTH (2.1 % of intra-assay and 2.3 % of inter-assay variability) and osteocalcin (2.4 % of intra-assay and 2.2 % of inter-assay variability) were measured using chemiluminescence immunoassays (Roche Diagnostics, Mannheim, Germany) on a Modular E170. Measurements of serum calcium (1.8 % of intra-assay variability and 2 % of inter-assay variability), phosphate (2.8 % of intra-assay and 2.6 % of inter-assay variability), and 24-h urinary calcium were determined using an Olympus AU 2700 automated multichannel analyzer (Olympus, Tokyo, Japan). Calcium was corrected for serum albumin concentration according the following formula: [0.8 × (4.0 − patient’s albumin) + serum calcium]. Determination of 25-OH vitamin D (4.6 % of intra-assay variability and 5.1 % of inter-assay variability) was performed using a DiaSorin kit on a LIAISON automated immunoassay analyzer (DiaSorin, Saluggia, Italy). Urinary concentrations of the amino-terminal cross-linked telopeptides of collagen (CTX) were measured with a commercial enzyme-linked immunoassay kit (Cross Laps ELISA, Osteometer, Denmark) (3.6 % of intra-assay and 4.3 % of inter-assay variability). BMD was measured using dual-energy X-ray absorptiometry (DXA) (Hologic Discovery QDR Instrument, MA, USA). DXA was performed at the L1–L4 lumbar spine (postero-anterior projection), total hip, and femoral neck at baseline and after 12 months.
Statistical analysis
Data were analyzed using SPSS version 13.0 for Windows. Variables were expressed as mean ± SD. BMD was expressed as g/cm2 and changes in BMD were shown either as percentage change or as absolute difference between values at 12th month and baseline. Differences of data between treated and control patients at baseline were analyzed using unpaired Student’s t test, as appropriate. Changes over time for each patient were evaluated by repeated measures ANOVA for PTH, calcium, phosphate, 25-OH vitamin D, osteocalcin, urinary calcium, and CTX. Wilcoxon test was used to determine BMD variations. Differences were considered significant when p < 0.05.
Results
Baseline biochemical and BMD characteristics of the patients are displayed in Table 1; no significant differences were found between treated and control patients for PTH, calcium, phosphates, 25-OH vitamin D, and osteocalcin concentrations, as well as for 24-h urinary calcium excretion and CTX. BMD at the spine, total hip, and femoral neck was similar in both groups of patients without significant differences (Table 1).
Table 2 shows biochemical data of treated and control patients at different time points. Over all time points, both groups did not show any significant differences in serum and urinary calcium levels as well as in serum, PTH, and urinary calcium concentrations compared to baseline values (Table 2).
A small, but statistically significant, positive trend was detected for 25-OH vitamin D levels from baseline to the end of the study in the treatment group (Table 2). A similar slightly significant trend was detected for phosphate. No difference was detected between groups, at each time point, for each variable.
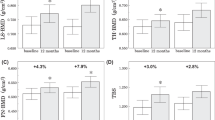
After 3 months, the treated group showed significantly decreased serum osteocalcin and urinary CTX concentrations (−46.4 and −69.4 %, respectively; p < 0.001 vs. baseline) and these values remained reduced after 6 months (−39.3 and −53.2 %, respectively; p < 0.001 vs. baseline). The control group did not demonstrate any significant change in osteocalcin and CTX concentration at any time points. A significant difference in CTX and osteocalcin levels was detected between the control and treated group both at 3 and 6 months (p < 0.001 for each comparison) (Fig. 1).
a Urinary CTX concentration at different timing in treated (□) and control (●) groups. A significant decrement compared to the baseline value (*) is observed in the group under treatment at 3rd and 6th month (p < 0.001). A significant decrement of urinary CTX concentration is observed in the group under treatment compared to the control group (°) at 3rd and 6th month (p < 0.001). b Serum osteocalcin concentration at different timing in treated (□) and control (●) groups. A significant decrement compared to the baseline value (*) is observed in the group under treatment at 3rd and 6th month (p < 0.001). A significant decrement of serum osteocalcin is observed in the group under treatment compared to the control group (°) at 3rd and 6th month (p < 0.001)
BMD values at baseline and after 12 months are reported for both groups of patients in Table 3. After a year of treatment, BMD in the treated group increased significantly at the lumbar, femoral neck, and total femur (p = 0.001).
In particular, the greatest increment was at the lumbar spine with a mean BMD increase of 4.7 % (ranging from 3.0 to 8.0 %). In the control group, a significant BMD reduction was recorded at all measured sites compared with baseline (p = 0.001). After 12 months, the alendronate plus vitamin D treatment group showed a higher significant increase of BMD (lumbar spine, femoral neck, and total femur) than the control group treated only with cholecalciferol (p = 0.001).
Discussion
This is the first study evaluating the effect of alendronate and vitamin D on patients affected by NPHPT. The underlying causes of NPHPT are still unknown but Rao et al. hypothesized that NPHPT and primary hyperparathyroidism are two phases of the same disease: the first would represent the subclinical condition and the second would be the overt disease with elevation of calcium levels [37]. Moreover, Murani et al. have shown that the resistance of kidney and bone to the actions of PTH could play an important role in the development of this subclinical condition [8].
Although the Fourth International workshop for the management of asymptomatic PHPT tries to clarify its diagnostic criteria and suggests the way to manage subjects with NPHPT, no prospective randomized controlled trials have evaluated the impact of the anti-resorptive therapy in this kind of population.
Few randomized controlled trials have investigated the role of bisphosphonates in the management of PHPT. However, Rossini et al. have demonstrated that 2 years of treatment with alendronate induced significant increases in BMD at the lumbar spine, total hip, and total body compared to control patients which showed a significant BMD reduction [33]. In another placebo-controlled trial, alendronate caused an increase in the lumbar spine and total hip BMD as well as a decrease in BMT without any changes of ionized calcium, phosphorus, and PTH [35]. Chow et al. have obtained similar results with a significant improvement of the spine and femoral neck BMD in subjects affected by PHPT after treatment with alendronate [34].
Our data have demonstrated the ability of alendronate to increase BMD in osteoporotic patients with NPHPT. As far as osteoporosis representing an indication for PTX, these findings might raise some doubts about the real need of parathyroidectomy in this group of patients. Moreover, our data seem to confirm the results of the meta-analysis by Sankaran et al. on skeletal effects of interventions in mild primary hyperparathyroidism. The authors have shown that surgical treatment and anti-resorptive therapies increase BMD in mild PHPT to a similar degree and that medical treatment could represent a reasonable option in a patient with mild hyperparathyroidism and low BMD [23]. According to other observations in primary hyperparathyroidism [38, 35], our results confirmed the effects of alendronate in decreasing both bone resorption and formation markers also in patients with NPHPT. The anti-resorptive effects of alendronate were rapidly seen within the first trimester of the study and they were sustained up to the 6th month, confirming the well-known data that are available in postmenopausal osteoporosis [39, 40].
Although treatment with vitamin D3 [25–28] and vitamin D2 [29, 30] slightly decreases PTH levels in patients with vitamin D deficiency and primary hyperparathyroidism, it is not clear whether they can be considered a valuable and safe tool to manage NPHPT due to the lack of published data in this particular disease. Only a randomized placebo controlled [28] and an uncontrolled trial [31] have demonstrated a significant reduction of bone resorption markers and an increase of lumbar spine BMD in patients with primary hyperparathyroidism treated with vitamin D. Some doubts were raised on the safety of this treatment: in fact, other investigators have reported increased plasma and urine calcium levels after treatment with vitamin D [26, 29]. In our population, the administration of vitamin D was safe and it did not induce any cases of hypercalcemia or hypercalciuria. As shown in Table 2, both plasma and urinary calcium did not significantly increase during the study and PTH was unaffected by the treatments. In contrast with patients treated with alendronate, the weekly treatment with 2800 IU of cholecalciferol in the control group was not able to arrest bone loss or to decrease BMT.
Although an alendronate alone group was not included in our study, it may be presumed that the beneficial effect seen on the BMD was entirely due to alendronate. Indeed, Macdonald HM et al. have demonstrated that, in postmenopausal women with vitamin D deficiency (at baseline), treatment with daily oral vitamin D3 at 400 IU (1 year) did not change markers of bone metabolism (CTX included) and was not able to significantly arrest the bone loss at hip compared to the treatment with 1000 IU/day [41]. Moreover, Recker et al. showed that a once-weekly tablet containing both cholecalciferol (2800 IU) and alendronate (70 mg) did not provide any further anti-resorptive improvement (evaluated by changes in bone bio-markers) compared to the single alendronate (70 mg) treatment [42].
To limit the potential difference in terms of bioavailability, all the subjects were instructed to take Fosavance® and cholecalciferol once a week, at the same time (in the morning, before breakfast) in a fasting state. Indeed, as vitamin D is liposoluble, its oral absorption could increase if ingested with a fat-rich meal [43] although there are contrasting evidences.
We found only a slight, not clinically significant change in 25-OH vitamin D levels after supplementation with cholecalciferol in the treated group. As we administered 2800 IU/week (400 IU/day) of cholecalciferol to our patients, it is reasonable to believe that they should have raised their plasma vitamin D of a small amount that would have been difficult to detect in our small groups. Indeed, it is described that 40 IU/day of vitamin D for 6 months can induce a rise in plasma 25(OH) D3 of about 0.7 ng/ml [44]. Holick et al. demonstrated that ergocalciferol can produce a significant rise in plasma 25(OH) D3 only in patients with low basal vitamin D. Our patients had normal plasma vitamin D before the study, and it is highly probable that their plasma 25(OH) D3 did not change over the study period [45]. It might be that in the control group, the compliance to the therapy was lower compared to the treated group. However, at each visit, we asked each subject to confirm they had taken the drugs as requested. Moreover, the small sample size makes further interpretation difficult.
Our study has some limitations. It was not designed as a double-blind trial, the sample size was small (even if the prevalence and incidence of NPHPT are low), and we did not measure ionized calcium nor the radius BMD. Moreover, we did not evaluate BMT at the end of the study as these measurements were only programmed after 3 and 6 months, respectively. This decision was taken in advance, as we were interested in measuring early changes of bone turnover. After having seen the unexpected increase of BMD, we realized that an evaluation of BMT at the end of the study could have added more power to our results.
In conclusion, for the first time, the results of this study indicate that in postmenopausal women with NPHPT, treatment with alendronate together with vitamin D significantly increases BMD at the most clinically relevant skeletal sites. Moreover, treatment with alendronate and/or vitamin D does not affect calcium, phosphate, and 25-OH vitamin D serum levels as well as urinary calcium excretion.
References
Fraser WD (2009) Hyperparathyroidism. Lancet 374:145–158
Cope O (1966) The study of hyperparathyroidism at the Massachusetts General Hospital. N Engl J Med 274:1174–1182
Silverberg SJ, Lewiecki EM, Mosekilde L, Peacock M, Rubin MR (2009) Presentation of asymptomatic primary hyperparathyroidism: proceedings of the third international workshop. J Clin Endocrinol Metab 94(2):351–365
Silverberg SJ1, Bilezikian JP (2006) The diagnosis and management of asymptomatic primary hyperparathyroidism. Nat Clin Pract Endocrinol Metab 2:494–503
Bollerslev J, Marcocci C, Sosa M, Nordenstrom J, Bouillon R, Mosekilde L (2011) Current evidence for recommendation of surgery, medical treatment and vitamin D repletion in mild primary hyperparathyroidism. Eur J Endocrinol 165(6):851–864
Bilezikian JP, Brandi ML, Eastell R, Silverberg SJ, Udelsman R, Marcocci C, Potts JT Jr (2014) Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the fourth international workshop. J Clin Endocrinol Metab 99:3561–3569
Bilezikian JP, Khan AA, Potts JT Jr (2009) Guidelines for the management of asymptomatic primary hyperparathyroidism: summary statement from the third international workshop. J Clin Endocrinol Metab 94:335–339
Maruani G, Hertig A, Paillard M, Houillier P (2003) Normocalcemic primary hyperparathyroidism: evidence for a generalized target-tissue resistance to parathyroid hormone. J Clin Endocrinol Metab 88(10):4641–4648
Silverberg SJ, Bilezikian JP (2003) “Incipient” primary hyperparathyroidism: a “forme fruste” of an old disease. J Clin Endocrinol Metab 88:5348–5352
Bilezikian JP, Silverberg SJ (2010) Normocalcemic primary hyperparathyroidism. Arq Bras Endocrinol Metab 54(2):106–109
Cusano N, Silverberg SJ, Bilezikian JP (2013) Normocalcemic primary hyperparathyroidism. J Clin Densitom 16:33–39
Eastell R, Brandi M, Costa AG, D’Amour P, Shoback DM, Thakker RV (2014) Diagnosis of asyntomatic primary hyperparathyroidism: proceedings of the fourth international workshop. J Clin Endocrinol Metab 99:3570–3579
Tordjman KM, Greenman Y, Osher E, Shenkerman G, Stern N (2004) Characterization of normocalcemic primary hyperparathyroidism. Am J Med 1:861–863
Garcia-Martin AR-GR, Munoz-Torres M (2012) Normocalcemic primary hyperparathyroidism: one-year follow-up in one hundred postmenopausal women. Endocrine 42:764–766
Balsa JA, Botella-Carretero JI, Peromingo R, Zamarron I, Arrieta F, Munoz-Malo T, Vazquez C (2008) Role of calcium malabsorption in the development of secondary hyperparathyroidism after biliopancreatic diversion. J Endocrinol Investig 31:845–850
Selby PL, Davies M, Adams JE, Mawer EB (1999) Bone loss in celiac disease is related to secondary hyperparathyroidism. J Bone Miner Res 14:652–657
Lowe H, McMahon DJ, Rubin MR et al (2007) Normocalcemic primary hyperparathyroidism: further characterization of a new clinical phenotype. J Clin Endocrinol Metab 92:3001–3005
Tordjman KM, Greenman Y, Osher E, Shenkerman G, Stern N (2004) Characterization of normocalcemic primary hyperparathyroidism. Am J Med 117:861–863
Amaral LM, Queiroz DC, Marques TF, Mendes M, Bandeira F (2012) Normocalcemic versus hypercalcemic primary hyperparathyroidism: more stone than bone? J Osteoporos 2012:128352
Wade TJ, Yen TW, Amin AL, Wang TS (2012) Surgical management of normocalcemic primary hyperparathyroidism. World J Surg 36:761–766
Charopoulos I, Tournis S, Trovas G, Raptou P, Kaldrymides P, Skarandavos G, Katsalira K, Lyritis GP (2006) Effect of primary hyperparathyroidism on volumetric bone mineral density and bone geometry assessed by peripheral quantitative computed tomography in postmenopausal women. J Clin Endocrinol Metab 91:1748–1753
Udelsman R, Akerstrom G, Biagini C, Duh QY, Miccoli P, Niederle B, Tonelli F (2014) The surgical managment of asyntomatic primary hyperparathyroidism: proceedings of the fourth international workshop. J Clin Endocrinol Metab 99:3595–3606
Sankaran S, Gamble G, Bolland M, Reid IR, Grey A (2010) Skeletal effects of interventions in mild primary hyperparathyroidism: a meta-analysis. J Clin Endocrinol Metab 95(4):1653–1662
Rubin MR, Bilezikian JP, McMahon DJ, Jacobs T, Shane E, Siris E, Udesky J, Silverberg SJ (2008) The natural history of primary hyperparathyroidism with or without parathyroid surgery after 15 years. J Clin Endocrinol Metab 93:3462–3470
LoCascio V, Adami S, Galvanini G, Ferrari M, Cominacini L, Tartarotti D (1985) Substrate-product relation of 1-hydroxylase activity in primary hyperparathyroidism. N Engl J Med 313:1123–1125
Grey A, Lucas J, Horne A, Gamble G, Davidson JS, Reid IR (2005) Vitamin D repletion in patients with primary hyperparathyroidism and coexistent vitamin D insufficiency. J Clin Endocrinol Metab 90(4):2122–2126. doi:10.1210/jc.2004-1772
Isidro ML, Ruano B (2009) Biochemical effects of calcifediol supplementation in mild, asymptomatic, hyperparathyroidism with concomitant vitamin D deficiency. Endocrine 36:305–310
Rolighed L, Rejnmark L, Sikjaer T, Heickendorff L, Vestergaard P, Mosekilde L, Christiansen P (2014) Vitamin D treatment in primary hyperparathyroidism: a randomized placebo controlled trial. J Clin Endocrinol Metab 99:1072–1080
Grubbs EG, Rafeeq S, Jimenez C, Feng L, Lee JE, Evans DB, Perrier ND (2008) Preoperative vitamin D replacement therapy in primary hyperparathyroidism: safe and beneficial? Surgery 144:852–858, discussion 858–859
Tucci JR (2009) Vitamin D therapy in patients with primary hyperparathyroidism and hypovitaminosis D. Eur J Endocrinol 161:189–193
Kantorovich V, Gacad MA, Seeger LL, Adams JS (2000) Bone mineral density increases with vitamin D repletion in patients with coexistent vitamin D insufficiency and primary hyperparathyroidism. J Clin Endocrinol Metab 85:3541–3543
Grey AB, Stapleton JP, Evans MC, Tatnell MA, Reid IR (1996) Effect of hormone replacement therapy on bone mineral density in postmenopausal women with mild primary hyperparathyroidism. A randomized, controlled trial. Ann Intern Med 125:360–368
Rossini M, Gatti D, Isaia G, Sartori L, Braga V, Adami S (2001) Effects of oral alendronate in elderly patients with osteoporosis and mild primary hyperparathyroidism. J Bone Miner Res 16:113–119
Chow CC, Chan WB, Li JK, Chan NN, Chan MH, Ko GT, Lo KW, Cockram CS (2003) Oral alendronate increases bone mineral density in postmenopausal women with primary hyperparathyroidism. J Clin Endocrinol Metab 88:581–587
Khan AA, Bilezikian JP, Kung AW, Ahmed MM, Dubois SJ, Ho AY, Schussheim D, Rubin MR, Shaikh AM, Silverberg SJ, Standish TI, Syed Z, Syed ZA (2004) Alendronate in primary hyperparathyroidism: a double-blind, randomized, placebo-controlled trial. J Clin Endocrinol Metab 89:3319–3325
Montomoli M, Gonnelli S, Mattei R, Cuda C, Rossi S, Gennari C (2002) Validation of a food frequency questionnaire for nutritional calcium intake assessment in Italian women. Eur J Clin Nutr 56:21–30
Rao DS, Wilson R, Kleerekoper M, Parfitt A (1988) Lack of biochemical progression or continuation of accelerated bone loss in mild asymptomatic primary hyperparathyroidism: evidence for biphasic disease course. J Clin Endocrinol Metab 67(6):1294–1298
Khan AA, Bilezikian JP, Kung A, Dubois SJ, Standish TI, Syed ZA (2009) Alendronate therapy in men with primary hyperparathyroidism. Endocr Pract 15:705–713
Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA, Satterfield S, Wallace RB, Bauer DC, Palermo L, Wehren LE, Lombardi A, Santora AC, Cummings SR, Group FR (2006) Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA 296:2927–2938
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture intervention trial research group. Lancet 348:1535–1541
Macdonald HM, Wood AD, Aucott LS, Black AJ, Fraser WD, Mavroeidi A, Reid DM, Secombes KR, Simpson WG, Thies F (2013) Hip bone loss is attenuated with 1000 UI but not 400 UI daily vitamin D3: 1 year double blind RCT in postmenopausal women. J Bone Miner Res 28:2202–2213
Recker R, Lips P, Felsenberg D, Lippuner K, Benhamou L, Hawkins F, Delmas PD, Rosen C, Emkey R, Salzmann G, He W, Santora AC (2006) Alendronate with and without cholecalciferol for osteoporosis: results of a 15 week randomized controlled trial. Curr Med Res Opin 22:1745–1755
Raimundo FV, Faulharber GA, Menegatti PK, Marques LS, Furlanetto TW (2011) Effect of high- versus low-fat meal on serum 25-hydroxyvitamin d levels after a single oral dose of vitamin D: a single-blind, parallel, randomized trial. Int J Endocrinol 2011. doi:10.1155/2011/809069.
Heaney RP, Chen TC, Holick MF, Barger-Lux MJ (2003) Human serum 25-hydroxycholecalciferol response to extended oral dosing with cholecalciferol. Am J Clin Nutr 77:204–210
Holick MF, Chen TC (2008) Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr 87:1080S–1086S
Acknowledgments
We acknowledge the “Tendi la mano-AIPOM Onlus” (an independent Italian non-profit association) which paid for the laboratory tests. We acknowledge Dr. Paul Christie for reviewing the manuscript.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Roberto Cesareo and Enrico Di Stasio contributed equally to this work.
Rights and permissions
About this article
Cite this article
Cesareo, R., Di Stasio, E., Vescini, F. et al. Effects of alendronate and vitamin D in patients with normocalcemic primary hyperparathyroidism. Osteoporos Int 26, 1295–1302 (2015). https://doi.org/10.1007/s00198-014-3000-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-3000-2