Abstract
Summary
Severe vertebral fractures strongly predicted subsequent hip fracture in this population-based study. Such high-risk patients should be provided with clinical evaluation and care for osteoporosis.
Introduction
Vertebral fractures are commonly osteoporotic and known to predict hip fracture. The aim of this study was to evaluate associations between the severity of vertebral fractures and the risk of subsequent hip fracture.
Methods
Chest radiographs were obtained of 7,095 Finnish men and women aged 30 years or over in the Mini-Finland Health Survey in 1978–1980. Record linkage to the National Hospital Discharge Register identified 182 subjects from the survey who had subsequently been hospitalized for primary treatment of hip fracture by the end of 1994. A nested case–control setting was adopted, where three controls individually matched for age, gender, and place of residence were drawn for 169 subjects with hip fracture from the same cohort. Baseline vertebral fractures were identified at levels T3 to T12, and their morphology was categorized to mild, moderate, or severe according to Genant's classification.
Results
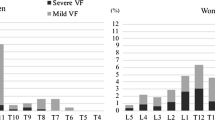
Severe vertebral fracture (>40% reduction in vertebral body height) strongly predicted hip fracture. After controlling for education, physical activity, smoking, alcohol consumption, and self-rated general health, the adjusted relative odds was 12.06 (95% confidence interval, 3.80–38.26). Mild to moderate fracture grades and the number of compressed vertebral bodies showed no prediction for hip fracture.
Conclusions
The presence of a severe vertebral fracture in the thoracic spine strongly predicts subsequent hip fracture. Such high-risk patients should be clinically evaluated and provided with care for osteoporosis and measures to reduce the risk of falling as required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis deteriorates bone tissue with a consequent increase in the fragility of bones and their susceptibility to fracture. Osteoporotic fractures result in increased mortality, many disabilities, and high economic cost. Hip fracture, the most serious outcome of osteoporosis, is becoming more frequent than before, because the world's population is aging [1]. Vertebral fractures are the most common osteoporotic fractures, but only about one third of them come to clinical attention [2]. Vertebral fractures are known to predict further vertebral and hip fractures. In large meta-analyses, the pooled estimates for the risk of a subsequent hip fracture were found to be approximately twofold in the presence of vertebral fracture [3, 4]. However, only two studies have taken account of the morphology of vertebral fractures in the prediction of hip fracture. Hasserius et al. [5] reported on the prevalence and morphology of vertebral fracture in men and women hospitalized because of a hip fracture. Schousboe et al. [6] studied the risk of future hip fracture in women over 65 years of age with mild to severe vertebral deformity. In both of these studies, the association between vertebral deformity and hip fracture was largely independent of the severity of the vertebral compression. Epidemiological research is needed to identify subjects at a high risk of disabling fractures in order to allocate the healthcare resources rationally according to the actual requirements [7].
The aim of the present study was to evaluate the association between the severity of vertebral fractures and the risk of subsequent hip fracture during a follow-up of up to 15 years in a large nationally representative population sample of men and women.
Methods
Study population and baseline examination
The Mini-Finland Health Survey [8] in 1978–1980 was based on a stratified two-stage cluster sample (N = 8,000) drawn from the population register to represent Finnish adults aged 30 years or over. In the first stage, 40 representative areas were selected. In the second stage, a systematic sample of inhabitants was drawn from each area. The subjects were interviewed at home, asked to fill in a basic questionnaire, and invited to attend a screening examination. Information was elicited on risk factors, disease histories, symptoms and signs, and findings suggestive of cardiovascular, respiratory, musculoskeletal, and other common diseases. A total of 7,217 subjects attended the baseline examination, and full-size chest radiographs (posteroanterior and lateral) were obtained from 3,280 men and 3,815 women (89% of the sample).
Definition of determinants
The subjects were asked to classify their leisure time physical activity during the usual week into one of three categories: low (walking, cycling, or similar light activities less than 3 h per week), moderate (ball games, jogging, or similar activities at least 3 h per week), and high (regular vigorous exercise). Self-rated general health was classified into good, moderate, or poor in a manner that has proved reliable in test–retest analysis [9]. Standing height and weight were measured, and body mass index (weight/height2, kg/m2) was used as a measure of relative weight. Smoking history was obtained in a standard interview and categorized as follows: never smoked, ex-smoker, or current smoker. The basic questionnaire also inquired about average weekly consumption of beer, wine, and strong beverages during the preceding month. The overall alcohol consumption was then calculated and expressed in grams of ethanol per week. The level of education was considered in three categories based on the years of education.
Follow-up
Morbidity and mortality in the cohort have been continuously followed up since the baseline examination. Information on mortality and causes of death, according to the International Classification of Diseases (ICD) codes, was obtained from Statistics Finland. Record linkage to the National Hospital Discharge Register identified 182 subjects who had been hospitalized for primary treatment of hip fracture by the end of 1994. All hip fractures as primary or secondary diagnoses were defined according to the eighth edition of the ICD, three-digit code 820.
Case–control setting and radiographic evaluation
A nested case–control setting was adopted. Two to three controls of same sex, per each hip fracture case, were drawn from the study cohort by individual matching for municipality and age. Follow-up started from the baseline examination, and the end points of follow-up were the occurrence of hip fracture, death of a subject, or the end of 1994. However, only subjects who had survived until the end of the follow-up (occurrence of hip fracture in matched case or end of the follow-up period) were considered potential candidates for the control group. Their age was not allowed to diverge more than 9 years from that of the case in question. No acceptable control was found for 13 cases, and these were consequently excluded from the study population. There were nine cases with only one matched control and eight cases with two matched controls. VP read the baseline chest radiographs without any information about the subsequent hip fracture status of the subjects. Vertebral fractures were identified at levels T3–T12. The severity of each vertebral compression was measured and graded as normal (grade 0), mildly deformed (grade 1, 20–25% reduction of anterior, middle, and/or posterior vertebral body height), moderately deformed (grade 2, 26–40% reduction in any height), and severely deformed (grade 3, over 40% reduction in any height) according to Genant's classification [10]. The final case–control set consisted of 169 cases and 485 controls.
In the mid thoracic region, over 99% of the vertebrae could be assessed for fractures. For the upper thoracic spine and the thoracolumbar junction, the proportions of vertebrae that could be assessed for fracture were as follows: T3, 84%; T4, 95%; T11, 99%; and T12, 94%.
We compared the results of the current semiquantitative (SQ) evaluation with the diagnoses of vertebral fractures made by two clinical radiologists at the time of the baseline examination [11]. The severity of the vertebral compression was not graded for these baseline diagnoses. The agreement between the clinical diagnoses at the baseline and the present SQ readings showed a kappa value of 0.40 for mild to moderate vertebral compression and 0.45 for severe compression. The modest kappa values presumably resulted from rather poor sensitivity of the clinical readings; the radiologists failed to identify almost half of the fractures identified by the SQ readings. This finding agrees with the results presented by Gehlbach et al. [12], indicating that clinical radiologists missed half of the moderate and severe fractures identified by the SQ method from chest radiographs.
Statistical analysis
The conditional logistic model was used to estimate the strength of associations between vertebral fractures and the risk of hip fracture. Level of education, physical activity, smoking, alcohol consumption, and self-rated general health were entered into the model as potential confounding or effect-modifying factors. Relative odds with 95% confidence intervals (CIs) were computed for subgroups of vertebral deformity. Statistical Analysis System (SAS) software (SAS Institute, Gary, North Carolina) was used for statistical analysis.
Ethical aspects
This study precedes current legislation on medical research. Thus, participants were fully informed about the study; they attended it on a voluntary basis, and the use of the collected information for medical research was explained to them.
Results
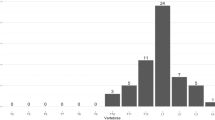
The study population comprised 36 men and 133 women with incident hip fracture and 100 and 385 individually matched controls, respectively. Their age at the baseline examination (during which the vertebral fractures were identified from chest radiographs) ranged from 32 to 91 years (mean, 67; SD, 9.7). The mean age of the cases at the time of hip fracture was 73.0 (SD, 11.8) in men and 78.5 (SD, 7.7) in women, and the mean interval between the radiography and the subsequent hip fracture was 9.5 (SD, 4.8) years in men and 8.9 (SD, 4.3) years in women. The mean age of the five controls with severe vertebral fractures ranged between 64 and 75 years (mean, 68.8). Other baseline characteristics of the cases and controls are described in Table 1.
The presence of severe vertebral compression (>40% reduction in vertebral body height) strongly predicted hip fracture. After controlling for education, physical activity, smoking, alcohol consumption, and self-rated general health, the adjusted relative odds was 12.06 (95% confidence interval, 3.80–38.3). Mild to moderate grades showed no prediction for hip fracture (Table 1). The adjusted relative odds for hip fracture in the presence of severe vertebral fracture was 8.15 (95% CI, 1.48–44.85) in those below the median of age (<72 years) and 24.66 (95% CI, 2.90–210.0) in those above the median (72 years or more). None of the interaction terms of vertebral fracture and age, sex, or any confounding factor mentioned in Table 1 showed statistical significance for prediction of hip fracture. After excluding the first 5 and 10 years of the follow-up, the corresponding relative odds was 10.56 (95% confidence interval, 2.79–39.9) and 6.77 (95% confidence interval, 1.62–28.2), respectively.
Of the incident cases with hip fracture, 43, 27, 9 and 2 had compressions in one, two, three, and four vertebral bodies, respectively. After controlling for Genant's severity grade, the adjusted relative odds of hip fracture per increment of one compressed vertebra was 1.22 (95% CI, 0.79–1.88; p value for trend, 0.37). Neither did the sites of the vertebral fractures show any association with the hip fracture risk.
Discussion
Summary
Our study showed that a severe thoracic vertebral fracture is a strong predictor of subsequent hip fracture, whereas mild or moderate fractures and the number of compressed vertebrae proved to be much weaker predictors far from being statistically significant.
Validity of the data
The strengths of this study were the large and nationally representative population sample and the exceptionally high participation rate. Our study population is therefore likely to be devoid of any selection bias due to health status. No association was found between severe vertebral fractures and illnesses predisposing to osteoporosis or osteolysis, such as cancer, chronic inflammatory bowel diseases, or other conditions that require regular corticosteroid use (data not shown). Determinants of vertebral fractures and associated mortality among adult Finns have been described previously [11]. The Finnish National Hospital Discharge Register, operating since 1967, contains records from every hospital in the country, including ICD codes of primary and secondary diagnoses. This register is the oldest nationwide discharge register in the world, and it has been shown to cover acute severe injuries adequately and record them accurately [13, 14]. Because hip fracture is severely incapacitating and painful, practically all patients with this condition are likely to be admitted to hospital for acute care.
A limitation of our study was that only the thoracic spine could be evaluated. Our material does not, therefore, include lumbar and cervical vertebral fractures. The thoracic spine and the thoracolumbar junction presumably are the principal sites of osteoporotic vertebral fractures [15, 16]. Nevertheless, it should be pointed out that the distributions of vertebral fractures differ between diagnostic methods. The semiquantitative method shows a large peak of vertebral fractures at the middle thoracic spine, which differs from the distributions found by means of both the algorithm-based qualitative method (ABQ) and the clinical diagnosis. Also, by using the SQ method, fractures identified in radiographic follow-ups are likely to show a different distribution than prevalent fractures identified by the same method. Concerning the identification of vertebral fractures, the SQ method is more sensitive than the clinical diagnosis but obviously less specific than the ABQ method [17]. The SQ method is based on apparent vertebral height reduction, whereas the ABQ method diagnoses vertebral fractures on the basis of endplate depression regardless of the reduction in vertebral height. The SQ method may therefore more easily misdiagnose low-height vertebrae without endplate depression (degenerative changes or normal variations) as vertebral fractures [17–19].
Another limitation of our study was that detailed information on the types of accident, which had led to the hip fractures, was available for only one fourth of the cases. However, none of these fractures were related to a high-energy accident.
Comparison with previous data
In the present study, smoking and low body mass index were associated with the risk of hip fracture, whereas physical activity provided protection against it. This conforms to previous literature on the risk factors for osteoporosis. Vertebral fractures are known to predict hip fractures [3–6], and this association was also evident in the present study. Hasserius et al. reported on the prevalence and morphology of vertebral deformities in male and female patients with hip fracture [5] from a study in which two population-based materials served as controls. The association between vertebral deformity and hip fracture was stronger in severe vertebral deformities, although the odds ratios were far less than twofold compared with mild vertebral deformities. Schousboe et al. [6] reported about associations of at least 10-year-old vertebral deformities with ensuing hip fractures in women over 65 years of age. The mean follow-up period in their study was 13 years. In that study, the risk ratio for hip fracture was less than twofold in subjects with mild to severe vertebral deformity compared with those showing no deformity in the same study population. To our knowledge, associations between vertebral fracture severity and subsequent hip fracture risk as strong as those found in the present study have so far not been published.
The difference in the results between previous studies and our study may have several explanations. The study populations differ from each other. Hasserius et al. [5] recruited mentally capacitated subjects who were admitted to hospital during the daytime selectively from one Swedish region only, whereas Schousboe et al. [6] studied only women over 65 years of age. The nationally representative sample of men and women with a wider age range in our study may offer a more solid basis to evaluate the association and to generalize about the results. The long follow-up of our cohort may have revealed hip fractures sensitively, whereas selective mortality may lead to weaker associations in cross-sectional studies. We evaluated only the thoracic spine from chest radiographs, whereas both of the prior studies identified vertebral deformities of the whole spine. The definitions of vertebral fracture morphology were similar in all of these studies. Our findings agree with those of Ferrar et al. and Jiang et al. [17–19] suggesting that non-osteoporotic low-height vertebrae may be misdiagnosed as vertebral fractures. Such misdiagnosis is especially likely in mild to moderate deformity which showed no prediction for hip fracture in the present study. Severe vertebral compressions, on the other hand, are more likely to be true osteoporotic fractures of the spine.
The clinical diagnosis of osteoporosis is currently based on the measurement of bone mineral density (BMD) using dual X-ray absorptiometry (DXA) [20]. BMD predicts osteoporotic fractures with a gradient of risk ranging from about 1.5 to 3.0 for each standard deviation decrease in BMD [21]. It is important to identify subjects at a high risk of disabling fractures and to provide them with targeted treatment and care that meets their individual needs. WHO has estimated that, in a few decades, most hip fractures will occur in developing countries in which DXA measurements are not generally available.
Conclusions
Chest radiography should not be performed in order to diagnose osteoporosis. However, if a severe vertebral fracture is identified from a chest radiograph, such finding obviously indicates a substantial risk of subsequent hip fracture. We recommend urgent clinical evaluation of such high-risk patients in order to offer them treatment, care, and follow-up as indicated.
References
Cummings SR, Melton LJIII (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Cooper C, Atkinson EJ, O’Fallon WM, Melton LJIII (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota 1985-1989. J Bone Miner Res 7:221–227
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Haentjens P, Autier P, Collins J, Velkeniers B, Vanderschueren D, Boonen S (2003) Colles fracture, spine fracture, and subsequent risk of hip fracture in men and women, a meta-analysis. J Bone Joint Surg 10:1936–1943
Hasserius R, Johnell O, Nilsson BE et al (2003) Hip fracture patients have more vertebral deformities than subjects in population-based studies. Bone 32:180–184
Schousboe JT, Howard AF, Li-Yung L, Taylor BC, Ensur KE (2006) Association between prior non-spine non-hip fractures or prevalent radiographic vertebral deformities known to be at least 10 years old and incident hip fracture. J Bone Miner Res 21:1557–1564
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Aromaa A, Heliövaara M, Impivaara O et al (1989) Health, functional limitations and need for care in Finland. Basic results from the Mini-Finland Health Survey. Publications of the Social Insurance Institution AL32, Helsinki, in Finnish with English Summary
Martikainen P, Aromaa A, Heliövaara M et al (1999) Reliability of perceived health by sex and age. Sos Sci and Med 48:1117–1122
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Puisto V, Rissanen H, Heliövaara M, Knekt P, Helenius I (2008) Mortality in the presence of a vertebral fracture, scoliosis, or Scheuermann’s disease in the thoracic spine. Ann Epidemiology 18:595–601
Gehlbach SH, Bigelow C, Heimisdottir M, May S, Walker M, Kirkwood JR (2000) Recognition of vertebral fracture in a clinical setting. Ostoporos Int 11:577–582
Sund R, Nurmi-Lüthe I, Lüthe P, Tanninen S, Narinen A, Keskimäki I (2007) Comparing properties of audit data and routinely collected register data in case of performance assessment of hip fracture treatment in Finland. Methods Inf Med 46:558–566
Keskimäki I, Aro S (1991) Accuracy of data on diagnosis, procedures and accidents in the Finnish Hospital Discharge Register. Int J Health Sci 2:15–21
Gallacher SJ, Gallagher AP, McQuillian C, Mithchell PJ, Dixon T (2007) The prevalence of vertebral fracture amongst patients presenting with non-vertebral fractures. Osteoporos Int 18:185–192
El Maghraoui A, Mounach A, Gassim S, Ghazi M (2008) Vertebral fracture assessment in healthy men: prevalence and risk factors. Bone 43:544–548
Jiang G, Eastell R, Barrington NA, Ferrar L (2004) Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int Nov 15:887–896
Ferrar L, Jiang G, Armbrecht G, Reid DM et al (2007) Is short vertebral height always an osteoporotic fracture? The Osteoporosis and Ultrasound Study (OPUS). Bone 41:5–12
Ferrar L, Jiang G, Cawthon PM et al (2007) Identification of vertebral fracture and non-osteoporotic short vertebral height in men: the MrOS study. J Bone Miner Res 22:1434–1441
Cummings SR, Black DM, Nevitt MC et al (1990) Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. JAMA 263:665–668
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936, Review
Acknowledgements
This study has been supported by the Finnish National Institute for Health and Welfare, Finnish Foundation for Paediatric Research, Finnish Orthopaedic Research foundation, Finnish Medical Foundation, Medronic International, and Baxter Finland.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Puisto, V., Heliövaara, M., Impivaara, O. et al. Severity of vertebral fracture and risk of hip fracture: a nested case–control study. Osteoporos Int 22, 63–68 (2011). https://doi.org/10.1007/s00198-010-1195-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1195-4