Abstract
Introduction and hypothesis
Female stress urinary incontinence (SUI) is a prevalent condition, and conservative treatment options are needed. Were evaluated CO2 laser and radiofrequency as treatment for SUI.
Methods
One hundred thirty-nine women with SUI were eligible and randomized in a three-arm double-blind randomized controlled trial into radiofrequency (RF), laser (LS) and sham control (SCT) groups, with 3-monthly outpatient treatment sessions. One hundred fourteen women were included, 38 in each group, during a 12-month follow-up.
The primary outcomes were: subjective improvement of SUI, evaluated on a Likert scale, and objective cure, which was a composite outcome defined according to negative stress tests, voiding diary and pad test. Questionnaires were also applied. The sample size was calculated to provide 80% power to identify a 20% difference between groups, p < 0.05.
Results
Subjective improvement and objective cure of SUI were identified respectively in 72.6% and 45.2% in LS and in 61.7% and 44.7% in RF, both significantly higher than the 30.0% and 14.0% in SCT. Considering only mild cases (pad test < 10 g), objective cure was achieved in 66.7% in LS, 63.6% in RF and 22.2% in SCT. Significant reduction in the number of episodes of urinary incontinence was found according to voiding diaries (p = 0.029) and pad weight (p = 0.021). A significant reduction in urgency and urinary loss during sexual intercourse was observed only with LS and RF. Improvement in quality of life was also verified by the I-QoL and ICIQ-SF in favor of the energy-treated groups.
Conclusions
CO2 laser and radiofrequency are outpatient options for SUI treatment, with no major complications. They had similar results and presented better results than in the sham control group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Female urinary incontinence (UI) is a highly prevalent condition that results in worsening of quality of life [1]. Several factors, such as aging, pregnancy, vaginal delivery, menopause and loss of collagen, may contribute to UI [1, 2]. Stress urinary incontinence (SUI) is defined as a sign and symptom of involuntary loss of urine on effort or physical exertion [3]. It affects 50% of all incontinent women.
In the absence of pelvic organ prolapse, conservative treatments for SUI, such as behavioral changes and physiotherapy, achieve up to 70% continence [4]; however, many women discontinue pelvic floor exercises after a few weeks, so surgery using polypropylene meshes has been considered the gold standard treatment [5].
Currently, there are concerns about the use of polypropylene due to postoperative chronic pain, mainly for the transobturator route. In addition, an increase in bladder perforation, major vascular or visceral injury and suprapubic pain, more related to the retropubic approach, was reported after the dissemination of this technique [6].
Within this scenario, alternative therapies have emerged. The use of vaginal energy in genitourinary syndrome of menopause (GSM) has shown promising results with consistent improvement in symptoms [7, 8]. Based on this, some authors suggested the use of laser (LS) for UI treatment [9, 10]. Another option to deliver energy to tissues is microablative fractionated radiofrequency (RF), a more accessible and less expensive technology than lasers. The use of radiofrequency for the treatment of UI and GSM has also already been described with good results [11, 12].
The aim of this study was to evaluate the use of LS and RF for SUI treatment compared to a sham control group (SCT).
Methods
This is a prospective double-blind randomized study to compare the efficacy of CO2 laser and RF compared to a SCT group for the treatment of SUI (LARF study-arm 3). It was conducted at the Sector of Urogynecology and Vaginal Surgery, Hospital São Paulo and Federal University of São Paulo, a tertiary referral academic center, after receiving the approval of the Institutional and National Ethics Committee. The study was registered at Brazilian National Clinical Trials (REBEC RBR-33jphr).
Women referred for SUI were eligible for the study, as confirmed by a stress test. Exclusion criteria were: the presence of urgent urinary incontinence [3] or pelvic organ prolapse beyond the hymen; use of medication for overactive bladder syndrome or vaginal estrogen therapy in the prior 6 months or diuretics; active infection of urinary tract or with HPV or herpes; abnormal vaginal bleeding; previous surgical SUI treatment or pelvic radiotherapy.
After providing written informed consent, women were randomized to be in the CO2 laser, RF or SCT group (allocation ratio 1:1:1). Block randomization was performed using a computerized random number generator (Microsoft® Excel), and the list was kept by the nurse in charge of the protocol, who scheduled the treatment sessions [13].
The pre- and posttreatment protocol included complete urogynecology history, gynecological examination, supine and standing cough stress test (performed with comfortably full bladder), 1-h pad-test [3], 7-day voiding diary [3], quality of life evaluation using the Incontinence Quality of Life Questionnaire (I-QoL) [14], International Consultation on Incontinence Questionnaire–Short Form (ICQ-SF) [15] and the Female Sexual Function Index (FSF-I) [16] validated for the Portuguese language. Participants’ subjective impression of improvement regarding SUI was also evaluated using a Likert scale (1 = much worse, 2 = worse, 3 = neutral, 4 =better, 5 = much better).
The severity of UI was classified by pad test weight as mild (< 10 g), moderate (11–50 g) or severe (> 50 g) [3]. Women were also classified by reported symptoms into pure SUI or predominant SUI when, in addition to SUI as their main complaint, they reported associated symptoms such as urgency or nocturia.
All participants received behavioral orientations at the first visit, including guidance on water intake and urinary frequency to prevent incontinence. All participants and the outcome assessors were blinded to the intervention group, and only the physician who performed the treatment application was aware of it.
The outpatient basis procedures were performed from August 2018 to September 2019. The treatment protocol included three subsequent monthly energy application sessions, lasting 15 min each. With the patient in gynecological position, after antisepsis, 2% lidocaine gel was applied to the vaginal introitus, and then after 10 min the vaginal epithelium was moistened with saline solution for RF and dried with gauze for laser. The probe was activated all over the vaginal walls, starting from the proximal third to the introitus, making matrix lines on all vaginal walls, and a second time between 10 and 2 o’clock positions addressing the suburethral area, by direct vision, using a vaginal speculum for RF and by rotating and pulling the vaginal probe according to the equipment orientation marks for laser.
The equipment used in the radiofrequency group was a Wavetronic™ 6000 Touch System with MegapulseHF FRAXX™, using a LINLY™ fractionated vaginal probe, manufactured by Loktal Medical Electronics (São Paulo, Brazil). The vaginal probe had 64 microneedles (800 μm long, 200 μm diameter) distributed in an 8 × 8 matrix, and the needles were separated from each other by 1.27 mm. The 4-MHz generator was configured to Fraxx mode, low intensity mode, with an activation time of 40 ms, power of 45 watts and 70.3 mJ/cm2 fluency, as recommended by the manufacturer. The electromagnetic energy shots were controlled by randomizer software and distributed for all 64 needles of the Linly™ probe, making a matrix of 64 microablations.
The equipment used in the laser group was Alma-Femilift™ (Nuremberg, Germany) adjusted for mode medium, 1 Hz, 100 W potency and 100 mJ/1.0 cm2 fluency, as recommended by the manufacturer. CO2 laser energy is delivered to the vaginal tissue through a holographic lens that pixelates the beam to 81 microscopic pixels in a 9 × 9 ablation pattern.
Participants in the SCT group underwent the same procedures; however, the equipment was blocked and could not release energy. The equipment’s display remained on, and sounds were emitted by pressing a pedal to ensure participant blinding.
Intraprocedural pain was evaluated by the end of each session by the visual analog scale (VAS) of pain (0–10).
Follow-up visits occurred at 1, 6 and 12 months after the procedure. Complications were assessed between treatment sessions and in all follow-up visits by clinical evaluation including physical examination.
The primary outcome was the participants’ subjective impression of improvement in SUI, defined as “better” or “much better” on the Likert scale. Objective cure was a composite outcome, defined when the women presented three negative tests: stress test (tested with comfortably full bladder in a gynecological and standing position), pad test and an absence of any urinary leakage in the 7-day voiding diary. These outcomes were also evaluated according to the severity of incontinence, menopausal status and type of incontinence.
Other secondary outcomes were the impact of the procedures on their quality of life (ICIQ-SF and IQol), sexual function (FSF-I), presence of urinary loss during intercourse and presence of associated symptoms such as urgency and nocturia.
The sample size was calculated to provide 80% power to identify a 20% difference between groups, considering a urinary incontinence improvement of 75% [17] with a 0.05 significance level. Therefore, a sample size of 36 participants per group was necessary. Anticipating 15% drop-out or loss to follow-up, at least 42 women per group should be included. Intention-to-treat analysis was used, so cases with loss to follow-up or cases with treatment drop-out were considered treatment failures [13].
Statistical analysis was performed using Minitab Statistical Software (V19 Minitab, LLC, State College, PA, USA). Normality of data was assessed. ANOVA and Kruskal-Wallis tests were used for continuous variables, and chi-square tests were used for categorical variables. McNemar was used to compare differences during the follow-up time of categorical variables. Mixed-model ANOVA was used to compare groups and their evolution during the follow-up time, where G = group, T = time and G*T = interaction factor. A post hoc Tukey’s test was used when a significant difference in the interaction factor was identified. The cut-off point of p < 0.05 for statistical significance was used.
Subjective improvement and objective cure results were also described by intention-to-treat (ITT) and per protocol (PP) analysis.
Results
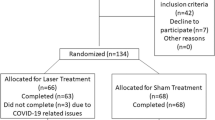
A total of 153 women with SUI were enrolled, and 139 were randomized to have CO2 laser (42), RF (47) or to SCT (50). A total of 114 women, 38 in each group, reached the 12-month follow-up (Fig. 1: consort flow chart).
The groups were similar regarding demographic and clinical pretreatment parameters (Table 1).
Subjective improvement rates at the 12-month follow-up, ITT and PP, respectively, were better in the laser (76.2% and 84.2%) and RF (61.7% and 76.3%) than in the SCT group (30.0% and 39.5%) (p = 0.01), mainly among premenopausal women and cases of pure SUI (Table 2).
A significant difference (p < 0.05) was also observed regarding objective continence rates with better results associated with the energy-treated groups, laser (45.2% and 50.0%) and RF (44.7% and 55.2%) than with SCT (14.0% and 18.4%), ITT and PP, respectively (Table 3). In addition, significantly better objective cure rates were mainly related to mild cases, premenopausal women and pure SUI.
A significant reduction in pad test weight (p < 0.05) was observed, and the groups were different (p = 0.03) at the 12-month evaluation. A similar result was achieved in relation to the number of episodes of urinary loss, with a significant reduction (p < 0.05) and differences between groups at the 12-month follow-up evaluation (p = 0.04). The energy-treated groups presented better findings, with similar results between them, when compared to the SCT group (Table 4).
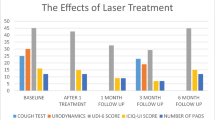
There was a significant improvement in quality of life, revealed by a reduction in I-QoL and ICIQ-SF scores after treatment (p < 0.001), with similar scores between the groups before treatment (A: Tukey-test) but with differences after treatment (I-QoL p = 0.018; ICIQ-SF p = 0.019). The laser and RF group results were similar (B: Tukey’s test) and different from the SCT group (C: Tukey’s test) at the 12-month follow-up evaluation (Table 4).
Nonetheless, no significant difference regarding sexual function, evaluated by the FSF-I, was demonstrated in any group before or after treatment (group p = 0.269), and no change was demonstrated in FSF-I after treatment (p = 0.216), which means that most women remained classified as having sexual dysfunction by presenting an FSF-I score < 26.55 (Table 4). In addition, a discrete increase in the number of sexually active women was observed at 12-month follow-up in the laser (28/38 to 30/38) and radiofrequency (24/38 to 27/38) groups but not in the sham control group (26/38 to 26/38).
The frequency of associated symptoms during the follow-up, such as urgency, nocturia and urinary loss in intercourse, also showed a significant reduction (Fig. 2). Frequency of urgency was similar between groups pretreatment (p = 0.53) but was significantly different (p = 0.01) at 12-month follow-up. Nocturia rates were similar between groups pre- (p = 0.53) and post-treatment (p = 0.06). The groups presented a similar frequency of urinary loss during intercourse pre-treatment (p = 0.67), but it was significantly different at the 12-month follow-up (p < 0.01), with significant reduction of this symptom in energy-treated groups but not in the SCT group (Fig. 1).
The pain related to the procedures was moderate (VAS scores > 3 and < 7) in all groups without differences among them. All women tolerated the procedure-related pain and completed the treatment. The pain occurred mainly during manipulation of the distal third of the vagina. The pain reported by the laser group (4.5 ± 2.3) did not differ from that of the other groups, but the reported pain was greater in the radiofrequency group (5.4 ± 2.1) than in the SCT group (4.2 ± 2.3) (p = 0.019). Pain was not related to age or hormonal status.
Mild vaginal bleeding immediately after the treatment sessions was reported (LS 29.0%, RF 36.0%, SCT 24.0%), and it was reduced as the treatments progressed (LS 8.0%, RF 5.0%, SCT 0%). Dysuria was reported mainly after the first application (LS 23.0%, RF 5.0%, SCT 1.0%) and did not occur after the third session in any group. No urinary infection or vaginal mucosa scarification or fibrosis was observed.
Discussion
This RCT evaluating the use of intravaginal energy to treat SUI has shown that CO2 laser and microablative radiofrequency are outpatient options, with not only subjective improvement but also an objective cure being achieved with no major complications. Both energy release forms had similar results and presented better outcomes compared to the sham control group.
The subjective improvement identified in the energy-treated groups was noteworthy, and it has been one of the most valued aspects in clinical trials recently. Furthermore, the results agreed with what was shown in the voiding diary and with previously described case series of both laser and radiofrequency treatment [10, 11, 17]. Moreover, an objective cure using strict criteria, the major strength of the study, was also demonstrated by a 12-month follow-up.
Recently, with increasing concern about the use of mid-urethral slings due to mesh complications, therapies using vaginal energies have been widely used in clinical practice for the treatment of vaginal atrophy, UI and voiding urgency. However, data are still limited, and international organizations have highlighted the need for comparative studies with longer follow-up to assess their efficacy and to ensure patient safety [18,19,20,21,22,23]. This study was conducted with the intention of providing high-level evidence in this field.
Assessing groups classified by the severity of UI demonstrated that the energy-treated groups reached very high subjective improvement and objective cure rates, mainly in mild cases. Therefore, this could be the major indication for their use. Similarly, better results were achieved by premenopausal women and in cases of pure SUI, which could be attributed to the time of onset of symptoms or to the effect of hormonal status on the tissue remodeling response. Thus, there may be the ideal patient and time for energy use; however, more studies are needed to confirm this information.
The mean age of the study’s women was approximately 50 years, so most of them could be experiencing the effects of hypoestrogenism. This could be noted by the pretreatment frequency of urgency and nocturia, symptoms related to atrophy; however, a significant reduction of these symptoms was achieved by the energy-treated groups, confirming the previous findings that intravaginal energy treatments could help with GSM [7, 8, 12].
It is interesting to note that participants with moderate and severe UI were also included, and even in these cases, satisfactory results occurred, suggesting that these therapies could also be offered to patients with more severe cases that have surgical contraindications.
The improvement rates of the sham control group should also be commented on. This group received, as the others, behavioral therapy and was verbally oriented to perform perineal exercises, emphasizing the importance of these measures for UI treatment. Unfortunately, these procedures are not very often adopted because they demand time and discipline. It is interesting to note that the adherence to the proposed measures or the placebo effects persisted until 4 months after the first application, with a reduction in symptoms, but it did not last, reflecting the importance of having a control group and a longer follow-up. This is also other the strength of this study. Nonetheless, this study has several limitations. First, a greater than expected and not homogeneous study discontinuation was observed; however, it did not compromise the study power. It occurred mainly in the control group after the first treatment session, so intention-to-treat analysis considering these cases as treatment failure was also performed. Second, patients with predominant SUI, not only those with pure SUI, were included. However, this not only allowed the observation of the impact of these treatments on other aspects, such as urgency and urinary loss during sexual intercourse, but also represents the real effect that could be achieved in clinical practice. Moreover, the lasting treatment efficacy and, eventually, a treatment protocol for reapplication are still uncertain.
UI could contribute to sexual dysfunction [24, 25], and this was demonstrated by pretreatment FSF-I mean scores < 26.55 in all groups. A significant reduction in urinary loss during intercourse was found in the energy-treated groups, a symptom that affects women’s sexual life and is often underreported [26, 27]. Different from what was expected, neither a significant improvement in FSF-I score post-treatment was reported nor a significant increase in sexually active women.
No major or late complications were identified; only mild symptoms were reported immediately after treatment sessions, and they resolved spontaneously, consistent with previous reports [8,9,10,11,12, 17]. Notably, moderate pain was also reported by the sham control group, revealing that simple manipulation of the vagina with a speculum or a probe is uncomfortable.
Conclusions
CO2 laser and radiofrequency are outpatient options for SUI treatment, with no major complications. They had similar results and presented better results compared to the sham control group.
References
MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000;107:1460–70. https://doi.org/10.1111/j.1471-0528.2000.tb11669.x.
Devore EE, Minassian VA, Grodstein F. Factors associated with persistent urinary incontinence. Am J Obstet Gynecol. 2013;209:145.e1–6. https://doi.org/10.1016/j.ajog.2013.05.002.
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. IntUrogynecol J. 2010;21:5–26. https://doi.org/10.1007/s00192-009-0976-9.
Cavkaytar S, Kokanali MK, Topcu HO, Aksakal OS, Doðanay M. Effect of home-based Kegel exercises on quality of life in women with stress and mixed urinary incontinence. J Obst Gynaecol. 2015;35:407–10. https://doi.org/10.3109/01443615.2014.960831.
Schimpf MO, Rahn DD, Wheeler TL, et al. Sling surgery for stress urinary incontinence in women: a systematic review and meta-analysis. Am J Obstet Gynecol. 2014;211(71):e1–27. https://doi.org/10.1016/j.ajog.2014.01.030.
Chang J, Lee D. Midurethral slings in the mesh litigation era. Transl Androl Urol. 2017;6(Suppl 2):S68–75. https://doi.org/10.21037/tau.2017.04.06.
Salvatore S, Leone RMU, Athanasiou S, et al. Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause. 2015;22:845–9. https://doi.org/10.1097/GME.0000000000000401.
Cruz VL, Steiner ML, Pompei LM, et al. Randomized, double-blind, placebo-controlled clinical trial for evaluating the efficacy of fractional CO2 laser compared with topical estriol in the treatment of vaginal atrophy in postmenopausal women. Menopause. 2018;25:21–8. https://doi.org/10.1097/GME.0000000000000955.
Okui N. Comparison between erbium-doped yttrium aluminum garnet laser therapy and sling procedures in the treatment of stress and mixed urinary incontinence. World J Urol. 2019;37(5):885–9. https://doi.org/10.1007/s00345-018-2445-x.
Fistonić N, Fistonić I, Lukanovič A, et al. First assessment of short-term efficacy of Er:YAG laser treatment on stress urinary incontinence in women: prospective cohort study. Climacteric. 2015;18(1):37–42. https://doi.org/10.3109/13697137.2015.1071126.
Dillon B, Dmochowski R. Radiofrequency for the treatment of stress urinary incontinence in women. Current Urology Reports . 2009;10(5):369–374. https://doi.org/10.1007/s11934-009-0058-z.
Kamilos MK, Borrelli CL. New therapeutic option in genitourinary syndrome of menopause: pilot study using microablative fractional radiofrequency. Einstein J. 2017;15:445–51. https://doi.org/10.1590/s1679-45082017ao4051.
Juszczak E, Altman DG, Hopewell S, Schulz K. Reporting of multi-arm parallel-group randomized trials: extension of the CONSORT 2010 statement. JAMA. 2019;321(16):1610–20. https://doi.org/10.1001/jama.2019.3087.
Souza CCC, Rodrigues AM, Ferreira CE, et al. Portuguese validation of the urinary incontinence-specific quality-of-life instrument: I-QOL. Int Urogynecol J. 2009;20(10):1183–9. https://doi.org/10.1007/s00192-009-0916-8.
Tamanini JTN, Dambros M, D'Ancona CAL, Palma PCR, Netto NR Jr. Validation of the “international consultation on incontinence questionnaire - short form” (ICIQ-SF) for Portuguese. Rev Saude Publica. 2004;38(3):438–44. https://doi.org/10.1590/S0034-89102004000300015.
Thiel RDRC, Dambros M, Palma PCR, Thiel M, Riccetto CLZ, Ramos MDF. Translation into Portuguese, cross-national adaptation and validation of the female sexual function index. Rev Bras Ginecol e Obstet. 2008;30(10):504–10. https://doi.org/10.1590/S0100-72032008001000005.
Conté C, Jauffret T, Vieillefosse S, Hermieu JF, Deffieux X. Laser procedure for female urinary stress incontinence: a review of the literature. Prog Urol. 2017;27(17):1076–83. https://doi.org/10.1016/j.purol.2017.09.003.
FDA warns against use of energy-based devices to perform vaginal ‘rejuvenation’ or vaginal cosmetic procedures: FDA Safety Communication. https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm615013.htm. Accessed 30 July 2018.
Preti M, Vieira-Baptista P, Digesu GA, et al. The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: an ICS/ISSVD best practice consensus document. Neurourol Urodyn. 2019;38(3):1009–23. https://doi.org/10.1002/nau.23931.
Digesu GA, Tailor V, Preti M, et al. The energy based devices for vaginal "rejuvenation," urinary incontinence, vaginal cosmetic procedures, and other vulvo-vaginal disorders: an international multidisciplinary expert panel opinion. Neurourol Urodyn. 2019;38(3):1005–8. https://doi.org/10.1002/nau.23927.
Shobeiri SA, Kerkhof MH, Minassian VA, Bazi T. IUGA Research and Development Committee. IUGA committee opinion: laser-based vaginal devices for treatment of stress urinary incontinence, genitourinary syndrome of menopause, and vaginal laxity. Int Urogynecol J. 2019;30(3):371–6. https://doi.org/10.1007/s00192-018-3830-0.
Escribano JJ, González-Isaza P, Tserotas K, et al. In response to the FDA warning about the use of photomedicine in gynecology. Lasers Med Sci. 2019;34(7):1509–11. https://doi.org/10.1007/s10103-019-02744-1.
Salvatore S, Athanasious S, Yuen HTH, Karram M. LASER users' expert opinion in response to "the clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: an ICS/ISSVD best practice consensus document". Neurourol Urodyn. 2019;38(8):2383–4. https://doi.org/10.1002/nau.24140.
Pace G, Vicentini C. Female sexual function evaluation of the tension-free vaginal tape (TVT) and transobturator suburethral tape (TOT) incontinence surgery: results of a prospective study. J Sex Med. 2008;5(2):387–93. https://doi.org/10.1111/j.1743-6109.2007.00708.x.
Jha S, Radley S, Farkas A, Jones G. The impact of TVT on sexual function. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(2):165–9. https://doi.org/10.1007/s00192-008-0743-3.
El-Azab AS, Yousef HA, Seifeldein GS. Coital incontinence: relation to detrusor overactivity and stress incontinence. Neurourol Urodyn. 2011;30(4):520–4. https://doi.org/10.1002/nau.21041.
Gray T, Li W, Campbell P, Jha S, Radley S. Evaluation of coital incontinence by electronic questionnaire: prevalence, associations and outcomes in women attending a urogynaecology clinic. Int Urogynecol J. 2018;29(7):969–78. https://doi.org/10.1007/s00192-017-3380-x.
Acknowledgments
This study received funding from CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior, a Brazilian Federal Agency, linked to the Ministry of Education) and Process 2019/15802-1, FAPESP (Fundação de Amparo à Pesquisa do Estado de São Paulo, a public institution to promote academic research linked to the São Paulo State Government). Thanks to the Sector of Urogynecology and Vaginal Surgery, Federal University of São Paulo.
Author information
Authors and Affiliations
Contributions
AS Seki: Project development, Data collection, Data analysis, Manuscript writing.
AMHMB Ferraro: Project Development, Data analysis, Manuscript writing/editing.
ESM Fonseca: Data collection.
MGF Sartori: Project development, Manuscript editing.
MJBC Girão: Project development, Data analysis.
ZIKJD Bella: Project development, Data analysis, Manuscript writing/editing.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Manoel J. B. C. Girão (in memoriam)
The preliminary results of this study were presented previously at the 58th Brazilian Congress of Gynecology and Obstetrics in Porto Alegre, Brazil (November 2019), and the paper received an awarded as an original study. It was also selected as an oral presentation at the 45th IUGA Annual Meeting (virtual), August/September 2020. In 2021, this study was presented and received first prize at the 26th Paulista Congress of Gynecology and Obstetrics in São Paulo (SOGESP).
Rights and permissions
About this article
Cite this article
Seki, A.S., Bianchi-Ferraro, A.M.H.M., Fonseca, E.S.M. et al. CO2 Laser and radiofrequency compared to a sham control group in treatment of stress urinary incontinence (LARF study arm 3). A randomized controlled trial. Int Urogynecol J 33, 3535–3542 (2022). https://doi.org/10.1007/s00192-022-05091-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05091-y