Abstract
Introduction and hypothesis
Urinary incontinence (UI) is common and the relationship among its subtypes complex. Our objective was to describe the natural history and predictors of the incontinence subtypes stress, urgency, and mixed, in middle-aged and older US women. We tested our hypothesis that UI subtype history predicted future occurrence, evaluating subtype incidence/remission over multiple time points in a stable cohort of women.
Methods
We analyzed longitudinal urinary incontinence data in 10,572 community-dwelling women aged ≥50 in the 2004–2010 Health and Retirement Study. Mixed, stress, and urgency incontinence prevalence (2004, 2006, 2008, 2010) and 2-year cumulative incidence and remissions (2004–2006, 2006–2008, 2008–2010) were estimated. Patient characteristics and incontinence subtype status 2004–2008 were entered into a multivariable, transition model to determine predictors for incontinence subtype occurrence in 2010.
Results
The prevalence of each subtype in this population (median age 63–66) was 2.6–8.9 %. Subtype incidence equaled 2.1–3.5 % and remissions for each varied between 22.3 and 48.7 %. Incontinence subtype incidence predictors included ethnicity/race, age, body mass index, and functional limitations. Compared with white women, black women had decreased odds of incident stress incontinence and Hispanic women had increased odds of stress incontinence remission. The age range 80–90 and severe obesity predicted incident mixed incontinence. Functional limitations predicted mixed and urgency incontinence. The strongest predictor of incontinence subtype was subtype history. The presence of the respective incontinence subtypes in 2004 and 2006 strongly predicted 2010 recurrence (odds ratio [OR] stress incontinence = 30.7, urgency OR = 47.4, mixed OR = 42.1).
Conclusions
Although the number of remissions was high, a previous history of incontinence subtypes predicted recurrence. Incontinence status is dynamic, but tends to recur over the longer term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than 20 million US women suffer from urinary incontinence (UI), a costly condition that increases with age [1–4]. The numbers of longitudinal studies describing overall UI incidence, remission, and predictors in women have increased over the last decade, but have largely focused on UI in general and not on incontinence subtypes, which include stress, urgency, and mixed UI. Complete descriptions of UI subtypes and predictors in older, non-institutionalized women are few in number [5–8]. Unprecedented growth of the population aged over 65 highlights the need to examine the natural history of incontinence in these older women [9]. We sought to specifically address this gap in the literature and evaluated the natural history of UI subtypes, including stress urinary incontinence (SUI), urgency urinary incontinence (UUI), and mixed urinary incontinence (MUI) in middle-aged and older community-dwelling women.
The optimal depiction of the natural history of UI requires not only recognition of its subtypes, but also better characterization of the remission and recurrence of these subtypes over time. Resolution of UI and its subtypes may be high in this population [6, 10, 11], but investigators have questioned whether the resolution is temporary or permanent [1]. Some have suggested that in the long term, UI and/or its subtypes tend to recur [10, 12]. To resolve these questions and provide detailed information on specific UI subtypes we chose to use transition models to evaluate UI subtypes over sequential increments of time.
Previously, we used a robust data-set, the Health and Retirement Study (HRS), to describe the occurrence and resolution of overall UI over a single 4-year period [13, 14]. For the current publication, we utilized the same database, but conducted in depth mathematical modeling (using Markov transition models) to assess the likelihood of remission and recurrence of UI subtypes over three consecutive, 2-year periods [15]. The objectives of this work were to describe the prevalence, incidence, remission, and predictors of UI subtypes in middle-aged and older women, and to assess the impact of UI subtype history on the likelihood of recurrence and remission. We hypothesized that the natural history of UI subtypes varied in older women and that past UI subtype history could be used to predict future continence status.
Materials and methods
Data source/study dates
Subjects were community-dwelling women in the HRS 2004–2010. The HRS has examined older Americans’ health with in-person, biennial interviews since 1992 and posts results on a publically available database [13]. HRS participants are chosen using multi-stage probability sampling [16]. Additional cohorts have been added every 6 years (1998, 2004, 2010) to maintain a steady state sample of participants. The HRS oversamples black and Hispanic subjects, allowing sub-group analysis of minorities and provides sampling weights based on US Census data to adjust for oversampling [16]. Zero weights are assigned to subjects institutionalized at survey follow-up to reflect community-dwelling estimates.
Our population consisted of women aged ≥50 with incontinence status information in the HRS database. We ascertained UI subtype prevalence in these women in 2004, 2006, 2008, and 2010. Subjects for 2-year incidence/remission analyses (2004–2006, 2006–2008, 2008–2010) had baseline and follow-up incontinence information. UI subtype prevalence, incidence and remission were reported using weight-adjusted proportions. We also included overall UI estimates to provide a context in which to interpret UI subtype estimates. This study was granted exempt review board status (HRRC #07-284) as all information in the HRS public database was de-identified.
Population characteristics
We previously identified UI risk factors in an earlier HRS population; these included age, ethnicity/race, BMI, history of psychiatric illness (including depression), functional limitations, and medical co-morbidities [14]. In the current study, age was stratified by decade (6–10th). Ethnicity/race was categorized as white, black, Hispanic, and other. BMI groups are noted in Table 1. We assessed functional limitations as a continuous variable (percentage of total) based on nine questions in the HRS, also described previously [14]. Medical comorbidities (hypertension, diabetes, cancer, lung disease, heart disease, arthritis, stroke) were categorized as ordinal variables (0, 1, 2, ≥3) based on subject history [14].
Definitions
Incontinence definitions were based on questions noted in Fig. 1. Frequency of urine loss greater than 1 day in the last month affirmed UI. We defined UUI as affirmation of the urgency question, SUI as affirmation of the stress question, MUI as affirmation of both, and uncategorized UI as affirmation of neither. Figure 1 also includes prevalence, incidence, and remission definitions. Remission was defined as UI at baseline, which resolved at the next follow-up interval and transitions from one UI subtype to another were not considered remissions.
Computations/statistical analysis
We estimated prevalence and 2-year incidence/remission of UI/UI subtypes. Because subjects’ ages spanned five decades, we also estimated proportions as age-stratified data. Multinomial logistic regression compared UI subtypes and associations with decade. Binary logistic regression analyzed associations between UI and decade (SAS/STAT®9.3). Results were reported as OR with 95 % CI.
We evaluated incontinence predictors and focused on information before 2010 that best predicted incontinence in 2010. This longitudinal analysis evaluated whether previous incontinence status and patient characteristics independently predicted 2010 incontinence. We developed a binary (present or absent UI) model for overall UI and a multinomial model for UI subtypes; MUI, SUI, UUI, and uncategorized. Transition models (called Markov models) were fitted using multivariate logistic regression. These models, as described by Diggle et al., assumed that subjects are in one of a limited number of discrete states (e.g., no UI, UUI, SUI, MUI, uncategorized), and the probabilities of transition between states were estimated [15]. These models have an associated “order,” which is the number of past time intervals employed to predict the future and the number of significant interactions between predictors and past states. These transition chains are characterized by a transition matrix, which records probabilities of these transitions from one state to the next. Transition events (presence/absence of UI/UI subtypes) were used to generate odds of incontinence occurrence and resolution and to indicate the effect that past states have in predicting future states.
Using logistic regression we modeled subjects’ 2010 incontinence status controlling for the following independent variables in 2004, 2006, and 2008: incontinence status, age, ethnicity/race, medical co-morbidities, functional limitations, BMI, psychiatric history, and associated interactions. The dependent variable was the categories’ multinomial outcome of no UI, UUI, SUI, MUI, and uncategorized UI. Computation was performed using ProcSurveylogistic with sampling weights from 2010 and generalized logit link in SAS®9.3. This was a large set of predictor variables and most terms were nonsignificant. We dropped nonsignificant terms (p ≥ 0.05) to arrive at a parsimonious model with the lowest possible order.
Results
Population characteristics are noted in Table 1. For prevalence data the number of women evaluated ranged from 10,572 women in 2004 to 7,908 women in 2010. Incidence data were available for 9,545–7,842 women during these same years. For each 2-year time increment for incidence calculations, there was missing follow-up information on approximately 9–12 % of participants. Most of this loss to follow-up was due to death or institutionalization in the older groups of women, and occurred largely in the group of woman 80 years and older. Less than 2 % of the loss to follow-up was for other reasons. Participants for both prevalence and incidence calculations, the majority of whom were white, had median ages between 63 and 66 years, were overweight, and had a median of 1–2 functional limitations and medical co-morbidities (Table 1).
Prevalence of overall UI (defined as the presence of any UI subtype) ranged between 19 and 26 % and increased with age during all study periods. Using the 6th decade as a reference, the prevalence of UI increased in all subsequent decades (all P < 0.0001). For example, UI occurred in 14.5–18 % of women in the 6th decade and in 39–42 % of women in the 10th decade of life. UUI, MUI, and SUI prevalence differed with respect to aging. UUI increased with age for all years (P < 0.0001), and this was most apparent in the 2004 data. The odds of occurrence of UUI in the 7th decade were 2.18 (CI = 1.5–3.15) compared with the 6th decade, and by the 10th the odds of UUI increased nine-fold (OR = 9.19, CI = 5.56–15.20). MUI prevalence, consistently increased in the 8th to 10th decades (all P ≤ 0.005). MUI in the 7th decade did not increase relative to the 6th at all time intervals and was found to be increased only in 2004 (P =0 .003) and 2006 (P < 0.001). SUI did not increase with the decade in any time interval (all P = 0.28–0.99).
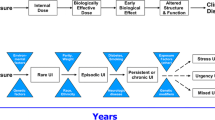
Two-year incidence/remissions are noted in Tables 2 and 3. UI subtype transitions (e.g., resolution, persistence or change to other UI subtypes) are noted in Fig. 2. Overall, UI incidence ranged between 11.8 and 13.3 %, while the incidence of each UI subtype was approximately 3 % (Table 2). UI remission was 30.0–34.6 % and remissions of UI subtypes ranged from 22 to 48 % (Table 3). MUI had the lowest probability of remission. Compared with MUI, the odds of SUI remission ranged from 1.5 (CI = 1.2–2.0) in 2004–2006 to 1.8 (CI = 1.4–2.3) in 2006–2008, and relative to MUI, remission of UUI ranged from 1.5 (CI = 1.1–1.9) in 2004–2006 to 1.7 (CI = 1.3–2.2) in 2006–2008.
Urinary incontinence status: transitions from baseline to 2-year follow-up. Transitions from incontinence status at baseline to 2-year follow-up (2004–2006, 2006–2008, 2008–2010). UI status at baseline: no UI, UUI (UUI only without other subtypes), SUI (SUI only without other subtypes) or MUI (both UUI and SUI present). UI status at 2-year follow-up: percentages of patients in each subtype at follow-up are expressed as the range in percentages for each of the 2-year follow-up periods
Characteristics in the multivariate model that predicted UI subtype incidence/remission included functional limitations, race/ethnicity, age and BMI, although their impact varied among subtypes. Increasing functional limitations predicted MUI and UUI in a linear fashion, whereas two limitations predicted incident UUI and MUI (UUI OR = 1.1 [CI = 1.03–1.15], MUI OR = 1.7 [CI = 1.5–2.0]), 9 limitations predicted UUI and MUI odds more markedly (UUI OR = 3.0 [CI = 1.5–6.2], MUI OR = 11.8 [CI = 6.0–23.2]). Race/ethnicity, rather than functional limitations, were more important predictors of SUI; black women had decreased odds of incident SUI (OR = 0.5, CI = 0.3–0.9) and Hispanic women had increased odds of SUI remission (OR = 7.7, CI = 1.1–53.4). Age and BMI were the only predictors for MUI; only the 9th decade predicted incident MUI (OR = 2.8, CI = 1.5–5.3), and only BMI ≥ 35 predicted increased MUI incidence (OR = 1.6, CI = 1.1–2.4) and decreased remission (OR = 0.6, CI = 0.4–0.9). Importantly, the strongest predictor of UI and UI subtype incidence and remission was previous UI and UI subtype history. The presence of a specific subtype in 2004 and 2006, increased odds of the recurrence of that subtype in 2010 thirty to forty-fold (Fig. 3).
History predicts the occurrence of urinary incontinence subtypes. The x-axis represents the odds ratio for the incidence of UI subtype in 2010. The y-axis represents UI subtypes (SUI, UUI, and MUI) and history of the UI subtype. “Distant” history = UI subtype present in only 2004, “recent” history = UI subtype present in only 2006, “repetitive” history = UI subtype present in both 2004 and 2006
Discussion
This study makes a significant contribution to the small body of literature regarding UI subtype epidemiology in older women. This large cohort from the HRS database allowed for robust evaluation of UI subtype predictors. The longitudinal analysis uniquely included incontinence status as a variable in the regression analysis, which both solidified and quantified the importance of incontinence history in UI subtypes.
Our study showed that the 2-year incidence for each UI subtype was approximately 3 % and remission was 22–48 %. We found that the 2-year incidence for overall UI, when calculated annually, was 5.9–6.7 %. This is comparable to the 7 % incidence reported in older women by an international review [10] and validates our definitions and methodology.
Longitudinal studies of UI subtypes in older women are scarce and even fewer have identified subtype predictors [5–8]. We were able to evaluate subject characteristics such as age, ethnicity/race, functional limitations/physical disability, and BMI to asses which of these independently predicted UI subtypes. The findings differed among subtypes. UUI and MUI increased with age, whereas SUI did not. Ethnicity/race was a predictor of SUI, but not UUI or MUI. Previous work has found that among young/middle-aged women black race has been reported to be a negative predictor of SUI [10, 17]. Our work showed similar findings in older women. However, unlike reports in younger women [10, 17], black race did not predict UUI in our study cohort. The higher overall prevalence of UUI in older women may overshadow differences in incidence attributable to race.
We also report on important findings on the relationship of UI subtypes and functional limitations. The number of functional limitations reported by participants was a strong predictor for the development of MUI and UUI. Women with a maximum number of limitations had 11-fold increased odds of developing MUI. Additionally, there is currently limited information on the importance of BMI in the prediction of UI subtype and most reports have not focused on older populations. Waetjen et al. reported that in middle-aged women, a BMI increase of 5 kg/m2 was associated with a 30 % increase in SUI and a 15 % increase in UUI [17]. Others have also reported the association between weight and UI subtypes in younger/middle-aged women; one study noted that a BMI of ≥35 kg/m2 was associated with a three-fold increased incidence of SUI, a five-fold increase in MUI, and a six-fold increase in UUI [18]. In our study of older women, BMI was found to predict only an increased risk of MUI. Women with BMI ≥35 had greater odds of developing MUI, and this remained significant after accounting for other covariates.
The most important finding of this current work was that it ascertained that previous UI subtype history had the greatest effect in predicting future UI subtypes. Jackson evaluated previous overall UI history as being an incontinence predictor using methods similar to ours [19]. That study employed transitional logistic regression analysis to evaluate overall UI over 2 years in 1,017 post-menopausal women and found that previous overall UI was the strongest incontinence predictor. Previous UI increased the odds of overall UI at follow-up by 24.7 (CI = 19.5–33.2). Our study specifically evaluated UI subtypes and did so in sequential, 2-year intervals over a longer period of time. Utilizing all UI subtypes in a multinomial model, we found that a repeated UI subtype history had a much stronger effect than overall UI, increasing UI subtype incidence 30–40 fold.
Our study quantified the degree to which incontinence history increased the probability of recurrence. We found that UI subtype status information from all three preceding time intervals (2004, 2006, 2008) improved the prediction of UI subtypes in 2010 and underscored the importance of previous incontinence status as a predictor (Fig. 3). In particular, if the history of UI subtype was found in both 2004 and 2006 this history was most predictive of 2010 recurrence. For example, when a specific subtype was present in 2004 and 2006, recurrence odds for that subtype in 2010 increased 30–40 fold. Subtype presence in the immediately preceding time interval was a stronger predictor than more distant intervals; 2006 UI subtype status was more powerful than 2004 status in predicting 2010 subtypes.
Limitations of this study include the lack of validated questionnaires and treatment data. However, it should be noted that questions similar to those used in the HRS have characterized incontinence in other studies with comparable findings [7, 17, 20]. The likelihood that treatment confounds our results is also small. Less than 20 % of women with mild to moderate UI seek care [10]. In the setting of SUI, surgery is chosen by only 2 % of patients [21, 22]. Additionally, in our opinion, treatment of UUI is unlikely to affect long-term continence; a recent meta-analysis noted that medication achieves continence in less than 20 % of patients and is often discontinued [23].
In conclusion, this study presents a unique, longitudinal evaluation of UI subtype epidemiology in a large, community-dwelling population of older women. The innovative models that were used demonstrate that previous incontinence subtype status profoundly affects future incontinence. Although shorter observation periods suggest that incontinence status might be dynamic with high remission [6, 11, 14], over longer observation periods, incontinence has a propensity to recur. As populations age, UI will increase and a better understanding of the incidence and remission of UI subtypes will affect treatment and healthcare resource planning.
References
Landefeld CS, Bowers BJ, Feld AD et al (2008) National institutes of health state-o-the-science conference statement: prevention of fecal and urinary incontinence in adults. Ann Intern Med 148(6):449–458
Kannan H, Radican L, Turpin RS et al (2009) Burden of illness associated with lower urinary tract symptoms including overactive bladder/urinary incontinence. Urology 74:34–38
Hu TW, Wagner TH, Bentkover JD et al (2004) Costs of urinary incontinence and overactive bladder in the United States: a comparative study. Urology 63:461–465
Nygaard I, Barber MD, Burgio KL et al (2008) Prevalence of symptomatic pelvic floor disorders in US women. JAMA 300(11):1311–1316
Thom DH, Brown JS, Schembri M et al (2010) Incidence and risk factors for change in urinary incontinence status in a prospective cohort of middle-aged and older women: the reproductive risk of incontinence study in Kaiser. J Urol 184:1394–1401
Nygaard IE, Lemke JH (1996) Urinary incontinence in rural older women: prevalence, incidence and remission. J Am Geriatr Soc 44(9):1049–1054
Lifford KL, Townsend MK, Curhan GC et al (2008) The epidemiology of urinary incontinence in older women: incidence, progression, and remission. J Am Geriatr Soc 56(7):1191–1198
Irwin DE, Milsom I, Chancellor MB et al (2010) Dynamic progression of overactive bladder and urinary incontinence symptoms: a systematic review. Eur Urol 58:532–543
The older population (2010) Issued November 2011. Available at: http://www.census.gov/prod/cen2010/briefs/c2010br-09.pdf. Retrieved 6 November 2014
Milsom I, Altman D, Lapitan M et al (2009) Epidemiology of urinary incontinence (UI) and faecal incontinence (FI) and pelvic organ prolapse (POP). In: Abrams P, Cardozo L, Khoury S et al (eds) Incontinence, 4th edn. Health Publications, Plymouth
Herzog AR, Diokno AC, Brown MB et al (1990) Two-year incidence, remission, and change patterns of urinary incontinence in noninstitutionalized older adults. J Gerontol 45(2):M67–M74
Hartmann KE, McPheeter ML, Biller DH et al (2009) Treatment of overactive bladder in women. Evid Rep Technol Assess 187:1–120
Health and Retirement Study, Data products (CORE files 2004, 2006, 2008, 2010 and Cross Wave: Tracker 2010 file0 public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, MI, (2004–2010). Available at: http://hrsonline.isr.umich.edu. Accessed 2 May 2014
Komesu YM, Rogers RG, Schrader RM et al (2009) Incidence and remission of urinary incontinence in a community-based population of women ≥50 years. Int Urogynecol J Pelvic Floor Dysfunct 20(5):581–589
Diggle PJ, Heagerty P, Liang K-Y et al (2009) Transition models. In: Analysis of longitudinal data, 2nd edn. Oxford University Press, New York, pp 190–207
Sampling weights revised for Tracker 2.0 and beyond. Available at: http://hrsonline.isr.umich.edu/sitedocs/wghtdoc.pdf and updates to HRS sample weights. Available at: http://hrsonline.isr.umich.edu/sitedocs/userg/dr-013.pdf
Waetjen LE, Liao S, Johnson WO et al (2006) Factors associated with prevalent and incident urinary incontinence in a cohort of midlife women: a longitudinal analysis of data. Study of women’s health across the nation. Am J Epidemiol 165(3):309–318
Jackson SL, Scholes D, Boyko EJ et al (2006) Predictors of urinary incontinence in a prospective cohort of postmenopausal women. Obstet Gynecol 108:855–862
Townsend MK, Danforth KN, Rosner B et al (2007) Body mass index, weight gain, and incident urinary incontinence in middle-aged women. Obstet Gynecol 110:346–353
Minassian VA, Devore E, Hagan K et al (2013) Severity of urinary incontinence and effect on quality of life in women by incontinence type. Obstet Gynecol 121:1083–1090
Hunskaar S, Lose G, Sykes D et al (2004) The prevalence of urinary incontinence in women in four European countries. Br J Urol Int 93:324–330
Reynolds WS, Dmochowski RR, Penson DF (2011) Epidemiology of stress urinary incontinence in women. Curr Urol Rep 12:370
Shamliyan T, Wyman J, Kane RL. Nonsurgical treatments for urinary incontinence in adult women: diagnosis and comparative effectiveness. Comparative Effectiveness Review No. 36. (Prepared by the University of Minnesota evidence-based practice Center under Contract No. HHSA 290-2007-10064-I.) AHRQ Publication No. 11(12)-EHC074-EF. Rockville, MD. Agency for Healthcare Research and Quality. April 2012. Available at: www.effectivehealthcare.ahrq.gov/reports/final.cfm
Funding
The Health and Retirement Study, data products (CORE files 2004, 2006, 2008, 2010 and Cross Wave: Tracker 2010 file public use dataset). Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). Ann Arbor, Michigan, USA. The current research was also supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health through grant number 8UL1TR000041, The University of New Mexico Clinical and Translational Science Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Y.M. Komesu: Co-PI for “Brain Centered Therapy versus Medication for Urgency Urinary Incontinence—An RCT,” grant number 5R-01AT007171-03, NIH PA-10-067, funding source: NIH (primary: NCCIH); R. Schrader: Co-Investigator grant number 5R-01AT007171-03 (see above); L.H. Ketai: Co-PI grant number 5R-01AT007171-03 (see above); R.R. Rogers: Co-Investigator grant number 5R-01AT007171-03 (see above), Up-to-Date and McGraw-Hill royalties, Associate Editor IUJ, Editorial Board Female Pelvic Medicine and Reconstructive Surgery and Obstetrics & Gynecology, DSMB Chair Transform Trial, ABOG Subspecialty Board Member; G.C. Dunivan: Liberate Site PI, American Urogynecologic Society Education Committee.
Rights and permissions
About this article
Cite this article
Komesu, Y.M., Schrader, R.M., Ketai, L.H. et al. Epidemiology of mixed, stress, and urgency urinary incontinence in middle-aged/older women: the importance of incontinence history. Int Urogynecol J 27, 763–772 (2016). https://doi.org/10.1007/s00192-015-2888-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2888-1