Abstract
Introduction and hypothesis
Mixed urinary incontinence (UI) is, on average, more severe than urgency UI or stress UI. We tested the hypothesis that mixed UI is a more advanced stage of UI by comparing transition probabilities among women with stress, urgency, and mixed UI.
Methods
We used data from the General Longitudinal Overactive Bladder Evaluation Study-UI, which included community-dwelling women, aged 40+ years, with UI at baseline. Study participants completed two or more consecutive bladder health surveys every 6 months for up to 4 years. Using sequential 6-month surveys, transition probabilities among UI subtypes were estimated using the Cox-proportional hazards model, with the expectation that probabilities from stress or urgency UI to mixed UI would be substantially greater than probabilities in the reverse direction.
Results
Among 6,993 women 40+ years of age at baseline, the number (prevalence) of women with stress, urgency, and mixed UI was 481 (6.9%), 557 (8.0%), and 1488 (21.3%) respectively. Over a 4-year period, the transition probabilities from stress UI (34%) and urgency UI (27%) to mixed UI was significantly higher than probabilities from mixed to stress UI (6%) or to urgency UI (rate = 9%). The adjusted transition hazard ratio for stress UI and urgency UI was 2.06 (95% CI: 1.73-2.92) and 1.85 (95% CI: 1.63-2.57) respectively compared with mixed UI.
Conclusion
The substantially higher transition from stress UI and urgency UI to mixed UI supports the hypothesis that mixed UI might represent a more advanced stage of UI that may have implications for understanding disease progression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
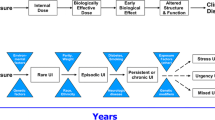
Urinary incontinence (UI) consists of three main subtypes. Stress and urgency UI occur either separately, or co-occur in the form of mixed UI, where the observed prevalence of mixed UI is significantly higher than expected if stress and urgency UI are assumed to be independent [1]. One explanation for this higher than expected prevalence is that mixed UI represents a more advanced stage of UI. This idea is consistent with mixed UI being more severe (e.g., Sandvik score, bothersome symptoms, and quality of life) [2,3,4]. Moreover, although UI has substantial variability in symptom expression [5] with high incidence and remission rates [6,7,8,9,10], when stress and urgency UI co-occur, they are less likely to remit and more likely to persist than when they occur in isolation [11]. If mixed UI represents a more severe stage of UI, we hypothesized that the transition probability of stress UI or urgency UI to mixed UI would be substantially greater than the reverse probabilities.
Most longitudinal studies on the natural history of UI define progression as moving from a mild to a more severe level of disease. However, relatively little is known about the population level transition probabilities from one UI subtype to another [11]. The definition of UI subtypes is based on cross-sectional interpretation of current UI symptoms, commonly within the past 1—6 months. However, women with mixed UI may not report co-occurring stress and urgency UI symptoms every time they experience urine loss. Therefore, in longitudinal studies, it is possible to identify women who in fact transition from one subtype to another. These transitions from pure to mixed UI subtypes or vice versa are not well understood and to our knowledge have not been previously studied. The objective of our study was to better understand transition rates of UI subtypes every 6 months and over a period of 4 years. We hypothesize that compared with stress and urgency UI, mixed UI is less likely to transition to a pure UI stage such as stress or urgency UI. To test this hypothesis, we determined transition rates among UI subtypes using longitudinal data from the General Longitudinal Overactive Bladder Evaluation Study of Urinary Incontinence (GLOBE-UI). We also examined whether these hypothesized stages of progression might be associated with indicators of early versus more advanced stages.
Materials and methods
The GLOBE-UI is a longitudinal study of the natural history of UI in women 40 years of age and older that started in 2009. The study is described in detail elsewhere [5, 12, 13]. Here, we summarize the source population, the study cohort, the Bladder Health Survey (BHS) and its validation, and other study details. The Geisinger Health System (GHS) institutional review board approved the study.
Source population and GLOBE-UI cohort
At the time the study was conducted, the Geisinger Clinic had 41 practice sites in central and northeastern Pennsylvania. We randomly sampled primary care patients and recruited 10,832 from 162,000 eligible women by mail. Eligibility criteria included female patients, ≥40 years of age, assigned to a primary care physician, and who had had at least one visit in the past 4 years.
Development of the Bladder Health Survey
The Bladder Health Survey (BHS) is a validated questionnaire that includes lifetime and 6-month questions on the occurrence of urgency, frequency, nocturia, UI, stress UI, urgency UI, and UI adaptive behavior [13]. There were two general UI questions followed by two questions for each of the two UI subtypes, in addition to questions about medical or surgical treatment for UI. Electronic health record (EHR) data were also obtained on UI medication and surgical treatment history. For this study, we used the 6-month symptom recall data from serial questionnaires to estimate transition probabilities among UI subtypes.
Most of the BHS questions were from the NOBLE Study self-administered questionnaire, which itself was clinically validated in a general population sample [14]. The test–retest reliability of BHS question responses (i.e., Spearman’s correlation coefficient) for UI-related items and the content, construct, and the clinical diagnostic validity was evaluated in a population sample. Sensitivity, specificity, and positive predictive values (PPVs) of the BHS ranged from 78 to 87%, 91 to 92%, and 96 to 97% respectively [13]. Furthermore, the BHS has been externally validated by the Sandvik score [15, 16].
Definitions of UI used in the BHS
A woman was defined as having UI if she:
-
1.
Lost more than a few drops or a small amount of urine at least once a month
-
2.
Reported having UI symptoms for 3 months or more in the past 6 months or, if not, having UI symptoms that were moderate to severe
-
3.
Reported past UI symptoms that were not due to urinary tract infections or to pregnancy
Active stress UI for a specific survey was defined as self-reported UI episodes in the past 6 months some of the time or more often (1+) with:
-
1.
Coughing hard, laughing or sneezing, or
-
2.
Lifting, pushing, or pulling a heavy object and she had no urgency UI symptoms, and
-
3.
No urgency UI symptoms
Active urgency UI was defined as having UI episodes in the past 6 months some of the time or more often (1+) associated with:
-
1.
Trouble getting to the bathroom on time
-
2.
A sudden urgency to urinate, and
-
3.
No stress UI symptoms
The possible answers and scores (range 0–8) to each of the above stress UI and the urgency UI questions were: never or rarely (0), some of the time (1), about half of the time (2), most of the time (3), and always (4). Active mixed UI was defined as having both stress and urgency UI symptoms some of the time or more over the past 6 months.
Statistical analysis
Analysis was limited to women who had UI symptoms at baseline and who completed at least one or more follow-up surveys within 6–12 months from baseline. Women were excluded from the analysis if they did not complete the baseline survey, or had no UI at baseline, or completed the baseline but failed to complete the 6- or 12-month follow-up survey.
A woman was defined as having transitioned to another UI subtype if she met criteria for one UI subtype in one 6-month period, and then met criteria for another UI subtype in the subsequent 6-month period. Women could also remit if they met criteria for active UI in one 6-month interval and reported no UI symptoms in a subsequent 6-month period. A woman was censored when she transitioned to another UI subtype or had a 6-month period without UI symptoms. All subsequent analyses were based on these 6-month criteria. In addition, we estimated transition probability using 12-month and 18-month criteria; that is, once a woman transitioned to another subtype, what is the probability of persisting in the latter subtype for 12 months or more (or 18 months or more).
We assessed selection bias by comparing EHR data on all nonrespondents with that of respondents excluded as previously noted and with that of respondents who were included in the analysis. Covariates analyzed included age, BMI, parity, disease comorbidities, smoking status, alcohol use, marital status, education, and hysterectomy. As some women may receive interval treatment for their UI, we also controlled for medical and surgical UI treatment. Cox-proportional hazards model was used to compare transition by UI subtype at baseline. Unadjusted hazard ratios (HR) for the transition rates between subtypes were estimated, followed by adjusted HR, first controlling for other covariates and a second model that controlled for other covariates and selection bias. Inverse probability weighting method [17, 18] was used to adjust for nonresponse bias, and adjusted HR was reported, and 95% confidence interval was calculated using bootstrap with 500 iterations [19]. We used the same inverse weight to adjust for transition probability (see Table 2). Additionally, we compared women with baseline urgency, stress or mixed UI who transitioned to another UI subtype versus those who did not by age, time since onset of UI, and Sandvik severity score; the hypothesis here was that women who transition to mixed UI would be older, have UI of longer duration or, on average, have more severe UI. For all comparisons, we used the t test for continuous variables and the Chi-squared test for categorical variables. Statistical significance was defined when the confidence interval did not include 1.0 and the p value was less than 0.05.
Analysis was performed using a SAS (version 9.3) statistical package (SAS institute, Cary, NC, USA).
Results
A total of 6,993 (65%) women responded to the baseline survey. Of those, 3,692 women were excluded because they reported no UI at baseline, and another 775 were excluded because they had incomplete follow-up data. Analysis of the follow-up experience was confined to 2,526 (36%) women who had UI at baseline, including 557 (22%) with stress UI, 481 (19%) with urgency UI, and 1,488 (59%) with mixed UI (Fig. 1). The mean age of respondents was 62.6 (±12.5). More than 75% had a BMI >25 kg/m2, and over 88% were parous. Compared with nonresponders, responders were older (49% vs 43% were 60+, p < 0.001), less likely to smoke cigarettes (58% vs 52%, p = 0.001), and more likely to be married (66% vs 60%, p = 0.05). Excluding age, most differences between responders and nonresponders were modest (Table 1). The 2,526 women with UI who were included in the final analysis, versus those who were excluded, were significantly older (52% vs 41% were 60+, p < 0.001), more likely to be ever-smokers (40% vs 36%, p = 0.005), more likely to report UI symptoms in the past 6 months (65% vs 51%, p < 0.001) at baseline. Surgical (less than 6%) and medical (less than 7%) treatment for UI were rare in both groups.
Among women who were included in the analysis, in addition to baseline survey, 15% completed one follow-up questionnaire, 81.1% completed 3 or more follow-up questionnaires, and 41.7% completed all eight follow-up questionnaires. The mean Sandvik severity score for women with baseline urgency UI (3.3–4.6) was significantly higher than those for stress UI (2.7–3.4; p < 0.001), and baseline Sandvik severity score for mixed UI (3.7–5.0) was significantly higher than those for UUI or SUI (both p -value <0.01).
The transition probabilities from stress UI (33.6%) or urgency UI (27.4%) to mixed UI were significantly and substantially greater than the transition probabilities from mixed UI to either stress UI (5.6%) or to urgency UI (8.6%). The probability of transition from stress UI to urgency UI (1.5%) or vice versa (1.0%) was very low (Table 2). Sensitivity analysis of transition probabilities using different criteria (i.e., requiring that the transition to the new state last for 6+, 12+ or 18+ months) showed that although the trends in transition probabilities did not differ in the 12+ or 18+ months versus the 6+-month criteria, the probabilities for the former groups were considerably lower (Table 2).
Using mixed UI as the reference, the transition hazard ratios (HRs) using the 6+ month criteria were highest for stress UI (HR = 2.34) followed by urgency UI (HR = 2.04). Adjusting for confounders had little to no impact on HR values; adjusting for selection bias reduced the HR values, but they remained statistically significant. The stress UI HR for transition was not significantly different from the HR for urgency UI (Table 3).
Women who transitioned from mixed to stress UI (mean age = 57) were younger than those who transitioned from mixed to urgency UI (mean age = 65) or who did not transition (mean age = 63), p < 0.01. Transition by time since the onset of UI differed only in the urgency UI group, where women with UI symptoms for more than 2 years were more likely to transition (57% versus 41%), p = 0.02. Women with stress UI who did not transition to mixed UI were more likely to have a slight Sandvik score (60.5%) versus those who transitioned (48%), p = 0.05; finally, women with mixed UI who transitioned to either stress or urgency UI were more likely to have a slight Sandvik score (38–41%) versus those who did not transition (28.5%), p = 0.02 (Table 4).
Discussion
The results of this study are consistent with the hypothesis that mixed UI might represent a more advanced stage of UI than either stress UI or urgency UI. The probabilities of transition from stress UI and urgency UI to mixed UI are substantially greater than transition probabilities in reverse, where women with mixed UI are the least likely to transition to another UI subtype over a period of 4 years. More than 85% of women with mixed UI did not transition to another subtype of UI. Moreover, transition in and out of stress UI occurs at a younger age (50s) when compared with urgency and mixed UI (60s), and women with stress UI have a lower mean Sandvik score when compared with women with mixed UI. Additionally, the mean Sandvik score differs in women defined by whether or not they transitioned from one UI subtype to another. In particular, the mean Sandvik score is lower for women with mixed UI who transition to another UI subtype. In contrast, women with stress UI who transition to mixed UI have a higher Sandvik score than women who do not. Finally, less severity is consistent with transition back to stress UI and urgency UI, which we suspect represents a transient change.
A number of potential mechanisms of action could explain the finding that women with stress and urgency UI have a higher probability of transitioning to mixed UI than in the reverse direction. One mechanism of how mixed UI develops may involve stress UI transitioning into urgency UI, or more likely, a stress event inducing an urgency UI episode, resulting in co-existing mixed UI symptoms [20]. Alternatively, persistent and severe urgency UI may lower the threshold for the onset of stress UI (or occurrence) leading to mixed UI. Future longitudinal studies with repeated surveys are needed to better characterize UI subtype progression and stages of disease. These findings suggest that a more comprehensive understanding of longitudinal UI experience would benefit from formal disease progression modeling that relies on an empirical or mechanistic approach to understanding mediators and modifiers of transition from one UI subtype to another [21]. Disease progression modeling could improve identification of prognostic factors and related interventions to slow or prevent transitions from stress UI or urgency UI to mixed UI. More formal use of disease progression models could also accommodate findings from a diversity of studies to inform or guide priorities for the development of prevention strategies and interventions that may help to modify or reverse the risk of disease progression into mixed UI, the UI subtype that is most challenging to treat.
Persistence of mixed UI or transition to mixed UI may be an indicator of disease progression. These findings also help to explain the paradox of why the observed prevalence of mixed UI is much higher than the expected prevalence, given the overall prevalence of stress and urgency UI and assuming independent co-occurrence of stress and urgency UI. First, stress UI prevalence peaks at an earlier age (fifth decade of life), whereas that of mixed UI peaks in late adulthood [1]. Second, as this current study shows, stress and urgency UI are more likely to transition to mixed UI (and do so at a faster pace) than vice versa. Third, in those who do not transition (i.e., persist), the Sandvik severity score is highest in women with mixed UI. Finally, remission data by Komesu et al. demonstrate that women with mixed UI are less likely to remit, and if they do, they are more likely to experience subsequent recurrent symptoms than women with either stress or urgency UI; furthermore, age-specific incidence of UI among women over 50 years of age does not vary by UI subtype [11]. These collective findings of incidence, transition, remission, and severity support the conclusion that progression of UI and its persistence favor an increasing prevalence of mixed UI with time and a dominance of this subtype at an older age.
Our bladder health survey was administered every 6 months. Most longitudinal UI studies survey individuals at longer time intervals (every 1 to 5 years) and demonstrate a high incidence coupled with high remission rates over time [6,7,8,9,10,11]. It could be argued that our transition data that favor progression of UI from pure the subtypes to mixed UI may be biased because of short term variability of symptoms, or because of the effect of confounders such as treatment on UI natural history. However, following our patients over 4 years revealed lower transition probabilities but similar trends over time. In addition, when potential confounders including age, BMI, and interventions such as medical or surgical treatment for UI were analyzed, none had an impact on transition rates (Table 3). In reality, it is well documented in epidemiological studies that only a minority of community-dwelling women seeks or receives care for UI [22].
A limitation to our study was a nonresponse rate of 35%. Nonresponders differed in certain demographic and clinical characteristics when compared with our active UI group. However, the response rate in our study was similar to or even higher than those of other population-based studies, and there is no evidence for a nonresponder bias in people over the age of 40 in surveys assessing urinary symptoms [23, 24]. Additionally, a number of potential confounders were significantly different between women who were included in the analysis versus those who were not. However, selection bias did not explain the differences in transition rates as the adjusted results for selection bias when estimating hazard ratios did not differ much from the unadjusted results. Accounting for both response bias and inclusion (or exclusion) of responders did not alter the main study findings, or their direction. Another limitation is that we only included women who were 40 years of age or older. As a result, it is not possible to ascertain if factors that occur before the age of 40, where prevalence of stress UI is dominant, may lead to co-existing and persistent stress and urgency UI (i.e., mixed UI). Finally, women with severe UI may be less likely to distinguish between stress and urgency UI, resulting in misrepresentation of the true estimates of transition rates across UI subtypes.
To conclude, UI is a highly dynamic condition that transitions from one subtype to another over time. Mixed UI is the most persistent subtype and least likely to transition when compared with stress and urgency UI. Based on the epidemiology of UI and its subtypes, it is possible that stress UI develops first, followed by urgency UI. Over time, we hypothesize that the co-occurrence of stress and urgency UI, or one subtype predisposing onset of the other promotes progression of UI into the more advanced stage of mixed UI.
References
Minassian VA, Stewart WF, Hirsch AG. Why do stress and urge incontinence co-occur much more often than expected? Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1429–40.
Coyne KS, Zhou Z, Thompson C, Versi E. The impact on health-related quality of life of stress, urge and mixed urinary incontinence. BJU Int. 2003;92:731–5.
Frick AC, Huang AJ, Van den Eeden SK, Knight SK, Creasman JM, Yang J. Mixed urinary incontinence: greater impact on quality of life. J Urol. 2009;182:596–600.
Dooley Y, Lowenstein L, Kenton K, FitzGerald M, Brubaker L. Mixed incontinence is more bothersome than pure incontinence subtypes. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1359–62.
Stewart WF, Minassian VA, Hirsch AG, Kolodner K, Fitzgerald M, Burgio K, et al. Predictors of variability in urinary incontinence and overactive bladder symptoms. Neurourol Urodyn. 2010;29:328–35.
Samuelsson EC, Victor FT, Svardsudd KF. Five-year incidence and remission rates of female urinary incontinence in a Swedish population less than 65 years old. Am J Obstet Gynecol. 2000;183:568–74.
Donaldson MM, Thompson JR, Matthews RJ, Dallosso HM, McGrother CW. Leicestershire MRC incontinence study group. The natural history of overactive bladder and stress urinary incontinence in older women in the community: a 3-year prospective cohort study. Neurourol Urodyn. 2006;25:709–16.
Hagglund D, Walker-Engstrom ML, Larsson G, Leppert J. Changes in urinary incontinence and quality of life after four years. A population-based study of women aged 22-50 years. Scand J Prim Health Care. 2004;22:112–7.
Nygaard IE, Lemke JH. Urinary incontinence in rural older women: prevalence, incidence and remission. J Am Geriatr Soc. 1996;44:1049–54.
Waetjen LE, Liao S, Johnson WO, Sampselle CM, Sternfield B, Harlow SD, et al. Factors associated with prevalent and incident urinary incontinence in a cohort of midlife women: a longitudinal analysis of data: study of women’s health across the nation. Am J Epidemiol. 2007;165:309–18.
Komesu YM, Schrader RM, Ketai LH, Rogers RG, Dunivan GC. Epidemiology of mixed, stress, and urgency urinary incontinence in middle-aged/older women: the importance of incontinence history. Int Urogynecol J. 2016;27:763–72.
Hirsch AG, Minassian VA, Dilley A, Sartorius J, Stewart WF. Parity is not associated with urgency with or without urinary incontinence. Int Urogynecol J. 2010;21:1095–102.
Minassian VA, Yan XS, Sun H, Platte RO, Stewart WF. Clinical validation of the bladder health survey for urinary incontinence in a population sample of women. Int Urogynecol J. 2016;27:453–61.
Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20:327–36.
Sandvik H, Seim A, Vanvik A, Hunskaar S. A severity index for epidemiological surveys of female urinary incontinence: comparison with 48-hour pad-weighing tests. Neurourol Urodyn. 2000;19:137–45.
Sandvik H, Espuna M, Hunskaar S. Validity of the incontinence severity index: comparison with pad-weighing tests. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:520–4.
Lunceford KJ, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effect: a comparative study. Stat Med. 2004;23:2937–60.
Little RJ, Vartivarian S. On weighting the rates in non-response weights. Stat Med. 2003;22:1589–99.
Efron B. Better bootstrap confidence intervals. J Am Stat Assoc. 1987;82:171–2.
Minassian VA, Yan XS, Pitcavage J, Stewart WF. Mixed incontinence masked as stress induced urgency urinary incontinence. J Urol. 2016;196:1190–5.
Cook SF, Bies RR. Disease progression modeling: key concepts and recent developments. Curr Pharmacol Rep. 2016;2:221–30.
Minassian VA, Yan X, Lichtenfeld MJ, Sun H, Stewart WF. The iceberg of health care utilization in women with urinary incontinence. Int Urogynecol J. 2012;23:1087–93.
Eaker S, Bergstrom R, Bergstrom A, Adami HO, Nyren O. Response rate to mailed epidemiologic questionnaires: a population based randomized trial of variations in design and mailing routines. Am J Epidemiol. 1998;147:74–82.
Dallosso HM, Matthews RJ, McGrother CW, Clarke M, Perry SI, Shaw C. An investigation into nonresponse bias in a postal survey on urinary symptoms. BJU Int. 2003;91:631–6.
Funding
Research reported in this publication was supported by the National Institutes of Health under Award Number #R01DK082551. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Minassian, V.A., Yan, X., Pilzek, A.L. et al. Does transition of urinary incontinence from one subtype to another represent progression of the disease?. Int Urogynecol J 29, 1179–1185 (2018). https://doi.org/10.1007/s00192-018-3596-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-018-3596-4