Abstract
Introduction and hypothesis
The aim of this study is to investigate changes in urinary nerve growth factor (NGF) and prostaglandin E2 (PGE2) in women with overactive bladder (OAB) following anticholinergic treatment.
Methods
A total of 30 female patients with OAB were enrolled and the control group included 15 healthy women who did not present any bladder symptoms. All subjects with OAB recorded voiding diaries, underwent urodynamic study, and were evaluated for urgency grade. They received anticholinergic treatment for 4 weeks, after which they were again evaluated for urinary urgency grade and voiding diaries. OAB patients were classified into three groups according to the change on the 5-point Urinary Sensation Scale after the treatment: group 1 (no change in urgency grade), group 2 (1 point of improvement), and, group 3 (more than 2 points of improvement). Urinary NGF and PGE2 levels between controls and OAB patients (before and after treatment in groups 1, 2, and 3) were compared.
Results
Urinary NGF and PGE2 levels were significantly higher in OAB patients than in the controls. NGF levels were not significantly different between pre- and post-treatment in groups 1 and 2. However, in group 3, NGF levels were significantly decreased after treatment. PGE2 levels were not significantly different between pre- and post-treatment in either group.
Conclusions
NGF and PGE2 have important roles in the development of OAB symptoms in women. Initial reduction of urgency severity after anticholinergic treatment in women with OAB could be associated with decreasing urinary NGF levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overactive bladder (OAB) is recognized as a “symptom syndrome suggestive of lower urinary tract dysfunction” and defined as “urgency, with or without urge incontinence, usually with frequency and nocturia.” Its overall prevalence in women is 12.8 % in Europe [1] and 16.9 % in the USA [2] and the prevalence increases with age. Its high prevalence rate has attracted growing interest. Although there have been several studies on the relationship between neural connections in the brain, spinal cord, and the detrusor muscle, the pathophysiology of OAB is still elusive. Moreover, prediction of treatment response remains limited. Nevertheless, it has been suggested that some neurotransmitters and inflammatory mediators, including nerve growth factor (NGF) and prostaglandin (PG), influence the symptoms of OAB in women. NGF is a small protein with key functions in the growth, maintenance, and survival of target neurons, including those of the sensory pathway. In the lower urinary tract, NGF is produced from bladder detrusor muscle and urothelium. It is noteworthy that NGF levels are elevated in the bladders of men with benign prostatic hyperplasia (BPH), in women with interstitial cystitis, and in idiopathic overactive bladder [3]. The role of NGF in storage symptoms, such as urgency and frequency, has been receiving the particular attention of urologists [4]. PGs are produced in the bladder muscle and mucosa via the cyclooxygenase (COX) pathway, which is related to the stretching of the detrusor muscle in response to bladder distension, inflammation, mucosal injury, nerve stimulation, and muscarinic receptor activation. PGs affect the micturition reflex by decreasing the thresholds of the stimuli necessary to trigger bladder contraction through activation of the capsaicin-sensitive afferent nerves [5–7]. Urinary prostaglandin E2 (PGE2) levels in OAB patients have been known to be increased and negatively correlated with the maximum cystometric capacity [8]. Estimation of NGF and PGE2 levels in patients with lower urinary tract symptoms (LUTS) including OAB might provide a diagnostic basis for OAB [9]. However, their use as therapeutic targets has not been investigated yet. The mainstay of pharmacological treatment for OAB is therapy with anticholinergic agents. In this study, we investigated the initial change in urinary NGF and PGE2 in women with OAB following anticholinergic treatment. Further, we evaluated the value of those changes in response to OAB treatment.
Materials and methods
We enrolled a total of 30 female patients (mean age 55 years, range 20–72 years) with symptoms of OAB and ≥3 urgency grade and ≥8 voids/24 h reported in 3-day voiding diaries. Patients were excluded if they had neurogenic bladder dysfunction, abnormal urinalysis or a history of recurrent urinary tract infection, stress urinary incontinence, and previous surgical intervention related to urinary symptoms. The control group included 15 healthy women (mean age 47.5 years, range 28–65 years) who visited our hospital for their regular checkup and did not present any LUTS and whose urinalysis revealed no abnormalities. All patients provided written informed consent, and the study protocols were approved by the Ethics Committee of our institution. All subjects with OAB recorded patient voiding diaries for 3 consecutive days, underwent urodynamic study, and were evaluated for urgency grade. Urodynamic parameters included the maximum flow rate, post-void residual volume, volume at first desire to void, maximum cystometric capacity and detrusor overactivity, and maximum detrusor pressure. Detrusor overactivity was defined as any involuntary detrusor contraction during the filling phase that was associated with the sensation of urgency or maximum cystometric capacity equal to less than 200 ml. Urinary urgency grade was classified according to the Urinary Sensation Scale (USS) and patients gave an overall score on the USS for all micturitions. Each point on the USS is the following:
-
1.
No urgency: no feeling of urgency; can continue activities until it is convenient to use bathroom
-
2.
Mild urgency: feel urgency; can easily tolerate; can finish usual activity and task quickly and then go right to the bathroom
-
3.
Moderate urgency: enough urgency discomfort; need to stop usual activity and task and go right to the bathroom
-
4.
Severe urgency: strong urgency discomfort; almost cannot hold urine; need to stop usual activity and task immediately and run to the bathroom to avoid a wetting accident
-
5.
Urge incontinence: extreme urgency discomfort; cannot hold urine and have a wetting accident before arriving at the bathroom
OAB patients received anticholinergic treatment (tolterodine 4 mg) for 4 weeks, after which they recorded voiding diaries for 3 consecutive days and were again evaluated for urinary urgency grade. OAB patients were classified into three groups according to the change on the USS after the treatment: group 1 (no change in urgency grade), group 2 (1 point of improvement), and group 3 (more than 2 points of improvement). We compared the results from the urodynamic study, voiding diaries, and urgency grade among the three groups.
Voided urine from all subjects was collected at full sensation to void. Urine samples were centrifuged at 3,000 rpm for 3 min. The liquid supernatant was separated into aliquots in 1.5-ml tubes and preserved at −80 °C. Voided urine from OAB patients was collected again under the same conditions after anticholinergic treatment. Urinary NGF and PGE2 levels were measured by the enzyme-linked immunosorbent assay (ELISA) method.
The urinary NGF concentration was determined using the Emax® ImmunoAssay System. For coating 96-well plates, 100 μl anti-NGF polyclonal antibody diluted in carbonate coating buffer [0.025 M sodium bicarbonate and 0.02 M sodium carbonate (pH9.7)] was pipetted into each well and incubated overnight at 4 °C after sealing the wells with an adhesive strip. Then, the wells were washed 3 times with TBST washing buffer (20 mM Tris-HCl, 150 mM NaCl, and 0.05 % Tween® 20). To prevent any nonspecific reaction, each well was incubated with 200 μl 1 × buffer and sample buffer for 1 h at room temperature. An NGF standard (prepared from the 1 μg/ml stock solution) or 100 μl urine was added to the wells. After a 6-h incubation, the wells were washed 5 times, 100 μl secondary antibody (2.5 μl anti-NGF monoclonal antibody diluted in 10 ml 1 × block and sample buffer) was added to each well, and the plates were incubated overnight at 4 °C. After washing 5 times, 100 μl anti-rat immunoglobulin (Ig) G horseradish peroxidase was added to each well and incubated for 2.5 h at room temperature. The wells were again washed 5 times and then incubated with 100 μl 3,3′,5,5′ tetramethylbenzidine (TMB, dissolved in a proprietary buffer) substrate solution for 10 min at room temperature. To terminate the reactions, 100 μl of 1 N HCl was added. The amount of NGF was determined by measuring the absorbance with an ELISA reader.
The amount of PGE2 was measured using a high-sensitivity ELISA kit. In antibody-coated wells, nonspecific binding (NSB) and maximum binding wells were marked as negative and positive controls, respectively. The assay buffer (in 21 ml of buffered protein base) was added to the NSB (200 μl) and the zero standard (B0) (150 μl) wells. Then, 150 μl of PGE2 standard or diluted urine samples (3:1) was pipetted into the remaining wells; 50 μl of anti-PGE2 antibody solution was added to each well, except the NSB wells. Then, 50 μl PGE2 conjugate was applied to all wells, which were covered with an adhesive strip and incubated for 16–20 h at 2–8 °C. After washing 3 times with 400 μl washing buffer, all liquid was removed from the wells; 200 μl of substrate solution was added to all wells and allowed to react for 20 min at room temperature after sealing with an adhesive strip. After adding 50 μl of stop solution (2 N sulfuric acid) to each well, the absorbance was measured with an ELISA reader.
Urinary NGF and PGE2 levels between controls and OAB patients (before and after treatment in groups 1, 2, and 3) were compared. We did not normalize NGF and PGE2 to the concentration of urinary creatinine (Cr) but measured total urinary NGF and PGE2.
All results are expressed as the mean ± standard error of the mean (SEM). The clinical characteristics of groups 1, 2, and 3 and the comparison of urinary NGF and PGE2 levels between controls and OAB patients (before and after treatment in groups 1, 2, and 3) were analyzed using Kruskal–Wallis tests. All other differences were determined using the Mann–Whitney U test. All analyses were conducted using the SigmaStat software for Windows®; P < 0.05 was considered statistically significant.
Results
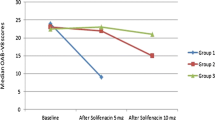
Of the 30 women with OAB, 7 (23.3 %) were assigned to group 1, 9 (30 %) to group 2, and 14 (46.7 %) to group 3. The grade of urinary urgency before anticholinergic treatment was 3.43 ± 0.20, 3.89 ± 0.31, and 4.57 ± 0.14 in groups 1, 2, and 3, respectively. Group 3 had significantly greater urinary urgency than the other 2 groups. However, other clinical characteristics were not different (Table 1). Urinary NGF and PGE2 levels were significantly higher in OAB patients than in the controls (Table 2). Urinary frequency changed from 11.29 ± 1.17 to 8.86 ± 0.88 in group 1, from 11.57 ± 1.31 to 8.57 ± 1.04 in group 2, and from 10.55 ± 0.84 to 7.64 ± 0.72 in group 3 from before to after treatment, respectively. The decrease in urinary frequency in group 3 was statistically significant (Fig. 1). Nocturia changed from 2.71 ± 0.42 to 1.57 ± 0.37 in group 1, from 3.22 ± 0.49 to 2.11 ± 0.42 in group 2, and from 2.46 ± 0.34 to 1.36 ± 0.15 in group 3 from before to after treatment, respectively. Again, the decrease in nocturia in group 3 was statistically significant (Fig. 2). Urinary urgency changed from 3.43 ± 0.20 to 3.43 ± 0.20 in group 1, from 3.89 ± 0.31 to 2.89 ± 0.31 in group 2, and from 4.57 ± 0.14 to 2.43 ± 0.14 in group 3 from before to after treatment, respectively. This decrease was statistically significant in group 3 (Fig. 3). Urinary NGF levels were not significantly different between pre-treatment and post-treatment in groups 1 and 2. On the other hand, in group 3, urinary NGF levels were significantly decreased after treatment than before treatment. Urinary PGE2 levels were not significantly different between pre-treatment and post-treatment in each group (Table 3).
Discussion
In this study, we found an association between urinary NGF, PGE2 levels, and OAB and between suppression of urinary urgency by anticholinergics and urinary NGF levels.
Sussman et al. [10] reported that responder rate for urgency in OAB patients who received treatment with tolterodine 4 mg was 78 % at week 12. The present study showed that 23 (76.7 %) of 30 women with OAB had reduced urinary urgency after anticholinergic treatment for 1 month and that 14 (46.7 %) women had less urinary sensation by 2 points or more. Pre-treatment clinical characteristics in OAB patients, including age, urodynamic study results, frequency, and nocturia, were not different. However, group 3, which showed more than 2 points of improvement after treatment, had significantly more severe urinary urgency than the other 2 groups. It is suggested that if patients have more severe urgency, then anticholinergics might exert their function more effectively, which means that there is a relationship between the severity of urinary urgency and the effect of anticholinergics. Consistent with the findings of a previous study [9], this study showed significantly increased urinary NGF and PGE2 levels in subjects with OAB as compared to the controls. It is possible that NGF and PGs play an important role in the activation of afferent neurons, which in turn induces OAB symptoms.
In the case of significant improvements of urinary urgency by anticholinergics, urinary NGF levels, but not urinary PGE2 levels, were significantly decreased as compared to pre-treatment levels. These results suggest that NGF is affected by anticholinergics. NGF controls the growth and survival of neurons and induces sensitization of nociceptive sensory neurons [11]. The mechanism of increasing NGF levels in OAB is not clear yet. Some studies reported that NGF hyperexpression in the bladder might be associated with mechanical stretching of the bladder [12] or bladder muscle hypertrophy [13] which results in bladder hyperactivity. Meanwhile, increased NGF in the bladder induces morphological and physiological changes in the afferent and efferent neurons [14]. Urinary NGF, tryptase, neurotrophin-3, and glial cell line-derived neurotrophic factor are increased in interstitial cystitis and bladder cancer [15]. Moreover, the levels of urinary NGF are higher in patients with urinary urgency and interstitial cystitis and in the urothelium of OAB patients compared with controls [9], as also shown by immunochemical staining [4]. All these reports showed that the expression of NGF in the bladder is associated with OAB. Some authors have suggested that NGF induces OAB by altering the properties or expression of the Na+ or K+ channels used by bladder afferent fibers. Indeed, alterations in NGF levels and in the channels of afferent nerve fibers have been observed after treatment for OAB or diabetic cystopathy [3]. Based on the presence of considerable NGF levels in the urine, researchers suggested the possibility of detecting changes in bladder function by means of diagnostic urinalysis. Giannantoni et al. [16] have shown that botulinum toxin A (BTX-A) reduces the levels of NGF in the bladder with detrusor overactivity and suggested that the decreased acetylcholine released at the presynaptic level induces decreased detrusor contractility and NGF production. Another possibility might be that decreased neurogenic inflammation is induced by BTX-A. Persson et al. [17] reported that stretching bladder smooth muscle cells in vitro increased expression of messenger RNA for NGF and stimulated the secretion of NGF. Our results showed that the levels of NGF in the OAB patients who had undergone anticholinergic treatment were decreased, which might be associated with suppression of the stretching of bladder smooth muscle as a consequence of improvement in the OAB symptoms.
PGs are synthesized from the bladder smooth muscle and the urothelium by physiological stimulation, such as stretching of the detrusor muscle, urothelial injury, nerve stimulation, and reaction to inflammatory mediators. PG may affect bladder activity directly by effects on the smooth muscle or indirectly via effects on neurotransmission [18]. The latter response is mediated by capsaicin-sensitive afferent neurons and might be blocked by capsaicin or tachykinin receptor antagonists [5, 19]. In fact, it has been reported that intravesically instilled PGE2 causes strong urgency sensation, resulting in reduced bladder capacity and ultimately leading to bladder instability [20]. Therefore, one can expect increased PG levels in OAB. In this context, other reports have shown that PGE2 levels are significantly higher than those of PGI2 and PGF2α in partial outlet obstruction of the rabbit bladder [21] and that PGE2 is increased in men with OAB symptoms [8]. Inhibition of COX—an enzyme important to the synthesis of PG—and decreased PG synthesis reduce the tone of bladder muscle strips [7]. Ketorolac, a PG synthesis inhibitor, reduces the frequency and severity of postoperative bladder spasm after ureteroneocystostomy [22]. Other reports have also shown that bladder symptoms are improved by inhibiting PG synthesis. However, our study showed that PGE2 levels were not different after improvement in OAB symptoms. Jin et al. [23] reported that the rat model with intravesical PGE2 administration was inappropriate for observing the effect of drugs or mechanisms on detrusor overactivity, because a small percentage of the intravesical pressure rises were confirmed as true detrusor overactivity. In addition, it is known that PGE2 facilitates afferent nerve activity via EP1 receptors [24]. PGE2 induced detrusor overactivity, which appears to be mediated only by the EP1 receptor [25]. If EP1 receptors are blocked by some mechanism which is related to anticholinergics, urinary urgency could be improved even though the PGE2 level is not decreased in the bladder. Our results showing suppression of urinary urgency in the absence of change in PGE2 levels is supported by these previous reports. However, the relationship between PGE2 and anticholinergics has been uncertain as yet, and further investigations on the relationship between anticholinergics and EP1 receptors are needed.
Additionally, only a very small percentage (25.3 %) of the women involved in this study had detrusor overactivity confirmed upon urodynamics. This result may be rather uncommon, as detrusor overactivity is thought of as one of the causes of OAB symptoms. However, the relationship between urgency and detrusor overactivity is unclear. Patients often report urgency without a rise in detrusor pressure [26]. In addition, the resolution of detrusor overactivity with treatment has been shown to bear less relation to improvement in OAB symptoms [27]. Because of the poor reliability and uncertain relationship to OAB severity and urodynamic study, we investigated new biomarkers of OAB such as NGF and PGE2 in this study.
The limitations of this study were that the enrollment numbers were small and we did not investigate serial changes of NGF and PGE2 after 4 weeks. Although OAB symptoms after anticholinergic treatment are reduced in the course of time, a considerable portion of median percent reductions in OAB symptoms were shown within 4 weeks. We could not provide information on persistence of changes in NGF and PGE2 levels; however, we focused on changes of NGF and PGE2 levels which are associated with most of the initial changes of OAB symptoms after treatment. Another limitation was that we did not normalize NGF to the concentration of urinary Cr but measured total urinary NGF. However, other studies showed that there was no significant difference in change of total urinary NGF levels and NGF/Cr levels in OAB [28]. We thought that the degree of hydration of each patient could affect the treatment of OAB. Keeping the difference of hydration without normalization by urinary Cr might reflect more natural results and responsiveness to the treatment.
NGF and PGE2 have important roles in the development of OAB symptoms in women. Initial reduction of urgency severity after anticholinergic treatment in female patients with OAB could be associated with decreasing urinary NGF levels. Further studies with a large number of female OAB patients should allow us to anticipate the response to anticholinergic treatment by determining changes in urinary NGF levels and associate those with the extent of anticholinergic treatment.
Abbreviations
- NGF:
-
Nerve growth factor
- PGE2 :
-
Prostaglandin E2
- OAB:
-
Overactive bladder
References
Irwin DE, Milsom I, Hunskaar S et al (2006) Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 50:1306–1314
Stewart WF, Van Rooyen JB, Cundiff GW et al (2003) Prevalence and burden of overactive bladder in the United States. World J Urol 20:327–336
Steers WD, Tuttle JB (2006) Mechanism of disease: the role of nerve growth factor in the pathophysiology of bladder disorders. Nat Clin Pract Urol 3:101–110
Lowe EM, Anand P, Terenghi G, Williams-Chestnut RE, Sinicropi DV, Osborne JL (1997) Increased nerve growth factor levels in the urinary bladder of women with idiopathic sensory urgency and interstitial cystitis. Br J Urol 79:572–577
Maggi CA (1992) Prostanoids as local modulators of reflex micturition. Pharmacol Res 25:13–20
Park JM, Schnermann JB, Briggs JP (1999) Cyclooxygenase-2. A key regulator of bladder prostaglandin formation. Adv Exp Med Biol 462:171–181
Bultitude MI, Hills NH, Shuttleworth KE (1976) Clinical and experimental studies on the action of prostaglandins and their synthesis inhibitors on detrusor muscle in vivo and in vitro. Br J Urol 48:631–637
Kim JC, Park EY, Hong SH, Seo SI, Park YH, Hwang TK (2005) Changes of urinary nerve growth factor and prostaglandins in male patients with overactive bladder symptom. Int J Urol 12:875–880
Kim JC, Park EY, Seo SI, Park YH, Hwang TK (2006) Nerve growth factor and prostaglandins in the urine of female patients with overactive bladder. J Urol 175:1773–1776
Sussman DO, Kraus SR, Carlsson M, Guan Z (2007) Onset of efficacy of tolterodine extended release in patients with overactive bladder. Curr Med Res Opin 23:777–781
Dmitrieva N, Shelton D, Rice AS, McMahon SB (1997) The role of nerve growth factor in a model of visceral inflammation. Neuroscience 78:449–459
Clemow DB, Steers WD, Tuttle JB (2000) Stretch-activated signaling of nerve growth factor secretion in bladder and vascular smooth muscle cells from hypertensive and hyperactive rats. J Cell Physiol 183:289–300
Steers WD, Kolbeck S, Creedon D, Tuttle JB (1991) Nerve growth factor in the urinary bladder of the adult regulates neuronal form and function. J Clin Invest 88:1709–1715
Steers WD, Ciambotti J, Erdman S, de Groat WC (1990) Morphological plasticity in efferent pathways to the urinary bladder of the rat following urethral obstruction. J Neurosci 10:1943–1951
Okragly AJ, Niles AL, Saban R et al (1999) Elevated tryptase, nerve growth factor, neurotrophin-3 and glial cell line-derived neurotrophic factor levels in the urine of interstitial cystitis and bladder cancer patients. J Urol 161:438–441
Giannantoni A, Di Stasi SM, Nardicchi V et al (2006) Botulinum-A toxin injections into the detrusor muscle decrease nerve growth factor bladder tissue levels in patients with neurogenic detrusor overactivity. J Urol 175:2341–2344
Persson K, Sando JJ, Tuttle JB, Steers WD (1995) Protein kinase C in cyclic stretch-induced nerve growth factor production by urinary tract smooth muscle cells. Am J Physiol Cell Physiol 269:C1018–C1024
Andersson KE (2002) Bladder activation: afferent mechanisms. Urology 59:43–50
Andersson KE (1993) Pharmacology of lower urinary tract smooth muscles and penile erectile tissues. Pharmacol Rev 45:253–308
Schüssler B (1990) Comparison of the mode of action of prostaglandin E2 (PGE2) and sulprostone, a PGE2-derivative, on the lower urinary tract in healthy women. A urodynamic study. Urol Res 18:349–352
Masick JM, Levin RM, Hass MA (2001) The effect of partial outlet obstruction on prostaglandin generation in the rabbit urinary bladder. Prostaglandins Other Lipid Mediat 66:211–219
Park JM, Houck CS, Sethna NF et al (2000) Ketorolac suppresses postoperative bladder spasms after pediatric ureteral reimplantation. Anesth Analg 91:11–15
Jin LH, Han JU, Park CS, Shin HY, Yoon SM, Lee T (2010) Intravesical PGE2 administration in conscious rats as an experimental model of detrusor overactivity observed by simultaneous registrations of intravesical and intraabdominal pressures. Int Neurourol J 14:69–77
Ikeda M, Kawatani M, Maruyama T, Ishihama H (2006) Prostaglandin facilitates afferent nerve activity via EP1 receptors during urinary bladder inflammation in rats. Biomed Res 27:49–54
Schröder A, Newgreen D, Andersson KE (2004) Detrusor responses to prostaglandin E2 and bladder outlet obstruction in wild-type and EP1 receptor knockout mice. J Urol 172:1166–1170
Digesu GA, Khullar V, Cardozo L, Salvatore S (2003) Overactive bladder symptoms: do we need urodynamics? Neurourol Urodyn 22:105–108
Nitti VW, Rovner ES, Bavendam T (2010) Response to fesoterodine in patients with an overactive bladder and urgency urinary incontinence is independent of the urodynamic finding of detrusor overactivity. BJU Int 105:1268–1275
Liu HT, Chen CY, Kuo HC (2011) Urinary nerve growth factor in women with overactive bladder syndrome. BJU Int 107:799–803
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cho, K.J., Kim, H.S., Koh, J.S. et al. Changes in urinary nerve growth factor and prostaglandin E2 in women with overactive bladder after anticholinergics. Int Urogynecol J 24, 325–330 (2013). https://doi.org/10.1007/s00192-012-1854-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1854-4






