Abstract
Purpose
The purpose of this study was to examine the predictive value concerning clinical outcome and implant survival, as well as the accuracy of individual tests of a recently published radiographic decision aid for unicondylar knee arthroplasty indication findings.
Methods
In the retrospective part of the study, 98 consecutive patients who had undergone unicondylar knee arthroplasty (Phase 3 Oxford medial UKA) were included, using revision questionnaires, as well as the Forgotten Joint Score-12 (FJS-12) and Knee Osteoarthritis Outcome Score (KOOS) and analysed for suitability of the radiographic decision aid. Inappropriate and appropriate indications were then compared concerning the clinical outcome and implant survival. The prospective part of the study assessed the accuracy of the decision aid's radiographic tests (varus and valgus stress views, true lateral view and skyline view), and included 90 patients. Definition as appropriate for UKA procedure included medial bone-on-bone situation in varus stress views, full-thickness lateral cartilage and functional medial collateral ligament in valgus stress views, functional anterior cruciate ligament (ACL) in true lateral views and absence of lateral facet osteoarthritis with bone loss in skyline views. Pre-operative radiographic assessment with respect to the decision aid was then compared with intraoperative articular conditions. The clinical outcome was analysed using non-parametric tests (Mann–Whitney U), and revision rates were compared using the Fisher’s exact test. Accuracy assessment included calculations of the sensitivity, specificity, negative predictive value and positive predictive value. A p value < 0.05 was considered statistically significant.
Results
Appropriate unicondylar knee arthroplasty with respect to the decision aid showed a significantly lower revision rate compared to inappropriate unicondylar knee arthroplasty (7.3% vs. 50.0%, p < 0.0001), as well as higher clinical outcome scores (FJS-12: 53.13 vs. 31.25, p = 0.041 and KOOS-QDL: 68.75 vs. 50.0, p = 0.036). The overall sensitivity (70.1%) and specificity (76.2%) for the radiographic decision aid was comparably low, which was essentially based on false negative cases (22.7%) regarding medial bone-to-bone conditions.
Conclusion
The radiographic decision aid is a helpful tool to predict clinical outcome and implant survival of mobile-bearing unicondylar knee arthroplasty. Strict use of the radiographic decision aid may lead to increased exclusion of appropriate patients with unicondylar knee arthroplasty implantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Unicondylar knee arthroplasty (UKA) is a widely used procedure to treat knee osteoarthritis (OA) with excellent clinical results [3, 11, 17, 24]. When compared to total knee arthroplasty (TKA), UKA is considered to provide certain advantages, like a shorter recovery time, better functional outcome scores, earlier return to pre-operative activity and higher patient satisfaction [7, 12, 17, 21, 24]. Nevertheless, UKA shows a more variable and decreased long-term implant survival, with higher revision rates in comparison to TKA [7, 11]. The higher incidence of UKA revision has been associated with implant malposition, surgical technique, as well as incorrect indication and especially incorrect patient selection [9, 13, 14, 16].
The correct indication for UKA remains debatable in the current literature. At present, anteromedial osteoarthritis (AMOA) and spontaneous osteonecrosis of the knee (SONK) are the main primary indications for UKA [2, 20]. Hence, identification of AMOA is crucial in patient selection for UKA. As patient factors like age, weight or level of daily activity reportedly do not compromise on outcomes, and are, therefore, no longer applied as contraindications, the indications for UKA especially depends on radiological criteria [2, 5, 6].
Recently, Hamilton et al. presented a radiographic decision aid for UKA, which included anteroposterior views, true lateral views, varus and valgus stress views and the patella axial view [5]. Suitability for UKA in the context of this decision aid is defined by (1) bone-to-bone OA in the medial compartment; (2) retained full-thickness lateral cartilage; (3) functionally intact medial collateral ligament (MCL); (4) functionally intact anterior cruciate ligament (ACL) and lack of severe damage to the lateral patellofemoral joint (PFJ) with bone loss, grooving and subluxation [5]. Hamilton et al. demonstrated superior functional outcome using the Knee Society Score and improved implant survival after UKA for patients meeting the criteria of the decision aid, in comparison to those not meeting the criteria [5].
The main purpose of this study was to examine the accuracy of the singular radiographic tests of the decision aid in a prospective comparison with intraoperative observations of intraarticular cartilage and ligament conditions. In contrast to our study, Hamilton et al. assessed the accuracy of the decision aid based on the procedure (UKA vs. TKA) was conducted, whereas the results of the singular tests were not considered for accuracy statistics. The secondary purpose of our study was to examine whether incorrect indications of UKA influence clinical outcome and implant survival in midterm follow-up in a cohort that is independent of the developers’ study of Hamilton et al. [5]. The purpose was to assess if comparable results in terms of clinical outcome and implant survival can be found in comparison to the developers’ study [5]. Regarding the high usage of the radiographic decision aid and its easy implementation in the clinical routine, the assessment of the radiographic tests’ accuracy is of high clinical relevance.
Materials and methods
This study was approved by the local ethics committee (Nr. 3299–2016/Nr. 3306–2016) and written informed consent was obtained from all study participants. The study consisted of two parts: part (1) retrospective implant survival and functional outcome based on meeting the decision aid criteria; and part (2) prospective radiographic decision aid accuracy in comparison with intraoperative findings.
Part (1): retrospective implant survival and functional outcome based on meeting the decision aid criteria
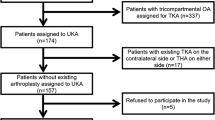
Between January 2009 and December 2011, 98 consecutive patients scheduled for UKA (Phase 3 Oxford medial UKA) underwent implantation via a minimally invasive approach by the same experienced surgeon (Fig. 1). Typical pre-operative diagnostic standards for the UKA procedure in the investigators’ clinic included all radiographs required for the decision aid. All patients were contacted to ascertain the current functional status of their knee and whether they had undergone re-operation or revision. Outcome assessments were performed for all cases of UKA, not revised or re-operated on, via postal questionnaire between September 2016 and September 2017. Clinical outcomes were assessed using the Forgotten Joint Score-12 (FJS-12) and Knee Injury Osteoarthritis Outcome Score (KOOS). Overall outcomes following cemented Phase 3 Oxford medial UKA were presented together with subgroup analysis comparing those identified by the decision aid as suitable with those identified as not suitable.
Part (2): decision aid accuracy compared with intraoperative findings
Between September 2016 and September 2017, 90 patients scheduled for knee arthroplasty by the same surgeon were included in the prospective part of the study. Apart from pre-operative radiological assessment (as described below), intraoperative articular surface assessment of the medial, lateral and patellofemoral compartments was conducted and the findings were recorded. The assessment was done using a 7-point modified surface scoring system established by Hamilton et al. [5]. Advanced surface damage leads to higher damage scoring (see Table 1). Additionally, ACL function (sufficient vs. insufficient) was tested with a tendon hook intraoperatively. The indications for UKA were defined as suitable intraoperatively, if damage scoring was ≥ 4 in the medial compartment, < 4 in the lateral compartment, < 7 in the patellofemoral compartment and if ACL function was sufficient. Intraoperative findings were then compared with the results of the pre-operative decision aid, to assess the accuracy of the radiographic subtests. Overall accuracy of the decision aid, as well as the accuracy of individual radiographic decision criteria were presented with the sensitivity (SEN), specificity (SPE), positive predictive values (PPV) and negative predictive values (NPV).
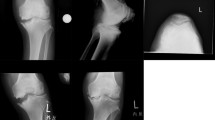
Radiographic assessment
Pre-operatively, all study participants were assessed clinically and radiographically with standing anteroposterior, varus and valgus stress views (15 Newton metres (NM)), skyline, as well as true lateral radiographs (see Table 2). All radiographs were assessed against the decision aid criteria, as described by Hamilton et al. [5], by two independent assessors (LT, PS) blinded to the clinical outcome, implant survival or intraoperative findings and procedures.
Statistical methods
Demographic parameters of study cohorts and subgroups were analysed descriptively and expressed as mean values of the minimum and maximum range. Analysis of the differences in clinical outcomes between subgroups was performed using non-parametric tests (Mann–Whitney U). The Fisher’s exact test was used to assess the differences in revision rate between appropriate and inappropriate UKA subgroups with respect to the decision aid. Accuracy assessment was performed, and several parameters were determined, as mentioned above. A p value < 0.05 was considered statistically significant.
Results
Part (1): implant survival and functional outcome based on meeting the decision aid criteria
Of the 98 consecutive medial UKA cases, 92 were unilateral procedures and three were bilateral, which were performed in a two-stage procedure. The mean age at the time of the operation was 69.1 years (range 53–84 years), and 31 patients were men (32.6%) and 64 were women (67.4%). A total of 71 UKA cases were available for assessment against the decision aid, owing to exclusion of 27 UKA cases, as shown in Fig. 1. The decision aid criteria were met in 55 UKA cases (77.5%). In all 16 UKA cases (22.5%), which did not meet the decision aid criteria, a single radiographic criterion was not appropriate. In such cases, 87.5% (14 knees) showed an incomplete medial collapse in stress views, 6.3% (one knee) showed lateral narrowing and 6.3% (one knee) showed posterior erosion in the true lateral view. Baseline demographics based on the decision aid criteria are outlined in Table 3. Baseline demographics showed no significant differences (Table 3).
Clinical outcomes were assessed for all UKA cases that were not revised (n = 59, 83.1%) and were made available for the decision aid assessment. At a mean follow-up of 6.68 years (range 5.58–8.42 years), the FJS-12 as well as the KOOS-QDL subscores were significantly higher for UKA cases that met all criteria of the decision aid (53.13 vs. 31.25, p = 0.041 and 68.75 vs. 50.0, p = 0.036). Although the remaining KOOS subscores showed no significant differences between the two groups, a distinct trend towards increased pain and reduced daily activity of the knees that did not meet the criteria was observed (Table 3, Fig. 2).
Comparison of clinical outcome scores and implant survival depending on radiological decision aid results. a Forgotten joint score-12, b knee injury and osteoarthritis outcome score (KOOS), c revision frequency of appropriate and inappropriate UKA cases. UKA unicompartmental knee arthroplasty, FJS forgotten joint Score, KOOS knee injury and osteoarthritis outcome score, ADL activity of daily life, QOL quality of life
Overall, 12 implant-related re-operations at a mean of 11.6 months (range 1–25 months) resulted in a 6-year survival of 83.1%. The appropriate UKA cases with respect to the decision aid showed a significantly lower revision rate, compared to the UKA cases that did not meet the decision aid criteria (7.3% vs. 50.0%, p < 0.0001). A detailed listing of revision causes is presented in (Fig. 1).
Part (2): decision aid accuracy compared with intraoperative findings
Of the 90 consecutive patients planned for knee arthroplasty operations (UKA or TKA), 68 (75.5%) were UKA procedures, 20 were (22.2%) TKA procedures and two (2.2) underwent an arthroscopy procedure. In those two cases, arthroscopy was performed prior to arthroplasty because of conflicting pre-operative indications. Both cases showed only tibial partial-thickness cartilage loss and preserved femoral cartilage, which led to cancellation of the arthroplasty procedure. The mean age at the time of operation in this group was 61.9 years (range 42–81 years), and 52.2% were men and 47.8% were women. The performance of the radiographic decision aid is outlined in Table 4.
Of those knees that met the criteria for the medial compartment in varus stress views, 98.3% (n = 56, bone-to-bone contact) showed an advanced cartilage defect, suitable for UKA. One knee (1.7%) alone showed partial-thickness cartilage loss, although it was considered suitable for UKA with respect to the decision aid (false positive). In addition, 57.7% of the knees that did not meet the criteria of the medial compartment (n = 15, no bone-to-bone contact) but showed a higher number of cartilage defects suitable for UKA implantation (false negatives).
In the valgus stress views, 89.0% of the knees met the criteria for the lateral compartment, showing an intact or minimally-damaged lateral compartment (n = 65). Consecutively, 11.0% of the knees considered suitable for UKA showed an advanced cartilage defect, leading to TKA implantation (n = 8). One knee (9.1%) showed only partial cartilage damage in the lateral compartment intraoperatively, although it was considered not suitable for UKA according to the decision aid.
Among the knees considered suitable for UKA with respect to ACL function in the true lateral radiographs, 92.1% demonstrated sufficient ACL function intraoperatively (n = 70). In line with this finding, 7.9% of the knees that met the criteria for functional ACL showed insufficient function intraoperatively (n = 6). On the other hand, 42.9% of the knees classified as not suitable showed fully sufficient function during surgery (n = 3, false negatives).
Advanced patellofemoral joint disease (“lateral patella facet osteoarthritis with bone loss”) was not observed in pre-operative radiographs or intraoperatively among all 90 consecutive cases. The assessment of MCL function in valgus stress views showed incomplete medial opening in five cases (5.6%). In all of those cases, at least two other criteria were not fulfilled; thus, a TKA was performed. Clinically, the MCL was stiffened intraoperatively in all cases.
Discussion
Patients with inappropriate indications for UKA with respect to the decision aid showed inferior clinical outcomes, as well as significantly higher revision rates, in comparison to patients with appropriate UKA indications in the midterm follow-up. These results are consistent with the findings of Hamilton et al. [5], who also observed lower functional outcome scores for UKA cases identified as not appropriate with respect to the decision aid, with a lower implant survival at a mean follow-up of 4.3 years. Hence, the decision aid might be a useful tool for pre-operative patient selection, especially with respect to outcome prediction.
In the present study, the most common reason for UKA identification as inappropriate with respect to the decision aid was missing medial bone-to-bone contact (87.5%). This suggests the assumption that partial cartilage damage in the medial joint compartment can lead to inferior clinical results and inferior implant survival. This observation is supported by the results of previous studies, which have also reported inferior clinical outcomes or higher revision rates in patients with partial-thickness cartilage loss or missing bone-to-bone contact [4, 15, 18, 19].
The most common reason for revision in patients with inappropriate decision aid indications was unexplainable persistent knee pain (37.5%), which was primarily treated with arthroscopic revision and secondarily with TKA implantation. Early revision, such as observed in the present study (13 months), and unexplainable persistent pain were also the most common reasons for revision observed by Maier et al. [15]. That group concluded that pre-operative knee pain in patients with such conditions might not be explained by cartilage damage alone.
In isolated cases only a single test of the radiographic decision aid might not meet the criteria for UKA indication, although all remaining tests support an UKA indication. In these cases, it is beneficial to know the accuracy of the singular tests to determine a correct indication or to initiate further diagnostic algorithm (e.g. additional MRI). Unnecessary exclusion for UKA indication might get reduced. To our knowledge, no study has been yet conducted to correlate the intraoperative articular condition with the findings of the radiographic decision aid. Currently, only the study of Hamilton et al. has investigated the accuracy of the radiographic decision aid in total [5]. In that study, Hamilton et al. [5] reported a sensitivity of 92% and a specificity of 88% for the decision aid, if only radiographic assessment is used. The present study showed a distinctly lower overall sensitivity (70.1%) and specificity (76.2%) for the radiographic decision aid. This is mostly due to false exclusion of appropriate patients (22.7% false negatives overall) leading to either low sensitivity or specificity of singular tests of the decision aid. In this context, it is noteworthy that sensitivity and specificity assume different meanings in the individual subtests.
While a positive test in varus stress views indicates that bone-to-bone contact is apparent, a positive test in valgus stress views indicates that the lateral joint space is intact. True lateral views and valgus stress views both showed excellent sensitivity (95.6% and 98.5%, respectively). Therefore, patients with lateral joint space narrowing and posterior erosion should be considered for TKA implantation. In 6.8% (n = 6, true lateral view) and 9.0% (n = 8, valgus stress views) of the cases, patients were identified as suitable for UKA, although intraoperative findings led to TKA implantation (false positives). When combined with a low number of true negative cases in these subtests, the specificity was low. This needs to be considered in pre-operative patient selection.
Nonetheless, assessment of the ACL and the lateral compartment is indispensable in intraoperative routines; therefore, these contraindications for UKA can be identified at the time of surgery. For this reason, it is mandatory to request patient consent for any possible changes in the procedure of TKA implantation. Moreover, in cases of unsuspected ACL deficiency intraoperatively, other techniques combined with UKA implantation show promising clinical outcomes and implant survival. A recently published fluoroscopy in vivo-study by Zumbrunn et al. [25] showed close to normal wave-form kinematics in patients with ACL deficiency after UKA implantation, compensated with intended posterior slope reduction. Tinius et al. [22] showed excellent implant survival and function scores for combined UKA implantation and ACL reconstruction in the midterm follow-up.
The results of the previous studies might suggest less restrictive indications for UKA implantation with respect to ACL function. Considering the fact that nearly 43% of the knees are classified as unsuitable for UKA implantation (false negatives) based on true lateral views, and assuming that ACL sufficiency showed full ACL function intraoperatively might reduce the number of false negative cases. Nevertheless, sufficient ligament function (ACL and MCL function) is crucial for UKA survival and function, and needs to be carefully considered, according to a recently published finite element model developed by Kwon et al. [10]. The ACL or MCL deficiency can lead to higher contact forces on the polyethylene insert and the lateral compartment, especially in varus morphotype patients, which might lead to inferior outcomes of medial UKA. Ligament deficiency, therefore, needs to be addressed thoroughly in cases of UKA implantation, with either a change in TKA implantation, combined slope compensation or ACL reconstruction.
The major reason for reduced test accuracy was the high number of false negative cases (n = 20). In 16 of those 20 cases, the decision aid was not appropriate for UKA implantation, with missing bone-to-bone contact, even though full-thickness cartilage loss (FTCL) in the medial compartment was observed intraoperatively. Owing to the number of false negative cases in the varus stress views, a decreased sensitivity and NPV was observed for this subtest. Maier et al. [15] showed that 23 out of 90 patients showed bone-to-bone contact in a different radiographic view, while no bone-to-bone contact was present in varus stress views. This might be considered when identifying the degree of cartilage damage in the medial compartment in varus stress views.
Furthermore, differentiation between medial PTCL and FTCL, as well as other diagnoses such as SONK and focal FTCL, appear to be challenging only with native radiographs. In this context, an extension of the diagnostic algorithm including MRI diagnostics might be considered in patients with missing medial bone-to-bone constitution, while typical symptoms and appropriate residual criteria of the decision aid are apparent in these patients. Further studies are needed to determine the extent to which MRI diagnostics help to identify patients with appropriate FTCL but lack bone-to-bone contact, and avoid unnecessary exclusion of patients for UKA implantation. Additionally, whether these patients benefit from UKA implantation compared to those with pre-operative bone-to-bone contact needs to be investigated.
Certain limitations of the present study must be considered. This study retrospectively analysed the clinical outcome of a mobile-bearing UKA, as well as midterm implant survival following implantation by the same surgeon. Pre-operative clinical and functional scoring data were not collected, leading to uncertainty regarding pre-operative functional status of the compared groups. Nevertheless, the study showed homogeneous groups with regard to demographic data, allowing an assumption of comparable pre-operative functional status between groups. Another limitation of this study was the group size of the retrospective study, with a limited number of UKA cases identified as not appropriate (n = 16); thus, statistical power was reduced.
Furthermore, the overall implant survival in our study (83%) at a mean follow-up of 6.6 years was inferior, when compared with the results of Hamilton et al. [5] (93%–98.9%, mean follow-up 6.7 years), Walker et al. [24] (92.4%, 10-year follow-up) as well as Mohammad et al. [16] (93%), recently published a 10-year follow-up meta-analysis. However, the revision rate was particularly high in the UKA cases identified as not appropriate (50%), which led to lower overall implant survival. If the implant survival is considered separately for the UKA cases identified as appropriate, a survival rate of 92.7% may be observed, which is comparable with the results of Mohammad et al. [16].
In addition, the literature shows heterogeneous long-term results for mobile-bearing UKA. In contrast to the previously cited survivorship studies, lower survival rates in a 10-year follow-up have been reported by the Finish prosthesis register [8], with 1819 UKAs (81%); Volte et al. [23], with the inclusion of 140 knees (82%); and Alnachoukati et al. [1], with 825 knees (85%). Another limitation of the present study is missing clinical data of the patients investigated in the prospective part, which would facilitate additional prospective clinical verification of the decision aid. Furthermore, this would add beneficial data to the study, the main aim of which was to compare intraoperative findings with subtest results, to investigate the accuracy of the radiographic decision aid.
Conclusion
The radiographic decision aid is a helpful tool to predict clinical outcomes as well as implant survival of mobile-bearing UKA. Nevertheless, strict use of the radiographic decision aid may lead to the exclusion of appropriate patients for UKA implantation, particularly because of a limited test accuracy for medial cartilage assessment. Therefore, the extension of the diagnostic algorithm with MRI diagnostics should be considered in sporadic cases.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- FTCL:
-
Full-thickness cartilage loss
- KOOS:
-
Knee Osteoarthritis Outcome Score
- KSS:
-
Knee Society Score
- LJ:
-
List JP
- MCL:
-
Medial collateral ligament
- MRI:
-
Magnetic resonance imaging
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- PTCL:
-
Partial-thickness cartilage loss
- SONK:
-
Spontaneous osteonecrosis of the knee
- TKA:
-
Total knee arthroplasty
- UKA:
-
Unicondylar knee arthroplasty
References
Alnachoukati OK, Barrington JW, Berend KR, Kolczun MC, Emerson RH, Lombardi AV Jr, Mauerhan DR (2018) Eight hundred twenty-five medial mobile-bearing unicompartmental knee arthroplasties: the first 10-year us multi-center survival analysis. J Arthroplasty 33:677–683. https://doi.org/10.1016/j.arth.2017.10.015
Berend KR, Berend ME, Dalury DF, Argenson JN, Dodd CA, Scott RD (2015) Consensus statement on indications and contraindications for medial unicompartmental knee arthroplasty. J Surg Orthop Adv 24:252–256
Bergeson AG, Berend KR, Lombardi AV Jr, Hurst JM, Morris MJ, Sneller MA (2013) Medial mobile bearing unicompartmental knee arthroplasty: early survivorship and analysis of failures in 1000 consecutive cases. J Arthroplasty 28:172–175. https://doi.org/10.1016/j.arth.2013.01.005
Hamilton TW, Pandit HG, Inabathula A, Ostlere SJ, Jenkins C, Mellon SJ, Dodd CA, Murray DW (2017) Unsatisfactory outcomes following unicompartmental knee arthroplasty in patients with partial thickness cartilage loss: a medium-term follow-up. Bone Joint J 99-B:475–482. https://doi.org/10.1302/0301-620X.99B4.BJJ-2016-1061.R1
Hamilton TW, Pandit HG, Lombardi AV, Adams JB, Oosthuizen CR, Clave A, Dodd CA, Berend KR, Murray DW (2016) Radiological decision aid to determine suitability for medial unicompartmental knee arthroplasty: development and preliminary validation. Bone Joint J 98-B:3–10. https://doi.org/10.1302/0301-620X.98B10.BJJ-2016-0432.R1
Kendrick BJ, Rout R, Bottomley NJ, Pandit H, Gill HS, Price AJ, Dodd CA, Murray DW (2010) The implications of damage to the lateral femoral condyle on medial unicompartmental knee replacement. J Bone Joint Surg Br 92:374–379. https://doi.org/10.1302/0301-620X.92B3.23561
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD (2018) Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc 26:1811–1822. https://doi.org/10.1007/s00167-017-4817-y
Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V (2007) Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop 78:128–135. https://doi.org/10.1080/17453670610013538
Kuipers BM, Kollen BJ, Bots PC, Burger BJ, van Raay JJ, Tulp NJ, Verheyen CC (2010) Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee 17:48–52. https://doi.org/10.1016/j.knee.2009.07.005
Kwon HM, Kang KT, Kim JH, Park KK (2019) Medial unicompartmental knee arthroplasty to patients with a ligamentous deficiency can cause biomechanically poor outcomes. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05636-7
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384:1437–1445. https://doi.org/10.1016/S0140-6736(14)60419-0
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint J 97-B:793–801. https://doi.org/10.1302/0301-620X.97B6.35155
Liow MH, Tsai TY, Dimitriou D, Li G, Kwon YM (2016) Does 3-dimensional in vivo component rotation affect clinical outcomes in unicompartmental knee arthroplasty? J Arthroplasty 31:2167–2172. https://doi.org/10.1016/j.arth.2016.03.003
Luscombe KL, Lim J, Jones PW, White SH (2007) Minimally invasive Oxford medial unicompartmental knee arthroplasty. A note of caution! Int Orthop 31:321–324. https://doi.org/10.1007/s00264-006-0202-z
Maier MW, Kuhs F, Streit MR, Schuhmacher P, Walker T, Ewerbeck V, Gotterbarm T (2015) Unicompartmental knee arthroplasty in patients with full versus partial thickness cartilage loss (PTCL): equal in clinical outcome but with higher reoperation rate for patients with PTCL. Arch Orthop Trauma Surg 135:1169–1175. https://doi.org/10.1007/s00402-015-2236-4
Mohammad HR, Strickland L, Hamilton TW, Murray DW (2018) Long-term outcomes of over 8,000 medial Oxford Phase 3 Unicompartmental Knees-a systematic review. Acta Orthop 89:101–107. https://doi.org/10.1080/17453674.2017.1367577
Morris MJ, Molli RG, Berend KR, Lombardi AV Jr (2013) Mortality and perioperative complications after unicompartmental knee arthroplasty. Knee 20:218–220. https://doi.org/10.1016/j.knee.2012.10.019
Niinimaki TT, Murray DW, Partanen J, Pajala A, Leppilahti JI (2011) Unicompartmental knee arthroplasties implanted for osteoarthritis with partial loss of joint space have high re-operation rates. Knee 18:432–435. https://doi.org/10.1016/j.knee.2010.08.004
Pandit H, Gulati A, Jenkins C, Barker K, Price AJ, Dodd CA, Murray DW (2011) Unicompartmental knee replacement for patients with partial thickness cartilage loss in the affected compartment. Knee 18:168–171. https://doi.org/10.1016/j.knee.2010.05.003
Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW (2015) The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Joint J 97-B:1493–1500. https://doi.org/10.1302/0301-620X.97B11.35634
Price AJ, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW, Oxford H, Knee G (2001) Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J Arthroplasty 16:970–976. https://doi.org/10.1054/arth.2001.25552
Tinius M, Hepp P, Becker R (2012) Combined unicompartmental knee arthroplasty and anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20:81–87. https://doi.org/10.1007/s00167-011-1528-7
Vorlat P, Putzeys G, Cottenie D, Van Isacker T, Pouliart N, Handelberg F, Casteleyn PP, Gheysen F, Verdonk R (2006) The Oxford unicompartmental knee prosthesis: an independent 10-year survival analysis. Knee Surg Sports Traumatol Arthrosc 14:40–45. https://doi.org/10.1007/s00167-005-0621-1
Walker T, Hetto P, Bruckner T, Gotterbarm T, Merle C, Panzram B, Innmann MM, Moradi B (2019) Minimally invasive Oxford unicompartmental knee arthroplasty ensures excellent functional outcome and high survivorship in the long term. Knee Surg Sports Traumatol Arthrosc 27:1658–1664. https://doi.org/10.1007/s00167-018-5299-2
Zumbrunn T, Schutz P, von Knoch F, Preiss S, List R, Ferguson SJ (2019) Medial unicompartmental knee arthroplasty in ACL-deficient knees is a viable treatment option: in vivo kinematic evaluation using a moving fluoroscope. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05594-0
Acknowledgements
L. Tuecking has nothing to disclose. Dr. Savov has nothing to disclose. PD Dr. Ettinger reports grants and personal fees from Smith & Nephew, personal fees from Stryker, Grants and personal fees from Waldemar Link Gmbh, grants and personal fees from Medacta, outside the submitted work. Prof. Dr. Windhagen reports personal fees from Aesculap, personal fees from Stryker, personal fees from Medacta, outside the submitted work.
Funding
No external source of funding was used for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LT, PS, TR, HW and ME declare that they have no conflict of interest.
Ethical approval
This study was approved by the local ethics committee (Nr. 3299–2016/Nr. 3306–2016).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tuecking, LR., Savov, P., Richter, T. et al. Clinical validation and accuracy testing of a radiographic decision aid for unicondylar knee arthroplasty patient selection in midterm follow-up. Knee Surg Sports Traumatol Arthrosc 28, 2082–2090 (2020). https://doi.org/10.1007/s00167-020-05912-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05912-x