Abstract
Purpose
While the classical indications and contraindications for unicondylar knee arthroplasty (UKA) are widely accepted there is not yet consensus if patients with partial thickness cartilage loss (PTCL) are equally suited for treatment with UKA. The aim of our study was to determine if patients with partial thickness cartilage loss do equally well after treatment with UKA.
Methods
The study retrospectively analyzed the clinical results as well as the survival rates of 64 patients treated with UKA with the medial Oxford knee system. 32 patients had shown PTCL on preoperative radiographs, while the matched control group presented with full thickness cartilage loss (FTCL) medially. Outcome parameters were the Oxford Knee Score (OKS), the American Knee Society Score (AKS), and radiographic analysis.
Results
Postoperative improvement in OKS was 16 (SD 9.0) for patients with PTCL and 17 (SD 8.1) for patients with FTCL. There were no significant differences in the clinical scores between the two groups. Five Patients with PTCL had reoperation whereas there were only two in the bone on bone group. Cumulative survival at 5 years for all revisions was 84 % (95 % CI 72–92 %) for the PTCL group and 97 % (95 % CI 92–100 %) for the FTCL group. This difference was not yet significant (log rank: p = 0.095).
Conclusions
Patients with PTCL are not equally suited for treatment with UKA like patients with bone on bone. Although PTCL has equal clinical results, it was associated with higher revision rates in our series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medial unicondylar knee arthroplasty (UKA) is an increasingly popular method of knee replacement in patients with isolated anteromedial osteoarthritis (OA) of the knee with very good long-term results [1–3]. It is recommended that UKA should be done if there is full thickness cartilage loss (FTCL) with “bone on bone” visible on the preoperative radiograph [4]. However, it is still unclear how to treat patients who suffer from similar clinical symptoms while meeting all the other criteria for UKA, except FTCL. To date there are only two studies analyzing the results of the Oxford UKA in patients with partial thickness cartilage loss (PTCL) in the affected compartment. Pandit et al. [5] showed that in patients with intraoperative finding of PTCL the clinical results were not as good as in patients with FTCL. Niinimäki et al. measured the medial and lateral joint space widths in the middle of the respective compartments on the preoperative radiographs and calculated the ratio of the medial/lateral joint space and expressed it as a percentage. They could demonstrate that the reoperation rate was significantly higher in patients with a medial joint space >2 mm or with the ratio of the medial/lateral joint space of >40 % [6]. Because of different conclusions in their studies how to deal with patients with PTCL the present study used the recommended Oxford X-ray criteria to distinguish between full and partial thickness cartilage loss and to determine a possibly different outcome for these two groups.
The purpose of this retrospective study was to compare the clinical results and implant survival of patients with medial unicompartmental OA with FTCL to patients with PTCL, analyzed in preoperative radiographs. The hypothesis was that there are differences in clinical outcome and revision rate comparing FTCL and PTCL patients.
Patients and methods
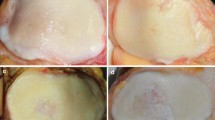
From 2001 to 2009, a total of 624 cemented medial Oxford UKA phase 3 was performed in 556 patients with anteromedial osteoarthritis. A retrospective analysis of preoperative varus stress radiographs regarding joint space width of the medial compartment was done. These radiographs were performed with the patient in supine position and with a wedge under the relevant knee leading to 20° flexion. Varus stress was applied with up to 15 daN by a manual device (“telos”; Marburg, Germany). The X-ray beam was tilted by 10° and centered to the middle of the femorotibial joint space parallel to the tibial joint space. 90 patients (90 knees) who showed residual joint space width in the medial compartment on varus stress radiographs were identified (Fig. 1). To ensure that there is partial thickness cartilage loss 4 radiographs of these patients were analyzed: ap and lateral weightbearing, varus stress, and full leg standing. 33 patients were identified with PTCL in all 4 radiographs, while the other patients showed full thickness cartilage loss (FTCL). From the FTCL group, a matched control group of 32 patients was defined. Matching criteria were gender, preoperative Oxford Knee Score (OKS), age at operation, and time to follow-up. Table 1 shows the demographics of both groups. The patients were clinically evaluated prospectively and the data were reviewed retrospectively. Informed consent was obtained from all patients. The study was approved by the ethics committee at the University of Heidelberg, Germany, and it was conducted in accordance with the Declaration of Helsinki of 1975, as revised in 2008.
All cemented Oxford UKA (phase 3) surgeries were performed at our department by 16 experienced surgeons through a minimally invasive incision. At a mean follow-up of 3.9 years (SD 1.6) the patients were assessed for clinical and functional outcome. Assessment for each patient included complete physical examination of the knee as well as documentation of the Oxford Knee Score (OKS) [7] and the American Knee Society (AKS) Score [8]. The Oxford Knee Score was used in the modified form reaching from 0 to 48 with 48 as the best result as proposed by Murray et al. [9].
Statistical analysis
The statistical analysis was done using SPSS Version 21.0 (SPSS Inc., Chicago, IL, USA). The main outcome measure was the difference between the preoperative OKS and the one at the last follow-up. The change in OKS of the two groups with analysis of covariance for significant difference was compared. All other clinical scores were analyzed using Student’s t test. p values of <0.05 were considered to be significant. Revision rates were calculated with Kaplan–Meier survival analysis and compared using the log-rank test. A test for the following endpoints was done: reoperation for any reason, reoperation for unexplained pain, implant-related revision.
Results
Sample
Minimum follow-up was 2 years except for patients who died or had earlier revision surgery. 3 patients of the PTCL group and 2 of the FTCL group had died. None of those five had any reoperation at the affected knee. With this information survival analysis could be done for all patients. Except for the patients who had revision surgery or died all others completed the questionnaires so that the OKS score and AKS Function Score were available for statistical analysis.
Clinical evaluation
PTCL group
The mean OKS improved from preoperatively 25 (SD 7.4, range 13–41) to postoperatively 41 (SD 5.8, range 28–48) in the PTCL group (Table 2). The mean change of 16 (SD 9.0, range 1–33) was statistically significant (p < 0.001). The mean AKS improved from preoperatively 46 (SD 13, range 26–76) to postoperatively 88 (SD 10, range 67–100). The mean AKS Function Score improved from preoperatively 58 (SD 21, range 20–90) to postoperatively 83 (SD 20, range 20–100). Mean Pain on the VAS reduced from 7.9 (SD 1.9, range 4–10) to 1.9 (SD 2.1, range 0–6). All these changes were highly significant (p < 0.001). Mean maximum flexion was 122° (SD 12°, range 95–150°) preoperatively and improved to 127° (SD 8°, range 110–140°) postoperatively. This change was also significant (p = 0.047).
FTCL group
In the bone on bone group, the mean OKS improved from preoperatively 25 (SD 6.8, range 14–37) to postoperatively 42 (SD 6.5, range 28–48) (Table 2). The mean change of 17 (SD 8.1, range −2 to 34) was statistically highly significant (p < 0.001). The mean AKS Knee Score improved from preoperatively 44 (SD 11, range 23–74) to postoperatively 87 (SD 16, range 54–100). The mean AKS Function Score improved from preoperatively 56 (SD 23, range 5–100) to postoperatively 86 (SD 18, range 30–100). Mean pain on the VAS reduced from 7.5 (SD 1.7, range 4–10) to 1.5 (SD 2.3, range 0–8). Mean maximum flexion was 110° (SD 11°, range 90–140°) preoperatively and improved to 125° (SD 9°, range 110–140°) postoperatively. All these changes were highly significant (p < 0.001).
Comparison of both groups
With p = 0.50 in the analysis of covariance, there was no significant difference in the absolute mean values and in the change of OKS and AKS between the two groups. Comparing the other clinical scores, pain on the VAS and maximum flexion at the last follow-up, none of them showed a significant difference (Figs. 2, 3, 4; Table 2).
Implant survival and revision surgery
In the PTCL group, 5 reoperations occurred whereas there were only 2 in the bone on bone group. Table 3 gives an overview of the reoperations. One more patient with PTCL had progressive pain for several years with a focus on the lateral side of the knee compartment. The radiographs at the time of last follow-up showed OA progression with decreasing joint space in the lateral compartment so we suggested at 7.2 years of follow-up revision to TKA.
PTCL group
There were two revisions for unexplained pain in the PTCL group: the first patient developed increasing pain after 12 months and underwent arthroscopic resection of a plica synovialis. One more patient with PTCL also presented progressive pain after 13 months. In this patient, a free joint body was found and removed performing the arthroscopy.
The 3rd patient with PTCL had an exchange of the mobile bearing because of early infection. Another had revision to total knee arthroplasty (TKA) after infection after 44 weeks with subsequent removal and secondary implantation of the TKA. Another revision to TKA was down after 12 months because of loosening of the femoral component with femoral osteolysis.
FTCL group
One patient with bone on bone had knee revision the 3rd day after primary operation because of intra-articular fixed Redon drainage. Another patient from this group had clinical and radiographic loosening of the femoral component and was revised to TKA after 7.9 years.
Survivorship analysis
Kaplan–Meier survival analysis, with the endpoint revision for any reason, estimated the 5-year survival rate at 84 % (95 % CI 72–92 %; 4 knees at risk) for the PTCL group and 97 % (95 % CI 91–100 %; 5 knees at risk) for the FTCL group. Comparing these two survival rates with the log-rank test, the difference was not yet significant (p = 0.095) (Fig. 5). Using revision for unexplained pain as the endpoint, five year survival was estimated at 94 % (95 % CI 84–100 %; 4 patients at risk) for the PTCL group and 100 % for the FTCL group. The difference was not significant (log rank: p = 0.140) (Fig. 6). With implant-related revision as the endpoint, cumulative survival was estimated at 91 % (95 % CI 80–100 %) for the PTCL group and 100 % for the FTCL group. This was not yet a significant difference (log rank: p = 0.083) (Fig. 7).
Discussion
The hypothesis of the present study was that there are differences in clinical outcome and revision rate comparing FTCL and PTCL. The results show, that patients with PTCL are not equally suited for treatment with UKA like patients with bone on bone. Although PTCL has equal clinical results it was associated with higher revision rates in our series.
Although a 27-year Finnish registry study has shown a lower survivorship of different UKAs in comparison to total knee arthroplasty survivorship, the medial Oxford UKA has documented very good medium and long-term clinical results with survival rates of 91 % after 20 years [10]. The classic indication for a UKA with the Oxford system is anteromedial osteoarthritis [11] presented with full thickness cartilage loss and bone on bone in the preoperative stress or standing radiographs [12, 13]. In clinical practice, there are some mid-aged patients with appropriate clinical symptoms (anteromedial pain; “one-finger-sign”) but only PTCL (partial thickness cartilage loss). Until today, the question remains, whether these patients also benefit from an UKA. Therefore, the purpose of this study was to compare patients with appropriate clinical symptoms with full and partial thickness cartilage loss in the medial compartment regarding their clinical outcome and revision rate.
There are only two studies published, focusing on this issue. There is a developer study by Pandit and Murray from 2011 [5]. They reviewed retrospectively the surgical reports and 29 of 1000 Oxford knees with an intraoperatively documented incomplete cartilage loss in the medial compartment. They compared this PTCL group with patients with full thickness cartilage loss. The clinical outcome of their PTCL group was significantly lower with respect to the change in Oxford Knee Score (OKS). In contrast, the results of the present study did not show any significant differences in the absolute and relative changes of the clinical scores between the two groups. Also reduction of pain and gain in range of motion was without significant difference between patients with bone on bone and the ones with PTCL. Therefore, the present study did not show that patients with PTCL do not benefit from the implantation of an Oxford prosthesis concerning clinical outcome.
Niinimäki et al. [6] retrospectively analyzed 113 medial Oxford prosthesis and correlated the revision rate with joint space on preoperative standing weight bearing radiographs. Their results showed that the revision rate did increase 6-fold with a medial joint space ≥2 mm. Additionally, they found that if the ratio of medial to lateral joint space was >40 %, the revision rate was even 8 times higher. Niinimäki et al. [6] concluded that in medial knee osteoarthritis, UKA should only be used if the preoperative medial joint space on standing radiographs is ≤40 % of the lateral joint space. Pandit [5] recommended to use a UKA only if there is bone on bone in medial compartment osteoarthritis. This discrepancy between the two studies led to the question how to deal with it if we define full and partial thickness cartilage loss not by using arthroscopy or MRI but by using the recommended Oxford X-ray criteria [14]. They recommended 4 preoperative radiographs—anteroposterior, lateral, varus stress, and valgus stress. Based on this, an anteromedial osteoarthritis of the knee can be divided into full (FTCL) and partial thickness cartilage loss (PTCL).
In the present study, the differences in the survival rates had a trend to lower values with PTCL without reaching statistical significance. Comparing with the results from Niinimäki et al. [6], there is the same tendency that patients with PTCL seem to have higher reoperation rates following implantation of an Oxford UKA. Quite striking is the aspect that all five reoperations in the PTCL group were within the first 13 months. In this short period of time, wear is very unlikely to be the reason for the revision. Instead it strengthens the assumption that the source of the knee pain in these patients is different, and cannot be treated appropriately by the implantation of an UKA. Very revealing was also the observation that of 90 knees that had shown PTCL in the varus stress radiograph, 23 showed bone on bone in at least one further radiograph. Especially, the lateral and the standing weight bearing view offered additional and more precise information in all cases. Therefore, there is a strong recommendation to evaluate joint space narrowing in the above-mentioned manner. In contrast to Pandit and Niinimäki, the present data showed an equally good clinical outcome comparing UKA in PTCL to FTCL medial knee osteoarthritis patients.
Revision for unexplained pain had to be done in 2 patients with PTCL. The first patient had an arthroscopic resection of a synovial plica which did not lead to persistent pain relief. No free joint body or any other source of the pain could be detected during the arthroscopic surgery. The other patient with revision for unexplained pain equally had no improvement by arthroscopic removal of a free joint body. Both situations strengthen the assumption that the cause for the pain is not the damaged cartilage but to be found elsewhere. With early and late infection (3 and 44 weeks postoperatively) and intraoperatively proven loosening of the femoral component, there were obvious reasons for revision done in three other patients with PTCL.
The present study has some limitations. The focus was on the preoperative radiographs for the classification and did not include preoperative MRI or intraoperative findings. Beside the small number of patients this is probably the main limitation. Further studies, eventually multicentered to increase the number of patients, are necessary to see in what extent preoperative MRI can help to predict clinical outcome in PTCL and who will benefit from implantation of an Oxford UKA. In conclusion patients with PTCL are not equally suited for treatment with UKA than patients with bone on bone because it is associated with higher revision rates.
Conclusion
In medial compartment osteoarthritis, patients with PTCL are not equally suited for treatment with UKA than patients with full thickness cartilage loss. Although PTCL has equal clinical results in our study, it might be associated with higher revisions rate. To define whether there is FTCL, we recommend to evaluate the knee joint space in all four—anteroposterior, lateral, standing weight bearing, and varus/valgus stress—radiographs.
References
Price AJ, Waite JC, Svard U (2005) Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res 435:171–180
Newman J, Pydisetty RV, Ackroyd C (2009) Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. Bone Joint J 91(1):52–57
Manzotti A, Confalonieri N, Pullen C (2007) Unicompartmental versus computer-assisted total knee replacement for medial compartment knee arthritis: a matched paired study. Int Orthop 31(3):315–319
Murray DW, Goodfellow JW, O’Connor JJ (1998) The Oxford medial unicompartmental arthroplasty: a 10-year survival study. Bone Joint J 80(6):983–989
Pandit H et al (2011) Unicompartmental knee replacement for patients with partial thickness cartilage loss in the affected compartment. Knee 18(3):168–171
Niinimaki TT et al (2011) Unicompartmental knee arthroplasties implanted for osteoarthritis with partial loss of joint space have high re-operation rates. Knee 18(6):432–435
Dawson J et al (1998) Questionnaire on the perceptions of patients about total knee replacement. Bone Joint J 80(1):63–69
Insall JN et al (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Murray DW et al (2007) The use of the Oxford hip and knee scores. Bone Joint J 89(8):1010–1014
Price AJ, Svard U (2011) A second decade lifetable survival analysis of the Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res 469(1):174–179
White SH, Ludkowski PF, Goodfellow JW (1991) Anteromedial osteoarthritis of the knee. Bone Joint J 73(4):582–586
Aldinger PR et al (2004) Medial unicompartmental knee replacement using the “Oxford Uni” meniscal bearing knee. Der Orthopade 33(11):1277–1283
Mukherjee K et al (2008) The Oxford unicompartmental knee arthroplasty: a radiological perspective. Clin Radiol 63(10):1169–1176
Gibson PH, Goodfellow JW (1986) Stress radiography in degenerative arthritis of the knee. Bone Joint J 68(4):608–609
Acknowledgments
This study was supported by the non-commercial research fund of our department.
Conflict of interest
Michael W. Maier, Felix Kuhs, Marcus R. Streit, Peter Schuhmacher, Tilman Walker, Volker Ewerbeck, Tobias Gotterbarm: the authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maier, M.W., Kuhs, F., Streit, M.R. et al. Unicompartmental knee arthroplasty in patients with full versus partial thickness cartilage loss (PTCL): equal in clinical outcome but with higher reoperation rate for patients with PTCL. Arch Orthop Trauma Surg 135, 1169–1175 (2015). https://doi.org/10.1007/s00402-015-2236-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2236-4