Abstract
Purpose
As the correct rotational and sagittal alignment of the tibial tray are of key importance for optimal total knee arthroplasty (TKA) function, the objective of this study was to determine these individual variations in the proximal tibial geometry in terms of posterior tibial slope (PTS) and tibial surface asymmetry by analysing a large dataset of computer tomography (CT) information.
Methods
A retrospective two-part review was performed on 15,807 datasets that were generated during the design phase for a customized TKA implant. First, 15807 CAD (computer-aided-design) models derived from CT data were used to conduct the analysis on the variation of the PTS. Second, the axial cut of each proximal tibia in a consecutively selected subset of 2202 datasets was used to measure the tibial asymmetry.
Results
The majority (65.5%) of tibiae had a posterior slope between 5° and 10°, while 26.5% of knees had a slope > 10°. The asymmetry measured as offset between the lateral and medial posterior boundaries was highly variable, with overall an increasing proportion of patients with high asymmetry with increasing tibial ML width. Only 14% of tibiae exhibited symmetric (< 2 mm offset) lateral and medial plateaus, and 22% had an offset > 5 mm.
Conclusion
This study from an extraordinary large data base reveals that tibial posterior slope and asymmetry of the tibial profile vary largely between patients receiving TKA with increasing tibial asymmetry with ML width. CT scans might help to preoperatively better select the best fitting TKA, otherwise surgeons intraoperatively will often have to deal with compromises regarding fitting, sizing and rotational issues.
Level of evidence
Retrospective case series, Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Personalised medicine has been introduced into total knee arthroplasty (TKA) [11] to overcome some of the limitations associated with standard TKA including low patient satisfaction of around 20% of the patients [4, 21]. The idea of tailoring the surgical approach closely to the patient’s anatomy implies that the specific anatomic variability is closely appreciated during reconstruction [11]. To descriptively address the anatomic complexity of different knee joints, scientist have begun to phenotype native [20] and osteoarthritic [10] knees morphologically and also functionally according to their respective coronal femoral and tibial alignment [12], which holds great promise for defining meaningful subgroups in future comparative outcome studies on surgical treatments of knee osteoarthritis (OA).
Apart from the coronal alignment there are many other topographical features that are of key importance for favourable outcomes in TKA surgery. In a previous study we investigated the extent of anatomic variability of the distal femur in a large computed tomography (CT) data base, with particular interest in the anterior–posterior (AP) and mediolateral (ML) width, as well as the condylar offsets and its implications for TKA [18, 20]. For the tibial anatomy, coronal alignment has been also intensively investigated in previous studies as outlined in a current systematic review [10], while there is only limited data on horizontal tibial offset, tibial AP and ML width, as well as PTS in the context of TKA implant design [8]. However, these issues are of key clinical importance, as outcome depends strongly on proper placement of TKA components, which includes optimal rotational alignment and proper bony surface coverage [17]. Moreover, sizing issues such as component overhang has been shown to cause soft tissue irritation resulting in pain and is associated with a decreased range of motion [3], while undercoverage may lead to subsidence and loosening of the implant [5]. Malrotated components can cause several problems such as patella maltracking and instability [1]. In addition, PTS plays a key role in knee kinematics because of its influence on inter alia sagittal plane stability, tibial load transfer and flexion ability [2, 9] and is mostly proposed in a fixed manner (0°, 5° or 7°) according to the instrumentation manuals of different TKA systems.
As there is no large-scale analysis of tibial asymmetry and PTS in the context of TKA surgery in the literature to date, it is hypothesised that by analysing an extraordinary large dataset of CT information on proximal tibial geometry, we are able to determine the individual variations in in terms of tibial surface asymmetry, AP and ML width, as well as PTS.
Materials and methods
Study design and setting
A retrospective review was performed on 15,807 datasets that were generated during the design phase for a customized, individually manufactured TKA implant from December 2013 to April 2016.
Participants/study subjects
The dataset was drawn from a cross-section of European and US-American patients.
Variables, outcome measures, data sources
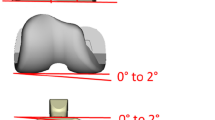
Data analysis was done in two parts. The first included analysing 15807 CAD (computer-aided-design) models derived from CT data for the proximal tibia that are used to design the implants. These were used to conduct the analysis on the variation of the posterior slope (PTS). The CT scans of the lower limb included the centre of hip, a detailed scan of the distal femur and proximal tibia and the ankle centre. The ankle joint centre was used to determine the mechanical axis of the tibia (Fig. 1). For determining the medial tibial slope, first a plane was defined to be perpendicular to the mechanical axis of the tibia. Then, a line was determined as the tangent to the most prominent aspects of the anterior and posterior cortices of the respective medial tibia. The PTS was then defined as the angle between plane perpendicular to the tibial mechanical axis and the line connecting the anterior and posterior prominences of the proximal tibia in the sagittal plane (Fig. 1).
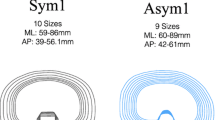
The second aspect of the analysis was carried out on a consecutively selected subset of 2202 datasets, where the axial cut of each proximal tibia was used to measure the tibial asymmetry. The rotational orientation of the tibial profile in the axial plane was determined according to the method of Cobb et al. [7] using best fit circles on the lateral and medial tibial condyle (Fig. 2). The axis passing through the centre of the medial and lateral circles was used to determine the ML-axis of the tibial tray. The axis perpendicular to this determines the anterior–posterior (AP) direction. The medial and lateral AP widths were determined via the anteriormost aspect of the patient specific profile measured to the posteriormost aspect of the patient specific profile for each condylar area. The difference between the medial and lateral AP widths was defined as the tibial asymmetry or horizontal tibial offset. The tibial asymmetry data were first analysed as a whole and then bucketed into 4 groups based on ML width (ML tibial width < 65 mm, 65–75, 75–85, > 85) and 6 groups based on the amount of asymmetry (< 1 mm, 2–3, 3–4, 4–5 and > 5).
An implant fit analysis was conducted using ML and tibia medial AP dimensions of the data set when compared with modern symmetric (S) TKA (Attune® Knee System; DePuy Synthes, Warshaw, IN, USA) and asymmetric (AS) TKA sizes (Persona® Knee System, Zimmer Biomet Inc, Warsaw, IN, USA). The sizes were determined from company data. For each TKA size, the implant medial AP and ML measurements were recorded and plotted along with the CT data of our patient population. The sizes of modern S-TKA and AS-TKA that fell outside the FDA clearance of our data base were excluded from the analysis.
Statistical analysis
Data analysis was performed using inbuilt and custom functions in MS Excel (Redmond, WA-USA) and Minitab 17.1 (State College, PA-USA).
Results
Posterior tibial slope (PTS)
The average PTS for the whole population of 15,807 patients was determined to be 7.4° (SD 3.47°). 65.5% of patients had a posterior slope between 5° and 10°. Of the remaining population 26.5% of patients exhibited a PTS ≥ 10°, while 8% of patients exhibited a PTS of < 5°.
Tibial width and asymmetry
Analysis of the tibial axial view revealed an average medial AP length of 49.45 mm (SD 4.41), an average lateral AP length of 45.74 mm (SD 4.27) and an average tibial asymmetry of 3.70 mm (SD 1.62). The average tibial ML width was 74 mm (SD 6.0 mm). Only 14% of tibiae were symmetric (< 2 mm asymmetry) and 64% of patients showed a tibial asymmetry between 2 and 5 mm. 22% of the tibiae were distinct asymmetric (> 5 mm asymmetry) (Table 1; left columns). To identify any correlation between asymmetry and ML-widths of the tibia, the dataset was separated into four groups of different ML-widths: < 65 mm, 65–75 mm, 75–85 mm and 85 mm. Each and every degree of asymmetry as defined above was observed in every ML-group. With increasing ML-widths, the proportion of symmetric tibiae (< 2 mm asymmetry) decreased from 26 to 9%, while the proportion of asymmetric tibiae (5 mm asymmetry) increased from 8 to 27%. Accordingly, there was a trend in the amount of asymmetry based on the overall ML width of the tibia, with proportion of patients with high asymmetry increasing with tibial ML-width (Table 1; right columns).
Implant fit analysis
In the S-TKA group, a potential mismatch between the patient’s bony anatomy and the dimensions of the tibial component was identified, with their tibial medial AP dimension being smaller than that of the tibial S-TKA implant, expecially for large ML diameter (> 70 mm) (Fig. 3) in many cases. Conversely, in the AS-TKA group, the tibial medial AP diameter was often times bigger than that of the tibial AS-TKA implant, throughout the range of ML dimension (Fig. 4).
Discussion
The key findings of our study were that using an extensive CT data base, the extent of variability of the PTS on the one hand and tibial asymmetry on the other hand could be described in a large gonarthrosis patient population to a degree, that has not been recognized in the literature to date.
Firstly, our hypothesis that the range of variability of the PTS could be clarified has been confirmed. Our data differs to some extent to those of Ho et al. who found high variability of the PTS determined by CT scans of n = 100 knees of an Asian population with a mean of 11° (range 5°–17°) [14]. Our data are in agreement with Meric et al. also found very high variability of the PTS determined using CT scans of n = 13,546 knees of a population of mixed countries (Europe, Asia, Middle East, Africa) with a mean of 7.2° with a reference range of − 5° to 25° [19]. In contrast, our data were generated from a cross section of the currently largest population to our knowledge in the literature (n = 15,807) from Europe and North America, with a mean PTS of 7.4° (range − 9 to 26°). This is of interest, as manufacturers of standard TKA systems such as P.F.C.® Sigma® and Attune® (both DePuy Synthes Johnson & Johnson) recommend using 0° of PTS (e.g. P.F.C.® PS) in cruciate substituting designs, or 3° of PTS (P.F.C.® CR) or 5–7° of PTS (Attune®) for cruciate retaining designs. Correlating the findings of the present study to the recommendations in these surgical technique guides, revealed that the postoperative PTS would be less than the patient’s native, preoperative PTS for a large number of patients. Presently, there is no generally accepted optimal angle of the PTS in TKA for ideal postoperative knee function which is also strongly dependent on the TKA implant design. An increase in PTS may affect the postoperative knee function in either a positive or a negative way: with increasing PTS flexion angle increases while quadriceps force for flexion decreases [2, 15, 22, 23]. On the other hand, excessive increase of PTS may cause anterior sliding and impingement of the tibial component, along with flexion instability [22, 25].
Secondly, our hypothesis that we were able to describe a variation for the tibial asymmetry has also been confirmed (Table 1; Figs. 3 and 4). This corresponds to the work of Dai et al. who also found a high variability of tibial surface geometry determined using CT scans and 3D models of n = 347 knees of a population of mixed ethnicities (Caucasian, Japanese, Indian) using a multifaceted approach to quantify morphology [8]. Interestingly, they found for each ethnic group, males had higher values than females for all dimensional and area measurements, and among ethnicities Caucasians had larger values than Indians for all dimensional and area metrics, and larger values than Japanese [8]. Concerning asymmetry Indians females had less AP asymmetry than Caucasian females; Indian males had less AP asymmetry than Japanese and Caucasian males [8]. In contrast to this work, we were not able to differentiate between gender and ethnicity; however, we were able to extract an increasing tendency towards asymmetry with increasing ML diameter (Table 1) due to the use of the Cobb-method on a large-scale data set (n = 2202). Another interesting finding of the present study was also that all ML-groups exhibited different degrees of asymmetry within each group, and that overall only 14% of tibiae were symmetric (< 2 mm asymmetry) (Tab. 1). Considering this small amount together with the fact, that a lot of TKA designs still have symmetric tibial trays renders the task of rebuilding the tibia in its natural shape to be a challenging one.
The variation in the AP and ML dimensions of the proximal tibia are demonstrated in Figs. 3 and 4, showing possible mismatches between a symmetric implant and the patient’s bony surface (Fig. 3) and between an asymmetric standard implant and the patient’s bony surface (Fig. 4). The challenge with using either symmetric or asymmetric implants having a fixed geometry lies in maintaining proper rotation while providing maximum coverage. Therefore, surgeons often are required to downsize the tibial implants to maintain proper axial rotation, while avoiding overhang of the tibial components. Increased sizing options and the availability of asymmetric tibial implants do alleviate some of these issues, but may not be able to address the varying geometry in the population of patients. Martin et al. [17] in their study utilized 30 CT reconstructions of tibial specimens to determine the effect of malrotation and sizing of two symmetric and two asymmetric implant designs. They reported that when tibiae are placed to maximize orientation, 70% of all tibiae were on average 9° internally rotated [17]. Asymmetric tibiae had a lower occurrence of malrotation than symmetric tibia’s, but 28% and 52% of asymmetric tibiae exhibited malrotation. Schroeder et al. [24] investigated the occurrence of tibial misfit in 44 patients undergoing TKA, using 3 implants with symmetric designs and 1 implant with a customized design. Implants were sized to minimize overhang, while maintaining proper rotation. They found that 18% of the symmetric implants exhibited tibial implant overhang > 3 mm, and none of the customized implants exhibited overhang [24]. Component underhang was seen in 37% of the symmetric tibial implants and 18% of customized TKA [24]. Rotational analysis conducted in the same paper showed that when the tibiae were sized to maximize coverage, 45% of symmetric tibiae exhibited > 5° of rotational mismatch [24]. Asymmetric designs do reduce the occurrence of sizing and rotational mismatches when compared to symmetric tibial implants, however, they have a fixed asymmetry between 5 and 7 mm as in the Persona® Knee System (Zimmer Biomet Inc., Warsaw, IN, USA). In contrast, our data showed that the majority of patients exhibit an asymmetry between 2 and 5 mm (average of 3.7 mm; SD 1.62 mm), which complies with values from the following literature: Yoshioka et al. [26] examined the articular geometry of the tibia on 31 cadaveric lower legs. Their mean medial AP width was 48 mm (SD 5.0) and their mean lateral AP width was 42 mm (SD 3.7), resulting in a mean asymmetry of the tibial plateau of 6 mm. Kwak et al. [16] did measurements of the cut surface of 200 tibiae of 100 Korean cadavers. As was done in the present study, they evaluated the degree of asymmetry by the difference between medial and lateral AP width and obtained 3.8 mm (SD 2.8) as mean of asymmetry. Cheng et al. [6] did a morphometric analysis of 172 knees of Chinese patients. They found that the medial AP width was larger than the lateral AP width by an average of 5.4 mm (SD 2.8). Hitt et al. [13] collected morphologic data of the proximal tibia from 337 knees during total knee arthroplasty. They reported that the medial AP width was larger than the lateral AP width by a mean of 5.2 mm (SD 3.1) for men and by 4.3 mm (SD 3.1) for women. The present study represents the largest CT dataset investigating AP and ML dimensions and also PTS of the proximal tibia so far in a representative European and North-American cross-section of patients. Therefore, possible mismatches between the implant and the patient’s bony surface resulting from the variability and potentially impairing the functional outcome of TKA could be evaluated.
The study had a number of limitations that need to be considered. Firstly, we measured the PTS on CAD models of the proximal tibia derived from CT data. Therefore, soft tissue information, including the cartilage thickness and menisci were not included in the model. Though this might present a limitation in interpreting the results of our study, the large dataset analysed here, provided the readers with an accurate idea on the variation of the PTS in patients receiving TKA.
Another limitation of the study is that the mapping of the tibial offset data and its correlation to tibial widths was conducted on a subset of patients from the larger population since analysis of the profile for the larger dataset was not possible. The consecutive selection of the subset does limit the chance of selection bias, but does not eliminate the possibility of it. However, the resultant subset is still large enough (n = 2202), and we believe this subset analysis is still an important finding of the study that demonstrated the variation in tibial AP offset between the medial and lateral compartments seen in patients requiring TKA.
Furthermore, as the dataset generated for this paper includes implant dimensions that are generated from the design process of a customized TKA, it does not include patient demographic information, and this study cannot apply equally to men and women or different groups of ethnicities. Of course, the conclusions drawn are limited to cases that fall into the range of sizes supported by the collected data. Accordingly, the conclusion drawn apply to patients having knees with dimensions falling into the FDA clearance range of customized TKA. The study does not apply to small knees with dimensions that do not fall in the clearance range, therefore probably representing parts of an Asian population. However, to our best knowledge, this is the largest dataset evaluated so far depicting a representative cross-section of European and US-American patients and highlighting that surgeons intraoperatively have to deal with individual anatomic geometries.
Not only the geometry of the tibia, but also of the femur shows a high degree of variability [18]. Since said study highlights the variability in femoral geometry only, while the present study highlights variability in tibial geometry only, both studies do not address the full complexity which results from interaction between tibia, femur and patella along with its interconnecting soft tissues. In the end, only considering both the variability in geometry of the femur as well as of the tibia and the effects resulting from interaction between femur and tibia may allow a reliable conclusion. This is beyond the topic of the paper which, however, highlights important differences to be addressed pre- as well as intraoperatively.
Lastly, all measurements were based on three-dimensional models of the knee joint and may therefore not be directly transferrable into the situation surgeons face intraoperatively. However, the data presented in this paper does provide important information on the variations of the tibial geometry that will help surgeons better plan sizing and correct placement of the tibial component. To the authors best knowledge, this is the greatest CT dataset evaluated of tibial morphology so far.
Conclusion
The study demonstrated that tibial posterior slope and asymmetry of the tibial plateau vary widely between patients receiving TKA. CT scans might help to preoperatively better select the best fitting TKA, otherwise surgeons intraoperatively will often have to deal with compromises regarding fitting, sizing and rotational issues.
References
Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L (2001) Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 392:46–55
Bellemans J, Robijns F, Duerinckx J, Banks S, Vandenneucker H (2005) The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 13:193–196
Bonnin MP, Schmidt A, Basiglini L, Bossard N, Dantony E (2013) Mediolateral oversizing influences pain, function, and flexion after TKA. Knee Surg Sports Traumatol Arthrosc 21:2314–2324
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Carpenter DP, Holmberg RR, Quartulli MJ, Barnes CL (2014) Tibial plateau coverage in UKA: a comparison of patient specific and off-the-shelf implants. J Arthroplasty 29:1694–1698
Cheng FB, Ji XF, Lai Y, Feng JC, Zheng WX, Sun YF et al (2009) Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee 16:341–347
Cobb JP, Dixon H, Dandachli W, Iranpour F (2008) The anatomical tibial axis: reliable rotational orientation in knee replacement. J Bone Jt Surg Br 90:1032–1038
Dai Y, Bischoff JE (2013) Comprehensive assessment of tibial plateau morphology in total knee arthroplasty: influence of shape and size on anthropometric variability. J Orthop Res 31:1643–1652
Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD (2007) Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med 35:1443–1449
Hess S, Moser LB, Amsler F, Behrend H, Hirschmann MT (2019) Highly variable coronal tibial and femoral alignment in osteoarthritic knees: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:1368–1377
Hirschmann MT, Friederich NF, Becker R, Karlsson J (2019) Personalised medicine in knee arthroplasty: we need more science! Knee Surg Sports Traumatol Arthrosc 27:1357–1358
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Hitt K, Shurman JR, Greene K, McCarthy J, Moskal J, Hoeman T et al (2003) Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am 85-A(Suppl 4):115–122
Ho JPY, Merican AM, Hashim MS, Abbas AA, Chan CK, Mohamad JA (2017) Three-dimensional computed tomography analysis of the posterior tibial slope in 100 knees. J Arthroplasty 32:3176–3183
Jojima H, Whiteside LA, Ogata K (2004) Effect of tibial slope or posterior cruciate ligament release on knee kinematics. Clin Orthop Relat Res 426:194–198
Kwak DS, Surendran S, Pengatteeri YH, Park SE, Choi KN, Gopinathan P et al (2007) Morphometry of the proximal tibia to design the tibial component of total knee arthroplasty for the Korean population. Knee 14:295–300
Martin S, Saurez A, Ismaily S, Ashfaq K, Noble P, Incavo SJ (2014) Maximizing tibial coverage is detrimental to proper rotational alignment. Clin Orthop Relat Res 472:121–125
Meier M, Zingde S, Steinert A, Kurtz W, Koeck F, Beckmann J (2019) What is the possible impact of high variability of distal femoral geometry on TKA? A CT data analysis of 24,042 knees. Clin Orthop Relat Res 477:561–570
Meric G, Gracitelli GC, Aram L, Swank M, Bugbee WD (2015) Tibial slope is highly variable in patients undergoing primary total knee arthroplasty: analysis of 13,546 computed tomography scans. J Arthroplasty 30:1228–1232
Moser LB, Hess S, Amsler F, Behrend H, Hirschmann MT (2019) Native non-osteoarthritic knees have a highly variable coronal alignment: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:1359–1367
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Nunley RM, Nam D, Johnson SR, Barnes CL (2014) Extreme variability in posterior slope of the proximal tibia: measurements on 2395 CT scans of patients undergoing UKA? J Arthroplasty 29:1677–1680
Okamoto S, Mizu-uchi H, Okazaki K, Hamai S, Nakahara H, Iwamoto Y (2015) Effect of tibial posterior slope on knee kinematics, quadriceps force, and patellofemoral contact force after posterior-stabilized total knee arthroplasty. J Arthroplasty 30:1439–1443
Schroeder L, Martin G (2019) In vivo tibial fit and rotational analysis of a customized, patient-specific TKA versus off-the-shelf TKA. J Knee Surg 32:499–505
Shelburne KB, Kim HJ, Sterett WI, Pandy MG (2011) Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res 29:223–231
Yoshioka Y, Siu DW, Scudamore RA, Cooke TD (1989) Tibial anatomy and functional axes. J Orthop Res 7:132–137
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
One of the authors (SZ) is an employee of Conformis Inc (Billerica, MA, USA) and received compensations between 100,000 and 1,000,000. He also received stock values between 10,000 and 100,000. One of the authors (LS) received an intern research scholarship from Conformis Inc. One of the authors certifies that he (AS) has received personal fees for consultant teaching, during the study period, in an amount of less than USD 10,000 from Conformis Inc (Billerica, MA, USA), outside the submitted manuscript. One of the authors certifies that he (JB) has received personal fees for consultant teaching, during the study period, in an amount of less than USD 10,000, from Smith & Nephew (Smith & Nephew GmbH, Hamburg, Germany), Conformis Inc (Billerica, MA, USA) and DePuy Synthes (Umkirch, Germany), all outside the submitted manuscript.
Ethical approval
Since the present study is based on analysing anonymised CT data, IRB approval was not required. Any information that could identify patients was not used in the analysis. Investigators and Statistician dealt with anonymised data only. All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964. Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Every patient involved agreed by giving informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Johannes Beckmann and Andre Friedrich Steinert share senior authorship.
Rights and permissions
About this article
Cite this article
Meier, M., Zingde, S., Best, R. et al. High variability of proximal tibial asymmetry and slope: a CT data analysis of 15,807 osteoarthritic knees before TKA. Knee Surg Sports Traumatol Arthrosc 28, 1105–1112 (2020). https://doi.org/10.1007/s00167-019-05728-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05728-4