Abstract
Purpose
It is proposed that central femoral ACL graft placement better controls rotational stability. This study evaluates the consequence of changing the femoral tunnel position from the AM position drilled transtibially to the central position drilled transportally. The difference in ACL graft failure is reported.
Methods
This prospective consecutive patient single surgeon study compares the revision rates of 1016 transtibial hamstring ACL reconstructions followed for 6–15 years with 464 transportal hamstring ACL reconstructions followed for 2–6 years. Sex, age, graft size, time to surgery, meniscal repair and meniscectomy data were evaluated as contributing factors for ACL graft failure to enable a multivariate analysis. To adjust for the variable follow-up a multivariate hazard ratio, failure per 100 graft years and Kaplan–Meier survivorship was determined.
Results
With transtibial ACLR 52/1016 failed (5.1%). With transportal ACLR 32/464 failed (6.9%). Significant differences between transportal and transtibial ACLR were seen for graft diameter, time to surgery, medial meniscal repair rates and meniscal tissue remaining after meniscectomy. Adjusting for these the multivariate hazard ratio was 2.3 times higher in the transportal group (p = 0.001). Central tunnel placement resulted in a significantly 3.5 times higher revision rate compared to an anteromedial tunnel placement per 100 graft years (p = 0.001). Five year survival was 980/1016 (96.5%) for transtibial versus 119/131 (90.5%) for transportal. Transportal ACLR also showed a significantly higher earlier failure rate with 20/32 (61%) of the transportal failing in the first year compared with 14/52 (27%) for transtibial. (p = 0.001.)
Conclusion
Transportal central femoral tunnel ACLR has a higher failure rate and earlier failure than transtibial AM femoral tunnel ACLR.
Level of evidence
Level II—prospective comparative study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Based on anatomical time zero biomechanical and clinical studies, “Anatomic ACL reconstruction” with a central femoral ACL footprint has been advocated to improve rotatory knee stability and outcome, with the aim of reducing post-ACL reconstruction osteoarthritis [2, 4, 6,7,8, 11, 15,16,17, 23, 25]. In response to these studies many surgeons changed their surgical technique from a transtibial approach which results in a high-anteromedial femoral tunnel placement to a transportal technique, in which the femoral tunnel position can be placed centrally in the ACL footprint.
When changing to the transportal central footprint the senior author found a higher and earlier ACL graft rupture rate. The Danish ACL registry [28] reported a significantly higher failure rate with transportal ACL reconstruction compared with transtibial ACL reconstruction. In response to the senior author’s early findings and the Danish Registry study [28] a study to determine whether there was a higher ACL graft failure rate in the senior authors hands was performed.
The hypothesis was that the central femoral footprint transportal technique would have a higher failure rate than the AM femoral footprint transtibial technique.
The Danish Registry studies [28] have proposed that the technique learning curve is the reason for the higher failure with a transportal technique. This study reports the experience of a high volume ACL surgeon. A significant increase in failure rate is thus unlikely to be due the learning curve enabling an analysis of other factors.
Materials and methods
A prospective cohort of 1480 consecutive patients who underwent ACL hamstring reconstruction surgery performed by a single surgeon between 2000 and 2013 were included in this study. In 1016 cases from 2000 to 2009, ACL reconstruction was performed using a transtibial technique, utilizing an oblique shallow tibia tunnel with an eccentrically place femoral tunnel within the original ACL footprint in the anteromedial bundle region. This technique enables the graft to lie within the femoral footprint, thus it is anatomically placed. It is thus different from the vertical ACL graft that is commonly criticized with the transtibial technique which is placed outside the anatomical femoral footprint.
The surgical technique was changed in 2009 to a transportal technique, in which the tibial and femoral tunnel were drilled separately, resulting in a longer and more anteriorly located tibial tunnel as well as a femoral tunnel placed centrally in the ACL footprint.
Graft fixation was similar in both groups.
Similar suspensory devices (Smith and Nephew, Endobutton Continuous Loop or Arthrex, Retrobutton RT) were used for femoral fixation while an intra tendon tibial screw and sheath device (Mitek, Intrafix or Arthrex, Graftbolt) were used for tibial fixation. All patients underwent the same ACL rehabilitation and return to activity program.
Patients were followed for a minimum of 2 years. The revision rate of transtibial hamstring ACL reconstructions followed for 6–15 years was compared with transportal hamstring ACL reconstructions followed for 2–6 years. ACL failure was determined by clinical failure and MRI confirmation with or without subsequent ACL revision surgery.
In addition, patient age, sex, graft size, time to surgery, as well as data regarding meniscal repair and meniscectomy procedures were collected and evaluated as contributing factors for ACL graft failure to enable a multivariate analysis.
Ethical approval was granted by the New Zealand Ethics Committee to evaluate this ACL cohort.
Statistical analysis
To adjust for the variation in follow-up of the two groups three statistical methods were evaluated. The hazard ratio, failure per 100 graft years and a Kaplan–Meier survivorship.
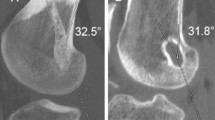
Figure 1 arthroscopic femoral tunnel positions.
Results
The revision rate after ACLR using a transtibial technique was 5.1% (52 revisions from 1016 ACL reconstructions). The revision rate after ACLR using a transportal technique was 6.9% (32 revisions from 464 ACL reconstructions). As the two groups had a different follow-up period the hazard ratio was utilized to adjust for the longer follow-up of the transtibial group. A transportal ACLR technique showed a significantly 2.4 times higher hazard ratio compared to a transtibial ACLR technique (p = 0.001).
Other factors were shown to be contributory to ACL failure (Table 1).
Significant differences were seen regarding graft diameter, time to surgery, medial meniscal repair rates and medial and lateral percent of remaining meniscal tissue after partial meniscectomy procedures No significant difference was seen regarding patient age, sex, or lateral meniscal repair rates.
A multivariate hazard ratio was thus determined to adjust for these possibly confounding variables.
After adjustment for all factors, the multivariate hazard ratio was significantly 2.3 times higher in the transportal group compared to the transtibial group (p = 0.001).
Another statistical method to adjust for variable follow-up is to evaluate the failures per 100 graft years. This evaluation is common place in joint registries. The transportal revision rate showed 0.14 failures per 100 graft years, while the transtibial revision rate showed 0.04 failures per 100 graft years. Thus, a central femoral tunnel placement resulted in a significantly 3.5 times higher revision rate compared to an AM tunnel placement per 100 graft years (p = 0.001).
Kaplan–Meier survivorship at 5 years was 980/1016 (96.5%) for transtibial versus 119/131 (90.5%) for AM femoral tunnel (Fig. 2).
Furthermore, the transportal ACLR technique showed a significantly higher earlier failure rate as 61% of the transportal ACL graft failures occurred in the first year post-surgery, while 27% of the transtibial ACL graft failures occurred in the first year post-surgery (p = 0.001). Finally, smaller graft diameter, younger patient age and concomitant medial meniscal repair procedures resulted in a significantly higher revision rate.
Discussion
The most important finding of this study is that moving the femoral tunnel from an anteromedial position drilled transtibially to a central position drilled transportally resulted in a higher and earlier ACLR failure.
In the early 1990s the all arthroscopic transtibial ACL reconstruction technique was popularized. This resulted in a more vertical graft with a femoral tunnel that was often outside the native ACL footprint. This was combined with a posteriorly placed tibial tunnel, which enabled the femoral tunnel to be placed at the back of the notch and avoid graft notch impingement.
The move to a central femoral tunnel placement, followed a period of popularity of double-bundle techniques and was based on anatomical studies showing a large femoral footprint that was more forward (distal) and lower (posterior) than the transtibially drilled femoral tunnel [11].
Time zero biomechanical studies of a centrally placed graft showed better rotational control than grafts placed outside the femoral footprint [2, 6, 7, 15,16,17, 23]. It was, therefore, proposed that the central femoral graft position with its more normal knee kinematics would reduce the incidence of graft failures, meniscal re-tears and further chondral damage and thus decrease the incidence of osteoarthritis [4, 11].
Two clinical studies have evaluated this by comparing ACL grafts placed outside the femoral footprint with a centrally placed ACL graft.
In the MOON group study [8], it was shown that the transtibial group had a 1.8X higher rate of subsequent meniscal surgery and a 3.4X higher rate of chondral surgery 6 years post-procedure than the transportal group.
In the Oxafor et al. study [25] non-anatomic graft placement demonstrated a significant decrease in cartilage thickness along the medial intercondylar notch in the operative knee relative to the intact knee (8%) while in the anatomic graft placement group, no significant changes were observed. It is, however, important when evaluating the significance of this paper that no differences were observed elsewhere in the knee and the area where changed occur was small and takes minimal load.
It is important to appreciate that these studies that criticized the transtibial technique placed a vertical ACL graft outside of the femoral ACL footprint which was not the case with patients from this study.
The Danish ACL Registry [28] was the first group to show a significantly higher failure rate with an anteromedial portal technique. This study and Williams [31], who has a very high demand patient population group, have shown a similar significant increase in the failure rate when the femoral tunnel position is moved from the ‘anatomical’ anteromedial position to the ‘anatomical’ center of the femoral footprint.
In response to the higher failure rate of ACL grafts placed centrally in the femoral footprint ACL anatomy and biomechanics has been revisited.
ACL fibers form an oblong femoral footprint that are organized such that the midsubstance of the ACL is narrower than the femoral footprint. Anatomic dissections have demonstrated that while the femoral footprint is oval, the direct fibers of the ACL forms a flat, ribbon like structure with a width of 9–16 mm and a thickness of only 2–4 mm as it takes off from the bone [29, 30].
Histologic analysis of the femoral footprint has provided further clarification of the relationship of the footprint with functional aspects of the native ACL. The femoral origin of the ACL has distinct direct and indirect insertions, which have been shown by histology and three-dimensional volume-rendered computed tomography [13, 22].
The direct insertion consists of dense collagen fibers anterior in the femoral footprint that connect to a bony depression immediately posterior to the lateral intercondylar ridge [10]. The indirect insertion consisted of more flimsy posterior collagen fibers that extend to blend into the articular cartilage of the posterior aspect of the lateral femoral condyle.
The dense collagen fibers of the direct insertion and the more membrane-like indirect insertion regions of the femoral footprint of the native ACL suggest that these regions may have different load sharing characteristics. Three recent biomechanical studies confirm this [14, 24, 26].
Kawaguchi and Amis [14] in an elegant ACL femoral origin sectioning study demonstrated that approximately 80% of the load during stability testing was taken up by the AM region of the direct insertion of the femoral footprint. Nawabi and Pearle [24] showed very similar results with the anterior region of the femoral footprint shares 80% of the load during stability testing and is more isometric during passive knee flexion than fibers in the posterior region of the footprint, which are adjacent to the posterior cartilage.
In a complimentary biomechanical study indirect fibers in the femoral footprint, were removed with only a minimal reduction in tibial translation and rotation during simulated pivot shift maneuvres confirming the direct ACL fibers primarily control translation and rotation [26].
Forty years ago, Artmann and Wirth [1] reported that a nearly isometric region for tunnel placement existed in the femur such that there is minimal elongation of the native anterior cruciate ligament during knee motion. The AM position (high in the footprint) identified by Hefzy et al. [12] demonstrates minimal change in length with 1–4 mm of length change through the range of motion.
In contrast, a central femoral tunnel would be expected to demonstrate 5–7 mm of length change while a lower graft (in the PL region of the footprint) demonstrates approximately 1 cm of length change through the range of motion [27].
In changing to the central femoral footprint position we found that the ACL graft was less isometric. It was common to have a negative Lachman, but a grade 1 anterior drawer at the completion of the procedure. This finding has been published by Lubowitz [18].
Thus, a non-isometric graft fixed in extension slackens during the flexion cycle and thus will not restrain anterior translation of the tibia or, if fixed in flexion will either capture the knee resulting in a fixed flexion deformity or excessive tension in extension will result in graft failure [3, 9, 20, 21].
As discussed earlier multiple cadaveric studies demonstrate superior time zero knee stability when the femoral tunnel is placed more centrally in the femoral footprint compared outside the footprint [2, 6, 7, 15,16,17, 23].
However, there is an emerging body of literature that demonstrates no significant difference in time zero stability between the AM femoral tunnel within the anatomic footprint (eccentrically located in the footprint) as compared to a centrally placed graft [5, 19].
In response to our higher failure rate and these recent anatomical and biomechanical studies the senior author has moved the femoral tunnel back to the AM position. He has continued to use a transportal technique. The transportal technique enables independent tibial tunnel drilling so the ACL graft can match the crescenteric tibial insertion of the native ACL and thus avoid the short oblique posterior tibial tunnel that is required to hit the femoral footprint with a trantibial technique.
In an ongoing study evaluating this change back to the AM femoral tunnel drilled transportally we have shown a reduction in our failure rate to a similar incidence to our transtibial group reported in this study. This indicates that the increased failure in the central footprint transportal group is due to tunnel placement rather than the transportal tunnel drilling surgical technique or a learning curve.
The primary limitation of this study is that all failures may not have captured. To capture patients with failures who presented to other surgeons all members of the New Zealand Knee Society were contacted to inform us of any failures. This study was performed prior to the introduction of our ACL registry.
The clinical relevance of this study is that it demonstrates that placement of the ACL graft in the AM position will result in a lower failure rate.
Central femoral tunnel ACLR placement results in an anisometric graft with high graft strain during extension, which is the likely explanation for the increased risk of revision. Femoral tunnel placement in the anteromedial bundle position is advantageous as it is the most isometric, placing the ACL graft in the direct fiber origin that takes up the most load during stability maneuvers.
Conclusion
Transportal central femoral footprint ACLR is associated with higher and earlier revision rate compared to AM femoral footprint transtibial ACLR.
References
Artmann M, Wirth CJ (1974) Investigation of the appropriate functional replacement of the anterior cruciate ligament (author’s transl). Z Orthop Ihre Grenzgeb 112:160–165
Bedi A, Musahl V, Steuber V, Kendoff D, Choi D, Allen AA et al (2011) Transtibial versus anteromedial portal reaming in anterior cruciate ligament reconstruction: an anatomic and biomechanical evaluation of surgical technique. Arthroscopy 27:380–390
Beynnon BD, Uh BS, Johnson RJ, Fleming BC, Renstrom PA, Nichols CE (2001) The elongation behavior of the anterior cruciate ligament graft in vivo. A long-term follow-up study. Am J Sports Med 29:161–166
Chu CR, Williams AA, West RV, Qian Y, Fu FH, Do BH et al (2014) Quantitative magnetic resonance imaging UTE-T2* mapping of cartilage and meniscus healing after anatomic anterior cruciate ligament reconstruction. Am J Sports Med 42:1847–1856
Cross MB, Musahl V, Bedi A, O’Loughlin P, Hammoud S, Suero E et al (2012) Anteromedial versus central single-bundle graft position: which anatomic graft position to choose? Knee Surg Sports Traumatol Arthrosc 20:1276–1281
Debandi A, Maeyama A, Lu S, Hume C, Asai S, Goto B et al (2011) Biomechanical comparison of three anatomic ACL reconstructions in a porcine model. Knee Surg Sports Traumatol Arthrosc 19:728–735
Driscoll MD, Isabell GP Jr, Conditt MA, Ismaily SK, Jupiter DC, Noble PC et al (2012) Comparison of 2 femoral tunnel locations in anatomic single-bundle anterior cruciate ligament reconstruction: a biomechanical study. Arthroscopy 28:1481–1489
Duffee A, Magnussen RA, Pedroza AD, Flanigan DC, Kaeding CC (2013) Transtibial ACL femoral tunnel preparation increases odds of repeat ipsilateral knee surgery. J Bone Joint Surg Am 95:2035–2042
Friederich N (1993) Knee joint function and the cruciate ligaments. Biomechanical principles for reconstruction and rehabilitation. Der Orthopäde 22(6):334–342
Fu FH, Jordan SS (2007) The lateral intercondylar ridge—a key to anatomic anterior cruciate ligament reconstruction. J Bone Joint Surg Am 89:2103–2104
Fu FH, van Eck CF, Tashman S, Irrgang JJ, Moreland MS (2015) Anatomic anterior cruciate ligament reconstruction: a changing paradigm. Knee Surg Sports Traumatol Arthrosc 23:640–648
Hefzy MS, Grood ES, Noyes FR (1989) Factors affecting the region of most isometric femoral attachments. Part II: the anterior cruciate ligament. Am J Sports Med 17:208–216
Iwahashi T, Shino K, Nakata K, Otsubo H, Suzuki T, Amano H et al (2010) Direct anterior cruciate ligament insertion to the femur assessed by histology and 3-dimensional volume-rendered computed tomography. Arthroscopy 26:S13–S20
Kawaguchi Y, Kondo E, Takeda R, Akita K, Yasuda K, Amis AA (2015) The role of fibers in the femoral attachment of the anterior cruciate ligament in resisting tibial displacement. Arthroscopy 31:435–444
Kondo E, Merican AM, Yasuda K, Amis AA (2011) Biomechanical comparison of anatomic double-bundle, anatomic single-bundle, and nonanatomic single-bundle anterior cruciate ligament reconstructions. Am J Sports Med 39:279–288
Lim HC, Yoon YC, Wang JH, Bae JH (2012) Anatomical versus non-anatomical single bundle anterior cruciate ligament reconstruction: a cadaveric study of comparison of knee stability. Clin Orthop Surg 4:249–255
Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL (2003) Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o’clock and 10 o’clock femoral tunnel placement. 2002 Richard O’Connor Award paper. Arthroscopy 19:297–304
Lubowitz JH (2014) Anatomic ACL reconstruction produces greater graft length change during knee range-of-motion than transtibial technique. Knee Surg Sports Traumatol Arthrosc 22:1190–1195
Markolf KL, Jackson SR, McAllister DR (2010) A comparison of 11 o’clock versus oblique femoral tunnels in the anterior cruciate ligament-reconstructed knee: knee kinematics during a simulated pivot test. Am J Sports Med 38:912–917
Markolf KL, Park S, Jackson SR, McAllister DR (2009) Anterior-posterior and rotatory stability of single and double-bundle anterior cruciate ligament reconstructions. J Bone Joint Surg Am 91:107–118
Markolf KL, Park S, Jackson SR, McAllister DR (2008) Contributions of the posterolateral bundle of the anterior cruciate ligament to anterior-posterior knee laxity and ligament forces. Arthroscopy 24:805–809
Mochizuki T, Fujishiro H, Nimura A, Mahakkanukrauh P, Yasuda K, Muneta T et al (2014) Anatomic and histologic analysis of the mid-substance and fan-like extension fibres of the anterior cruciate ligament during knee motion, with special reference to the femoral attachment. Knee Surg Sports Traumatol Arthrosc 22:336–344
Musahl V, Plakseychuk A, VanScyoc A, Sasaki T, Debski RE, McMahon PJ et al (2005) Varying femoral tunnels between the anatomical footprint and isometric positions: effect on kinematics of the anterior cruciate ligament-reconstructed knee. Am J Sports Med 33:712–718
Nawabi DH, Tucker S, Schafer KA, Zuiderbaan HA, Nguyen JT, Wickiewicz TL et al (2016) ACL fibers near the lateral intercondylar ridge are the most load bearing during stability examinations and isometric through passive flexion. Am J Sports Med 44:2563–2571
Okafor EC, Utturkar GM, Widmyer MR, Abebe ES, Collins AT, Taylor DC et al (2014) The effects of femoral graft placement on cartilage thickness after anterior cruciate ligament reconstruction. J Biomech 47:96–101
Pathare NP, Nicholas SJ, Colbrunn R, McHugh MP (2014) Kinematic analysis of the indirect femoral insertion of the anterior cruciate ligament: implications for anatomic femoral tunnel placement. Arthroscopy 30:1430–1438
Pearle AD, Shannon FJ, Granchi C, Wickiewicz TL, Warren RF (2008) Comparison of 3-dimensional obliquity and anisometric characteristics of anterior cruciate ligament graft positions using surgical navigation. Am J Sports Med 36:1534–1541
Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind MC (2013) Increased risk of revision after anteromedial compared with transtibial drilling of the femoral tunnel during primary anterior cruciate ligament reconstruction: results from the Danish Knee Ligament Reconstruction Register. Arthroscopy 29:98–105
Siebold R, Schuhmacher P, Fernandez F, Smigielski R, Fink C, Brehmer A et al (2014) Flat midsubstance of the anterior cruciate ligament with tibial “C"-shaped insertion site. Knee Surg Sports Traumatol Arthrosc 2015 Nov;23(11):3136–3142
Smigielski R, Zdanowicz U, Drwiega M, Ciszek B, Ciszkowska-Lyson B, Siebold R (2014) Ribbon like appearance of the midsubstance fibres of the anterior cruciate ligament close to its femoral insertion site: a cadaveric study including 111 knees. Knee Surg Sports Traumatol Arthrosc 23(11):3143–3150
Smigielski R, Zdanowicz U, Drwiega M, Ciszek B, Williams A (2016) The anatomy of the anterior cruciate ligament and its relevance to the technique of reconstruction. Bone Joint J 98-B:1020–1026
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Contributions
MC performed all the surgery and followed all the patients. He was involved in patient evaluation and statistical evaluation. He edited the final manuscript. He agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SS reviewed the results and statistical analysis and wrote the manuscript. TR collected all the revision’s from MC’s database. He reviewed patient clinical records on all 1480 patients to ensure the data was accurate and was involved in the statistical analysis.
Corresponding author
Ethics declarations
Conflict of Interest
Mark Clatworthy receives consulting fees from Johnson and Johnson and fellowship support from Johnson and Johnson and Athrex and royalties from Athrex Steffen Sauer and Tim Roberts have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Clatworthy, M., Sauer, S. & Roberts, T. Transportal central femoral tunnel placement has a significantly higher revision rate than transtibial AM femoral tunnel placement in hamstring ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 27, 124–129 (2019). https://doi.org/10.1007/s00167-018-5036-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5036-x