Abstract
Purpose
Infection complicating total knee arthroplasty (TKA) has serious implications. Traditionally the debate on whether one- or two-stage exchange arthroplasty is the optimum management of infected TKA has favoured two-stage procedures; however, a paradigm shift in opinion is emerging. This study aimed to establish whether current evidence supports one-stage revision for managing infected TKA based on reinfection rates and functional outcomes post-surgery.
Methods
MEDLINE/PubMed and CENTRAL databases were reviewed for studies that compared one- and two-stage exchange arthroplasty TKA in more than ten patients with a minimum 2-year follow-up.
Results
From an initial sample of 796, five cohort studies with a total of 231 patients (46 single-stage/185 two-stage; median patient age 66 years, range 61–71 years) met inclusion criteria. Overall, there were no significant differences in risk of reinfection following one- or two-stage exchange arthroplasty (OR −0.06, 95 % confidence interval −0.13, 0.01). Subgroup analysis revealed that in studies published since 2000, one-stage procedures have a significantly lower reinfection rate. One study investigated functional outcomes and reported that one-stage surgery was associated with superior functional outcomes. Scarcity of data, inconsistent study designs, surgical technique and antibiotic regime disparities limit recommendations that can be made.
Conclusion
Recent studies suggest one-stage exchange arthroplasty may provide superior outcomes, including lower reinfection rates and superior function, in select patients. Clinically, for some patients, one-stage exchange arthroplasty may represent optimum treatment; however, patient selection criteria and key components of surgical and post-operative anti-microbial management remain to be defined.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infection of total knee arthroplasty (TKA) is a recognised and devastating complication of the procedure, with an incidence of between 0.5 and 2.5 % in patients with osteoarthritis [3, 15], and significantly higher in patients with rheumatoid arthritis, history of previous joint surgery and a higher Charlson comorbidity index [6, 18]. There has been wide debate as to the most appropriate management protocol of infected TKA.
There are currently three conventional treatment options for infected TKA: Débridement, antibiotics and implant retention (DAIR), one-stage exchange arthroplasty and two-stage exchange arthroplasty surgery.
DAIR has a limited role. It is typically indicated in patients presenting with acute infection and well-fixed prostheses; however, outcomes are highly variable (ranging from 14 to 100 % of patients with infection free survival) dependent on appropriateness of patient selection [5, 27]. Often, definitive treatment remains to be surgical, with exchange arthroplasty of prostheses in a one-stage or two-staged fashion [13].
Two-stage exchange arthroplasty surgery refers to the removal of infected prostheses, débridement of surrounding tissues, addition of an antibiotic delivery device and a subsequent period of systemic antibiotic treatment followed by reimplantation, rather than exchange of prosthesis within the same procedure as in one-stage exchange arthroplasty [11].
The aim of this systematic review was to establish whether there is a difference in (1) reinfection rates or (2) functional outcomes, when comparing one- and two-stage exchange arthroplasty surgery for infected TKA. This study will summarise and critically appraise the evidence for the management of the patient with an infected TKA and investigate whether temporal changes in surgical management have influenced outcomes in this patient group.
Materials and methods
Search strategy and criteria
A study protocol was developed and registered on the open-access database of systematic reviews, PROSPERO [19]. A complete literature search of the MEDLINE/PubMed database and CENTRAL/Cochrane Library was undertaken between August 2014 and January 2015 using the search string ‘Infect* AND (“total knee replace*” OR “total knee arthroplast*”) AND revis*’.
The study protocol was designed with the inference that one-stage procedures were less numerous in frequency, and also in the number of institutions where this procedure was performed. Therefore, in accordance with previously published peer-reviewed systematic reviews, cohort studies were included in the analysis (prospective and retrospective), despite their propensity to bias [9, 16].
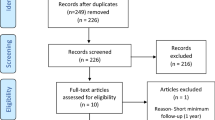
The inclusion criteria applied to studies were: an n value (number of patients in the study) ≥ten, a minimum two year follow-up and two-arm, comparative studies. Strict exclusion criteria were also applied, with any exchange arthroplasty studies involving generic lower limb arthroplasty, inadequate detail of study methodology and non-English language papers omitted. Studies satisfying inclusion and exclusion criteria were independently reviewed by all authors. The search process to determine which studies were selected is detailed as a flow diagram (Fig. 1).
The primary outcome measure of interest was incidence of reinfection, and the secondary outcome measure was functional outcome.
Five papers were found to adequately match our strict criteria for review with full agreement of all authors. All five original papers studied reinfection rates (Table 1), of which one paper followed functional outcomes after procedures quantified by Knee Society Scores (KSS) [10].
A total of 231 patients (46 one-stage and 185 two-stage surgeries) were included in this systematic review to compare and determine reinfection trends, as defined by each study’s own criteria (Table 1).
Certain studies [28] defined débridement and retention of prostheses as a one-stage exchange arthroplasty; however, as this technique is associated with variable outcomes, particularly in chronic infections, the data were excluded from analysis and the definition of a one-stage exchange arthroplasty was limited to ‘débridement of infected tissues with removal and replacement of prostheses’.
Analysis of data
Bias within studies was quantified using ‘Preferred Reporting Items for Systematic reviews and Meta-Analyses’ (PRISMA) guidelines, and methods used within studies were critically appraised using the Methodological Index for Non-Randomised Studies (MINORS) score, a tool to determine the calibre of the methods used within a non-randomised study [26].
For the primary outcome of risk of reinfection, the odds ratio (OR) was calculated. Heterogeneity of included studies was examined using the I 2 statistic, and as a degree of variability is expected among eligible studies, a random-effects model was used. The pooled OR and 95 % confidence intervals (CI) were estimated using the Mantel–Haenszel method. Subgroup analysis was performed by year of publication to investigate longitudinal changes in surgical practice. Two subgroups based on those studies published prior to the year 2000 and those studies published after this, were investigated. All analyses were performed and figures produced using Review Manager 5.3.3 (The Cochrane Collaboration, Oxford, UK).
Outcomes of search
Five studies were included within the systematic review (Table 1) [4, 8, 14, 18, 25]. All included studies were non-randomised, single-centre, retrospective cohort studies. One- and two-stage groups were matched for age (65.9 years, range 61–71 years) and time to follow-up (61.3 months, range 25–159 months). The infecting organisms were reported in 198 knees and are outlined in Table 2. The quality of studies as determined by the MINORS score was low (mean 17.6, range 14–20), falling short of minimum value of 24 for a comparative study [26].
Inclusion criteria and the indications for two-stage, compared with one-stage, procedures were poorly reported. One study excluded complex cases, including infections with psoriatic skin involvement, draining sinuses or resistant organisms [4], and three studies reported the indications for two-stage procedures [4, 8, 18] (Table 3).
Wide variations in surgical techniques, within and between, studies of both the one- and two-stage exchange arthroplasty surgeries were noted. One-stage exchange arthroplasty procedures varied according to the extent of débridement, type of antibiotic (broad-spectrum or organism specific) and use of intraoperative techniques, which can help reduce the rate of reinfection including the use of hydrogen peroxide and Betadine solutions [8].
Two-stage exchange arthroplasty procedures varied with respect to time between first and second stages (3–20 weeks), the duration and route of administration (intravenous versus oral) of antibiotics between procedures and requirement for negative cultures prior to reimplantation [4, 25].
All two-stage procedures utilised antibiotic cement when implanting the new prosthesis, as would be expected. A range of concentrations of antibiotic was impregnated into the cement mixtures, from 1 g antibiotic in 80 g cement to 1.2 g in 40 g cement. There were no references made to evidence base for these concentrations. Post-reimplantation patients received a mean of 4.6 weeks of IV antibiotics with additional oral follow-on therapy, compared to a mean of 4.1 weeks of IV antibiotics following one-stage procedures [8, 14].
Results
Cumulative reinfection rates for one-stage exchange arthroplasty procedures were 4.3 % (two of 46 cases) and for two-stage procedures were 13.5 % (25 of 185 cases). No single study self-reported any statistical significance to favour one type of exchange arthroplasty surgery over another. When pooling the number of reinfections to calculate an overall OR, the comparative studies produced an OR of −0.06 (95 % CI −0.13 to 0.01), suggesting no significant difference in risk of reinfection between one- and two-stage procedures. Subgroup analysis based on year of publication demonstrated that in papers published prior to 2000 no significant difference in reinfection rates is detected between one- and two-stage exchange arthroplasty (OR 0.08; 95 % CI −0.20 to 0.36); however, studies published since 2000 demonstrate significantly lower reinfection rates in one-stage exchange arthroplasty (OR −0.08; 95 % CI −0.20 to 0.00). A summary of the findings from different studies, with ORs extrapolated from data within papers, calculated by our group, is shown in Fig. 2.
Summary of findings from studied papers, with extrapolated odds ratios and 95 % CI, extrapolated from data within papers. Two subgroups based on those studies published prior to the year 2000 and those studies published after this, were investigated. All analyses were performed and figures produced using Review Manager 5.3.3
One study by Haddad et al. [8] was deemed suitable for studying functional outcomes as it determined patient’s pre-operative function, assessed using the Knee Society Score (KSS), in addition to their post-operative status. This study found a statistically significant difference in improvement of functional scores, favouring the one-stage procedure. The mean increase in KSS scores was +56 for one-stage and +45 for two-stage, which takes into account a patient’s anatomical stability post-operatively, but also their self-reported functional status, including pain levels [10].
Discussion
The most important finding of this study is that no significant difference in reinfection rates was detected between knees treated with one- or two-stage exchange arthroplasty procedures across the published literature. Furthermore, subgroup analysis of studies published since 2000 demonstrates that with appropriate patient selection and surgical technique, one-stage exchange arthroplasty procedures are associated with lower reinfection rates and may be associated with superior functional outcomes.
This systematic review found no statistical difference in rates of reinfection following one- and two-stage exchange arthroplasty for infected TKA (−0.06, 95 % CI −0.13 to 0.01). Reinfection was defined by clinical, biochemical, radiological or a combination of these criteria [8], although the majority of studies did not describe the criteria for reinfection fully.
Interestingly, subgroup analysis revealed that while older studies, prior to the year 2000, find no difference in reinfection rates between one- and two-stage exchange arthroplasty, recent studies shift support away from two-stage procedures and provide evidence of superiority of one-stage exchange arthroplasty. The reasons for this shift are unclear and will be multi-factorial with improved patient selection, surgical technique and antibiotic protocols likely all having a role. These results hold promise as the limited evidence suggests that one-stage surgery has significantly better functional outcomes and is more cost-effective than a two-stage technique [8].
While there has been a significant quantity of literature exploring the different techniques and attempting to compare and contrast these, there are few long-term follow-up, high power studies explicitly endorsing the use of one method. Previous reviews on this subject have summarised single-arm studies, separately investigating one- and two-stage exchange arthroplasty or have only provided a descriptive summary [7, 12, 23]. As part of our study, two review studies were separately analysed, which combined data from papers reporting on either one- or two-stage exchange arthroplasty in isolation. Jamsen et al. [12] and Romano et al. [23] looked specifically at papers with a minimum follow-up of 12 months and minimum n value of five per study.
Jamsen et al. studied 926 two-stage and 152 one-stage procedures and the number of recurrent or new infections after surgery. Two-stage procedures were noted to have lower reinfection rates, but this was not significant. Romano et al. [23] stated that mobile spacers were also associated with significantly lower reinfection outcomes, and again, although there was a higher percentage of reinfection amongst one-stage procedures (18.1 % of 204) versus two-stage (10.2 % of 1421 procedures), this did not reach significance.
These studies support our conclusions of non-statistical, but descriptive differences in reinfection outcomes of one- and two-stage exchange arthroplasty surgery for TKA. The two reviews had 41.5 % reviews in common between them and in addition to studying similar material, the reviews had similar weaknesses, whereby they performed an overview of heterogeneous studies and methods and were limited to a descriptive review only.
Similar to the Jamsen and Romano studies, the limitations of this systematic review lie within the evidence studied. Although a large body of evidence was reviewed, the studies remain inconsistent with regards to sample size, operative techniques, length of time of follow-up and indeed conclusion of recommendations.
Due to the absence of RCTs, patients either had one type of surgery or another dependent on surgeon’s preference and/or hospital protocol. This introduced an inherent patient selection bias whereby certain patients are selected for a specific procedure dependent on surgeon’s preference or hospital protocol, removing any randomisation from the operative technique used.
Overall, when comparing one and two-stage exchange arthroplasty surgery, the evidence base is weighed down by older studies. We can demonstrate this by taking the arbitrary time-point of the turn of the twenty-first century: two comparative studies meeting our inclusion criteria written before the year 2000 reported no significant difference in reinfection rates between procedures [4, 25]; beyond this date, however, three studies produced a mean OR of −0.08, significantly favouring one-stage exchange arthroplasty [8, 14, 18].
Upon further scrutiny, it appears that this discrepancy of worse outcomes in two-stage exchange arthroplasty may be explained in part by operative technique and patient selection. Haddad et al. [21] classified infection with resistant organisms (MRSA and MRSE) and polymicrobial infections as contraindications for one-stage surgery; moreover, a strict rescrubbing procedure was described intraoperatively within the one-stage procedure, which has been shown to be highly efficacious in lowering reinfection rates. The length of course of antibiotics was also found to be of considerable length in papers where the one-stage procedure had superior outcomes, averaging 3.2 weeks of IV treatment followed by an unspecified length of oral antibiotic treatment, of a minimum of 6 months in the paper by Laffer et al. [14]. This suggests that pre-selection of patients can help to shape favourable outcomes for the one-stage procedure.
The conclusion of one-stage surgery having greater functional outcomes is fragile, as only one study was deemed adequate in reaching a conclusion on this matter. This is because most studies in this field are retrospective case series, and so there is limited data available on pre-surgical functional morbidity, as one would be expected to determine were a trial to be prospectively designed for comparison to post-surgical scores.
Some studies have reported no difference between the one- and two-stage technique and PROMs [1]; however, the general consensus of literature tends to support one-stage procedures with regards to functional outcomes, citing greater ROM, decreased stiffness and limited anatomical deterioration compared to a two-stage procedures [2].
Future directions
There is an increasing vogue to establish a protocol, which could be applied to all patients with different forms of prosthetic joint infection, taking into account patient co-morbidity, chronicity of infection, radiographical changes/stability of implant and appreciation of the infective organism (and therefore its resistance) [17, 24, 29, 30], as described in Fig. 3. This stems from data showing that acute and superficial infections with a stable implant respond well to one-stage intervention or indeed simple débridement and retention of the original prosthesis with concomitant antibiotic therapy [8]. Furthermore, recent international efforts (International Consensus meeting on peri-prosthetic joint infection) have intimated specific conditions where two-stage exchange may be indicated over one-stage exchange, which include (1) patients with systemic manifestations of infection (sepsis); (2) the scenario where infection appears obvious but no organism has been identified; (3) pre-operative cultures identifying difficult to treat and antibiotic-resistant organisms; (4) presence of a sinus tract and (5) inadequate and non-viable soft tissue coverage [22].
Protocol for diagnosis and subsequent management of infected TKA. This figure was published in Int. J. Infect. Dis., Volume 14, Gruppo Italiano di Studio sulle Infezioni Gravi Group, Consensus document on controversial issues in the diagnosis and treatment of prosthetic joint infections, S67–77, Copyright Elsevier 2010 [17]
Having said this, approaches will continue to be explored, to aim for a ‘magic bullet’ to the problem of infected TKA, such as the two-in-one approach described originally by Parkinson et al. [21] where a two-stage procedure is undertaken in one operation. These novel approaches require a shorter average length of stay in hospital and along with DAIR and one-stage surgery can generate substantial financial savings for healthcare systems [20].
In the long term, a multi-centre prospective RCT could be employed. Such a study would implement a management protocol into several centres and assess reinfection and functional outcomes (taking into account pre-intervention state) compared to centres where this protocol was not in place. It is important to appreciate the difference in patient populations and take account of these. This trial could establish selection criteria of patients for either one- and two-stage exchange arthroplasty and ultimately improve outcomes of patients with infected TKA.
This study presents evidence that in appropriate patient groups one-stage exchange arthroplasty may be associated with lower rates of reinfection with the potential for superior functional outcomes. This study challenges the assumption that two-stage exchange arthroplasty procedures represent the gold standard of care in all patients and therefore encourages clinicians to consider one-stage exchange arthroplasty when they encounter infected TKA. The indications for a single-stage procedure remain to be defined, as do the critical steps in the surgical and post-operative management. However, this study demonstrates that recent improvements in our management of patients with this devastating complication are translating into improved clinical outcomes.
Conclusion
No difference in reinfection rates was detected between one- and two-stage exchange arthroplasty procedures in the management of infected TKA. Subgroup analysis of studies published since 2000 demonstrated lower infection rates following one-stage procedures with limited evidence that one-stage procedures are associated with superior functional outcomes. This study presents evidence that with improved patient selection and surgical management, one-stage procedures may have significant patient benefits in select patient cohorts.
References
Baker P, Petheram TG, Kurtz S, Konttinen YT, Gregg P, Deehan D (2013) Patient reported outcome measures after revision of the infected TKR: comparison of single versus two-stage revision. Knee Surg Sports Traumatol Arthrosc 21:2713–2720
Bauer T, Piriou P, Lhotellier L, Leclerc P, Mamoudy P, Lortat-Jacob A (2006) Results of reimplantation for infected total knee arthroplasty: 107 cases. Rev Chir Orthop Reparatrice Appar Mot 92:692–700
Blom A, Brown J (2004) Infection after total knee arthroplasty. J Bone Joint Surg 12:433–439
Borden LS, Gearen PF (1987) Infected total knee arthroplasty: a protocol for management. J Arthroplasty 2:27–36
Byren I, Bejon P, Atkins BL, Angus B, Masters S, McLardy-Smith P, Gundle R, Berendt A (2009) One hundred and twelve infected arthroplasties treated with “DAIR” (debridement, antibiotics and implant retention): antibiotic duration and outcome. J Antimicrob Chemother 63:1264–1271
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Clement ND, Burnett RBS (2013) Should single- or two-stage revision surgery be used for the management of an infected total knee replacement? A critical review of the literature. OA Orthop 1:2
Haddad FS, Sukeik M, Alazzawi S (2014) Is single-stage revision according to a strict protocol effective in treatment of chronic knee arthroplasty infections? Clin Orthop Relat Res 473:8–14
Higgins JP, Green S (eds) (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0. Cochrane Collaboration. http://www.cochranehandbook.org
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the knee society clinical rating system. Clin Orthop Relat Res 248:13–14
Insall JN, Thompson FM, Brause BD (1983) Two-stage reimplantation for the salvage of infected total knee arthroplasty. J Bone Joint Surg Am 65:1087–1098
Jämsen E, Stogiannidis I, Malmivaara A, Pajamäki J, Puolakka T, Konttinen YT (2009) Outcome of prosthesis exchange for infected knee arthroplasty: the effect of treatment approach. Acta Orthop 80:67–77
Kuiper JW, Willink RT, Moojen DJF, van den Bekerom MP, Colen S (2014) Treatment of acute periprosthetic infections with prosthesis retention: review of current concepts. World J Orthop 5:667–676
Laffer RR, Graber P, Ochsner PE, Zimmerli W (2006) Outcome of prosthetic knee-associated infection: evaluation of 40 consecutive episodes at a single centre. Clin Microbiol Infect 12:433–439
Lentino JR (2003) Prosthetic joint infections: bane of orthopedists, challenge for infectious disease specialists. Clin Infect Dis 36:1157–1161
Leonard HAC, Liddle AD, Burke O, Murray DW, Pandit H (2014) Single- or two-stage revision for infected total hip arthroplasty? A systematic review of the literature. Clin Orthop Relat Res 472:1036–1042
Leone S, Borrè S, Monforte AA, Mordente G, Petrosillo N, Signore A, Venditti M, Viale P, Nicastri E, Lauria FN, Carosi G, Moroni M, Ippolito G, the GISIG (Gruppo Italiano di Studio sulle Infezioni Gravi) Working Group on Prosthetic Joint Infections (2010) Consensus document on controversial issues in the diagnosis and treatment of prosthetic joint infections. Int J Infect Dis 14(Suppl 4):67–77
Mortazavi SMJ, Schwartzenberger J, Austin MS, Purtill JJ, Parvizi J (2010) Revision total knee arthroplasty infection: incidence and predictors. Clin Orthop Relat Res 468:2052–2059
Nagra NS, Hamilton TW, Ganatra S, Murray DW, Pandit H (2014) PROSPERO international prospective register of systematic reviews CRD42014013351
Oduwole KO, Molony DC, Walls RJ, Bashir SP, Mulhall KJ (2010) Increasing financial burden of revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 18:945–948
Parkinson RW, Kay PR, Rawal A (2011) A case for one-stage revision in infected total knee arthroplasty? Knee 18:1–4
Parvizi J, Gehrke T, Chen AF (2013) Proceedings of the international consensus on periprosthetic joint infection. Bone Joint J 95-B:1450–1452
Romanò CL, Gala L, Logoluso N, Romanò D, Drago L (2012) Two-stage revision of septic knee prosthesis with articulating knee spacers yields better infection eradication rate than one-stage or two-stage revision with static spacers. Knee Surg Sports Traumatol Arthrosc 20:2445–2453
Savarino L, Tigani D, Baldini N, Bochicchio V, Giunti A (2009) Pre-operative diagnosis of infection in total knee arthroplasty: an algorithm. Knee Surg Sports Traumatol Arthrosc 17:667–675
Scott IR, Stockley I, Getty CJ (1993) Exchange arthroplasty for infected knee replacements. A new two-stage method. J Bone Joint Surg Br 75:28–31
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (Minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Vasso M, Schiavone Panni A (2015) Low-grade periprosthetic knee infection: diagnosis and management. J Orthop Traumatol 16:1–7
Wolff LH, Parvizi J, Trousdale RT, Pagnano MW, Osmon DR, Hanssen AD, Haidukewych GJ (2003) Results of treatment of infection in both knees after bilateral total knee arthroplasty. J Bone Joint Surg Am 85-A:1952–1955
Zimmerli W (2006) Infection and musculoskeletal conditions: prosthetic-joint-associated infections. Best Pract Res Clin Rheumatol 20:1045–1063
Zimmerli W, Ochsner PE (2003) Management of infection associated with prosthetic joints. Infection 31:99–108
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. All work was performed at the Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), University of Oxford, Botnar Research Centre, Windmill Road, Oxford OX3 7LD, UK.
Rights and permissions
About this article
Cite this article
Nagra, N.S., Hamilton, T.W., Ganatra, S. et al. One-stage versus two-stage exchange arthroplasty for infected total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 24, 3106–3114 (2016). https://doi.org/10.1007/s00167-015-3780-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3780-8