Abstract
Purpose
The best method for treating chronic periprosthetic knee infection remains controversial. Randomized, comparative studies on treatment modalities are lacking. This systematic review of the literature compares the infection eradication rate after two-stage versus one-stage revision and static versus articulating spacers in two-stage procedures.
Methods
We reviewed full-text papers and those with an abstract in English published from 1966 through 2011 that reported the success rate of infection eradication after one-stage or two-stage revision with two different types of spacers.
Results
In all, 6 original articles reporting the results after one-stage knee exchange arthoplasty (n = 204) and 38 papers reporting on two-stage revision (n = 1,421) were reviewed. The average success rate in the eradication of infection was 89.8% after a two-stage revision and 81.9% after a one-stage procedure at a mean follow-up of 44.7 and 40.7 months, respectively. The average infection eradication rate after a two-stage procedure was slightly, although significantly, higher when an articulating spacer rather than a static spacer was used (91.2 versus 87%).
Conclusions
The methodological limitations of this study and the heterogeneous material in the studies reviewed notwithstanding, this systematic review shows that, on average, a two-stage procedure is associated with a higher rate of eradication of infection than one-stage revision for septic knee prosthesis and that articulating spacers are associated with a lower recurrence of infection than static spacers at a comparable mean duration of follow-up.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to a recent epidemiological study of revision total knee arthroplasty in the United States, periprosthetic knee infection is the first reason for revision and is associated with a huge economic burden [5]. However, the best method for treating this challenging complication remains controversial. To date, no prospective study on the treatment of delayed and late or chronic infections has directly compared two-stage versus one-stage revision or the use of static versus articulating knee spacers in two-stage procedures.
In the 1990s, impregnated antibiotic cement spacer blocks came into use to maintain joint space and stability, prevent collateral ligament retraction, and provide local antibiotic release [4, 7, 64]. Complete rest between stages was also considered helpful for soft tissue healing. Later, articulating spacers were introduced to overcome the disadvantages of block spacers. This new option was developed to facilitate exposure at reimplantation, preserve knee function and prevent interim bone loss [7] between stages, and ultimately enhance functional outcome. Various different types of articulating spacers are employed: re-sterilized prosthetic components or new components (spacer prostheses) [28, 29, 52]; cement spacers molded during the operation with a thin metal-on-polyethylene runner [14, 15, 41–43, 45]; all-cement spacers molded [36, 53] or custom-made [48, 61, 62] during the operation; and, more recently, preformed antibiotic-loaded cement spacers [46, 50, 60].
In the ensuing two decades, numerous studies showed that the interim use of an articulating antibiotic-impregnated spacer provides high infection eradication rates, coupled with acceptable function between stages, thus minimizing bone loss and improving patient function and satisfaction. But other centers reported favorable results also after a one-stage approach [6, 17]. A recent systematic review of the literature published as of January 2009 failed to show a difference in the infection eradication rate of one- versus two-stage procedures [34]; importantly, however, the review did not examine whether different types of interim spacers could be associated with different outcomes in infection control.
Prospective, randomized controlled comparative trials between one- and two-stage procedures or between the use of different types of spacer are lacking, and the results from case series are controversial. Currently, the apparently only way to compare outcomes after treatment is by systematic review of the available data.
With this study, we attempted to verify the hypothesis that different surgical treatment modalities afford a better chance of infection control. To do this, we conducted a systematic review of the literature updates and compared the eradication rates of infection after one- and two-stage procedures with static and articulating interim spacers in the treatment of delayed, late, and chronic periprosthetic knee infection.
Materials and methods
We reviewed papers with a full text or an abstract in English, published from 1966 through July 2011, which reported the success rate of eradication of periprosthetic knee infection after one-stage or two-stage revision in which two different types of spacers were used. The international databases were searched as described by Jämsen and co-workers [34] and included: EMBASE; PubMed/Medline; Medline Daily Update; Medline In-Process and other non-indexed citations; Google Scholar; SCOPUS; CINAHL; Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews; NHS Health Technology Assessment; http://www.google.com; and http://www.yahoo.com.
The following keywords were entered either alone or in different combinations: knee, infection; arthroplasty; prosthesis; total knee replacement; TKR; prosthetic knee infection; one-stage revision; and two-stage revision.
The inclusion criteria were the following:
-
(a)
Papers written fully or with an abstract in English;
-
(b)
Papers reporting the results of management of infected knee arthroplasty with one-stage or two-stage exchange arthroplasty;
-
(c)
Study design classifiable as: randomized controlled trial; comparative prospective study; prospective study with historical controls; prospective case series with no comparison group; comparative retrospective study; retrospective study with historical control group; retrospective study with no control group;
-
(d)
If more than one paper by the same author(s) was retrieved, only the most recent reference with the longest follow-up and largest patient series was included;
-
(e)
The study population had to be 5 or more cases treated with a minimum follow-up of 1 year;
-
(f)
At least all of the following variables had to be reported: number of patients treated; type of treatment; number of recurrent infections after treatment.
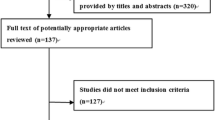
Figure 1 illustrates the flow chart for inclusion of papers in the review.
Study quality was assessed against a checklist informed by previously published criteria [34, 40, 59] of studies in systematic reviews and adapted for the purposes of this review:
-
(a)
Description of the patient population (patient age and sex, indications for primary knee replacement, host type, and isolated pathogens);
-
(b)
Description of the treatment (indication for type of treatment, length of antibiotic therapy, spacer type, duration of interim period between stages, and type of implants used at revision);
-
(c)
Outcomes reported (number of all posttreatment infections, number of reinfections, and number of patients lost to follow-up).
The quality score was calculated as a percentage of the above-mentioned items the reviewed study included; however, the quality score was not used as an exclusion criterion.
Two investigators, LD and DR, independently searched and reviewed the literature and classified the references in terms of whether they should be included on the basis of the paper’s title and abstract. Original study reports as well as review articles were retrieved, and the reference lists from all reviewed articles were assessed to complete the literature search. If the same material was presented in more than one study, only the most recent one was taken. At the end of the review process, the two reviewers’ lists of papers were compared and discrepancies were solved by reclassification as mutually agreed.
Within the limitations posed by the heterogeneity of the studies and the low-quality scores, the raw number of infection eradication rates were reported, together with the calculated percentage and the average of the different treatment modalities with respective follow-up periods.
Statistical analysis
Statistical analysis was performed using the two-tailed Chi-square test with the Yates correction for categorical data (http://faculty.vassar.edu/lowry/odds2x2.html).
Results
In all, 6 original articles on one-stage knee exchange arthoplasties (n = 204) and 38 papers on two-stage revisions (n = 1,421) were reviewed (Tables 1, 2). The range in the number of cases was between 5 and 124, and the range in the duration of follow-up was from 12 to 108 months.
The database search retrieved no randomized, controlled trials. The majority of the papers described retrospective case series without a control group (Level of evidence: IV) and most gave an incomplete description of the study material. The percentage of reported items was 59.3% on average (Table 3). In addition, no detailed description was given of the criteria for selecting one- or two-stage revision or for implanting static or articulating spacers. Similarly, other relevant variables such as the relative proportion of compromised hosts or multiresistant pathogens were only occasionally reported.
The infection eradication rate after a one-stage procedure ranged from 73.1% in the largest patient series to 100% in a retrospective case series of only 8 knees (Table 1). The eradication rate after a two-stage revision ranged from 69.2% in a series of 13 cases to 100% in 9 studies, for a total of 150 patients. At a mean follow-up of 44.7 ± 25.5 months, the calculated average success rate in the eradication of infection was 89.8% after two-stage revision (including all types of spacers) as compared to 81.9% (95% confidence interval [CI] 0.51, 0.34–0.77; P = 0.0001) after one-stage revision, at a mean follow-up of 40.7 ± 24.4 months. The average infection eradication rate after a two-stage procedure was higher with the use of an articulating spacer (91.2% at 43.3 ± 27.7 months follow-up) than with a static spacer (87% at 43.5 ± 20.1 months) (95% CI 0.64, 0.44 to 0.93; P = 0.02) (Tables 4, 5).
Discussion
The most important finding of this study is that the rate of infection eradication is higher after a two stage than after a one-stage procedure for chronic knee periprosthetic infection and that the rate of infection recurrence is lower in patients treated with articulating spacers than in those who received a static spacer. Furthermore, we found that two-stage procedures are routinely performed in the vast majority of orthopedic centers around the world and that far more cases are reported of patients undergoing a two-stage procedure.
Moreover, this review provides evidence supporting the use of two-stage delayed reimplantation as the gold standard in periprosthetic knee infections. The statistical analysis shows, for the first time to our knowledge, a significantly higher eradication rate after two stage over one-stage procedures.
This is also the first review to evidence a small but statistically significant eradication rate associated with the use of articulating versus static spacers. As such, it updates the results from a study by Lombardi and co-workers [36], which failed to show a clear difference between the two methods.
Block spacers were devised to relieve knee pain from instability, maintain joint space, and safely elute high concentrations of antibiotics. Advocates of static spacers also claimed placing the wound at rest as a basic tenet of infection treatment. Accordingly, static spacers were developed and implemented with excellent published results for many years and remain in wide use today. Despite these purported advantages, their use was soon found to be coincident with impaired function between stages due to knee movement restriction and the frequent need of a cast or brace immobilization, quadriceps and collateral ligament shortening and arthrofibrosis, and difficult surgical exposure in the second-stage procedure. Tibial bone loss was also reported to occur after placement of static spacers in nearly half of the cases, with bone defect directly related to the length of the interim period [7].
Articulating spacers were introduced to overcome the drawbacks to block spacers and to facilitate reimplantation surgery. Like static spacers, mobile spacers preserve joint space and elute high antibiotic concentrations [35, 46], coupled with the added advantages of: greater postoperative range of motion; improved patient comfort during the interim period and easier reimplantation owing to minimal tibial and femoral bone loss; reduced incidence of quadriceps shortening and arthrofibrosis; and improved soft tissue health.
These claimed advantages aside, the current debate revolves around whether static or articulating spacers are the better treatment method. Typically, because studies involve a small patient sample, with a short follow-up period and limited outcome measures, there is scant evidence that the use of interim articulating spacers could be associated with better long-term function [12, 14, 15]. In addition, the reports are often unclear about differences in the rate of infection eradication between static and articulating spacers.
Given the quality and the heterogeneous material of the reviewed studies, the data presented here should be interpreted with caution. The possible bias and limitations of this study are the following:
-
Patient selection and treatment indications. Eligibility for one-stage or two-stage procedures may differ across different centers, as does patient selection for the implant of an articulating or a static spacer. The criteria for electing the type of treatment were not clearly stated in the studies, suggesting that the choice largely relies, at least in continuous case series, on a school-based routine rather than on case-by-case evaluation. Patient selection may not only bias the result of systematic reviews, but it can also strongly limit the feasibility of controlled randomized trials. The relatively low prevalence of the disease and the high number of preoperative variables (patient age and sex, local and general co-morbidities, previous surgeries, pathogen type, implant type, etc.) may, in fact, well explain the lack of published randomized prospective studies. Presently, the only possible way to reduce the selection bias of systematic reviews seems to be to include larger case series from different centers. Comparison of results would be easier if future clinical studies included at least the criteria for electing a one- or a two-stage procedure or for using a static or an articulating spacer;
-
Postoperative treatment varies widely across studies, which may influence the relative eradication rate of infection, particularly with regard to the use of antibiotics [2, 9, 10, 27] and their duration [24, 30];
-
This review did not investigate the relative effect the many variables may have on outcome after joint revision surgery (e.g., co-morbidities, age, body-mass index, type of implant, use of cement at revision, interval between the first and the second procedure, etc.);
-
Quality of life and the costs of one-stage versus two-stage procedures were not addressed in this analysis;
-
Articulating spacers were all grouped as one procedure; however, at least five different types of articulating spacers were reported: re-sterilized prosthetic components or new components (spacer prostheses); cement spacer molded during the operation with a metal-on-polyethylene runner; all-cement spacer molded or custom-made during the operation; and preformed antibiotic-loaded cement spacers. Case series treated according to each spacer type would be too small to allow a comparative analysis of the results;
-
Due to the differences in the “Materials and methods” across the studies, in this review, we restricted our evaluation of the outcomes to the reported infection eradication rate. This limits the ability to catch differences in functional outcome or quality of life or costs related to a given surgical option. Furthermore, when analyzing the data, we did not distinguish between recurrent and new infections because this distinction was not made in most of the papers and because the criteria for differentiating between recurrent and new infections are weakly supported in the literature and somewhat artificial. The conventional definition of a new infection as an event in which a newly isolated microorganism is found, as opposed to the detection of the same pathogen in so-called recurrent infection does not seem, in our opinion, a reliable one, the results of cultural examination in periprosthetic infection being too unpredictable, especially after previous antibiotic treatments [57];
-
Comparison of percentages instead of raw numbers may be confounding and should be regarded with caution. Jämsen and co-workers compared percentages and reported fairly similar infection eradication rates after one-stage (73–100%) and two-stage (82–100%) revisions of infected knee prosthesis [34]; however, if the average raw numbers of their study are compared, two-stage procedures performed clearly better than one-stage revision (94.8 versus 80.8%), which is very similar to what we observed in our analysis, where all calculations for statistical analysis were done on the raw numbers, although percentages are also shown;
-
Another limitation of this review is the inclusion of only papers published in English.
In conclusion, this systematic review of the reported infection eradication rates of different treatment modalities for septic knee prosthesis showed, on average, a better result after two-stage procedures than after one-stage revision and with the use of articulating versus static spacers. Nonetheless, the limitations and bias of the current literature point to the need for prospective, randomized studies to establish the superiority of one type of surgical treatment over another. That said, certain circumstantial limitations (low incidence of the disease, relatively small patient cohorts, need for long-term follow-up, differences in patient characteristics and microorganisms, etc.) would also make a controlled prospective study in this field extremely challenging. For the surgeon, the expectation that the risk of infection associated with treatment can be minimized is a key factor in deciding how to treat an implant-related infection. For the patient, the final choice will depend on parameters not addressed in this review, including preoperative clinical status, possible benefits in function and quality of life to be gained from treatment, its costs, and complication rates.
Conclusion
Within the limitations posed by the methodological quality of the studies selected for this systematic review, the two-stage procedure was associated with a higher rate of infection eradication than one-stage revision in periprosthetic knee infections at comparable follow-up duration. Articulating spacers were found to be associated with lower recurrence of infection than static spacers. Two-stage revision with the use of an articulating spacer appears to provide better infection control of chronically infected knee prosthesis, and so may be considered as the treatment of choice over other revision strategies.
References
Anderson JA, Sculco PK, Heitkemper S, Mayman DJ, Bostrom MP, Sculco TP (2009) An articulating spacer to treat and mobilize patients with infected total knee arthroplasty. J Arthroplasty 24:631–635
Bernard L, Legout L, Zürcher-Pfund L, Stern R, Rohner P, Peter R, Assal M, Lew D, Hoffmeyer P, Uçkay I (2010) Six weeks of antibiotic treatment is sufficient following surgery for septic arthroplasty. J Infect 61(2):125–132
Booth RE, Lotke PA (1989) The results of spacer block technique in revision of infected total knee arthroplasty. Clin Orthop Relat Res 248:57–60
Borden LS, Gearen PF (1987) Infected total knee arthroplasty: a protocol for management. J Arthroplasty 2(1):27–36
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468:45–51
Buechel FF, Femino FP, D’Alessio J (2004) Primary exchange revision arthroplasty for infected total knee replacement: a long-term study. Am J Orthop 33(4):190–198
Calton TF, Fehring TK, Griffin WL (1997) Bone loss associated with the use of spacer blocks in infected total knee arthroplasty. Clin Orthop Relat Res 345:148–154
Cuckler JM (2005) The infected total knee: management options. J Arthroplasty 20(2):33–36
Darley ES, Bannister GC, Blom AW, Macgowan AP, Jacobson SK, Alfouzan W (2011) Role of early intravenous to oral antibiotic switch therapy in the management of prosthetic hip infection treated with one- or two-stage replacement. J Antimicrob Chemother 66(10):2405–2408
Duncan CP, Beauchamp C (1993) A temporary antibiotic-loaded joint replacement system for management of complex infections involving the hip. Orthop Clin North Am 24(4):751–759
Durbhakula SM, Czajka J, Fuchs MD, Uhl RL (2004) Antibiotic-loaded articulating cement spacer in the 2-stage exchange of infected total knee arthroplasty. J Arthroplasty 19:768–774
Emerson RH Jr, Muncie M, Tarbox TR, Higgins LL (2002) Comparison of a static with a mobile spacer in total knee infection. Clin Orthop Relat Res 404:132–138
Evans RP (2004) Successful treatment of total hip and knee infection with articulating antibiotic components: a modified treatment method. Clin Orthop Relat Res 427:37–46
Fehring TK, Odum S, Calton TF, Mason JB (2000) Articulating versus static spacers in revision total knee arthroplasty for sepsis. The Ranawat Award. Clin Orthop Relat Res 380:9–16
Freeman MG, Fehring TK, Odum SM, Fehring K, Griffin WL, Mason JB (2007) Functional advantage of articulating versus static spacers in 2-stage revision for total knee arthroplasty infection. J Arthropl 22(8):1116–1121
Gacon G, Laurencon M, Van de Velde D, Giudicelli DP (1997) Two stages reimplantation for infection after knee arthroplasty. Apropos of a series of 29 cases. Rev Chir Orthop Reparatrice Appar Mot 83:313–323
Goksan SB, Freeman MA (1992) One-stage reimplantation for infected total knee arthroplasty. J Bone Joint Surg Br 74:78–82
Goldman RT, Scuderi GR, Insall JN (1996) 2-stage reimplantation for infected total knee replacement. Clin Orthop Relat Res 331:118–124
Goldstein WM, Kopplin M, Wall R, Berland K (2001) Temporary articulating methylmethacrylate antibiotic spacer (TAMMAS). A new method of intraoperative manufacturing of a custom articulating spacer. J Bone Joint Surg Am 83:92–97
Gooding CR, Masri BA, Greidanus NV, Garbuz DS (2011) Durable infection control and function with the PROSTALAC spacer in two-stage revision for infected knee arthroplasty. Clin Orthop Relat Res 469:985–993
Haddad FS, Masri BA, Campbell D et al (2000) The Prostalac functional spacer in two-stage revision for infected knee replacements. J Bone Joint Surg (Br) 82(6):807–812
Haleem AA, Berry DJ, Hanssen AD (2004) Mid-term to long-term follow-up of two-stage reimplantation for infected total knee arthroplasty. Clin Orthop Relat Res:35
Hanssen AD, Rand JA, Osmon DR (1994) Treatment of the infected total knee arthroplasty with insertion of another prosthesis. The effect of antibiotic-impregnated bone cement. Clin Orthop Relat Res 309:44–55
Hart WJ, Jones RS (2006) Two-stage revision of infected total knee replacements using articulating cement spacers and short-term antibiotic therapy. J Bone Joint Surg Br 88(8):1011–1015
Henderson MH Jr, Booth RE Jr (1991) The use of an antibiotic-impregnated spacer block for revision of the septic total knee arthroplasty. Semin Arthroplasty 2(1):34–39
Hirakawa K, Stulberg BN, Wilde AH, Bauer TW, Secic M (1998) Results of 2-stage reimplantation for infected total knee arthroplasty. J Arthroplasty 13:22–27
Hoad-Reddick DA, Evans CR, Norman P, Stockley I (2005) Is there a role for extended antibiotic therapy in a two-stage revision of the infected knee arthroplasty? J Bone Joint Surg Br 87(2):171–174
Hofmann AA, Goldberg T, Tanner AM, Kurtin SM (2005) Treatment of infected total knee arthroplasty using an articulating spacer: 2- to 12-year experience. Clin Orthop Relat Res 430:125–131
Hofmann AA, Kane KR, Tkach TK, Plaster RL, Camargo MP (1995) Treatment of infected total knee arthroplasty using an articulating spacer. Clin Orthop Relat Res 321:45–54
Hsieh PH, Huang KC, Lee PC, Lee MS (2009) Two-stage revision of infected hip arthroplasty using an antibiotic-loaded spacer: retrospective comparison between short-term and prolonged antibiotic therapy. J Antimicrob Chemother 64(2):392–397
Hsu YC, Cheng HC, Ng TP, Chiu KY (2007) Antibiotic-loaded cement articulating spacer for 2-stage reimplantation in infected total knee arthroplasty. A simple and economic method. J Arthroplasty 22:1060–1066
Huang HT, Su JY, Chen SK (2006) The results of articulating spacer technique for infected total knee arthroplasty. J Arthroplasty 21:1163–1168
Jamsen E, Sheng P, Halonen P, Letho MU, Moilanen T, Pajamäki J, Puolakka T, Konttinen YT (2006) Spacer prostheses in two-stage revision of infected knee arthroplasty. Int Orthop 30:257–261
Jämsen E, Stogiannidis J, Malmivaara A, Pajamäki J, Puolakka T, Konttinen YT (2009) Outcome of prosthesis exchange for infected knee arthroplasty: the effect of treatment approach. A systematic review of the literature. Acta Orthopaedica 80(1):67–77
Koo KH, Yang JW, Cho SH, Song HR, Park HB, Ha YC, Chang JD, Kim SY, Kim YH (2001) Impregnation of vancomycin, gentamicin, and cefotaxime in a cement spacer for two-stage cementless reconstruction in infected total hip arthroplasty. J Arthroplasty 16:882–892
Lombardi AV, Karney JM, Berend KR (2007) A motion maintaining antibiotic delivery system. J Arthroplasty 22:50–55
Lonner JH, Beck TD Jr, Rees H, Roullet M, Lotke PA (2001) Results of twostage revision of the infected total knee arthroplasty. Am J Knee Surg 14:65–67
Lu H, Kou B, Lin J (1997) One-stage reimplantation for the salvage of total knee arthroplasty complicated by infection. Zhonghua Wai Ke Za Zhi 35:456–458
MacAvoy MC, Ries MD (2005) The ball and socket articulating spacer for infected total knee arthroplasty. J Arthroplasty 20:757–762
Malmivaara A, Koes BW, Bouter LM, van Tulder MW (2006) Applicability and clinical relevance of results in randomized controlled trials: the Cochrane review on exercise therapy for low back pain as an example. Spine 31(13):1405–1409
Masri BA, Kendall RW, Duncan CP, Beauchamp CP, McGraw RW, Bora B (1994) Two-stage exchange arthroplasty using a functional antibiotic-loaded spacer in the treatment of the infected knee replacement: the Vancouver experience. Semin Arthroplasty 5:122–136
Masri BA, Duncan CP, Beauchamp CP (1998) Long-term elution of antibiotics from bone-cement: an in vivo study using the prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) system. J Arthroplasty 13(3):331–338
McPherson EJ, Lewonoswski K, Dorr LD (1995) Use of an articulated PMMA spacer in the infected total knee arthroplasty. J Arthroplasty 10(1):87–89
McPherson EJ, Patzakis MJ, Gross JE, Holtom PD, Song M, Dorr LD (1997) Infected total knee arthroplasty: two-stage reimplantation with a gastrocnemius rotational flap. Clin Orthop Relat Res 341:73–76
Meek RM, Dunlop D, Garbuz DS, McGraw R, Greidanus NV, Masri BA (2004) Patient satisfaction and functional status after aseptic versus septic revision total knee arthroplasty using the PROSTALAC articulating spacer. J Arthroplasty 19(7):874–879
Mutimer J, Gillespie G, Lovering AM, Porteous AJ (2009) Measurements of in vivo intra-articular gentamicin levels from antibiotic loaded articulating spacers in revision total knee replacement. Knee 16(1):39–41
Ocguder A, Firat A, Tecimel O, Solak S, Bozkurt M (2010) Two-stage total infected knee arthroplasty treatment with articulating cement spacer. Arch Orthop Trauma Surg 130:719–725
Pascale V, Pascale W (2007) Custom-made articulating spacer in two-stage revision total knee arthroplasty. An early follow-up of 14 cases of at least 1 year after surgery. HSSJ 3:159–163
Pietsch M, Wenisch C, Traussing S, Trnoska R, Hofmann S (2003) Temporary articulating spacer with antibiotic-impregnated cement for an infected knee endoprosthesis. Orthopade 32:490–497
Pitto RP, Castelli CC, Ferrari R, Munro J (2005) Pre-formed articulating knee spacer in two stage revision for the infected total knee arthroplasty. Int Orthop 29:305–308
Rosenberg AG, Haas B, Barden R, Marquez D, Landon GC, Galante JO (1988) Salvage of infected total knee arthroplasty. Clin Orthop Relat Res 226:29–33
Scott IR, Stockley L, Getty CJM (1993) Exchange arthroplasty for infected knee replacements. J Bone Joint Surg (Br) 75(1):28–31
Shen H, Zhang X, Jiang Y, Wang Q, Chen Y, Wang Q, Shao J (2010) Intraoperatively-made cement-on-cement antibiotic-loaded articulating spacer for infected total knee arthroplasty. Knee 17(6):407–411
Siebel T, Kelm J, Porsch M, Regitz T, Neumann WH (2002) Two-stage exchange of infected knee arthroplasty with a prosthesis-like interim cement spacer. Acta Orthop Belg 68:150–156
Silva M, Tharani R, Schmalzried TP (2002) Results of direct exchange or debridement of the infected total knee arthroplasty. Clin Orthop Relat Res 404:125–131
Sofer D, Regenbrecht B, Pfeil J (2005) Early results of one-stage septic revision arthroplasties with antibiotic-laden cement. A clinical and statistical analysis]. Orthopade 34(6):592–602
Spangehl MJ, Masri BA, O’Connell JX, Duncan CP (1999) Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg Am 81:672–683
Van Thiel GS, Berend KR, Klein GR, Gordon AC, Lombardi AV, Della Valle CJ (2011) Intraoperative molds to create an articulating spacer for the infected knee arthroplasty. Clin Orthop Relat Res 469:994–1001
van Tulder MW, Assendelft WJ, Koes BW, Bouter LM (1997) Method guidelines for systematic reviews in the Cochrane collaboration back review group for spinal disorders. Spine 22(20):2323–2330
Villa T, Carnelli D (2007) Experimental evaluation of the biomechanical performances of a PMMA-based knee spacer. Knee 14:145–153
Villanueva-Martinez M, Rios-Luna A, Pereiro J, Chana F, Fahandez-Saddi H (2006) Hand-made articulating spacers for infected total knee arthroplasty: a technical note. Acta Orthop 77(2):329–332
Villanueva-Martínez M, Ríos-Luna A, Pereiro J, Fahandez-Saddi H, Villamor A (2008) Hand-made articulating spacers in two-stage revision for infected total knee arthroplasty: good outcome in 30 patients. Acta Orthop 79(5):674–682
von Foerster G, Kluber D, Kabler U (1991) Mid- to long-term results after treatment of 118 cases of periprosthetic infections after knee joint replacement using one-stage exchange surgery. Orthopade 20:244–252
Walker RH, Schurman DJ (1984) Management of infected total knee arthroplasties. Clin Orthop Relat Res 186:81–89
Whiteside LA (1994) Treatment of infected total knee arthroplasty. Clin Orthop Relat Res 299:169–172
Wilde AH, Ruth JT (1988) Two-stage reimplantation in infected total knee arthroplasty. Clin Orthop Relat Res 236:23–27
Windsor RE, Insall JN, Urs WK, Miller DV, Brause BD (1990) Two-stage reimplantation for the salvage of total knee arthroplasty complicated by infection. Further follow-up and refinement of indications. J Bone Joint Surg Am 72:272–278
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Romanò, C.L., Gala, L., Logoluso, N. et al. Two-stage revision of septic knee prosthesis with articulating knee spacers yields better infection eradication rate than one-stage or two-stage revision with static spacers. Knee Surg Sports Traumatol Arthrosc 20, 2445–2453 (2012). https://doi.org/10.1007/s00167-012-1885-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-012-1885-x