Abstract
Purpose
Restoration of neutral mechanical alignment is traditionally considered as one of the prerequisites for successful total knee replacement. The purpose of this study was to investigate whether a certain bias towards undercorrection exists with conventional total knee arthroplasty (TKA) instruments.
Methods
A cohort of 456 consecutive patients, who underwent the same standardised TKA with restoration of neutral mechanical alignment as target, was studied. Based on the preoperative alignment, patients were stratified into three categories: valgus, neutral and varus. Component and limb alignment were compared between these groups.
Results
The mean post-operative hip–knee–ankle angle was −0.7° (SD 2.5) in valgus knees, 0.2° (SD 1.9) in neutral knees and 2.4° (SD 3.9) in varus knees (p < 0.001). About 39.8 % of the varus knees remained in >3° of varus post-operative and 20.2 % of the valgus knees remained in <−3° of valgus. A systematic unintentional undercorrection was noted in varus knees, which was proportional to the preoperative varus deformity and which was caused by varus positioning of both the femoral and tibial components. In valgus knees, the undercorrection was caused almost exclusively by valgus bias of the femoral component’s position.
Conclusion
This study showed that conventional TKA instruments are associated with a systematic unintentional bias towards undercorrection of the pre-existing deformity. The clinical relevance of this study is that intentionally aiming at slight undercorrection of the deformity may lead to excessive undercorrection in reality in case the surgeon does not recognise the automatic bias that already exists with standard instruments.
Level of evidence
Therapeutic study, Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The concept of the constitutional varus was recently introduced by Bellemans et al., showing that a significant proportion of the healthy population has a natural alignment ≥3° of varus at the end of growth [1]. Correcting the coronal limb alignment during total knee arthroplasty (TKA) to a neutral mechanical axis might indeed create an abnormal situation in these patients. Only correcting for the worn cartilage and bone and not for the pre-existing varus deformity would therefore mean that one would have to accept post-operative varus. Growing evidence exists that slight undercorrection might not be as harmful for the survival of the implant as previously thought [2, 6, 8, 10, 11], and might actually result in a better clinical outcome [13]. However, aiming at slight undercorrection also inherently carries the risk of ending up in severe undercorrection, which could be detrimental for implant survivorship.
Based upon these arguments, surgeons recently have started to consider slight undercorrection of the deformity, while at the same time avoiding important severe undercorrection. Such requires of course a great degree of accuracy during surgery, as well as a correct understanding of what is obtained today when using contemporary TKA systems. It has indeed for a long time been our impression that with current TKA techniques and instruments, a certain error bias towards undercorrection already exists. Recent literature has demonstrated that with contemporary TKA systems, neutral mechanical alignment is only obtained in 70–80 % of the patients, even when performed by experienced surgeons [2, 8, 10, 11, 13].
The purpose of this study was to investigate this in a large patient cohort. Our hypothesis was that current TKA instruments are already associated with an automatic bias towards undercorrection of the deformity (1), and that such bias is proportional to the magnitude of the arthritic deformity (2).
Materials and methods
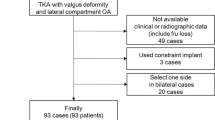
A cohort of 456 consecutive patients who underwent a posterior stabilised (PS) TKA at our service between 2009 and 2011 were studied. All patients (1,045) undergoing a TKA during that period were prospectively included in our knee arthroplasty database. Selection criteria were applied to these 1,045 patients. Only the patients with primary osteoarthritis as indication were selected (997). Patients with rheumatoid arthritis or post-traumatic osteoarthritis were excluded (48). To avoid bias from different instrumentation systems, only the patients receiving the Genesis II PS prosthesis (Smith & Nephew Inc., Andover, MA) were included (509). Other types of prostheses were excluded. Twenty-two cases were excluded because radiographs were not taken according to Paley’s criteria [9]. Fourteen patients with bilateral TKA surgery (2 × 14) were also excluded. As a result of all these selection criteria, our working database consisted of 456 patients.
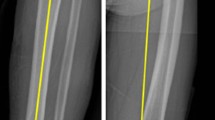
All surgeries were performed in a single institution (Department of Orthopaedic Surgery, University Hospital Leuven, Pellenberg, Belgium) by one surgical team. An intramedullary instrumentation technique was used on both the femur and tibia with the restoration of a neutral mechanical alignment as target in all knees. To obtain a tibial cut perpendicular to the mechanical axis, the extramedullary alignment system was used in conjunction with the intramedullary alignment. First, the tibial cutting block was fixed using the intramedullary system, introduced through a central drill hole in the proximal tibia. Next, the extramedullary alignment system was attached to the cutting block as a check and adjustment were made when necessary. In cases of excessive tibial bowing, only the extramedullary system was used. For the femur, a standard 5° valgus angle was used in all patients except in women with an 8° or more valgus angle as measured on the preoperative full-limb standing radiographs. A 6° valgus angle was used in these patients. In all cases, the intramedullary rod was inserted through a centrally located drill hole just anterior to the top of the notch and slightly medial.
Standard standing anteroposterior (AP), lateral and full-leg radiographs were obtained for all knees pre- and post-operatively as part of a standard TKA protocol. The weight-bearing full-leg radiographs, which included the whole pelvis, were obtained with the patient standing while ensuring that the patellae were oriented forwards, as we described previously [1]. These radiographs were calibrated, and all measurements were taken using the AGFA Picture Archive and Communication System (PACS) (Agfa-Gevaert, Mortsel, Belgium). Alignment of the leg was determined based on these radiographs. Femoral and tibial mechanical axes were defined according to the criteria defined by Cooke et al. [5]. The hip centre was obtained using concentric Moose circles. The preoperative centre of the knee was determined as the intersection of the midline between the tibial spines and the midline between the femoral condyles and tip of the tibia. The centre of the ankle was determined as the mid-width of the talus. Post-operatively, full-length hip–knee–ankle radiographs were repeated, and the centre of the hip and ankle was calculated as mentioned above. After TKA, the centre of the knee was determined as the intersection of the midline in the middle of the polyethylene inlay and the midline between the condyles of the femoral component and the tip of the tibial component. Using these three points on the pre- and post-operative radiographs, the hip–knee–ankle (HKA) angle of the lower leg could be calculated. The HKA angle was defined as the angle formed by the mechanical femoral axis and the mechanical tibial axis. The HKA angle was expressed as a deviation from 180° with a negative value for valgus and positive value for varus alignment. The lateral angle formed between the mechanical femoral axis and the knee joint line of the distal femur was defined as the mechanical lateral distal femoral angle (mLDFA). The medial proximal tibial angle (MPTA) was defined as the medial angle formed between the mechanical tibial axis and the knee joint line of the proximal tibia. The angle between the knee joint lines of the distal femur and proximal tibia was called the joint line convergence angle (JLCA). An independent observer (FV) performed the radiographic measurements within a range of accuracy of 0.1°. Literature has shown a high intra- and inter-observer accuracy using this method [4, 12].
The patients were subdivided into three categories, based on their preoperative HKA angle: HKA angle > 3° = varus; −3° ≤ HKA angle ≤ 3° = neutral; HKA angle < −3 = valgus.
The study protocol was approved by the Ethics Committee of the University of Leuven, Belgium.
According to the preoperative alignment, there were 249 varus knees (54.6 %), 103 neutral knees (22.6 %) and 104 valgus knees (22.8 %). Demographic variables for these groups are presented in Table 1.
Statistical analysis
Signed rank tests are used to evaluate the differences between pre- and post-operation measurements. Groups are compared with χ 2-test (or Fisher’s exact tests) and Mann–Whitney U tests (Kruskal–Wallis for the comparison of more than two groups). Associations between variables are verified with Spearman correlations. A (bivariable) linear regression model is used to relate the post-operative HKA with the post-operative tibial and femoral joint line orientation. P values smaller than 0.01 are considered significant. All analyses have been performed using SAS software, version 9.2 of the SAS System for Windows (SAS Institute Inc., Cary, NC, USA).
Results
The mean HKA angle was found to be 3.2° (SD 7.7) in the osteoarthritic knee and was 1.2° (SD 3.1) after TKA (p < 0.001) (Fig. 1). The mean HKA angle after TKA was −0.7° (SD 2.5) in knees that were preoperatively in valgus, 0.2° (SD 1.9) in knees that were preoperatively neutral and 2.4° (SD 3.9) in knees that were preoperatively in varus. This was a statistically significant difference (Table 2).
Out of the 249 patients with preoperative varus, 39.8 % remained in >3° of varus after TKA. Out of the 104 patients with preoperative valgus, 20.2 % remained in <−3° of valgus (Table 3). About 85.4 % of the preoperative neutrally aligned knees remained neutral post-operative. About 14.6 % of the neutral knees were overcorrected to either a varus or valgus alignment post-operative.
A systematic unintentional undercorrection was seen in varus knees (R 2 = 0.58597) (Fig. 2). The more preop varus, the more undercorrection was performed. The same undercorrection existed for valgus knees, although significantly less pronounced (R 2 = 0.60561) (p < 0.001). The median correction of the alignment deformity was 89.3 % in valgus knees versus 75.7 % in varus knees (p = 0.002).
Scatter plot of the preoperative mTFA against the alignment correction that was performed. The red lines represent the required correction for a 0° mTFA. The blue line represents the linear correlation for the actual achieved correction. All values above the red lines represent overcorrection, everything below the line represents undercorrection, e.g., a knee with a preoperative mTFA of 5° requires a 5° correction to achieve a neutral alignment but on average, a 4° correction was done. A systematic undercorrection is seen in varus knees. The more the varus, the more undercorrection. The same observation exists in valgus knees, although significantly less pronounced
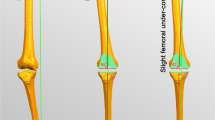
The undercorrection in varus knees was the consequence of varus of both the femoral and tibial components (Fig. 3). The femoral component contributed to 45.8 % of the post-operative varus and the tibial component to 50 %. In valgus knees, the undercorrection was caused almost exclusively by valgus bias of the femoral component’s position.
Different joint line angles after TKA and their contribution to the overall limb alignment (HKA angle) are stratified according to the preoperative alignment. The medial proximal tibial angle (MPTA) and the mechanical lateral distal femoral angle (mLDFA) are expressed as deviation from neutral. The average value for each alignment category is shown
The joint line anatomy (MPTA, mLDFA) of the osteoarthritic knee proved to be significantly different in the different alignment groups (Table 2). In valgus knees, the main coronal plane deformity is located on the femoral side with an average 4.5° deviation of the mLDFA from neutral (Fig. 4). The deviation on the tibial side in valgus knees is minimal in most cases (mean 0.9°). In varus knees, on the other hand, the femur is almost neutrally aligned with an mLDFA of on average 89.5°. The deformity is found on the tibial side here with a deviation from neutral of the MPTA of on average 5.0°. The neutral knee shows a combination of slight femoral valgus with slight tibial varus.
Different joint line angles in the native osteoarthritic knee and their contribution to the overall limb alignment (HKA angle) are stratified according to the preoperative alignment. The medial proximal tibial angle (MPTA) and the mechanical lateral distal femoral angle (mLDFA) are expressed as deviation from neutral. The average value for each alignment category is shown
After TKA, the mLDFA and MPTA were similar in neutral and valgus knees but significantly different when compared to varus knees (Table 2).
Discussion
The most important finding of this study was that in conventional TKA, there is an inherent unintentional bias towards undercorrection of the pre-existing deformity. Such bias is proportional to the magnitude of the preoperative deformity. In other words, the more preoperative varus (or valgus), the more undercorrection is performed. The bias towards undercorrection is also greater in varus knees than in valgus knees. The median correction of the alignment deformity was 89.3 % in valgus knees versus 75.7 % in varus knees (p = 0.002). It is important to note that the target in all of these cases was to restore the knee to neutral mechanical alignment. The tendency towards undercorrection was therefore unintentional.
These observations shed a new light over the alignment discussion in TKA. Should we aim at undercorrection in patients with preoperative varus in order to restore the patient’s anatomy rather than reproduce a neutral mechanical alignment? Before we can answer that question, we should first understand what alignment is actually achieved with classic instrumented TKA and identify the factors influencing this. Such knowledge is crucial before a shift in alignment target can be advocated. Based on our data, aiming at slight varus instead of neutral when performing a TKA is very likely to cause more varus outliers. In our series, already 8.8 % of the patients had an HKA angle of more than 6° of varus after TKA. And according to our previously published data, those patients might perform worse [13]. We would therefore caution against a global shift of the alignment target towards slight varus.
There are several mechanisms that can explain these findings. The use of an intramedullary instrumentation system on the femur and a combined system on the tibia is influenced by the patient’s anatomy. Femoral bowing and the position of the entry hole will influence the course of the intra-medullary rod in the femur and thus the valgus resection angle. From our previous work, we know that the valgus angle is on average 4.51° in varus knees, 4.44° in neutral knees and 3.98° in valgus knees [1]. One would therefore expect that a standard 5° valgus cut would cause some undercorrection on the femoral side. This is indeed true for valgus knees. However, a slight varus position of the femoral component is observed in most varus knees in our series. Varus femoral bowing observed in varus knees might be an explanation for this [1]. This varus femoral bowing was found to be 0.45° in varus knees [1]. In neutral knees and valgus knees, a femoral bowing of 0.11° and 0.16°, respectively, was observed. Proximal tibial varus is another important variable. With an intramedullary technique and a central entry hole on the tibia, this proximal tibial varus will cause a bias towards varus of the tibial cut. We were well aware of this bias while performing the surgery. To avoid it, we use a combined intra- and extramedullary technique on the tibia. Nevertheless, a bias towards varus of the tibial component in varus knees was still observed. This effect was absent in valgus and neutral knees. Also, the surgeon should be considered an important variable in the alignment equation. In this study, all surgeries were performed by the same surgical team. This team consisted of two leading senior surgeons and senior orthopaedic residents under their supervision. As multiple surgeons were involved, we believe that these results are relative surgeon independent and can therefore be attributed to the instrumentation technique and the patient’s anatomy mainly.
In the debate on limb alignment after TKA, the focus has mainly been on varus knees as they make out the biggest proportion of the osteoarthritic knees that are treated with a TKA (54.6 % of the knees in our series). However, neutral knees and valgus knees should not be overlooked. In this study, we found a distinct joint line anatomy between the 3 alignment categories (Fig. 4). In valgus knees, the main coronal plane deformity is mainly located on the femoral side with an average −4.5° deviation of the mLDFA from neutral. The deformity on the tibial side in valgus knees is minimal in most cases (mean 0.9°). In varus knees, on the other hand, the femur is almost perfectly neutrally aligned with an mLDFA of on average 89.5°. The deformity is found on the tibial side here with on average 5.0° proximal tibial varus. The same instrumentation technique resulted in a different post-operative joint line configuration in the three groups (Fig. 3). Conclusions on varus knees can therefore not automatically be implemented on neutral and valgus knees. Femoral component valgus, for instance, might indeed be harmful for a knee that was preoperatively in varus [8] but might on the other hand give a better result in a valgus knee. Failure to stratify results according to the preoperative alignment is therefore one of the major limitations of previous outcome studies on alignment after TKA [11].
This study has several limitations. First of all, patients with a flexion contracture were not excluded from the analysis. We are well aware of the fact that a flexion contracture decreases the accuracy of measuring coronal limb alignment [3, 7]. However, a flexion contracture is inherently bound to the osteoarthritic process and is frequently seen in more severe osteoarthritis. Exclusion of these patients would therefore also introduce selection bias. Secondly, only results of one instrumentation system were analysed. Other systems could produce different results. Thirdly, a standard 5° valgus resection angle was selected in most cases. Using a different angle might result in different data.
Conclusion
This study showed that conventional TKA instruments are inherently associated with a systematic unintentional bias towards undercorrection of the pre-existing deformity. Such bias was proportional to the magnitude of the preoperative deformity, and was greater in varus knees than in valgus knees. Based on these results, we caution against a shift of the alignment target towards more varus, as this is likely to cause more varus outliers. The clinical relevance of this study is that intentionally aiming at undercorrection of the deformity during TKA may lead to excessive undercorrection in reality in case the surgeon does not recognise this automatic bias.
References
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470:45–53
Bonner TJ, Eardley WGP, Patterson P, Gregg PJ (2011) The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg Br 93:1217–1222
Brouwer RW, Jakma TSC, Brouwer KH, Verhaar JAN (2007) Pitfalls in determining knee alignment: a radiographic cadaver study. J Knee Surg 20:210–215
Colebatcha AN, Hartb DJ, Zhaib G, Williamsb FM, Spectorb TD, Ardena NK (2009) Effective measurement of knee alignment using AP knee radiographs. Knee 16:42–45
Cooke TDV, Sled EA, Scudamore RA (2007) Frontal plane knee alignment: a call for standardized measurement. J Rheumatol 34:1796–1801
Fang DM, Ritter MA, Davis KE (2009) Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplast 24:39–43
Lonner JH, Laird MT, Stuchin SA (1996) Effect of rotation and knee flexion on radiographic alignment in total knee arthroplasties. Clin Orthop Relat Res 331:102–106
Magnussen RA, Weppe F, Demey G, Servien E, Lustig S (2011) Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res 469:3443–3450
Paley D (2003) Principles of deformity correction. Springer, Heidelberg, pp 1–60
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92:2143–2149
Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 93:1588–1596
Sabharwal S, Zhao CEM (2008) Lower limb alignment in children: reference values based on a full-length standing radiograph. J Pediatr Orthop 28:740–746
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Luyckx, T., Vanhoorebeeck, F. & Bellemans, J. Should we aim at undercorrection when doing a total knee arthroplasty?. Knee Surg Sports Traumatol Arthrosc 23, 1706–1712 (2015). https://doi.org/10.1007/s00167-014-3185-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3185-0