Abstract
Purpose
To investigate the differences in the incidence and severity of knee osteoarthritis (OA), joint space narrowing, knee laxity, and knee flexion and extension strength between an anterior cruciate ligament (ACL)-reconstructed knee and the contralateral non-reconstructed limb.
Methods
Retrospective case series of patients from a single surgeon that had an ACL reconstruction with a semitendinosus/gracilis autograft more than 12 years ago. Outcome measures included radiographic analysis, International Knee Documentation Committee Subjective Knee Evaluation Form (IKDC), KT-1000, Tegner Activity Level Scale, Lysholm Knee Score, ACL quality of life score (ACL-QOL) and knee flexor/extensor strength.
Results
Seventy-four patients consented and sixty-eight (43 male, 25 female) were included for analysis. Average age (SD) at the time of surgery was 31.2 (±9.1) years. At follow-up of 14.6 (1.9) years, 9 % had re-ruptured their ACL, whereas 5 % ruptured the contralateral ACL. Reconstructed knees had a greater incidence and severity of OA (P < 0.01). Medial meniscus surgery was a strong predictor of OA. Seventy-five per cent scored a normal or nearly normal knee on the IKDC. The mean Lysholm score was 75.8 % and Tegner Activity Level Scale scores decreased (P < 0.001) from the time of surgery. Knee extension strength was greater in the contralateral knee at speeds of 60°/s (P = 0.014) and 150°/s (P = 0.012).
Conclusions
Reconstructed knees have a greater incidence and severity of OA than non-reconstructed knees, which suggests degenerative changes are secondary to ACL rupture. Medial meniscus surgery is a strong predictor of OA. Despite this, 75 % of patients reported good outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anterior cruciate ligament (ACL) plays a critical role as a primary stabilizer of the human knee [5]. Rupture of the ACL is one of the most common knee injuries with an annual incidence in the United States of 80,000 tears and a cost of more than 1 billion dollars to the health care system [11]. Adolescents and young adults who sustain an ACL injury are at an increased risk for the development of osteoarthritis (OA) [3–6, 8, 22, 21, 30], with >50 % of ACL injured knees demonstrating OA 5–15 years after initial injury [7, 11, 12, 15, 30, 32]. Reconstruction attempts to re-establish normal joint kinematics and structural integrity, while at the same time decreasing the likelihood of suffering further joint injury or deterioration [14].
Since 2005, several studies have investigated long-term results (7 years or greater) of ACL reconstruction [2, 4, 12, 13, 15, 16, 19, 20, 22, 25, 28, 29, 32, 35, 37–40]. However, ACL reconstruction is an oversimplified description of the procedure since several variations exist, including, but not limited to, tunnel placement, graft fixation and type of graft used to reconstruct the ligament. Current autograft options include the patellar tendon or the semitendinosus/gracilis (hamstring) tendons [23]. In addition, several allograft (tissues from cadaver) options are available, including, but not limited to, patellar tendon, hamstring tendons, Achilles tendon and tibialis anterior or posterior tendons [7].
Long-term follow-up studies that included patients who had undergone ACL reconstruction using hamstring tendons, as a case series or compared to bone–patellar tendon–bone grafts, have been reported [4, 18, 20, 32, 33, 37]; however, the number of patients evaluated beyond 10 years is limited. The high incidence of OA in long-term studies of ACL reconstruction [15, 20, 25, 26, 29, 31, 32] and paucity of information on thigh strength in these patients [25, 28] motivated the authors to undertake this study (Table 1). Since major muscle tendons are harvested during ACL reconstruction, the authors felt it was imperative to investigate the thigh strength at long-term follow-up to determine whether graft site morbidity persists beyond 14 years following surgery. To date, this is the largest sample size of patients that have undergone strength testing on long-term follow-up following an ACL reconstruction with a hamstring autograft.
The primary objective of this retrospective study was to determine whether ACL-reconstructed knees with a hamstring autograft have a greater incidence of degenerative changes compared with the contralateral non-reconstructed knee. Secondary objectives were to determine whether there was a difference between the ACL- and non-reconstructed knees in knee flexion and extension concentric strength; to determine whether there was an association between patient quality of life and joint degeneration; and to identify risk factors that may predispose individuals to long-term degenerative changes of the knee joint, including age, gender, body mass index (BMI), time to surgery and medial/lateral meniscal damage at the time of surgery.
The primary hypothesis of this study was that there is no difference in the incidence and severity of knee OA in the ACL-reconstructed limb compared with the contralateral limb of patients that had surgery more than 12 years ago. Secondary hypotheses were that there is no difference in knee laxity and knee flexion and extension strength between ACL- and non-reconstructed-knees.
Materials and methods
Human research ethics approval was obtained from the local review board prior to the initiation of any study activities. All study activities took place at a sports medicine clinic.
This was a retrospective case series of consecutive patients from a single surgeon. The surgeon is a fellowship trained orthopaedic sports medicine surgeon with over 20 years of experience. All patients that underwent ACL reconstruction between 1992 and 1998 were eligible for the study. Potential patients were identified through a computer database and medical records reviewed to confirm eligibility. Patients were excluded if they had an ACL reconstruction or previous knee surgery, other than an arthroscopic surgery, on either knee.
Surgical procedure
Patients were given a spinal or general anaesthetic. A trans-tibial tunnel technique was utilized and a four-strand semitendinosus/gracilis autograft was harvested to reconstruct the native ACL. Tension was maintained on the graft while a bioscrew was placed on the guidewire and into the tibial tunnel. Bioscrews (Linvatec, Largo, FL) were used to secure the reconstructed ligament in both the femoral and tibial tunnels. A standardized post-operative rehabilitation program emphasized early swelling control and knee range of motion.
Outcome measures
Standardized bilateral weight-bearing radiographs were obtained for each patient at the commencement of the assessment appointment. The primary outcome measure was evidence of OA based on the Kellgren–Lawrence Scale [16], where 0 = none; 1 = doubtful; 2 = minimal; 3 = moderate; and 4 = severe. This scale takes into account joint space narrowing, osteophytes and sclerosis. Bilateral anterior/posterior-, lateral- and notch-view X-rays were obtained and reviewed by a musculoskeletal-trained radiologist. The radiologist also reported presence and severity of joint line narrowing in each of the medial and lateral compartments as ‘none’, ‘mild’, ‘moderate’ or ‘severe’.
Secondary measures included the following: (1) demographic information, (2) ACL quality of life subjective outcome score, (3) Lysholm Knee Scale, (4) Tegner Activity Level Scale, (5) the International Knee Documentation Committee (IKDC) clinical assessment form, (6) anterior tibial translation and (7) concentric knee flexion and extension strength. The ACL-QOL subjective outcome score is a self-administered disease-specific questionnaire developed and validated for patients with ACL deficiency [27]. The IKDC is a well-referenced knee joint-specific clinical assessment that includes range of motion, as well as pertinent clinical tests to evaluate laxity of ACL, PCL, and medial and lateral collateral ligaments: Lachman’s test, anterior drawer, posterior drawer, pivot shift and external rotation (IKDC 2000). It also includes a single hop functional test. The KT-1000 arthrometer (Medmetric Corporation, San Diego, CA) was used for measuring anterior tibial translation on the femur [3].
Concentric isokinetic knee flexion and extension strength were measured in a seated position from 5º to 85º knee flexion on a Biodex III dynamometer (Biodex Medical Systems Inc., Shirley, NY). After warm-up, three repetitions were performed for each movement at 60°/s, 150°/s and 240°/s with 20-s rest between speeds. Peak knee flexion and knee extension torques were determined for each velocity.
Approval was obtained from the University of Manitoba Health Research Ethics Board and the Winnipeg Regional Health Authority Research Access Committee prior to the initiation of any study activities.
Statistical analysis
Descriptive statistics were generated for demographic data. Wilcoxon signed-rank tests were performed to evaluate the differences in Kellgren–Lawrence ratings between knees, as well as differences between medial and lateral joint line narrowing. Repeated measures t tests were used to compare knee laxity, as well as pre-operative and current Tegner scores. A repeated measures ANOVA was utilized to compare reconstructed and non-reconstructed knee flexion and extension strength at all three velocities.
Linear regression was performed to determine the contribution of specific variables in predicting Kellgren–Lawrence grade in the reconstructed knee. The variables included the following: present age, age at the time of surgery, height, weight, BMI, gender, and medial and lateral meniscal damage at the time of surgery. A Pearson correlation was also conducted to identify the association between the presence or absence of ACL reconstruction and OA grade according to Kellgren–Lawrence Scale.
All analyses were performed using SPSS 16.0 (IBM SPSS, Atlanta, GA). Statistical tests were considered significant at α = 0.05.
Results
Investigators made verbal contact with a total of 107 patients. Thirty-three patients refused to participate (Fig. 1). Therefore, a total of 74 (69 %) individuals consented to the study. Ten per cent (7/74) of participants underwent a subsequent ACL revision, while an additional five per cent (4/74) had an ACL reconstruction on the opposite leg following initial injury. Participants that had an ACL rupture of the opposite leg were excluded from the analysis. One patient was excluded for having a previous ACL reconstruction and high tibial osteotomy and another for an ongoing workers compensation claim. Therefore, 68 patients (43 male, 25 female) were included in the analysis.
The mean (SD) age of participants at the time of initial surgery was 31.2 (9.1) years and at the time of follow-up was 45.8 (9.2) years. The mean number of years since surgery was 14.6 (1.9). The average BMI at the time of follow-up was 28.5 (4.7). Forty-six per cent (31/68) of participants underwent reconstruction of the right knee and 54 % the left.
Radiological findings
The frequency distribution of Kellgren–Lawrence grades for reconstructed and non-reconstructed knees is presented in Fig. 2. Six per cent of non-reconstructed knees had normal radiological findings; however, 95 % demonstrated a Kellgren–Lawrence grade of 1 or greater. All reconstructed knees had a Kellgren–Lawrence grade of 1 or greater with a higher percentage of knees demonstrating Grade 3 changes (19 %) compared with non-reconstructed knees (4 %). Reconstructed knees presented with increased arthritic changes compared to the contralateral side (P = 0.001). Reconstructed knees had increased medial (P < 0.001) and lateral (P < 0.01) joint line narrowing compared with the non-reconstructed side (Fig. 3). Medial joint space narrowing was more prevalent than lateral (P < 0.001) joint space narrowing for both reconstructed and non-reconstructed knees.
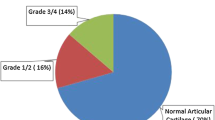
Clinical assessment
International Knee Documentation Committee (IKDC) clinical assessment scores are presented in Fig. 4 with 65 % (44/68) of participants attaining Grade B. Ligament laxity was 7.2 mm (2.7) for the reconstructed side and 6.2 mm (1.8) for the non-reconstructed side. The difference in laxity, as measured by the KT 1000, between the reconstructed side and non-reconstructed side was statistically significant (difference = 1.0; 95 % CI = 0.2–1.8; P = 0.02), although this difference is not considered clinically significant [3].
Knee flexor and extensor strength
Mean (SD) side-to-side knee flexion and extension strength are presented in Table 2. Knee extension strength was greater in the contralateral knee at speeds of 60°/s [reconstructed = 113.9 N/m, contralateral = 120.9 N/m; difference = 7.0 N/m (95 % CI’s = 1.5, 12.5), P = 0.01] and 150°/s (reconstructed = 81.6 N/m, contralateral = 86.2 N/m; difference = 4.6 N/m; 95 % CI’s = 1.1, 8.22; P = 0.01). Conversely, there were no differences between limbs in knee flexion strength at 60°/s (P = n.s.), 150°/s (P = n.s.) or 240°/s (P = n.s.).
Subjective assessment
The mean (SD) Lysholm score was 76.7 (15.4), 5 (7.5 %) patients scored >91, 32 patients (47 %) 81–90, 15 patients (22 %) 71–80 and 16 patients (24 %) below 70. Participants reported a decrease in activity level based on the Tegner Activity Level Scale (P < 0.001). The median pre-operative score was 7 (range = 3–10) and score at long-term follow-up was 5 (range = 1–9). The mean ACL-QOL score was 67.4 % (24.0).
In terms of sporting activity, 23 % (15/64) of participants reported involvement in light sports, 19 % (12/64) in moderate, 1 % (1/64) in moderate and light, and 5 % (3/64) in moderate and contact sports. Fifty-two per cent (33/64) were not involved in any sports.
Factors related to degenerative changes
Potentially relevant variables were included in a regression analysis in an attempt to identify variables that predict Kellgren–Lawrence grade in the reconstructed knee. Medial meniscal surgery (repair or partial meniscectomy) was the only variable found to be a statistically significant predictor (P = 0.012). The presence of joint degeneration, based on Kellgren–Lawrence grade, was found to be significantly correlated with ACL reconstruction (r = 0.366; P = 0.005). In other words, ACL-reconstructed knees were associated with higher (worse) Kellgren–Lawrence grades.
Discussion
The most important finding of this study was that reconstructed knees had a greater incidence and severity of OA than the non-reconstructed side. Medial meniscal surgery (repair or partial meniscectomy) was a strong predictor of OA. Although activity level decreased compared to pre-surgery levels, clinical and subjective outcome measures demonstrated that most patients were satisfied with the surgical outcome and quality of life. Despite harvesting of the semitendinosus and gracilis tendons for the ACL graft, there was no difference in knee flexor strength between the reconstructed and non-reconstructed limbs. However, knee extension strength was decreased in the reconstructed limb compared with the non-reconstructed knee at 60°/s and 150°/s, but not at 240°/s.
Results of the present study demonstrated that in this cohort of hamstring tendon ACL reconstructions, reconstructed knees demonstrate a greater incidence and severity of OA than the control knee. In addition, within ACL-reconstructed knees, medial joint line narrowing was more prevalent than joint space narrowing on the lateral side. Nakata et al. [29] demonstrated that 25 (41 %) patients that had an ACL allograft reconstruction 10 years earlier presented with radiographic evidence of OA. However, there was a greater incidence of joint degeneration in the lateral compartment (33 %) compared with the medial compartment (15 %), which is in contrast to our study and others [2]. Shorter-term follow-up studies have showed a very low incidence of OA in ACL-reconstructed knees at 10- [1] and 7-year post-operatively [4, 20]. Although there is a large variation in the incidence, severity and location of OA in ACL-reconstructed knees at long-term follow-up, meniscectomy has been shown to be a very strong predictor of OA [25, 29–31]. OA has been demonstrated in both ACL-deficient and ACL-reconstructed knees in longer than 10-year follow-up. Reconstructing the ACL has not been shown to be protective against preventing joint degeneration.
International Knee Documentation Committee (IKDC) assessments at long-term follow-up demonstrated that 75 % of patients had normal and nearly normal knees which is consistent with other findings, 80 % [2] and 76 % at 11.5 years [31]. In all three studies, less than 20 % of patients had abnormal knees and 10 % or fewer had severely abnormal knees. In contrast, 99 % of patients that had bone-free allogeneic tendon grafts have reported normal or nearly normal knees at greater than 10-year follow-up [29]. Although the long-term natural history of ACL-reconstructed knees has yet to be determined, IKDC scores at 24.5-year post-surgery have indicated that normal knees remain normal, but nearly normal knees degrade to an abnormal or severely abnormal status [28]. This is cause for concern since more than 75 % of knees that were nearly normal at an 11.5-year follow-up had degraded to abnormal or severely abnormal 13 years later [31].
Using a hamstring graft for ACL reconstruction did not result in decreased knee flexion strength at a mean of 14.6 years following surgery. Although Nakata et al. also assessed leg strength at long-term follow-up, a statistical analysis was not performed and strength was only tested at a slow speed of 60 /s. Our results showed that knee extension strength of the ACL-reconstructed knee was decreased compared to the contralateral control limb. This is in agreement with Nakata et al., but again, a statistical analysis was not performed. Decreased quadriceps strength has been demonstrated almost immediately after ACL rupture [6] and at 5-year post-operatively [17]. To date, there is no mechanistic explanation as to why this muscle group decreases in strength and size following ACL injury. Decreased quadriceps strength and size may be a protective mechanism since contraction of the quadriceps muscle group causes anterior tibial translation with respect to the femur, which would stress the reconstructed ACL.
At long-term follow-up, ACL-reconstructed patients had a median score of 5 on the Tegner Activity Level Scale which was 2 points lower than the median score of 7 at the time of surgery. Several long-term follow-up studies have demonstrated a similar decrease in activity level years after surgery [2, 20, 26]. This suggests that patients continue to play sports like soccer, rugby, hockey, etc., but do so at a recreational level compared to a competitive level at the time the injury occurred. However, Zaffagnini et al. [40] have demonstrated that non-anatomical double-bundle hamstring autograft resulted in less of a decrease in Tegner Activity Level Scale scores compared to lateralized single-bundle bone–patellar tendon–bone autograft [40]. Given the average age at the time of injury and then at the time of follow-up, the decrease in activity may be more a reflection of lifestyle change and not decreased function.
Anterior cruciate ligament (ACL) quality of life score was approximately 67 at long-term follow-up which is similar to three-year follow-up results (67) of ACL-reconstructed patients randomized to a physical therapy-supervised rehabilitation protocol versus a home-based program [8].
There are several limitations to this study. A recruitment bias may have been present since 72 of the patients with current contact information did not respond to our request. In addition, 33 patients that were contacted opted not to participate in the study. Therefore, study participants that did consent to the study may have had more favourable outcomes than those that did not. Subjective outcome scores used in this study have all been validated; however, the validity and reliability of these outcome measures was determined at a shorter time of follow-up and does not necessarily ensure these scores are valid and reliable in the long term. All surgeries were performed by one surgeon, which can be interpreted as either a strength or weakness of the study.
Conclusion
To our knowledge, this is the longest follow-up reported on the largest sample size of patients that had an ACL reconstruction with a semitendinosus/gracilis autograft by a single surgeon. At a mean of 14-year post-operative, ACL-reconstructed knees demonstrated a higher incidence and severity of OA than control knees, more so in patients that also had a medial meniscus repair or excision. However, despite a higher incidence of OA on the reconstructed knee, most participants were satisfied with the surgical outcome and current quality of life. Despite harvesting semitendinosus/gracilis tendons, knee flexor strength was not compromised and participants remained active. The higher incidence of OA in the reconstructed knee is cause for concern and should be investigated further to determine when this sequelae of events is initiated, and whether it can be prevented.
References
Ahn JH, Kim JG, Wang JH, Jung CH, Lim HC (2012) Long-term results of anterior cruciate ligament reconstruction using bone-patellar tendon-bone: an analysis of the factors affecting the development of osteoarthritis. Arthroscopy 28:1114–1123
Almqvist KF, Willaert P, Brabandere S, Criel K, Verdonk R (2009) A long-term study of anterior cruciate ligament allograft reconstruction. Knee Surg Sports Traumatol Arthrosc 17:818–822
Arneja S, Leith J (2009) Review article: validity of the KT-1000 knee ligament arthrometer. J Orthop Surg (Hong Kong) 17:77–79
Asik M, Sen C, Tuncay I, Erdil M, Avci C, Taser OF (2007) The mid- to long-term results of the anterior cruciate ligament reconstruction with hamstring tendons using Transfix technique. Knee Surg Sports Traumatol Arthrosc 15:965–972
Benjaminse A, Gokeler A, van der Schans CP (2006) Clinical diagnosis of an anterior cruciate ligament rupture: a meta-analysis. J Orthop Sports Phys Ther 36:267–288
Eitzen I, Holm I, Risberg MA (2009) Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J of Sports Med 43:371–376
Fu FH, Bennett CH, Ma CB, Menetrey J, Lattermann C (2000) Current trends in anterior cruciate ligament reconstruction. Part II. Operative procedures and clinical correlations. Am J Sports Med 28:124–130
Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ (2000) Joint injury in young adults and risk for subsequent knee and hip osteoarthritis. Ann Intern Med 133:321–328
Gerhard P, Bolt R, Dück K, Mayer R, Friederich NF, Hirschmann MT (2012) Long-term results of arthroscopically assisted anatomical single-bundle anterior cruciate ligament reconstruction using patellar tendon autograft: are there any predictors for the development of osteoarthritis? Knee Surg Sports Traumatol Arthrosc [Epub ahead of print]
Grant JA, Mohtadi NGH (2010) Two- to 4-year follow-up to a comparison of home versus physical therapy-supervised rehabilitation programs after anterior cruciate ligament reconstruction. Am J Sports Med 38:1389–1394
Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, Garrett WE, Garrick JG, Hewett TE, Huston L, Ireland ML, Johnson RJ, Kibler WB, Lephart S, Lewis JL, Lindenfeld TN, Mandelbaum BR, Marchak P, Teitz CC, Wojtys EM (2000) Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg 8:141–150
Hart AJ, Buscombe J, Malone A, Dowd GSE (2005) Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament: a study using single-photon emission computed tomography at ten years. J Bone Joint Surg Br 87:1483–1487
Hertel P, Behrend H, Cierpinski T, Musahl V, Widjaja G (2005) ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg Sports Traumatol Arthrosc 13:248–255
Hinterwimmer S, Engelschalk M, Sauerland S, Eitel F, Mutschler W (2003) Operative or conservative treatment of anterior cruciate ligament rupture: a systematic review of the literature. Unfallchirurg 106:374–379
Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS (2008) Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc 16:442–448
Kostogiannis I, Ageberg E, Neuman P, Dahlberg L, Fridén T, Roos H (2007) Activity level and subjective knee function 15 years after anterior cruciate ligament injury: a prospective, longitudinal study of nonreconstructed patients. Am J Sports Med 35:1135–1143
Lautamies R, Harilainen A, Kettunen J, Sandelin J, Kujala UM (2008) Isokinetic quadriceps and hamstring muscle strength and knee function 5 years after anterior cruciate ligament reconstruction: comparison between bone-patellar tendon-bone and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc 16:1009–1016
Leys T, Salmon L, Waller A, Linklater J, Pinczewski L (2011) Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J of Sports Med 40:595–605
Lidén M, Ejerhed L, Sernert N, Laxdal G, Kartus J (2007) Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med 35:740–748
Lidén M, Sernert N, Rostgard-Christensen L, Kartus C, Ejerhed L (2008) Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autografts: a retrospective, 7-year radiographic and clinical follow-up study. Arthroscopy: J Arthrosc Relat Surg 24:899–908
Lohmander LS, Englund PM, Dahl LL, Roos EM (2007) The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 35:1756–1769
Louboutin H, Debarge R, Richou J, Selmi TA, Donell ST, Neyret P, Dubrana F (2009) Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee 16:239–244
Mascarenhas R, MacDonald PB (2008) Anterior cruciate ligament reconstruction: a look at prosthetics–past, present and possible future. Mcgill J Med 11:29–37
Melton JTK, Murray JR, Karim A, Pandit H, Wandless F, Thomas NP (2011) Meniscal repair in anterior cruciate ligament reconstruction: a long-term outcome study. Knee Surg Sports Traumatol Arthrosc 19:1729-34
Meunier A, Odensten M, Good L (2007) Long-term results after primary repair or non-surgical treatment of anterior cruciate ligament rupture: a randomized study with a 15-year follow-up. Scand J Med Sci Sports 17:230–237
Mihelic R, Jurdana H, Jotanovic Z, Madjarevic T, Tudor A (2011) Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17–20 years. Int Orthop 35:1093–1097
Mohtadi N (1998) Development and validation of the quality of life outcome measure (questionnaire) for chronic anterior cruciate ligament deficiency. Am J Sports Med 26:350–359
Möller E, Weidenhielm L, Werner S (2009) Outcome and knee-related quality of life after anterior cruciate ligament reconstruction: a long-term follow-up. Knee Surg Sports Traumatol Arthrosc 17:786–794
Nakata K, Shino K, Horibe S, Tanaka Y, Toritsuka Y, Nakamura N, Koyanagi M, Yoshikawa H (2008) Arthroscopic anterior cruciate ligament reconstruction using fresh-frozen bone plug-free allogeneic tendons: 10-year follow-up. J Arthroscop Relat Surg 24:285–291
Neuman P, Englund M, Kostogiannis I, Friden T, Roos H, Dahlberg LE (2008) Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury: a prospective cohort study. Am J Sports Med 36:1717–1725
Neuman P, Kostogiannis I, Fridén T, Roos H, Dahlberg LE, Englund M (2010) Knee laxity after complete anterior cruciate ligament tear: a prospective study over 15 years. Scand J Med Sci Sports 22:156–63
Pernin J, Verdonk P, Si Selmi TA, Massin P, Neyret P (2010) Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med 38:1094–1102
Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M (2005) A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med 33:1337–1345
Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K (2011) Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: an 11-year follow-up of a randomized controlled trial. Am J Sports Med 39:2161–2169
Struewer J, Frangen TM, Ishaque B, Bliemel C, Efe T, Ruchholtz S, Ziring E (2011) Knee function and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft: long-term follow-up. Int Orthop 36:171–177
Selmi TA, Fithian D, Neyret P (2006) The evolution of osteoarthritis in 103 patients with ACL reconstruction at 17 years follow-up. Knee 13:353–358
Tayton E, Verma R, Higgins B, Gosal H (2009) A correlation of time with meniscal tears in anterior cruciate ligament deficiency: stratifying the risk of surgical delay. Knee Surg Sports Traumatol Arthrosc 17:30–34
Wipfler B, Donner S, Zechmann CM, Springer J, Siebold R, Paessler HH (2011) Anterior cruciate ligament reconstruction using patellar tendon versus hamstring tendon: a prospective comparative study with 9-year follow-up. Arthroscopy 27:653–665
Yamaguchi S, Sasho T, Tsuchiya A, Wada Y, Moriya H (2006) Long term results of anterior cruciate ligament reconstruction with iliotibial tract: 6-, 13-, and 24-year longitudinal follow-up. Knee Surg Sports Traumatol Arthrosc 14:1094–1100
Zaffagnini S, Bruni D, Marcheggiani Muccioli GM, Bonanzinga T, Lopomo N, Bignozzi S, Marcacci M (2011) Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc 19:390–397
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leiter, J.R.S., Gourlay, R., McRae, S. et al. Long-term follow-up of ACL reconstruction with hamstring autograft. Knee Surg Sports Traumatol Arthrosc 22, 1061–1069 (2014). https://doi.org/10.1007/s00167-013-2466-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-013-2466-3