Abstract
Purpose
To determine whether there was an association between adjunctive therapy with IgM-enriched immunoglobulin (IgM) and the 30-day mortality rate in patients with septic shock.
Methods
In 2008 we introduced IgM as a possible adjunctive therapy to be provided within 24 h after shock onset in the management protocol for patients with septic shock. In this retrospective study we included the adult patients suitable for IgM therapy admitted to our ICU from January 2008 to December 2011. An unadjusted comparison between patients who did or did not receive IgM therapy, a multivariate logistic model adjusted for confounders and propensity score-based matching were used to evaluate the association between early IgM treatment and mortality.
Results
One hundred and sixty-eight patients were included in the study. Of these, 92 (54.8 %) received IgM therapy. Patients who did or did not receive IgM were similar with regards to infection characteristics, severity scores and sepsis treatment bundle compliance. Patients who received IgM were more likely to have blood cultures before antibiotics and to attain a plateau inspiratory pressure less than 30 cmH2O (p < 0.05). The 30-day mortality rate was reduced by 21.1 % (p < 0.05) in the group that received IgM compared to the group that did not. The multivariate adjusted regression model (OR 0.17; CI 95 % 0.06–0.49; p = 0.001) and the propensity score-based analysis (OR 0.35; CI 95 % 0.14–0.85; p = 0.021) confirmed that IgM therapy was associated with reduced mortality at 30 days after the onset of septic shock.
Conclusions
Our experience indicates that early adjunctive treatment with IgM may be associated with a survival benefit in patients with septic shock. However, additional studies are needed to better evaluate the role of IgM therapy in the early phases of septic shock.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite recent advances concerning the pathophysiological mechanisms of sepsis and treatment options, mortality rates in patients admitted to the intensive care unit (ICU) with septic shock remain high [1]. The high mortality rate is attributable to several factors including challenges with early identification of severe sepsis symptoms, limited resources and incorrectly applied treatment guidelines [2, 3]. The use of sepsis treatment bundles has been consistently associated with improved patient outcome. However, it is not clear whether the success of sepsis treatment bundles is due to individual elements of the bundle or to synergistic effects of the bundle as a whole [4].
In addition to standard sepsis bundles, novel therapies have been tested for patients with severe sepsis and septic shock [5]. Immunoglobulin (Ig) preparations are a promising treatment option owing to their pleiotropic effects on bacteria and the host response to infection. The mechanism of action for Ig therapy is likely multifaceted and could include direct antibacterial and anti-endotoxin activities; reducing the expression of inflammatory mediators or directly scavenging these molecules; and other complex immunomodulatory effects [6]. Clinically, the serum Ig concentrations are generally low in patients with septic shock, and the level and kinetics of serum Ig are related to patient outcome [7, 8].
Despite the promise of Ig therapy, the recent revision of the Surviving Sepsis Guidelines [3] does not suggest using intravenous Ig in adults with severe sepsis or septic shock, because the only randomised trial with an adequate sample size found no benefit to the 28-day mortality rate after adjunctive therapy with polyclonal IgG [9]. However, several meta-analyses suggest that adjunctive treatment with intravenous Ig, particularly IgM preparations, could have beneficial effects for patients with severe sepsis, but the evidence remains insufficient to be conclusive [10–13].
In 2004, we started an in-hospital stewardship sepsis program to improve the treatment of patients with severe sepsis [14]. The program included a systematic review of the clinical protocols for diagnosing and treating septic patients. In 2008, on the basis of published meta-analyses [10–13], we began treating patients with septic shock using IgM preparations as possible adjunctive therapy within 24 h of the onset of shock.
The purpose of the current retrospective cohort analysis was to determine whether early treatment with IgM as an adjunctive therapy to evidence-based treatment affected the 30-day mortality rate of patients with septic shock. We hypothesised that patients treated with IgM in conjunction with standard sepsis bundles would have a lower mortality rate than patients treated only with the sepsis bundles.
Subjects and methods
Study Population
This retrospective cohort study included all adult patients with septic shock (n = 246) admitted to the ICU of Modena University Hospital from January 2008 to December 2011. Septic shock was defined using the International Sepsis Definitions Conference criteria [15]: (a) documented or suspected infection; (b) two or more systemic inflammatory syndrome criteria (e.g. body temperature greater than 38 °C or less than 36 °C; tachycardia, tachypnoea, leukocytosis or leukopenia; (c) systolic arterial pressure less than 90 mmHg or mean arterial pressure (MAP) less than 60 mmHg despite adequate fluid resuscitation (infusion of more than 20 mL/kg of crystalloids or synthetic colloids) and (d) signs of tissue hypoperfusion (e.g. oliguria, acidosis or worsening of mental status). Patients less than 18 years of age with end-stage liver disease, do-not-resuscitate orders or end-of-life decisions during the ICU stay were excluded from the study. This study was reviewed and approved by the ethics committee of Modena (n°251/12, approved 4 September 2013). Because the study was retrospective and did not require any active intervention apart from standard medical care, the ethics committee deemed informed consent unnecessary.
Treatment protocol
A sepsis stewardship program (SSP) has been active since 2004 in our hospital coordinated by the “Soppravvivere alla Sepsi” group [14]. The SSP continuously educates the healthcare staff, systematically revises and promotes local protocols for managing patients with severe sepsis and septic shock, and provides a biannual analysis of the SSP results. During the study period (2008–2011), the standard ICU treatment protocol for patients with septic shock did not change. The standard of care is a combination of five resuscitation interventions (6-h bundles) and four management interventions (24-h bundles). The components of the 6-h bundles included collecting blood cultures before administering antibiotics, adequate empirically based antibiotic therapy within 3 h of diagnosis, controlling the source of the infection within 6 h, adequate fluid resuscitation before administering vasopressors, and attaining a central venous oxygen saturation (ScvO2) above 70 % within 6 h. The 24-h bundles included attaining a median glucose concentration of less than 150 mg/dL in the first 24 h, administering low dose hydrocortisone to patients on vasopressor support, reaching a plateau inspiratory pressure below 30 cmH2O in patients with acute lung injury/adult respiratory distress syndrome (ALI/ARDS), and administering recombinant human activated protein C (rhAPC) when indicated. Adequate empirically based antibiotic therapy is defined as the use of appropriate targeted antibiotics in patients with an infection caused by an identified microorganism or the use of broad-spectrum antibiotics in patients where the microorganism was not identifiable. The term adequate fluid resuscitation indicated a central venous pressure greater than 6 or greater than 8 mmHg if the patient was mechanically ventilated, or a global end-diastolic volume by transpulmonary thermodilution (PiCCO system, Pulsion, Germany) greater than 700 mL/m2. Cristalloid and 20 % albumin (when serum albumin level was less than 2.0 g/dL) solutions were used for fluid resuscitation. All of the patients received noradrenaline as vasopressor therapy, and dobutamine or levosimendan as inotropic drug when indicated. IgM was administered within 24 h of the onset of shock, as a part of the 24-h bundles, and was administered at the discretion of the attending physician on the basis of personal scientific opinion. All of the ICU medical staff (eight intensivists) participated in a 4-h meeting regarding the scientific rationale for early administration of IgM in septic shock patients in 2007. The frequency of IgM administration was audited yearly by the ICU staff during the study period. When IgM was prescribed, it was administered through a dedicated intravenous line at a dosage of 250 mg/kg per day (20 mg/kg/h) for three consecutive days [16, 17].
Data collection
Two of the authors (C.I. and S.G), who were not involved in the management of the patients, collected information from the clinical charts pertaining to the use of each standard sepsis bundle (6 and 24 h) and IgM administration. Any data that was unclear was audited by the attending physician. The interventions were classified as completed and not completed. An intervention that was not applicable to an individual patient (e.g. low plateau inspiratory pressure in a patient without ALI/ARDS) was reported as completed. Time zero for the bundles was defined as the time at which the study inclusion criteria were documented in the clinical notes. The type of admission, relevant pre-existing diseases (i.e. heart failure, chronic obstructive pulmonary disease, end-stage renal disease and history of cancer), the primary site of infection, microbiology lab results, SAPS II and SOFA scores when sepsis was diagnosed [18, 19], the use of inotropic drugs, duration of vasopressor administration and mechanical ventilation, adverse events possibly related to IgM therapy (e.g. anaphylactic reaction, severe hypotension and exanthema), the length of stay in the ICU and 30-day mortality rate were recorded for each patient. Patients discharged to home within 30 days of septic shock occurring were considered survivors. Multidrug-resistant bacteria were defined as previously described by Magiorakos et al. [20].
Statistical analysis
The patients that received adjunctive IgM therapy were compared to the patients that did not receive IgM. Differences between the groups were assessed using the Mann–Whitney U or Fisher’s exact test, as applicable. The 30-day mortality rate was compared between the two groups using Kaplan–Meier curves and log-rank tests. To estimate the association between IgM therapy and the 30-day mortality rate, univariate unadjusted analysis, multivariate logistic regression modelling and propensity score-based matching were used. IgM therapy and variables that differed (α level less than 0.1) between patients who were or were not treated with IgM therapy were included as independent covariates in the multivariate regression model. Variables for which a biological effect was highly likely (age, type of admission, pre-existing diseases, site of infection, infection by multidrug-resistant bacteria, and SOFA and SAPS II scores) were also included in the model.
A propensity score was also established using the following covariates: age, year of admission, type of admission, primary site of infection, pre-existing diseases, SOFA and SAPS II score, and 6- or 24-h bundle compliance. This score was then used to match patients with and without IgM treatment. For the matching process, 1:1 matching (5 → 1 digit) was used with no replacements for previously matched patients allowed [21]. The 30-day mortality rate was then compared between patients who received IgM and patients who did not receive IgM using a logistic regression model stratified to matched pairs.
P < 0.05 was considered significant. The goodness of fit was assessed by the Hosmer–Lemeshow test. The statistical software package SPSS version 20.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
Results
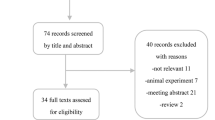
During the study period, 246 patients with septic shock were admitted to the ICU. Twenty-nine patients with do-not-resuscitate orders or end-of-life decisions and 49 patients with end-stage liver disease were excluded from the study. The lung and abdominal cavities were the most common infection sites, and gram-negative bacterial infections were the cause of shock in the majority of our patients (Table 1). Each individual intervention in the management protocol was completed in at least 70 % of patients, except optimising ScvO2 within 6 h, which was only achieved in 49 % of patients. Ninety-two patients (54.8 %) received IgM therapy and all patients completed the 3 days of IgM preparation. All of the patients who received IgM therapy were treated within 24 h of the onset of shock. There were no adverse events attributable to IgM treatment identified.
Patients treated with IgM were similar to patients who did not receive IgM with regards to age, sex, type of admission, pre-existing diseases, primary site of infection, the type of microorganisms identified, SOFA score and treatments provided. However, the patients that received IgM had a greater percentage of unidentified microorganisms (p > 0.05), significantly higher SAPS II (p < 0.05), were more likely to have their blood collected for culture before receiving antibiotic therapy (p < 0.05), and in patients with ALI/ARDS, the plateau inspiratory pressure less than 30 cmH2O was more frequently completed (p < 0.05) than the patients that did not receive IgM (Table 1). The 30-day mortality rate was reduced by 21.1 % in the patients that received IgM compared to the patients who did not receive IgM (Fig. 1). The causes of death were refractory shock in 15 patients (five in the IgM group), multiple organ dysfunction in 38 patients (16 in the IgM group) and other causes such as myocardial infarction and major bleeding in five patients (two in the IgM group). The unadjusted regression analysis indicated that the presence of pre-existing diseases, pneumonia as the site of infection, SAPS II and SOFA scores, compliance with the 24-h bundle, empirically based antibiotic therapy within 3 h of diagnosis, a median glucose concentration less than 150 mg/dL in the first 24 h, receiving rhAPC when indicated and IgM treatment were significantly associated (p < 0.05) with the 30-day mortality rate. The multivariate adjusted analysis confirmed that IgM treatment was associated with a reduced probability of death 30 days after the onset of septic shock (Table 2). The median values of free days from mechanical ventilation and ICU stay in the 30 days after shock onset were slightly larger (p > 0.05) in patients treated than in patients not treated with IgM (Table 2).
One hundred and eighteen of the 168 study patients (70 %) were included in the propensity score-based analysis (IgM, n = 59; no IgM, n = 59), all of the variables were balanced after 1:1 matching between the groups. In the propensity score-based analysis, the 30-day mortality rate (25.4 % vs 45.8 %; OR 0.35; CI 95 % 0.14–0.85; p = 0.021) was significantly different between patients who were or were not treated with IgM therapy (Table 3).
Discussion
This study was a retrospective cohort study assessing the efficacy of adjunctive therapy with IgM for reducing the 30-day mortality rate of patients with septic shock. IgM administration within 24 h of the onset of shock, in conjunction with the standard of care recommended by evidence-based guidelines, appears to be safe and may improve patient survival.
For over 20 years, Ig has been used as adjunctive therapy in patients with sepsis despite the lack of robust evidence of its efficacy [10, 22]. Ig has many immunomodulatory effects including neutralising endotoxins, stimulating opsonic and bactericidal activity, reducing pro-inflammatory mediators and increasing anti-inflammatory mediators [6]. Moreover, patients with hypogammaglobulinemia have a high incidence of infections, and a high proportion of patients with severe sepsis and septic shock have low serum levels of Ig, which seems to be associated with a significantly higher mortality rate [7–23]. However, it is not clear whether patients with sepsis and hypogammaglobulinemia would benefit from the administration of Ig at the currently recommended doses. A recent multicentre observational study by the Hellenic Sepsis Study Group demonstrated that a significant decrease in IgM serum concentrations occurs when severe sepsis progresses to septic shock, and that IgM distribution over time is lower in patients who do not survive [8].
Recently published reviews and meta-analyses are based on small, outdated, heterogeneous, randomised studies; however, they suggested that patients with severe sepsis may have a lower mortality rate after treatment with IgM rather than standard polyclonal Ig [12, 24]. In contrast, the only large (n = 653) randomised trial to treat patients with severe sepsis with adjunctive polyclonal IgG did not show an effect on the 28-day mortality rate [9]. The difference between IgM and standard polyclonal IgG could stem from intrinsic factors, such as IgM polyreactivity, IgM more rapidly activates complement to neutralise bacteria, or the higher titre of bacteria-reactive antibodies in IgM preparations that recognize a broad spectrum of bacterial pathogens [25–27]. The capacity of IgM to facilitate the removal of apoptotic cells also seems to have an important role in modulating the immune response during sepsis, and in facilitating the resolution of inflammation [26]. In animal models, impaired microcirculatory perfusion during sepsis is attenuated more by the use of IgM than IgG, and an infusion of IgM protects the lungs from histological changes that occur during endotoxemia [28, 29]. In septic patients, IgM therapy also seems to have a positive effect on muscular microcirculation when used early after the onset of shock [30]. However, a recent meta-analysis of randomised control trials using Ig to treat adults with severe sepsis demonstrated that when measures of study quality (e.g. choice of control) and dosing regimen (e.g. duration of Ig therapy) were considered, all-cause mortality was not reduced with IgM compared to standard polyclonal Ig [22].
The reduced 30-day mortality rate in our study following treatment with IgM is consistent with previous clinical studies [16, 31, 32] and a recent meta-analysis [12]. In a multicentre, randomised, double blind study of patients with abdominal sepsis, Rodríguez et al. [33] observed a 25 % reduction in 30-day mortality among patients treated with appropriate antibiotic therapy and high doses of IgM or albumin. Berlot et al. [34] demonstrated in a retrospective study of 129 patients that the effectiveness of Ig depends on the time elapsed between the occurrence of sepsis and administration of the IgM preparation. This study showed that the risk of death increased by approximately 3 % for each day IgM treatment was delayed. Taken together with animal model studies [35], Berlot et al. [34] indicates that IgM treatment likely has an important role in the early stages of the inflammatory and immune response to infection. The early administration of IgM in our study, within 24 h of the onset of shock, may also explain the beneficial effects observed in our population. It must also be emphasized that this is the first study where IgM therapy was used as adjunctive therapy in patients with consistent and monitored application of evidence-based treatment guidelines [2, 3], and that this may not be the case in previous studies [16, 17, 31–33].
The primary limitations of our study are the retrospective observational design, and the limited number of patients. Although age, sex, type of admission, and pre-existing diseases were similar between patients who were and were not treated with IgM, selection bias based on the attending physician for each case cannot be excluded given the retrospective nature of the data collection. Thus, it is interesting to note that the SAPS II and SOFA scores were higher in patients who received IgM therapy. This was first observed in an internal data audit in 2009. We postulated that the medical staff was more likely to use IgM as adjunctive therapy in complicated cases given the cost of the treatment. In addition, because IgM had to be started within 24 h patients treated with IgM may have received more aggressive treatment overall, which might partially explain the better outcome. In fact, two of the nine treatments included in the 6- and 24-h bundles were more frequently completed in patients who received IgM. Finally, retrospective analysis of medical charts does not allow an accurate identification of adverse events such as anaphylaxis or hypotension, particularly in patients with multiple organ dysfunction or receiving vasopressor therapy. For these reasons, the current results should be read with care and may not be applicable to contexts other than those of the study.
Conclusions
The exact role that Ig may have in the immune and inflammatory response of patients with sepsis is still unclear. It is possible that Ig plays different roles based on the pathophysiological context of the patient, the type of Ig and the dose used. Our experience suggests that early adjunctive treatment with IgM at a dose of 250 mg/kg per day for 3 days results in an approximately 20 % reduction in the absolute risk of 30-day mortality in patients with septic shock treated according to guidelines. However, additional studies are needed to confirm these results and better evaluate the use of IgM therapy early on in patients with septic shock.
References
Sakr Y, Elia C, Mascia L, Barberis B, Cardellino S, Livigni S et al (2013) The influence of gender on the epidemiology of and outcome from severe sepsis. Crit Care 17:R502
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R et al (2008) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med 34:17–60
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM et al (2013) Surviving sepsis campaign guidelines committee including the pediatric subgroup: surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Intensive Care Med 39:165–228
Barochia AV, Cui X, Vitberg D, Suffredini AF, O’Grady NP, Banks SM et al (2010) Bundled care for septic shock: an analysis of clinical trials. Crit Care Med 38:668–678
Reinhart K, Brunkhorst FM, Bone H-G, Bardutzky J, Dempfle C-E, Forst H et al (2010) Prevention, diagnosis, therapy and follow-up care of sepsis: 1st revision of S-2 k guidelines of the German Sepsis Society [Deutsche Sepsis-Gesellschaft e.V. (DSG)] and the German Interdisciplinary Association of Intensive Care and Emergency Medicine [Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin (DIVI)]. Ger Med Sci 8
Shankar-Hari M, Spencer J, Sewell WA, Rowan KM, Singer M (2012) Bench-to-bedside review: immunoglobulin therapy for sepsis-biological plausibility from a critical care perspective. Crit Care 16:206
Taccone FS, Stordeur P, De Backer D, Creteur J, Vincent J-L (2009) Gamma-globulin levels in patients with community-acquired septic shock. Shock 32:379–385
Giamarellos-Bourboulis EJ, Apostolidou E, Lada M, Perdios I, Gatselis NK, Tsangaris I et al (2013) Kinetics of circulating immunoglobulin M in sepsis: relationship with final outcome. Crit Care 17:R247
Werdan K, Pilz G, Bujdoso O, Fraunberger P, Neeser G, Schmieder RE et al (2007) Score-based immunoglobulin therapy of sepsis (SBITS) study group. Score-based immunoglobulin G therapy of patients with sepsis: the SBITS study. Crit Care Med 35:2693–2701
Alejandria MM, Lansang MA, Dans LF, Mantaring JB 3rd (2013) Intravenous immunoglobulin for treating sepsis and septic shock. Cochrane Database Syst 9:CD001090
Turgeon AF, Hutton B, Fergusson DA, McIntyre L, Tinmouth AA, Cameron DW et al (2007) Meta-analysis: intravenous immunoglobulin in critically ill adult patients with sepsis. Ann Intern Med 146:193–203
Kreymann KG, de Heer G, Nierhaus A, Kluge S (2007) Use of polyclonal immunoglobulins as adjunctive therapy for sepsis or septic shock. Crit Care Med 35:2677–2685
Laupland KB, Kirkpatrick AW, Delaney A (2007) Polyclonal intravenous immunoglobulin for the treatment of severe sepsis and septic shock in critically ill adults: a systematic review and meta-analysis. Crit Care Med 35:2686–2692
Girardis M, Rinaldi L, Donno L, Marietta M, Codeluppi M, Marchegiano P et al (2009) Effects on management and outcome of severe sepsis and septic shock patients admitted to the intensive care unit after implementation of a sepsis program: a pilot study. Crit Care 13:R143
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D et al (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med 29:530–538
Karatzas S, Boutzouka E, Venetsanou K, Myrianthefs P, Fildisis G, Baltopoulos G (2002) The effects of IgM-enriched immunoglobulin preparations in patients with severe sepsis: another point of view. Crit Care 6:543–544
Tugrul S, Ozcan PE, Akinci O, Seyhun Y, Cagatay A, Cakar N et al (2002) The effects of IgM-enriched immunoglobulin preparations in patients with severe sepsis. Crit Care 6:357–362
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H et al (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. Intensive Care Med 22:707–710. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine
Magiorakos A-P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG et al (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18:268–281
Rosenbaum PR, Rubin DB (1985) Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat 39:33–38
Soares MO, Welton NJ, Harrison DA, Peura P, Shankar-Hari M, Harvey SE et al (2012) An evaluation of the feasibility, cost and value of information of a multicentre randomised controlled trial of intravenous immunoglobulin for sepsis (severe sepsis and septic shock): incorporating a systematic review, meta-analysis and value of information analysis. Health Technol Assess 16:1–186
Tamayo E, Fernández A, Almansa R, Carrasco E, Goncalves L, Heredia M et al (2012) Beneficial role of endogenous immunoglobulin subclasses and isotypes in septic shock. J Crit Care 27:616–622
Norrby-Teglund A, Haque KN, Hammarström L (2006) Intravenous polyclonal IgM-enriched immunoglobulin therapy in sepsis: a review of clinical efficacy in relation to microbiological aetiology and severity of sepsis. J Intern Med 260:509–516
Trautmann M, Held TK, Susa M, Karajan MA, Wulf A, Cross AS et al (1998) Bacterial lipopolysaccharide (LPS)-specific antibodies in commercial human immunoglobulin preparations: superior antibody content of an IgM-enriched product. Clin Exp Immunol 111:81–90
Ehrenstein MR, Notley CA (2010) The importance of natural IgM: scavenger, protector and regulator. Nat Rev Immunol 10:778–786
Rieben R, Roos A, Muizert Y, Tinguely C, Gerritsen AF, Daha MR (1999) Immunoglobulin M-enriched human intravenous immunoglobulin prevents complement activation in vitro and in vivo in a rat model of acute inflammation. Blood 93:942–951
Hoffman JN, Fertmann JM, Vollmar B, Laschke MW, Jauch KW, Menger MD (2008) Immunoglobulin M-enriched human intravenous immunoglobulins reduce leukocyte-endothelial cell interactions and attenuate microvascular perfusion failure in normotensive endotoxemia. Shock 29:133–139
Stehr SN, Knels L, Weissflog C, Schober J, Haufe D, Lupp A et al (2008) Effects of IGM-enriched solution on polymorphonuclear neutrophil function, bacterial clearance, and lung histology in endotoxemia. Shock 29:167–172
Cavazzutti I, Rinaldi L, Braccini S, Bertolotti V, Andreotti A, Busani S et al (2009) Effects of intravenous IgM-enriched immunoglobulins on muscle tissue microcirculation in septic shock: a preliminary report. Intensive Care Med 35:s239
Yavuz L, Aynali G, Aynali A, Alaca A, Kutuk S, Ceylan BG (2012) The effects of adjuvant immunoglobulin M-enriched immunoglobulin therapy on mortality rate and renal function in sepsis-induced multiple organ dysfunction syndrome: retrospective analysis of intensive care unit patients. J Int Med Res 40:1166–1174
Schedel I, Dreikhausen U, Nentwig B, Höckenschnieder M, Rauthmann D, Balikcioglu S et al (1991) Treatment of gram-negative septic shock with an immunoglobulin preparation: a prospective, randomized clinical trial. Crit Care Med 19:1104–1113
Rodríguez A, Rello J, Neira J, Maskin B, Ceraso D, Vasta L et al (2005) Effects of high-dose of intravenous immunoglobulin and antibiotics on survival for severe sepsis undergoing surgery. Shock 23:298–304
Berlot G, Vassallo MC, Busetto N, Bianchi M, Zornada F, Rosato I et al (2012) Relationship between the timing of administration of IgM and IgA enriched immunoglobulins in patients with severe sepsis and septic shock and the outcome: a retrospective analysis. J Crit Care 27:167–171
Jacobs S, Sobki S, Morais C, Tariq M (2002) Effect of pentaglobin and piperacillin on survival in a rat model of faecal peritonitis: importance of intervention timings. Acta Anaesthesiol Scand 44:88–95
Acknowledgments
We wish to thank Mervyn Singer and Matteo Bassetti for critical revisions of the manuscript and their clever suggestions.
Conflicts of interest
Cavazzuti Ilaria and Massimo Girardis have consulted for Biotest-Germany, the remaining authors have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: Adjunctive treatment with IgM early on resulted in a 20 % reduction of the absolute 30-day risk of mortality in patients with septic shock treated using evidence-based guidelines.
Rights and permissions
About this article
Cite this article
Cavazzuti, I., Serafini, G., Busani, S. et al. Early therapy with IgM-enriched polyclonal immunoglobulin in patients with septic shock. Intensive Care Med 40, 1888–1896 (2014). https://doi.org/10.1007/s00134-014-3474-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3474-6