Abstract
The recent guidelines on the treatment of sepsis and sepsis-related conditions, published on behalf of the “Surviving Sepsis Campaign” (SSC) [1], consider the use of intravenous immunoglobulin (IvIg) with a certain degree of ambiguity: on the one hand, a series of papers and meta-analysis that demonstrates their efficacy in terms of mortality reduction of both adult and child/infant are quoted, but on the other hand, the use of IvIg is strongly discouraged as it is considered not supported enough by studies satisfying the evidence-based medicine (EBM) requirements, that claim for randomized, controlled, double-blind, multicenter trials, involving an adequate number of patients who are subjected to the same entry criteria in terms of diagnosis and timing of the studied treatment. This ambiguity can make the clinician facing a septic patient doubt about the opportunity to use IvIg despite the vast majority of published studies reporting a better outcome in patients given IvIg. This situation is further complicated by the consideration that the number of patients involved in the studies on IvIg quoted in the SCC largely exceeds those enrolled in the investigations chosen to support the hemodynamic management of the resuscitation bundle, which basically relies on only two studies, of which one has been published in Chinese without English translation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
3.1 Introduction
The recent guidelines on the treatment of sepsis and sepsis-related conditions, published on behalf of the “Surviving Sepsis Campaign” (SSC) [1], consider the use of intravenous immunoglobulin (IvIg) with a certain degree of ambiguity: on the one hand, a series of papers and meta-analysis that demonstrates their efficacy in terms of mortality reduction of both adult and child/infant are quoted, but on the other hand, the use of IvIg is strongly discouraged as it is considered not supported enough by studies satisfying the evidence-based medicine (EBM) requirements, that claim for randomized, controlled, double-blind, multicenter trials, involving an adequate number of patients who are subjected to the same entry criteria in terms of diagnosis and timing of the studied treatment. This ambiguity can make the clinician facing a septic patient doubt about the opportunity to use IvIg despite the vast majority of published studies reporting a better outcome in patients given IvIg. This situation is further complicated by the consideration that the number of patients involved in the studies on IvIg quoted in the SCC largely exceeds those enrolled in the investigations chosen to support the hemodynamic management of the resuscitation bundle, which basically relies on only two studies, of which one has been published in Chinese without English translation.
With these limitations in mind, it must be admitted that, in the everyday practice, we still lack a method able to identify the patients in which the administration of IvIg can represent a precise therapeutic choice, comparable, for example, to measurement of cardiac enzymes for the primary angioplasty in acute myocardial infarction.
Several causes can account for this lack of certainty deriving from the published studies, including:
-
(a)
The use of IvIg preparation containing different classes of Ig: actually, the biological characteristics of each of them and the chemical reactions with different antigens which they are directed against make impossible to compare their effect and can justify the somehow conflicting results deriving from studies in which different preparations have been used.
-
(b)
The heterogeneity of the treated patients, in terms of causes of sepsis (e.g., surgery or medical), age (adults vs. infants and/or pediatrics), and concomitant diseases (e.g., burns, cancer, etc.).
-
(c)
The absence of cheap and immediately available laboratory tests that could indicate whether the administration of IvIg is warranted
-
(d)
The uncertain relationship between the timing of IvIg administration and the onset of sepsis: it is likely that, likewise antibiotics, their use is more effective in the initial stage of sepsis than in the more advanced ones, where a full-blown multiorgan dysfunction syndrome (MODS) is established. Conversely, an indiscriminate treatment extended also to patients with less severe conditions who do not really need them could elevate costs without gaining any benefit. In both conditions, the informations derived from their use are hard to understand.
Then it is clear how that, independently from the SCC recommendations, several factors contribute to confound the clinician that considers IvIg as a reasonable therapeutic option. This can determine either an unjustified negative attitude toward substances that can be considered as drugs and biological agent in the same time, or, conversely, the choice to treat all patients with expensive medication whose use could be reserved to more severe cases.
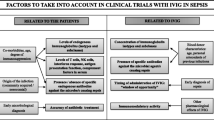
The final aim of this chapter is to give some useful indications to the practitioner facing a patient with severe sepsis and/or septic shock in order to identify the circumstances in which the maximum advantage of administration of IvIg can be expected.
3.2 Structure and Biologic Role of Ig
Before examining the issues related to the clinical use of IvIg, it is necessary to consider some basic concepts in order to show how the host reacts to an infection.
Briefly, the immune system has been developed during the evolution to recognize and neutralize the extraneous substances invading the organism [2, 3].
The reaction is based on two different but strictly related systems:
-
(a)
The natural immunity, mostly based on the cells belonging to the reticuloendothelial system (SRE) cells, on the SRE-produced mediators, and on the complement system: in functional terms, the natural immunity is a fast-reacting and is an unspecific system which is immediately available and does not require any sophisticated procedure for the recognition of extraneous substances.
In an immunological mature and competent organism, the natural immunity acts concomitantly with:
-
(b)
The adaptive immunity, which is based on the production of immunoglobulins by the plasma cells, which, in turn, are obtained by the exposure of B lymphocytes to the antigens (Ag) moving and localized on the immune cells surface under the stimulus provided by the T lymphocytes belonging to the CD4 class. In evolutionary terms, it can be supposed that the adaptive immunity has evolved since the number of the receptors on the SRE cells that form the natural immunity is genetically limited and, regardless of its relevancy, it is not able to recognize all the extraneous molecules which could interact with the organism throughout its life span.
Depending on their chemical and physical characteristics and the dimensions, geometric shape, and their antigen-binding capabilities, the molecules of Ig can be subdivided in five classes (G, A, M, D, E) (Fig. 3.1).
The G class is considered prototypical and is formed by two heavy chains (H) with variable weight between 50 and 70 kDa and two light chains (L) weighing around 20–25 kDa (Fig. 3.2). Electrostatic bonds and bisulphurate bridges keep the single chains together.
Schematic two-dimensional structure of an IgG molecule. VH and VL indicate the variable regions of the heavy and light chains, respectively. The different epitopes are recognized by the variable regions located on both the light and heavy chains (Fab region). The CDR segments are hypervariable domains located in the Fab regions, which are separated from each other by relatively constant polypeptide chains. The Fc region binds to the complement and to the receptors located on the surface of the RES cells and triggers their activation
Both chains have a variable (V) region which interacts with the antigen and a constant one (C) which activates the immune system functions like the complement system, the phagocytosis, the cell’s mediated lysis, etc.
The interconnection region between V and C components undergoes three-dimensional arrangements in order to adapt its structure to the Ag surface. Each variable region is formed by other three hypervariable subregions where their shape defines the specificity of the molecule. Both variable and fixed regions on the chains L and H are arranged on of Fab region, which binds the Ag.
In general terms, the Ig molecules can be considered biochemical transducers able to (Table 3.1):
-
Recognize and neutralize infective germs and their derived substances
-
Opsonize extraneous molecules in order to facilitate their elimination by the reticulum-endothelial system
-
Recognize and inhibit early and late-released sepsis mediators, by a direct effect on the cell nucleus which produces and facilitates their scavenging by the SREs
-
Activate the complement system
-
Influence the death of the immunitary cells via apoptotoc and non-apoptotic pathways
Then, it appears that the Ig can modulate the inflammatory response, and this capability can be useful in the different phases of sepsis, which are characterized by a different arrangement of the immune response. Actually, sepsis and its related conditions as severe sepsis and septic shock can be considered as a complex and articulated response to an infection, which is characterized by (at least) two different phases. In the first one, whose features are the classical signs of fever, leucocytosis, hemodynamic instability, metabolic acidosis, etc., there is a predominant secretion of proinflammatory mediators (TNF, various interleukins, etc.) that can cause the derangement of organs different from the one in which the infective process and immunity response have started. This reaction is mainly determined by the action of the indicated proinflammatory mediators, whose qualitative and quantitative properties are genetically determined and thus vary from an individual to another; the subsiding of this initial response is determined either by reduction of the production of proinflammatory substances and by the contemporaneal release of mediators with anti-inflammatory capabilities [3].
If the patient survive the initial insult, a second phase ensues, which is characterized by the reduction and progressive disappearance of the above described proinflammatory response due to the overwhelming action of anti-inflammatory mediators ultimately leading to a state of immunoparalysis; this condition is characterized by a profound alteration of both natural and adaptive immunity mechanism, and the consequent immunitary state can be compared to that present in advanced neoplastic conditions [4, 5]. This state, which is difficult to diagnose due to the lack of suitable biological markers, is particularly frequent in patients affected by multiple chronic conditions, who can survive the infection and/or its related conditions causing the intensive care unit admission (surgery, lung infection, etc.) but who cannot be weaned from the mechanical ventilation and are prone to multiple infections, thus becoming critically ill chronic patients.
The above described clinical aspects can justify the use of IvIg both in the early phase of sepsis, in which they can modulate an excessive systemic inflammatory response, and in the more advanced phase, during which their antibacterial action can restore the adaptive immune response. These actions are only partly shared by other immunomodulatory substances recommended by the SSC guidelines, like steroids with glucocorticoid activity: indeed, if their use has a rationale in the early inflammatory phase, in the later one, their use can contribute at the occurrence of immunoparalysis. Anyhow, the use of IvIg does not replace the other therapies indicated by the SSC, including the early administration of appropriate antibiotics and the surgical drainage of infective sources. Even if it is probable that in the next future some other immunomodulatory and immunostimolatory molecules can be introduced in clinical practice, actually their application has to be considered only experimental.
3.3 The Administration of IvIg in Sepsis
Although the IvIg use has long anticipated the first edition of the SSC, their administration in septic patients has been initiated long before and was based for long time more on the intuition of their utility than on robust scientific bases. In general, the different IvIg preparation currently used in clinical practice can be divided into two principal categories. The first one is formed by monoclonal antibodies directed versus one single antigen (e.g., the antitetanic toxin Ig), and the other is compounded by polyclonal antibodies directed against different antigens.
On the other hand, the application’s modality in the sepsis treatment is based essentially on two different strategies [6]:
-
(a)
The administration of polyclonal antibodies directed versus Ag expressed on the surface of the infection responsible bacteria and/or versus bacteria’s produced substances like endotoxin, peptidoglycans, etc., that are released when the antibiotics cause cellular lysis; the IvIg actually in use belongs from this category, and it is composed by mixtures of IgG, IgM, and IgA in concentrations different than in plasma (Table 3.2). Independently of single composition, the IvIg solutions derive from a plasma pool of 1.000–10.000 donators and so contain a great variety of antibodies directed versus a myriad of different antigens that can vary with the different geographic donator origins and with their exposure on different antigens. The main preparation’s process consists on the extraction and cold fractionation in ethanol, instead, whereas the inactivation of any blood donator virus involves the use of solvents, detergents, the pH reduction to 4, the incubation, the nanofiltration, and the chromatography
Table 3.2 Concentrations of the different classes of IgG in the available preparations -
(b)
The administration of monoclonal antibodies in order to neutralize a single mediator that is produced and released from different immune system cells during the interaction between the bacteria and the host or, alternatively, versus its receptors on the target cells. Even though this strategy is based on clear pathophysiological and experimental assumptions, a wide number of clinical trials conducted with antibodies directed against different sepsis mediators (tumor necrosis factor, platelet-activating factor, etc.) carried results largely inferior to the expectations so that no one of this substances is used for the treatment of septic patients [7]. The causes of these results are not clear; it is likely, however, that the antagonism of only one of the many mediators that are released during sepsis and that are connected to each other with numerous negative or positive feedback cannot be sufficient per se to reduce the systemic inflammation process typical of the early phase of sepsis. Moreover, as the production of septic mediators is genetically determinate, the administration of a specific Ig directed versus one determinate molecule does not take into account this peculiarity. Anyway, these substances find extensive application in treatment of diseases characterized by chronic and/or relapsing inflammation state (e.g., rheumatoid arthritis, Crohn’s disease, etc.).
Currently, only preparations containing polyclonal antibodies belonging from the IgG, IgM, and IgA classes are clinically used in the treatment of sepsis. The rationale for their use, as well as the pathophysiological premises exposed before, is based on the results of different studies and meta-analysis that have demonstrated that (a) the administration of polyclonal IvIg is associated with the reduction of mortality in different populations of septic patients [8–11] and that (b) the preparations containing IgM are more effective as compared with those containing IgG [12–15]. These results cannot be applied to all septic patients, because other studies have demonstrated that the IvIg administration does not improve the surviving of neutropenic patients and/or patients with hematology malignancy [16, 17]. The skepticism expressed by the SSC guidelines is principally derived from a number of causes, including the relatively poor number of patients enrolled in each single study, the heterogeneity of the underlying clinical conditions, the difference in pharmacological preparation used, and the different IvIg doses used [1, 14].
3.4 The Choice of the Patient
According to the authors of the SSC guidelines, the administration of IvIg cannot be recommended mainly due to lack of EBM criteria in the published studies and the consequent difficult identification of one or more categories of septic patients who likely could take advantage from their use. Presently, as stated above, this treatment is based more on the experience of the single centers than on sound biological and/or pathophysiological criteria, leaving a great probability of subjective decisions. The lack of precise indications is a relevant clinical issue as this relatively expensive treatment should be reserved to patients who could take maximum benefit from it, thus maximizing the risk/benefit ratio; despite the lack of a biological or clinical marker (as troponin in the case of ischemic cardiopathy) that can be suited to start and/or to continue for the administration of IvIg, it is possible to present some findings derived from different studies that could be considered as a possible starting point for the identification of the patient in which the treatment is effective:
-
(a)
In a group of patients with severe sepsis or septic shock, Maury et al. have demonstrated that the most elevated spontaneous IgM concentration has associated with a better outcome [18].
-
(b)
Reduced spontaneous anti-endotoxin IgM antibodies concentration was associated with the increase in number of infective complications in a group of cardio-surgery patients [19].
-
(c)
In septic shock patients, Venet et al. have demonstrated that the IgM and IgG concentrations were decreased at the beginning but increased in the following days [20]; the reduction of both classes was more nonsignificantly more pronounced in dead patients.
-
(d)
Conversely, in another study, plasmatic IgM levels in patients with septic shock were significantly lower than in patients with systemic inflammatory response syndrome or severe sepsis; the IgM concentrations gradually increased in the survivor patients, whereas in nonsurvivors, they remained unchanged or decreased [21].
-
(e)
Several meta-analyses in adult, pediatric, or neonatal patients demonstrate that IgM and IgA preparation are more effective than IgG in terms of mortality reduction [12–15].
-
(f)
The IgM administration is more effective in the early phase of septic shock or severe sepsis [22], but the improvement in the clinical condition monitored with SOFA score does not increase before 48 h from the beginning of the treatment [23].
-
(g)
The administration IgM did not decrease the mortality of neutropenic patients with leukemia or lymphoma but was associated with a decreased rate of MODS [16, 17]. This observation probably reflects the impossibility to restore the immune competence by reinforcing only one arm of its components.
In conclusion, despite the caution derived from the absence of one or more biological marker to monitor the effectiveness, the ideal patient candidate to IvIg treatment could be considered as a subject with severe sepsis or septic shock of both medical and surgical origin, with at least one organ dysfunction [16], caused by either gram − and gram + germs [19], treated in the early phase of illness [22], and without advanced cancer disease or other conditions that could reduced his/her life expectation. The monitoring of plasmatic IgM and IgG concentrations could be useful to early identify the patient to treat, even if the waiting for the result should not delay the beginning of the treatment.
In order to have a more precise idea about the biological effects of the IvIg administration, it could be useful to measure repeatedly the concentration of each Ig class concentration in order to understand the causes of their variations and to identify the dose needed for every single patient [24].
3.5 Conclusions
Despite a number of experimental and clinical evidences demonstrated that the sepsis and its derived conditions are characterized in the early phases by excessive inflammatory response and in the later phases by a state of depression of both natural and adaptive response, the IvIg treatment that can modulate both conditions is often chosen on a subjective basis and not on indications derived from international guidelines that, instead, advise against this approach.
This situation derives from the lack of studies based on EBM criteria and of data about the Ig kinetics during sepsis. However, despite these relevant limitations, it is possible to identify with clinical and time criteria the kind of patient who could have their prognosis improved by the administration of IvIg.
References
Dellinger P, Levy MM, Rhodes A et al (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39:165–228
Cohen J (2002) The immunopathogenesis of sepsis. Nature 420:885–891
Hotchkiss RS, Karl IE (2003) The pathophysiology and treatment of sepsis. N Engl J Med 348:138–150
Späth PJ (1999) Structure and function of immunoglobulins. Sepsis 3:197–218
Hotchkiss RS, Monneret G, Payen D (2013) Immunosuppression in sepsis: a novel understanding of the disorder and a new therapeutic approach. Lancet Infect Dis 13:260–268
Darabi K, Abdel-Wahab O, Dzik WH (2006) Current usage of intravenous immune globulins and the rationale behind it. The Massachusetts General Hospital data and a review of the literature. Transfusion 47:741–753
Deans KJ, Haley M, Natanson C et al (2005) Novel therapies for sepsis: a review. J Trauma 58:867–874
Rodriguez A, Rello J, Neira J et al (2005) Effects of intravenous immunoglobulin and antibiotics on survival for severe sepsis undergoing surgery. Shock 23:298–304
Dominioni L, Dionigi R, Zanello M et al (1991) Effects of high-dose IgG on survival of surgical patients with sepsis score of 20 or greater. Arch Surg 126:236–240
Cafiero F, Gipponi M, Bonalimi U et al (1992) Prophylaxis of infection with intravenous immunoglobulins plus antibiotics for patients at risk for sepsis undergoing surgery for colorectal cancer: results of a randomized, multicentre clinical trial. Surgery 112:24–31
Schedel I, Dreikhausen U, Newtig B et al (1991) Treatment of gram negative septic shock with immunoglobulin preparation: a prospective, randomized clinical trial. Crit Care Med 19:1104–1113
Alejandra MM, Lansang MA, Dans LF et al (2002) Intravenous immunoglobulin for treating sepsis an septic shock. Cochrane Database Syst Rev (1):CD001090
Turgeon AF, Hutton B, Fergusson DA et al (2007) Meta-analysis: intravenous immunoglobulin in critically ill adult patients with sepsis. Ann Intern Med 146:193–203
Pildal J, Goetzshe PC (2004) Polyclonal immunoglobulins for the treatment of bacterial sepsis: a systematic review. Clin Infect Dis 39:38–46
Norby-Teglund A, Haque KN, Hammarström L (2006) Intravenous polyclonal IgM-enriched immunoglobulin therapy in sepsis: a review of clinical efficacy in relation to microbiological aetiology and severity of sepsis. J Intern Med 260:509–516
Hentrich M, Fehnle M, Ostermann H et al (2006) IgMA-enriched immunoglobulin in neutropenic patients with sepsis syndrome and septic shock: a randomized, controlled multiple-center trial. Crit Care Med 34:1319–1325
Tugrul S, Ozoan PE, Akinci O et al (2002) The effects of IgM-enriched immunoglobulin preparations in patients with severe sepsis (ISRCTN28863830). Crit Care 6:357–362
Maury E, Blanchard HS, Cahuvin P et al (2003) Circulating endotoxin and antiendotoxin antibodies during severe sepsis and septic shock. J Crit Care 18:115–120
Bennet Guerrero E, Ayuso L, Hamilton-Davies C et al (1997) Relationship of preoperative antiendotoxin core antibodies and adverse outcomes following cardiac surgery. JAMA 277:646–650
Venet F, Gebeile R, Bancel J et al (2011) Assessment of plasmatic immunoglobulin G, a and M levels in septic shock patients. Int Immunopharmacol 11:2086–2090
Giomarellos-Bourboulis E, Apostolidou E, Lada M et al (2013) Kinetics of circulating immunoglobulin M in sepsis: relationship with final outcome. Crit Care 17:R 247
Berlot G, Vassallo MC, Busetto N et al (2012) Relationship between the timing of administration of IgM and IgA enriched immunoglobulins in patients with severe sepsis and septic shock and the outcome: a retrospective analysis. J Crit Care 27:167–171
Berlot G, Dimastromatteo G (2004) Impiego delle immunoglobuline arricchite con IgM e IgA nel trattamento della sepsi severa e dello shock settico. Esperienza clinica. Minerva Anestesiol 70:739–745
Shanka-Hari M, Spencer J, Sewell WA, Rowan KM, Singer M (2012) Bench-to-bedside review: immunoglobulin therapy for sepsis: biological plausibility from a critical care perspective. Crit Care 16:206–280
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Berlot, G., Rossini, P., Turchet, F. (2015). Which Among Septic Patients Are the Best Candidate for Immunoglobulins?. In: Chiumello, D. (eds) Practical Issues Updates in Anesthesia and Intensive Care. Springer, Cham. https://doi.org/10.1007/978-3-319-18066-3_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-18066-3_3
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-18065-6
Online ISBN: 978-3-319-18066-3
eBook Packages: MedicineMedicine (R0)