Abstract
Purpose
Sodium citrate has antibacterial and anticoagulant properties that are confined to the catheter when used as a catheter lock. Studies of its use as a catheter lock in chronic hemodialysis patients suggest it may be efficacious in preventing infection and thrombotic complications. We compared sodium citrate with saline catheter locks for non-tunneled hemodialysis central venous catheters in critically ill adult patients. Primary endpoint was catheter life span without complication.
Methods
This was a randomized, controlled, open-label trial involving intensive care patients with acute renal failure requiring hemodialysis. Events were defined as catheter-related bloodstream infection and catheter malfunction.
Results
Seventy-eight patients were included. Median catheter life span without complication was 6 days (saline group) versus 12 days (citrate group) [hazard ratio (HR) 2.12 (95% CI 1.32–3.4), p = 0.0019]. There was a significantly higher rate of catheter malfunction in the saline group compared with in the citrate group (127 catheter events/1,000 catheter-days, saline group vs. 26 events/1,000 catheter-days, citrate group, p < 0.00001). There was no significant difference in incidence of infections between groups. We observed a significantly longer time to occurrence of infection in the citrate group (20 days vs. 14 days, HR 2.8, 95% CI 1.04–7.6, p = 0.04). By multivariate analysis, age and citrate group were the only independent factors that influenced catheter life span.
Conclusions
This study shows for the first time that citrate lock reduced catheter complications and increased catheter life span as compared to saline lock in critically ill adults requiring hemodialysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Venous catheters are the only feasible invasive approach in patients with acute renal failure requiring emergency hemodialysis [1–3]. Complications of venous catheters are common and can be classified as either minor complications, which do not involve the patient’s prognosis but result in intermittent failures; or major complications, which can be life-threatening, such as thrombosis, infection, or pulmonary embolism.
The systematic use of an antiseptic “fluid lock” between two dialysis sessions can significantly reduce the incidence of infectious complications [4, 5]. These locks prevent proliferation of bacteria and other pathogens in the catheter lumen [6]. Locks using antithrombotic agents such as heparin injected into the catheter lumen between two dialysis sessions maintain the permeability of the endovascular catheter and prevent thrombus formation [7, 8].
Some studies have shown that locking catheters between two hemodialysis sessions with solutions containing sodium citrate could prevent the occurrence of thrombosis and catheter infections in patients suffering from chronic kidney disease [9–11]. This can be explained not only by the role of citrate in chelation of calcium, which is an essential factor for coagulation, but also by the bacteriostatic role of citrate [11–13]. Traditionally, heparin is used as the standard catheter lock, particularly in North America [14, 15]. A recent meta-analysis of pooled data from all trials using citrate locks, as compared with heparin, showed a significant reduction in catheter-related bloodstream infections (CRBSI), need for catheter removal, and exit-site infections [16]. However, in the intensive care unit (ICU) setting, the use of heparin can be associated with life-threatening side effects such as bleeding [17], or heparin-induced thrombocytopenia [18]. Similarly, other drugs frequently used in critical care, in addition to a wide range of non-drug causes, can induce thrombocytopenia [19]. In ICU patients, occurrence of thrombocytopenia reportedly increases the prevalence of bleeding and the need for transfusion, and can indirectly influence mortality rates [20]. Heparin is also contraindicated in patients at high hemorrhagic risk [21]. In this context, it is common practice in France to lock catheters with a solution of physiological (saline) serum in the ICU, rather than heparin.
We hypothesized that the use of a citrate lock would reduce the incidence of catheter malfunction and CRBSI, and lead to an increase in the duration of the catheter before occurrence of a first event (i.e., its life span) in ICU patients with acute renal insufficiency undergoing emergency hemodialysis.
We report a randomized, controlled trial aiming to compare a citrate lock versus saline lock in terms of catheter life span without complications in an ICU population of hemodialysis patients.
Methods
This was a prospective, randomized, open-label trial conducted from May 2009 to August 2010 in one medical and one surgical ICU in the University Hospital of Dijon, France. The study protocol was approved by the Institutional Review Board of Dijon University Hospital (Comité Consultatif de Protection des Personnes), according to French law, and the research was carried out in compliance with the Helsinki Declaration. All patients (or next of kin) were informed about study participation.
Study data management and data analyses were shared by an independent committee financed by the clinical research division (DRCI) of the University Hospital of Dijon. Outcomes were evaluated locally and adjudicated by an independent clinical event committee composed of a nephrologist and an infectious disease specialist who were not involved in the trial and were blinded to patients’ treatment group assignments. The study procedures were performed by research nurses, who were aware of the treatment allocation, but were not involved in routine care of the patient. As far as possible, the nurses and physicians in the unit in charge of the routine care were blinded to each patient’s treatment.
Patients
The inclusion criteria were adult patients (>18 years) requiring continuous or intermittent hemodialysis for acute renal failure hospitalized in the ICU. Patients had to be included before the beginning of hemodialysis and before catheter insertion. In accordance with published recommendations for the prevention of central venous catheter complications [22, 23], all catheters were inserted under ultrasound guidance, and standard hygiene precautions were taken (e.g., use of mask, cap, gown, sterile gloves, sterile drapes, disinfection of catheter hubs) to minimize contamination.
Exclusion criteria were known allergy to citrate, pregnancy, liver failure, and history of thromboembolic disease.
Definition of events
In clinical practice, blood flow rates, as well as inflow and outflow line pressures are monitored during hemodialysis sessions. Low flows can hamper the efficiency of dialysis. A maximum arterial and venous pressure of −250 mmHg and +250 mmHg respectively are the accepted limits. In case of problems with catheter flow or pressures, both catheter lumens were flushed with a saline solution using a 10-ml syringe. If the problem persisted, the catheter was mobilized and the lines inversed. If all these maneuvers failed to restore adequate flow or pressure levels, the catheter was removed. Catheter malfunction was thus defined as a reduction of 20% or more in blood flow through the catheter, despite attempts to restore patency.
Catheter-related bloodstream infection (CRBSI) was defined as fever (temperature >38°C) with concordant positive blood cultures drawn from the catheter and a peripheral vein or a peripheral blood culture and a concordant exit-site culture, in the absence of any other clinically identifiable source of bloodstream infection other than the catheter. Probable CRBSI was defined as fever with one positive blood culture, in the absence of any other clinically identifiable source of infection other than the catheter. Probable CRBSIs were included as endpoints. Study patients were evaluated for fever and other signs suggestive of infection every 3 h by the nurses on duty, according to standard practice in our unit. Blood cultures, exit-site cultures if there was purulence at the exit site, and other studies, as indicated, were obtained whenever study patients had fever or chills, unexplained hypotension, or other clinical signs or symptoms suggestive of systemic infection, as previously described [24].
Recorded data
We prospectively recorded age, sex, type of unit (medical/surgical), SAPS II score [25], body mass index (BMI), diagnosis at admission, comorbidities, localization of vascular access, type of extracorporeal renal replacement therapy (ERRT), occurrence of CRBSI and catheter malfunction, and catheter life span until occurrence of first complication (if any).
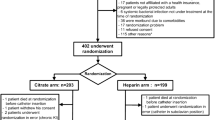
Intervention
All patients included in the study were randomized between the control group (saline group) and the experimental group (citrate group) (treatment allocation given in numbered sealed envelopes). In the saline group, locks were made by injecting 10 ml of saline in the two branches of the catheter; these branches were then rinsed every 6 h with 10 ml of saline after aspiration of their contents. In the citrate group, locks were made by injecting 10 ml saline and then filling each branch of the catheter with the corresponding volume of citrate solution (Dura Lock® 46.7%). Once citrate locks were in place, manipulations of the catheter were forbidden until the next hemodialysis. Before the next hemodialysis, the citrate lock was removed by aspiration. In both medical and surgical ICUs, the catheters used were 13-Fr biocompatible, polyurethane, double-lumen, radio-opaque dialysis catheters in both groups (Jet Cath™, Jet Medical Inc, Mainland, PA, USA); 16 cm in length for jugular access, and 25 cm in length for femoral access.
Statistics
Quantitative data are shown as mean ± standard deviation, with minimum and maximum values, and qualitative data as frequency (n) and percentage. Quantitative data were compared using the Student t test and qualitative data with the χ2 test.
In the design of the study, on the basis of observational data from our own department and in the absence of any published precedent, we hypothesized that the catheter life span would be increased by 30% by the use of citrate locks. According to Fleming’s one-stage procedure [26], we calculated that 39 patients per arm would be required with an alpha risk of 5% and a beta risk of 10%. All analyses were performed by intention-to-treat.
The life span of the catheter in each group was determined as the duration from the date of catheter placement to the date of withdrawal for any cause. All catheters still in use when dialysis was stopped, or at last follow-up date were censored.
The life span of the catheter without infection in both groups was determined as the duration from the date of catheter placement to the date of withdrawal because of catheter infection as demonstrated by a positive bacteriological culture of the catheter. All catheters still in use and without infection when dialysis was stopped, or at last follow-up date were censored.
Catheter life span without thrombosis in both groups was determined as the duration from the date of catheter placement to the date of withdrawal because of catheter thrombosis, as proven by the presence of a thrombus preventing dialysis. All catheters still in use and without thrombosis when dialysis was stopped, or at last follow-up date were censored.
Catheter life span without any event, without infection, or without thrombosis was estimated using the Kaplan–Meier method and groups were compared with the log-rank test. The hazard ratios (HR) and related 95% confidence interval (95% CI) were calculated using a univariate Cox model for each of the variables of interest. All variables with p value less than 0.20 as estimated by the Cox univariate method were selected for inclusion in the Cox multivariate model. All p values were two-tailed. The level of statistical significance was 5%.
Comparison of event rates per 1,000 catheter-days between groups was performed according to the binomial exact test.
All analyses were performed by one author (FG) using MedCalc software (MedCalc, Mariakerke, Belgium).
Results
Patient characteristics
From May 2009 to August 2010, 78 patients were included: 39 in each group (Table 1). Clinical characteristics were similar in both groups, particularly mean age, sex ratio, and BMI. There were no significant differences in terms of comorbidities. The predominant cause of admission to the ICU was sepsis; however, there was no significant difference in diagnosis at admission or severity score (SAPS II) between groups. Similarly, there was no significant difference in vascular access localization or type of hemodialysis between groups.
The mortality rate at the end of resuscitation was comparable in both groups: 54% in the saline group and 62% in the citrate group (p = 0.65).
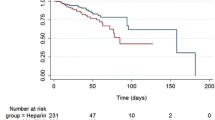
Catheter life span
During the study, a total of 135 catheters were used: 77 in the saline group and 58 in the citrate group. The median catheter life span was 6 days [3–10] in the saline group and 12 days [8–17] in the citrate group (HR 2.12, 95% CI 1.32–3.4, p = 0.0019) (Fig. 1).
Catheter malfunction
There was a significantly higher rate of catheter malfunction in the saline group as compared to the citrate group, with 127 catheter events per 1,000 catheter-days in the saline group, versus 26 events per 1,000 catheter-days in the citrate group (p < 0.00001). There was no significant difference in time to occurrence of first catheter malfunction event, which was 18 days in the citrate group versus 12 days in the saline group (HR 1.8, 95% CI 0.97–3.45, p = 0.08).
Catheter-related bloodstream infection
No difference was observed in the incidence of CRBSI between groups (30 vs. 24 infections per 1,000 catheter-days, saline vs. citrate groups respectively, p = not significant). However, we did observe a significantly longer time to occurrence of infection in the citrate group (20 days versus 14 days, HR 2.8, 95% CI 1.04–7.6, p = 0.04) (Fig. 2). The microbes responsible for infection are detailed in Table 2.
Predictors of catheter malfunction
Univariate analysis identified seven criteria that were related to occurrence of catheter malfunction and subsequently included in the multivariate model, namely age, sex, treatment group, SAPS II, diagnosis at admission, catheter localization, and type of dialysis. Only age, sex, SAPS II, and treatment group were retained in the final multivariate model, and of these, only age and treatment group were identified as independent predictive factors of catheter malfunction (HR 2.17, 95% CI 1.35–3.45, for age >60 years vs. <60 years, p = 0.0014, and HR 0.61, 95% CI 0.39–0.96, p = 0.034 for the citrate group, respectively].
Discussion
This study shows that citrate locks increase the median life span of hemodialysis catheters as compared to saline locks in patients with acute renal failure in the ICU. Complications associated with hemodialysis catheters are frequent in the ICU and, in many cases, require removal of the catheter. Thrombosis is the most frequent problem and can be life-threatening, by inducing pulmonary embolism. Our results thus confirm, in an acute setting, previous reports of the antithrombotic effectiveness of citrate locks in patients on maintenance hemodialysis [7, 8, 12].
Catheter malfunction is a frequent cause of premature catheter withdrawal. The primary cause of catheter malfunction is catheter thrombosis, but complications can arise from catheter position pressure problems or accidental disengagement of the catheter by the patient or paramedical staff during medical care. In both units involved in this study, an institutional protocol is in place for monitoring catheter blood flow and attempting to restore patency in cases of reduced permeability. The rate of catheter malfunction per 1,000 catheter-days observed in our study was considerably higher than that observed in other reports [14, 27]. This can be explained firstly by the different population included in our study, which was comprised of critically ill patients in need of acute hemodialysis. Conversely, a recent meta-analysis of published studies evaluating antibiotic catheter locks was mainly focused on patients on chronic hemodialysis [16].
Secondly, the type of equipment used may partially explain the differences in findings. Indeed, in the studies by Maki and Hemmelgarn [14, 27], tunneled catheters of the upper central venous system were used, whereas in our study, non-tunneled catheters were used, with both jugular and femoral access. It has previously been shown that tunneled catheters induce a lower risk of event [28].
Thirdly, the type of dialysis was also different, with both continuous and intermittent dialysis in our study, as compared to maintenance hemodialysis in other reports. The use of continuous dialysis can indeed increase the potential for malfunction or infectious complications [29]. However, the type of dialysis was not significantly associated with the incidence of complications in our study. This failure to observe any difference may be due to the small sample size or to a greater effect of citrate locks in this subset of patients.
Fourthly, in the studies by Maki and Hemmelgarn, jugular access only was used, whereas both femoral and jugular approaches were used in our study. However, according to recent reports from the French Cathedia study group, jugular access was not shown to be superior to femoral access in terms of catheter dysfunction and dialysis performance [29, 30].
Importantly, despite the US Federal Drug Agency (FDA) warning against using concentrated sodium citrate catheter lock solutions in hemodialysis patients, we did not observe the classical side effects described with citrate injection, such as hydroelectrolyte disorders that may cause cardiac arrhythmias [31], or adverse events leading to curtailed citrate treatment as reported by Power et al. [32]. This suggests that the citrate lock is not followed by release of the solution into the systemic circulation or, if there is any release, then the only very small amounts that did not affect overall biological parameters.
Infections are also a frequent cause of catheter removal. We also investigated the capacity of citrate lock to prevent catheter infection, and observed that the incidence of infections was similar in both groups. However, the life span of the catheter before first occurrence of infection was longer in the citrate group. This could suggest a bacteriostatic role of citrate, as has been shown in previous studies [11–13]. Given the higher rate of catheter malfunctions in the saline group, it is likely that the increased frequency of catheter manipulations in this group may have promoted infection and shorter catheter life span. Previous studies have suggested that filling catheters with antiseptic solution between two dialysis sessions can reduce the incidence of infectious complications [6, 33].
Finally, multivariate analysis confirmed that only age and the use of citrate lock significantly affected catheter complications. Older age was associated with a higher rate of complications, and this can probably be explained by the more frequent comorbidities in elderly patients, which may favor infection and thrombotic events.
Surprisingly, in this study, SAPS II and BMI were not associated with catheter complications. Indeed, the severity of disease at admission is often associated with thrombotic events, and catheter insertion is much more difficult in these patients, thus potentially favoring catheter events. The number of insertion sites is smaller, because femoral venous access may be impossible and jugular routes are already used for the central venous catheter (for therapies and parenteral nutrition). These difficulties result in increased punctures, which can favor sepsis events [34–36].
Study limitations
This study suffers from several limitations that deserve to be underlined. The sample size of the study is relatively small. However, this sample size was calculated according to established statistical methods in order to ensure sufficient statistical power for the analysis of catheter life span. Secondly, the study population is heterogeneous, with the inclusion of both medical and surgical patients. Similarly, the study was conducted in two different ICUs (medical and surgical). Nonetheless, a standardized institutional protocol for catheter hygiene is in place and thus, in theory, practices are identical in both units. Thirdly, the study was performed according to an open-label design, such that both nurses and physicians handling the catheters knew the treatment allocation. However, the study procedures were performed by research nurses not involved in the routine care of the patient, and the analysis of the results was performed by an independent statistician, who was blinded to the treatment assignments of all patients. Lastly, the comparator used in the control group was saline serum, and not heparin. As stated previously, it is current practice in France to use saline locks rather than heparin as in previous reports [29]. The difference observed in our study might have been less pronounced if the control group comparator had been heparin, and we would undoubtedly have required a larger sample size in order to be able to detect such a difference with sufficient statistical power.
Conclusion
This study is the first prospective randomized study conducted in an ICU setting that compares the effectiveness of citrate locks versus saline locks to avoid catheter complications. We demonstrate the superiority of citrate locks in this context. Citrate locks increase the catheter life span and decrease the incidence of catheter malfunction. Given the longer time to occurrence of first infection observed with citrate catheter locks, the findings of this study strongly support the use of citrate locks in patients hospitalized in intensive care and undergoing hemodialysis.
References
Agee KR, Balk RA (1992) Central venous catheterization in the critically ill patient. Crit Care Clin 8:677–686
Canaud B, Leray-Moragues H, Leblanc M, Klouche K, Vela C, Beraud JJ (1998) Temporary vascular access for extracorporeal renal replacement therapies in acute renal failure patients. Kidney Int Suppl 66:S142–S150
Robert R, Honoré PM, Bastien O (2006) Les circulations extracorporelles en réanimation. Elsevier, Paris
Allon M (2003) Prophylaxis against dialysis catheter-related bacteremia with a novel antimicrobial lock solution. Clin Infect Dis 36:1539–1544. doi:10.1086/375234
Hendrickx L, Kuypers D, Evenepoel P, Maes B, Messiaen T, Vanrenterghem Y (2001) A comparative prospective study on the use of low concentrate citrate lock versus heparin lock in permanent dialysis catheters. Int J Artif Organs 24:208–211
Vercaigne LM, Sitar DS, Penner SB, Bernstein K, Wang GQ, Burczynski FJ (2000) Antibiotic-heparin lock: in vitro antibiotic stability combined with heparin in a central venous catheter. Pharmacotherapy 20:394–399
Bailey E, Berry N, Cheesbrough JS (2002) Antimicrobial lock therapy for catheter-related bacteraemia among patients on maintenance haemodialysis. J Antimicrob Chemother 50:615–617
Poole CV, Carlton D, Bimbo L, Allon M (2004) Treatment of catheter-related bacteraemia with an antibiotic lock protocol: effect of bacterial pathogen. Nephrol Dial Transplant 19:1237–1244. doi:10.1093/ndt/gfh041
Grudzinski L, Quinan P, Kwok S, Pierratos A (2007) Sodium citrate 4% locking solution for central venous dialysis catheters–an effective, more cost-efficient alternative to heparin. Nephrol Dial Transplant 22:471–476. doi:10.1093/ndt/gfl606
Lok CE, Appleton D, Bhola C, Khoo B, Richardson RM (2007) Trisodium citrate 4%—an alternative to heparin capping of haemodialysis catheters. Nephrol Dial Transplant 22:477–483. doi:10.1093/ndt/gfl570
Weijmer MC, Debets-Ossenkopp YJ, Van De Vondervoort FJ, ter Wee PM (2002) Superior antimicrobial activity of trisodium citrate over heparin for catheter locking. Nephrol Dial Transplant 17:2189–2195
Weijmer MC, van den Dorpel MA, Van de Ven PJ, ter Wee PM, van Geelen JA, Groeneveld JO, van Jaarsveld BC, Koopmans MG, le Poole CY, Schrander-Van der Meer AM, Siegert CE, Stas KJ (2005) Randomized, clinical trial comparison of trisodium citrate 30% and heparin as catheter-locking solution in hemodialysis patients. J Am Soc Nephrol 16:2769–2777. doi:10.1681/ASN.2004100870
Ash SR, Mankus RA, Sutton JM, Criswell RE, Crull CC, Velasquez KA, Smeltzer BD, Ing TS (2000) Concentrated sodium citrate (23%) for catheter lock. Hemodial Int 4:22–31
Hemmelgarn BR, Moist LM, Lok CE, Tonelli M, Manns BJ, Holden RM, LeBlanc M, Faris P, Barre P, Zhang J, Scott-Douglas N (2011) Prevention of dialysis catheter malfunction with recombinant tissue plasminogen activator. N Engl J Med 364:303–312. doi:10.1056/NEJMoa1011376
Allon M (2007) Current management of vascular access. Clin J Am Soc Nephrol 2:786–800. doi:10.2215/CJN.00860207
Yahav D, Rozen-Zvi B, Gafter-Gvili A, Leibovici L, Gafter U, Paul M (2008) Antimicrobial lock solutions for the prevention of infections associated with intravascular catheters in patients undergoing hemodialysis: systematic review and meta-analysis of randomized, controlled trials. Clin Infect Dis 47:83–93. doi:10.1086/588667
Yevzlin AS, Sanchez RJ, Hiatt JG, Washington MH, Wakeen M, Hofmann RM, Becker YT (2007) Concentrated heparin lock is associated with major bleeding complications after tunneled hemodialysis catheter placement. Semin Dial 20:351–354. doi:10.1111/j.1525-139X.2007.00294.x
Selleng K, Warkentin TE, Greinacher A (2007) Heparin-induced thrombocytopenia in intensive care patients. Crit Care Med 35:1165–1176. doi:10.1097/01.CCM.0000259538.02375.A5
Priziola JL, Smythe MA, Dager WE (2010) Drug-induced thrombocytopenia in critically ill patients. Crit Care Med 38:S145–S154. doi:10.1097/CCM.0b013e3181de0b88
Strauss R, Wehler M, Mehler K, Kreutzer D, Koebnick C, Hahn EG (2002) Thrombocytopenia in patients in the medical intensive care unit: bleeding prevalence, transfusion requirements, and outcome. Crit Care Med 30:1765–1771
Kellum JA, Mehta RL, Angus DC, Palevsky P, Ronco C (2002) The first international consensus conference on continuous renal replacement therapy. Kidney Int 62:1855–1863. doi:10.1046/j.1523-1755.2002.00613.x
O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, Lipsett PA, Masur H, Mermel LA, Pearson ML, Raad, II, Randolph AG, Rupp ME, Saint S (2011) Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control 39:S1–34. doi:10.1016/j.ajic.2011.01.003
McGee DC, Gould MK (2003) Preventing complications of central venous catheterization. N Engl J Med 348:1123–1133. doi:10.1056/NEJMra011883
Allon M (2004) Dialysis catheter-related bacteremia: treatment and prophylaxis. Am J Kidney Dis 44:779–791
Le Gall JR, Neumann A, Hemery F, Bleriot JP, Fulgencio JP, Garrigues B, Gouzes C, Lepage E, Moine P, Villers D (2005) Mortality prediction using SAPS II: an update for French intensive care units. Crit Care 9:R645–R652. doi:10.1186/cc3821
Fleming TR (1982) One-sample multiple testing procedure for phase II clinical trials. Biometrics 38:143–151
Maki DG, Ash SR, Winger RK, Lavin P (2011) A novel antimicrobial and antithrombotic lock solution for hemodialysis catheters: a multi-center, controlled, randomized trial. Crit Care Med 39:613–620. doi:10.1097/CCM.0b013e318206b5a2
Timsit JF, Bruneel F, Cheval C, Mamzer MF, Garrouste-Orgeas M, Wolff M, Misset B, Chevret S, Regnier B, Carlet J (1999) Use of tunneled femoral catheters to prevent catheter-related infection. A randomized, controlled trial. Ann Intern Med 130:729–735
Parienti JJ, Thirion M, Megarbane B, Souweine B, Ouchikhe A, Polito A, Forel JM, Marque S, Misset B, Airapetian N, Daurel C, Mira JP, Ramakers M, du Cheyron D, Le Coutour X, Daubin C, Charbonneau P (2008) Femoral vs jugular venous catheterization and risk of nosocomial events in adults requiring acute renal replacement therapy: a randomized controlled trial. JAMA 299:2413–2422. doi:10.1001/jama.299.20.2413
Parienti JJ, Megarbane B, Fischer MO, Lautrette A, Gazui N, Marin N, Hanouz JL, Ramakers M, Daubin C, Mira JP, Charbonneau P, du Cheyron D (2010) Catheter dysfunction and dialysis performance according to vascular access among 736 critically ill adults requiring renal replacement therapy: a randomized controlled study. Crit Care Med 38:1118–1125. doi:10.1097/CCM.0b013e3181d454b3
Uhl L, Maillet S, King S, Kruskall MS (1997) Unexpected citrate toxicity and severe hypocalcemia during apheresis. Transfusion 37:1063–1065
Power A, Duncan N, Singh SK, Brown W, Dalby E, Edwards C, Lynch K, Prout V, Cairns T, Griffith M, McLean A, Palmer A, Taube D (2009) Sodium citrate versus heparin catheter locks for cuffed central venous catheters: a single-center randomized controlled trial. Am J Kidney Dis 53:1034–1041. doi:10.1053/j.ajkd.2009.01.259
Dogra GK, Herson H, Hutchison B, Irish AB, Heath CH, Golledge C, Luxton G, Moody H (2002) Prevention of tunneled hemodialysis catheter-related infections using catheter-restricted filling with gentamicin and citrate: a randomized controlled study. J Am Soc Nephrol 13:2133–2139
Berenholtz SM, Pronovost PJ, Lipsett PA, Hobson D, Earsing K, Farley JE, Milanovich S, Garrett-Mayer E, Winters BD, Rubin HR, Dorman T, Perl TM (2004) Eliminating catheter-related bloodstream infections in the intensive care unit. Crit Care Med 32:2014–2020
Warren DK, Zack JE, Mayfield JL, Chen A, Prentice D, Fraser VJ, Kollef MH (2004) The effect of an education program on the incidence of central venous catheter-associated bloodstream infection in a medical ICU. Chest 126:1612–1618. doi:10.1378/chest.126.5.1612
Kaplowitz LG, Comstock JA, Landwehr DM, Dalton HP, Mayhall CG (1988) A prospective study of infections in hemodialysis patients: patient hygiene and other risk factors for infection. Infect Control Hosp Epidemiol 9:534–541
Acknowledgments
We are grateful to the patients and their families and the nurses and physicians in the participating ICU for their support of this trial. We would also like to thank the clinical research division (DRCI) of the University Hospital of Dijon for their support. The authors thank Fiona Ecarnot for translation and editorial assistance. This work was financed by the University Hospital of Dijon Clinical Research Division.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
L. Hermite, J.-P. Quenot, A. Nadji, and S. D. Barbar contributed equally to the work.
Rights and permissions
About this article
Cite this article
Hermite, L., Quenot, JP., Nadji, A. et al. Sodium citrate versus saline catheter locks for non-tunneled hemodialysis central venous catheters in critically ill adults: a randomized controlled trial. Intensive Care Med 38, 279–285 (2012). https://doi.org/10.1007/s00134-011-2422-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-011-2422-y