Abstract
Background
Central venous catheters (CVC) are the only option when hemodialysis is needed for patients without definitive vascular access. However, CVC is associated with complications, such as infection, thrombosis, and dysfunction, leading to higher mortality and expenditures. The aim of this study was to compare the effectiveness of 30 % trisodium citrate (TSC30 %) with heparin as CVC lock solutions in preventing catheter-related bloodstream infections (CRBSI) and dysfunction in hemodialysis patients.
Methods
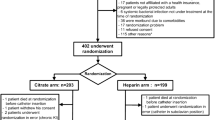
Randomized, double-blind controlled trial comparing the event-free survival of non-tunneled CVC locked with heparin or TSC30 % in adult hemodialysis patients.
Results
The study included 464 catheters, 233 in heparin group, and 231 in TSC30 % group. The CRBSI-free survival of TSC30 % group was significantly shorter than that of heparin group. When stratified by insertion site, heparin was better than TSC30 % only in subclavian CVC. The dysfunction-free survival was not different between groups in the main analysis, but there is also a shorter survival among subclavian CVC locked with TSC30 % in stratified analysis.
Conclusion
There was no difference on CRBSI-free or dysfunction-free survival between jugular vein CVC locked with heparin or 30 % citrate. However, subclavian CVC locked with 30 % citrate presented shorter event-free survival. This difference may be related to anatomical and positional effects, CVC design, and hydraulic aspects of the lock solution.
ClinicalTrials.gov identifier
NCT02563041.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of end-stage renal disease (ESRD) requiring renal replacement therapy (RRT) has increased in the last decade, and it is expected a continuous increase over the next years [1, 2]. Hemodialysis (HD), the main modality of RRT, depends on long term and effective vascular access. The vascular access of choice is the arteriovenous fistula (AVF). Vascular grafts and central venous catheters (CVC) are considered second and third options, due to the greater risk of infection, thrombosis, need of rescue procedures, and higher mortality and hospitalization rates [3, 4]. However, recent data show that 42–71 % of ESRD patients in Europe and 67 % in the US started the HD program using a CVC [5]. Furthermore, a significant number of patients need temporary vascular access to manage acute kidney injury, during delayed AVF maturation, or as a bridge to kidney transplantation or peritoneal dialysis.
Infection is the second leading cause of death in patients on HD [6, 7]. The use of a CVC is the major risk factor for bacteremia in HD, which can result in life-threatening complications in over 10 % of cases, such as septic shock, endocarditis, septic arthritis, osteomyelitis, and epidural abscesses. The relative risk of hospitalization for infection and death is 2–3 times greater in patients using CVC compared with patients with AVF or vascular graft [4], with consequent increase in health expenditures.
Considering the widespread use of CVC, adherence to prophylaxis protocols, early diagnosis, and effective treatment of CVC-related infections are fundamental to improve outcome. Antibiotic lock solutions have been presented as a potential strategy to reduce infectious complications and catheter dysfunction. The principle of CVC lock is to instill an anticoagulant solution into the lumen of the catheter after each hemodialysis session, leaving it in until the next session. Heparin is the most frequently used substance in lock solutions, exerting its anticoagulant activity by binding to antithrombin and antagonizing coagulation factors. The addition of antibiotics as gentamicin or taurolidine to heparin decreases catheter-related bloodstream infections by 60–70 %, according to five recent meta-analyses, [8–12]. However, this result was limited by heterogeneity among studies, few large trials, evidence of publication bias, and most studies conducted in populations with higher than expected infections rates. Furthermore, the use of antibiotic locks is not recommended by guidelines mainly due to concerns on induction of bacterial resistance [13, 14].
Citrate is an alternative to heparin, exerting its effect by chelation of calcium, essential element to the coagulation cascade. In addition to anticoagulant effects, chelation of calcium by citrate can also prevent the biofilm formation, rendering this lock solution more effective than heparin in reducing infectious complications, without the concerns on bacterial resistance. However, the previous studies on the effects of citrate lock solutions have heterogeneous findings [9, 11, 12, 15–22].
This study was designed to compare the effectiveness of 30 % trisodium citrate with heparin as CVC lock solutions on the prevention of premature withdrawal for catheter-related bloodstream infections or dysfunction in hemodialysis patients.
Methods
Study design
This double-blind randomized controlled trial (RCT) was conducted from July 2012 until July 2014 in the dialysis and transplantation unit of a Brazilian university hospital. Each new double-lumen non-tunneled catheter to be implanted was randomly assigned to be locked with either unfractionated sodium heparin 5000 U/mL or 30 % trisodium citrate (Citra-Lock™ 30 %, Fresenius Medical Care). The randomization was performed through a computer-generated list of random numbers in blocks of six. Patients and investigators were unaware of the treatment assignments. Allocation concealment was performed using opaque, sealed envelopes.
After each HD session, the catheter lumens were flushed with 0.9 % sodium chloride and locked with a volume of the assigned solution exactly equivalent to the catheter internal lumen. Catheter care was according to the international guidelines, including strict asepsis on insertion and exit-site dressing changes after each HD session by staff wearing masks and sterile gloves. No intranasal mupirocin was used.
Selection of patients
Patients eligible for enrollment in the RCT were older than 18 years, with a diagnosis of chronic or acute renal failure that required hemodialysis through a catheter. Patients admitted to the intensive care ward, receiving a tunneled catheter, with suspected heparin-induced thrombocytopenia, allergy to heparin or TSC30 %, with systemic or localized infection, or pregnant women were excluded. The site of insertion and specific type of double-lumen catheter were submitted to interventionist physician discretion.
Primary outcomes
Catheter-related bloodstream infection (CRBSI)
CRBSI was defined according to criteria of definite or probable bloodstream infection from the Centers for Disease Control (CDC, Atlanta, GA, USA) [14]. The CDC definitions are as follows: (1) definite bloodstream infection: isolation of the same organism from a semiquantitative culture of the catheter tip (>15 colony-forming units per catheter segment) and from a peripheral or catheter blood sample in a symptomatic patient with no other apparent source of infection; and (2) probable bloodstream infection: defervescence after antibiotic therapy with or without removal of the catheter in the setting, where blood cultures confirm infection, but the catheter tip does not, or the catheter tip confirms infection, but blood cultures do not in a symptomatic patient with no other apparent source of infection.
The management of the CRBSI was performed according to guidelines, including empirical antibiotic therapy and catheter removal.
Catheter dysfunction
Dysfunction was defined as a persistent inability to obtain a blood flow above 200 mL/min (extreme dysfunction) at a pre-pump arterial pressure more negative than −250 mmHg. In this setting, the catheter would be removed or exchanged over guidewire.
Potential confounding factors, adverse events, and death rates
Patients related
Data were also collected about age, gender, skin color, presence of diabetes, diagnosis of CKD or acute kidney injury, and hemodialysis vintage.
Catheter related
Site of insertion (jugular, subclavian, or femoral veins), and ordinal number of the catheter in the same patient (considering only the study period) are catheter related.
Adverse events that were considered as related to the lock solutions and all-cause mortality were registered.
Statistical analysis
Calculation of the required sample size was based on primary outcomes. It was assumed that the group with heparin lock would have a rate of catheter-related bloodstream infection of 150 % greater than that of catheters with TCS30 % lock (based on the previous evidence) [11, 12, 15–22]. With a two-sided test, and an alfa error of 5 and 80 % of power, it was required 112 catheters for each group.
The primary analysis was made through survival analysis with Cox proportional hazard regression. Initially, we proceed to univariate analysis using Kaplan–Meier curves and log-rank test for the categorical variables and univariate Cox regression for continuous variables. The predictors which have a p value lower than 0.25 in univariate analysis were included in final model. Two final models were constructed, one with the outcome infection-free survival and another with dysfunction-free survival as dependent variables. Predictors which had no significant association with the outcome were progressively removed from the models, starting with those with lower association (backward regression). Interactions were checked for any possible association of predictors. The likelihood ratio test was used for compare nested with full models. The proportionality of predictors was verified by introduction of time-dependent variables in the model. If any predictor violates the proportionality assumption, the analysis would be stratified for that predictor. Well-functioning catheters at the end of the study period, catheters removed, because patients acquired functional arteriovenous fistula, renal function recovery, changed to peritoneal dialysis, had transplantation, or death were analyzed as censored data. The analysis was all done on intention-to-treat base. All reported p values are two sided. The analysis was performed using the STATA 11.2 statistical software (Stata Corporation, College Station, TX, USA).
Ethical aspects
The study protocol was approved by the local review board. Written informed consent was obtained from all patients before enrollment.
The protocol was registered in ClinicalTrials.gov with identifier NCT02563041.
Results
A total of 179 patients, who received 464 non-tunneled central venous catheters, were selected for the study. There was no refusal to participate. After randomization, 233 catheters were included in the heparin group and 231 catheters in the 30 % TSC group. Each patient received a median of 2 (range 1–18) catheters throughout the study. The majority of the sample was composed of CKD patients (76 %), who used 87 % of the catheters, with mean hemodialysis vintage of 2 (±3.3) months. Among CKD patients, there were 26 % of diabetic renal disease and 26 % of obstructive nephropathy. Twenty-four percent of patients suffered acute kidney injury, mostly (50 %) in a sepsis context. There was no difference on baseline characteristics between heparin and 30 % TSC groups (Table 1). There was no difference in the insertion site according to the physician. There was also no difference in infection-free survival or dysfunction-free survival according to the operator.
The catheter median length of stay was of 18.00 (IQR 37) days in heparin group and 18.00 (IQR 25) days in 30 % TSC group, with a total of 6927 catheter/days in heparin group and 6052 catheter/days in TSC group. The rate of CRBI was 5.2 per 1000 catheter-days in TSC30 % group and 3.4 per 1000 catheter-days in heparin group [RR 1.53 (95 % CI 0.90–2.58)]. The more frequently micro-organism responsible for CRBSI was coagulase-negative staphylococci (46 % blood cultures), followed by Staphylococcus aureus (35 %), with no significant difference between lock solution groups. The rate of dysfunction was 11.4 per 1000 catheter-days in TSC30 % group and 9.4 per 1000 catheter-days in heparin group [RR 1.21 (95 % CI 0.87–1.70)]. There were only two records of adverse events, both in 30 % TSC group and both of less severity (metallic taste in the mouth during lock solution instillation). There were 34 deaths during the study period, 18 patients died with a 30 % TSC locked CVC and 16 using a heparin-locked catheter (RR 0.88 95 % CI 0.46–1.68). No death was considered to be related to the catheter lock solution.
Catheter-related bloodstream infection
The predictors’ site of insertion, diabetic renal disease, and lock solution groups were associated with CRBSI in the univariate analysis. There was a longer CRBSI-free survival for catheters placed in subclavian vein, for non-diabetic patients, and for CVC locked with heparin (Fig. 1). The multivariate model, including these variables, maintained a significant association only between CRBSI and lock solution group, with the predictors’ diabetic state and site of insertion no more significantly associated with the outcome in adjusted analysis. However, these variables were maintained in the model, because of their well-known effect on CVC infectious complications (Table 2). There was no interaction between any pair of model predictors. The 30 % TSC group presented a hazard ratio of 1.95 (95 % CI 1.03–3.67) in the final model, which means that the use of citrate lock was associated with a risk 95 % greater of catheter removal for CRBSI when compared with heparin lock, after adjusting for diabetic state and insertion site.
However, the predictor insertion site violated the proportionality assumption, which led to a stratified analysis for CVC inserted in jugular vein and CVC inserted in subclavian vein. No predictor had any significant association with CRBSI-free survival in the subgroup of jugular CVC (Table 2), not even lock solution (Fig. 2). However, 30 % TSC lock solution maintained an association with event-free survival among subclavian catheters, with a hazard ratio of 3.36 (95 % CI 1.02–11.04) (Table 2; Fig. 3). It means that subclavian catheters locked with 30 % TSC presented a risk 236 % greater to be removed for infection. The small number of femoral insertions precludes their inclusion in analysis.
Catheter poor blood flow
The predictors site of insertion, ordinal number of catheter, and lock solution groups showed a tendency of association with catheter removal for dysfunction in the univariate analysis (p value <0.25). There was a tendency for longer event-free survival for catheters placed in jugular vein, for initial catheters, and for CVC locked with heparin. The multivariate model, including these variables, showed no significant association with the outcome (Table 3). There was no interaction between any pair of model predictors. The predictor insertion site violated the proportionality assumption, which led to a stratified analysis for CVC inserted in jugular vein and CVC inserted in subclavian vein. The ordinal number of the catheter presented a significant association with dysfunction-free survival in the subgroup of jugular CVC, favoring initially placed catheters with a hazard ratio of 1.13 (95 % CI 1.03–1.23) (Table 3). This finding means that each subsequent catheter if implanted in jugular vein in the same patient had a 13 % greater risk of dysfunction. The lock solution group presented an association with dysfunction-free survival only among subclavian catheters, with a hazard ratio of 1.80 (95 % CI 1.00–3.22) (Table 3). It means that subclavian catheters locked with 30 % TSC presented a risk 80 % greater to be removed for dysfunction. The small number of femoral insertions precludes their inclusion in analysis.
Discussion
This RCT analyzed almost 500 non-tunneled hemodialysis CVC comparing CRBSI-free and dysfunction-free survival between heparin and 30 % TSC lock solution groups. It is the largest RCT on the issue published so far. The study found no advantage of 30 % TSC, with similar dysfunction-free survival between the lock groups as a whole, and, surprisingly, an increased CRBSI-free survival in heparin lock group. The analysis stratified for insertion site found that catheters placed into subclavian veins and locked with 30 % citrate attained worse results in both infection and dysfunction outcomes.
This finding goes against the results of Weijmer et al., who randomized 291 HD patients with CVC, most of them with non-tunneled catheters, and compared 30 % TSC lock solution with a standard heparin lock [18]. The frequency of catheter-related bacteremia was substantially lower in patients using the concentrated citrate lock (1.1 versus 4.1 episodes/1000 catheter-days). However, in the stratified analysis, the subgroup of non-tunneled catheters had no significantly different rates of bacteremia between citrate or heparin-locked CVC. Betges et al. also found a significantly longer sepsis-free survival for tunneled catheters locked with citrate, but non-tunneled catheters had no significantly different survival curves if locked with citrate or heparin [19]. Other studies using high or low citrate concentration as lock solution in hemodialysis CVC have found heterogeneous results [9, 11, 12, 15–22]. However, most of them include a small number of non-tunneled catheters or do not include this type of CVC at all.
A recently published meta-analysis describes the interesting finding that lock solutions with lower concentration of citrate, but not that with higher concentration, is more effective in prevent infectious complications than heparin [12]. There are some potential explanations for this, at first sight, illogical difference in effect. First of all, around 20 % of the volume of any catheter locks leaks into systemic circulation at the time of instillation, due to parabolic flow that occurs within cylindrical tubes [23]. Furthermore, the spillage is even greater if the lock solution has higher concentration of citrate, because its greater density compared with blood leads to gravity-induced loss of lock solution into the systemic circulation [24]. Hence, the intra-luminal citrate concentration varies from zero (at the tip in CVC with side holes) to unchanged concentration at the highest point of the CVC, with possible differences in antimicrobial effects [25].
In addition to spillage and heterogeneous lock concentrations within the CVC, even the in vivo antimicrobial effect of citrate lock solution has been questioned. Schilcher et al. found that 46.7 % citrate reduced the number of E. coli by 2 log units, but after 24 h, 106 CFU/mL were still present. Citrate 3 % and citrate-free blood, as were found in medium and lower CVC sections after spillage and dilution of citrate 46.7 %, had no antimicrobial effect on E. coli. Citrate 46.7 %, citrate 3 %, and citrate-free blood had scarce antimicrobial effect on S. aureus within 24 h [25]. There is a huge predominance of staphylococcus species in blood cultures of CRBSI in hemodialysis patients, exactly the micro-organism with lower sensibility to citrate.
The same previously cited meta-analysis [12] found that CRBSI rate was lower with citrate lock, but CRBSI-free catheter survival was similar between citrate and heparin groups. The analysis included 11 RCTs comparing the incidence of CRBSI between citrate and heparin, but only 3 of them reported CRBSI-free catheter survival [26–28].
Nevertheless, there is no obvious explanation for the longer CRBSI-free and dysfunction-free survival in subclavian catheters locked with heparin solution. It is known that citrate solutions reduce biofilm formation, although there are doubts about its effect on floating micro-organisms. In addition, there is some evidence that hypertonic citrate lead to protein precipitation inside CVC [29]. The actual implications of this phenomenon are not clear. There is worry that this proteinaceous material could lead to venous embolism, but it has not been documented. Another concern relates to the occlusion of CVC holes causing malfunction. However, there is also evidence that the proteins that are precipitated by hypertonic citrate are readily again solubilized when citrate is diluted after gravitational and injection spillage. The worse results of citrate in subclavian catheters may be related to anatomical and positional aspects, CVC design, and/or hydraulic effects of the lock solution. Most of the previous trials include a small number of subclavian catheters [18, 22, 26, 28], and no study had compared citrate with heparin lock solutions stratifying for insertion site. However, our RCT was not powered to analyze subclavian catheter alone, and this finding should be confirmed in adequately powered studies. Another weak point is that only non-tunneled CVC was included in this trial, which precludes the extrapolation of the findings to tunneled catheters. Most guidelines suggest that a tunneled CVC should be implanted if the intended stay is above 3 weeks [14, 30]. However, the evidence on advantages of tunneled catheters over non-tunneled is entirely based on observational studies, and there is no randomized clinical trial comparing the two options in HD patients [13, 31, 32], therefore, it is unknown to what extent the tunneling could actually reduce the CVC complications in HD. In addition, tunneled CVC insertion is associated with increased cost, the need for skilled operators, and fluoroscopic monitoring facilities, which sometimes is not readily available. According to The Dialysis Outcomes and Practice Patterns Study (DOPPS), 75 and 31 % of catheters in Europe and 48 and 41 % in the USA among incident and prevalent HD patients, respectively, were non-tunneled CVC [33].
Despite all these unanswered questions, there seem to be currently enough evidences to proscribe the use of higher concentrations of citrate as lock solution in hemodialysis central venous catheters. In addition to the risks associated with inadvertent systemic instillation of citrate [34], and the higher economic costs, there is now a growing body of evidence signaling to the lack of additional benefits of hypertonic citrate compared to heparin-locking solutions.
References
Mills KT, Xu Y, Zhang W, Bundy JD, Chen SC, Kelly TN, Chen J, He1 J. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int Adv Online Publ, Kidney Int. 2015 Jul 29. doi:10.1038/ki.2015.230. (Epub ahead of print)
Zoccali C, Kramer A, Jager KJ. Epidemiology of CKD in Europe: an uncertain scenario. Nephrol Dial Transplant. 2010;25:1731–3.
Pisoni RL, Arrington CJ, Albert JM, Ethier J, Kimata N, Krishnan M, Rayner HC, Saito A, Sands JJ, Saran R, Gillespie B, Wolfe RA, Port FK. Facility hemodialysis vascular access use and mortality in countries participating in DOPPS: an instrumental variable analysis. Am J Kidney Dis. 2009;53:475–91.
Dhingra RK, Young EW, Hulbert-Shearon TE, Leavey SF, Port FK. Type of vascular access and mortality in US hemodialysis patients. Kidney Int. 2001;60:1443–51.
Pisoni RL, Zepel L, Port FK, Robinson BM. Trends in US vascular access use, patient preferences, and related practices: an update from the US DOPPS practice monitor with international comparisons. Am J Kidney Dis. 2015;65:905–15.
US Renal Data System. Annual data report: An overview of the epidemiology of kidney disease in the United States. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2014.
de Jager DJ, Grootendorst DC, Jager KJ, et al. Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA. 2009;302:1782–9.
James MT, Conley J, Tonelli M, Manns BJ, MacRae J, Hemmelgarn BR, Alberta Kidney Disease Network. Meta-analysis: antibiotics for prophylaxis against hemodialysis catheter-related infections. Ann Intern Med. 2008;148:596–605.
Yahav D, Rozen-Zvi B, Gafter-Gvili A, Leibovici L, Gafter U, Paul M. Antimicrobial lock solutions for the prevention of infections associated with intravascular catheters in patients undergoing hemodialysis: systematic review and meta-analysis of randomized, controlled trials. Clin Infect Dis. 2008;47:83–93.
Jaffer Y, Selby NM, Taal MW, Fluck RJ, McIntyre CW. A metaanalysis of hemodialysis catheter locking solutions in the prevention of catheter-related infection. Am J Kidney Dis. 2008;51:233–41.
Labriola L, Crott R, Jadoul M. Preventing haemodialysis catheter- related bacteraemia with an antimicrobial lock solution: a meta-analysis of prospective randomized trials. Nephrol Dial Transplant. 2008;23:1666–72.
Zhao Y, Li Z, Zhang L, Yang J, Yang Y, Tang Y, Fu P. Citrate versus heparin lock for hemodialysis catheters: a systematic review and meta-analysis of randomized controlled trials. Am J Kidney Dis. 2014;63:479–90.
Betjes MGH. Prevention of catheter-related bloodstream infection in patients on hemodialysis. Nat Rev Nephrol. 2011;7:257–65.
O’Grady NP, Alexander M, Dellinger EP, et al. Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2002;51:1–29.
Moran J, Sun S, Khababa I, Pedan A, Doss S, Schiller B. A Randomized trial comparing gentamicin/citrate and heparin locks for central venous catheters in maintenance hemodialysis patients. Am J Kidney Dis. 2011;59:102–7.
Winnett G, Nolan J, Miller M, Ashman N. Trisodium citrate 46.7 % selectively and safely reduces staphylococcal catheter-related bacteraemia. Nephrol Dial Transplant. 2008;23:3592–8.
Allon M. Prophylaxis against dialysis catheter-related bacteremia with a novel antimicrobial lock solution. Clin Infect Dis. 2003;36:1539–44.
Weijmer MC, van den Dorpel MA, van de Ven PJG, et al. Randomized, clinical trial comparison of trisodium citrate 30 % and heparin as catheter-locking solution in hemodialysis patients. J Am Soc Nephrol. 2005;16:2769–77.
Betjes MG, van Agteren M. Prevention of dialysis catheter-related sepsis with a citrate-taurolidine-containing lock solution. Nephrol Dial Transplant. 2004;19:1546–51.
Lok CE, Appleton D, Bhola C, Khoo B, Richardson RM. Trisodium citrate 4 %––an alternative to heparin capping of haemodialysis catheters. Nephrol Dial Transplant. 2007;22:477–83.
Grudzinski L, Quinan P, Kwok S, Pierratos A. Sodium citrate 4 % locking solution for central venous dialysis catheters––an effective, more cost-efficient alternative to heparin. Nephrol Dial Transplant. 2007;22:471–6.
MacRae JM, Dojcinovic I, Djurdjev O, et al. Citrate 4 % versus heparin and the reduction of thrombosis study (CHARTS). Clin J Am Soc Nephrol. 2008;3:369–74.
Polaschegg HD. Catheter locking-solution spillage: theory and experimental verification. Blood Purif. 2008;26:255–60.
Doorenbos CJ, Van den Elsen-Hutten M, Heuven MJ, et al. Estimation of trisodium citrate (Citra-Lock) remaining in central venous catheters after the interdialytic interval. Nephrol Dial Transplant. 2006;21:543–5.
Schilcher G, Schneditz D, Ribitsch W, Horina JH, Hoenigl M, Valentin T, Rosenkranz AR, Krause R. Loss of antimicrobial effect of trisodium citrate due to ‘lock’ spillage from haemodialysis catheters. Nephrol Dial Transplant. 2014;29:914–9.
Power A, Duncan N, Singh SK, et al. Sodium citrate versus heparin catheter locks for cuffed central venous catheters: a single center randomized controlled trial. Am J Kidney Dis. 2009;53:1034–41.
Nori US, Manoharan A, Yee J, Besarab A. Comparison of low-dose gentamicin with minocycline as catheter lock solutions in the prevention of catheter-related bacteremia. Am J Kidney Dis. 2006;48:596–605.
Filiopoulos V, Hadjiyannakos D, Koutis I, et al. Approaches to prolong the use of uncuffed hemodialysis catheters: results of a randomized trial. Am J Nephrol. 2011;33:260–8.
Schilcher G, Scharnagl H, Horina J, et al. Trisodium citrate induced protein precipitation in haemodialysis catheters might cause pulmonary embolism. Nephrol Dial Transplant. 2012;27:2953–7.
National Kidney Foundation KDOQI Work Group. KDOQI clinical practice guidelines and clinical practice recommendations for vascular access. Am J Kidney Dis. 2006;48:S176–322.
Weijmer MC, Vervloet MG, ter Wee PM. Compared to tunneled cuffed haemodialysis catheters, temporary untunnelled catheters are associated with more complications already within 2 weeks of use. Nephrol Dial Transplant. 2004;19:670–7.
Ponikvar R, Buturović-Ponikvar J. Temporary hemodialysis catheters as a long-term vascular access in chronic hemodialysis patients. Ther Apher Dial. 2005;9:250–3.
Pisoni RL, Young EW, Dykstra DM, Greenwood RN, Hecking E, Gillespie B, Wolfe RA, Goodkin DA, Held PJ. Vascular access use in Europe and the United States: results from the DOPPS. Kidney Int. 2002;61:305–16.
Bunker JP, Bendixen HH, Murphy AJ. Hemodynamic effects of intravenously administered sodium citrate. N Engl J Med. 1962;266:372–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this study have no conflict of interest. The results presented in this paper have not been published previously in whole or part, expect in abstract form. There is no funding source.
Additional information
The randomized controlled study CITRIM has compared 30 % trisodium citrate with heparin as lock solutions in 464 non-tunneled hemodialysis central venous catheters and found similar dysfunction-free survival and an increased CRBSI-free survival in heparin lock group.
Rights and permissions
About this article
Cite this article
Correa Barcellos, F., Pereira Nunes, B., Jorge Valle, L. et al. Comparative effectiveness of 30 % trisodium citrate and heparin lock solution in preventing infection and dysfunction of hemodialysis catheters: a randomized controlled trial (CITRIM trial). Infection 45, 139–145 (2017). https://doi.org/10.1007/s15010-016-0929-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-016-0929-4