Abstract
Background
Several studies have emphasized that the magnetically controlled growing rod (MCGR) technique decreases complications and costs and could be considered a safe procedure for treating patients with early onset scoliosis (EOS). To the best of our knowledge, the sagittal profile of patients with an implanted MCGR has not been sufficiently studied before.
Objective
The objectives of this study were twofold: firstly, to evaluate the influence of MCGR on the coronal, sagittal and axial planes. Secondly, to analyze changes of cervical alignment post-MCGR implantation.
Material and methods
This was a retrospective study of patients with EOS who underwent MCGR from 2012 to 2018. Patients were included if they presented with a thoracic or lumbar curvature greater than 40° (Cobb angle) and Risser’s sign 0. Global analysis of all patients was reported. Patients were stratified preoperatively by thoracic alignment into a hypokyphotic or kyphotic group. Furthermore, the study population was divided into an anteriorly aligned group and a posteriorly aligned group. Sagittal alignment parameters and parameters of coronal and axial plane were measured and the preoperative to postoperative change was compared then analyzed 1 year after surgery. No external funding was procured for this research and the authors’ conflicts of interest are not pertinent to the present work.
Results
A total of 21 patients were included in the study. There was a significant coronal correction of the structural and compensatory curves (p < 0.01). Before and after surgery, the coronal C7 plumbline was unchanged and remained within the normal range. Postoperatively, a significant derotation of the apical vertebra in thoracic and lumbar curves was observed (p < 0.05). Global analysis of the sagittal profile revealed a significant decrease of TK (p < 0.001) and T9SPi (p = 0.002) with a simultaneous significant increase of T1T3 angle (p = 0.015) and T1T4 angle (p = 0.015). No significant changes of the sagittal parameters of cervical, lumbar and spinopelvic parameters were noted. Among all groups, cervical parameters did not reveal any statistically significant changes. At 1‑year follow up the T1T3 angle (p = 0.01) and T1T4 angle (p = 0.03) were significantly increased. All other measured parameters of sagittal, coronal and axial profile were unchanged.
Conclusion
The implantation of MCGR had a significant impact on the sagittal profile. Notwithstanding, no further compensatory mechanisms of the cervical spine and pelvis had to be recruited to safeguard sagittal alignment.
Zusammenfassung
Hintergrund
Einige Studien konnten bereits zeigen, dass die Anwendung von magnetisch kontrollierten mitwachsenden Stäben (MCGR) bei Patienten mit einer Early-onset-Skoliose (EOS) sicher und weniger kostspielig für das Gesundheitssystem ist. Allerdings wurde bislang die Auswirkung des implantierten MCGR auf das sagittale Profil und die axiale Rotation noch nicht umfänglich untersucht.
Ziel der Arbeit
Ziel dieser Studie war die Evaluation der Auswirkung von MCGR auf das sagittale Alignement und die Ermittlung der koronaren und axialen Korrektur nach der Implantation der magnetisch kontrollierten mitwachsenden Stäbe.
Material und Methoden
In der retrospektiven Studie wurden 21 Patienten mit einer EOS idiopathischer Genese und operativer Behandlung mit MCGR eingeschlossen. Alle Patienten hatten einen Cobb-Winkel >40° und Risser-Zeichen 0 (Sanders ≤3). Die spinopelvinen Parameter wurden für alle Patienten erhoben. Es erfolgte eine Stratifizierung der Patienten bezüglich des thorakalen Alignments in die hypokyphotische und normokyphotische Gruppe. Ferner erfolgte die Einteilung dieser Patienten in die Gruppe mit einem anterioren Alignment (SVA >0 mm) und in die Gruppe mit einem posterioren Alignment (SVA ≤0 mm). Die Parameter des sagittalen Alignments, der koronaren und der axialen Ebene wurden gemessen und die prä- und postoperativen Daten miteinander verglichen.
Ergebnisse
Es konnte eine signifikante Korrektur der strukturellen und der kompensatorischen Kurven ermittelt werden (Cobb-Winkel; p < 0,01). Vor und nach der Operation war die koronare C7-Senkrechte unverändert und innerhalb der normalen Variationsbreite. Postoperativ zeigte sich eine signifikante Derotation der apikalen Wirbelkörper in den thorakalen und lumbalen Kurven (p < 0,05). In der Auswertung der gesamten Gruppe zeigte sich postoperativ eine signifikante Abflachung der TK (p < 0,001) und T9SPi (p = 0,002) mit gleichzeitig signifikanten Zunahme der hochthorakalen T1T3-Winkel (p = 0,015) und T1T4-Winkel (p = 0,015). Die lumbalen, zervikalen und die spinopelvinen Parameter blieben unverändert. Auch in den stratifizierten Gruppen waren die Parameter des seitlichen zervikalen Profils postoperativ unverändert. In der einjährigen Verlaufskontrolle konnte eine weitere signifikante Zunahme vom hochthorakalen T1T3-Winkel (p = 0,01) und T1T4-Winkel (p = 0,03) beobachtet werden, jedoch ohne Einfluss auf alle anderen Parameter des sagittalen Profils, der koronaren und der axialen Parameter.
Diskussion
Nach Implantation des MCGR kam es nachweislich zur Veränderungen des regionalen (thorakalen und lumbalen) seitlichen Profils, jedoch ohne Rekrutierung weiterer Kompensationsmechanismen der Halswirbelsäule und des Beckens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterior spinal distraction techniques were developed to treat pediatric patients with scoliosis and to correct spinal deformity without bone fusion or jeopardizing trunk growth. The first report was published in 1984 by Moe et al. [1] using Harrington’s instrumentation [2]. This procedure was unfortunately doomed with many implant failures, flattening of the sagittal profile and the lack of true three-dimensional correction [3]. Over the last decades the technological developments in the sphere of spinal instrumentation permitted the advent of novel techniques which revolutionized the treatment of scoliosis. One of the most recent developments is the utilization of dual rod systems which comprise the implantation of four rods through cranial and caudal midline incisions. Each set of two rods is coupled with a connector. Consequently, cranial and caudal connectors are surgically distracted at predetermined intervals.
Until 2003, the mean intervals of distraction ranged between 10 and 20 months, but the tendency now is to confine distraction to 6‑month intervals [4] in order to follow the growth in height. Performing distraction is a short, albeit an invasive procedure which is laden with postdistraction complications. The longitudinal follow-up of the study population of Bess et al. revealed an overall complication rate of 55% [5] and 58% of these complications occurred during distraction [5]. Interestingly, thoracic hyperkyphosis, which is found in approximately 30% of scoliosis patients, is a major risk factor which triples the incidence of complications and increases the likelihood of mechanical failure [6]. An additional problem which underlies traditional treatment with growing rods is the ensuing stiffness of the spine which is found in 80% of treated patients after an average of 5 distractions before patients undergo final spinal fusion [7].
To avoid these complications a magnetically controlled growing rod (MCGR) system was introduced. This method enables magnetic distraction at shorter intervals without the use of analgesia or anesthesia; however, there is a lack of long-term results due to complication rates using MCGR systems [8, 9] but there are first reports which describe MCGR to be mechanically reliable [7, 10,11,12]. An interesting aspect of using MCGR as well as conventional growing rods is the changes of coronal, axial and sagittal profiles of the spine. Despite recent attempts to highlight the influence of growing rods on the sagittal and coronal profiles, the findings of these investigations did not include detailed parameters to elucidate the changes that occur in the sagittal, coronal and axial profiles via MCGR implantation. Aside from a possible correction of the coronal and axial planes, it was hypothesized that MCGR implantation causes relevant changes of regional alignment (thoracic spine) and causes reciprocal changes in the lumbar and cervical spine.
The purpose of this study was twofold: firstly, to estimate the correction of coronal, axial and sagittal planes in early onset scoliosis (EOS) patients treated with MCGR. Secondly, to analyze the influence of sagittal thoracic alignment on the cervical and lumbar spine.
Material and methods
Patient population
This was a retrospective single center study of idiopathic EOS patients with a Cobb angle greater than 40° and Risser’s sign 0 (Sanders classification 0–3) who were treated surgically with a fusionless MCGR system between 2012 and 2018 [13, 14]. All patients were diagnosed with scoliosis before the age of 10 years and were initially conservatively managed via bracing until the scoliotic curve reached the threshold for surgery of >40°. Exclusion criteria were previous spinal surgery and patients with congenital, syndromic or neuromuscular scoliosis. Patients who fulfilled these criteria (n = 21) were included.
Radiographic acquisition
Patients underwent anteroposterior (AP) and lateral full-length X‑rays of the spine before surgery, immediately after surgery and at 1‑year follow-up. The X‑rays were taken with the patient in the standing position and in order to reduce any inaccuracies with patients barefoot and holding the arms crossed over the chest. All X‑rays in this study population fulfilled these requirements. Therefore, no patients were excluded. All data was saved as a digital imaging and communications in medicine (DICOM) file and exported from a picture archiving and communication system (PACS) to validated software to be analyzed. Surgimap® software [15] (version 2.2.13.1) was utilized to assess the different parameters included in this study. All measurements were performed by a spinal surgeon and first author (WP).
The ethics committee of the medical faculty of Heidelberg University approved this study (vote no. S‑378/2016). Radiographs of the study cohort were conducted routinely, i.e. no additional radiographs were performed in the context of this study. These radiographs were retrospectively analyzed. Hence, no informed consent of the participants was required to perform this study.
Surgical technique
The MCGR is a spinal distractible rod with an enlarged portion in the middle of the rod containing a magnetically controlled lengthening system. In all cases a dual rod construct was used. The size of the rods and anchoring screws was customized according to patient’s height and pedicle thickness. The vertebral levels for anchoring of MCGRs were defined on the basis of preoperative X‑rays of the patient in a standing position (Table 1).
A senior author (MA) performed the surgery with the patient under general anesthesia with neurological monitoring using a triggered electromyogram device and two small posterior midline incisions were performed cranially and caudally to the structural scoliotic curve. The two vertebral levels in both incisions were dissected and four pedicle screws as fixation anchors for MCGR were implanted. All screws were placed using the freehand technique based on specific anatomical landmarks [16]. Subsequently, MCGRs (standard MCGR on concave and offset MCGR on convex sites of scoliotic curve) were inserted subfascially through the cranial to distal incision and connected with the implanted pedicle screws. In the offset rods, the internal lengthening system is positioned at the opposite end of the thickened portion of the MCGR compared with the standard rod to ensure that the magnetic components do not interact during individual distraction procedures. All subjects remained free from any postoperative neurological impairment.
Data collection and radiographic analysis
Demographic and clinical characteristics of patients were obtained from medical records. Evaluation of radiographs included analysis of coronal, sagittal and axial parameters preoperatively and postoperatively. Further evaluation of radiographs at 1‑year follow-up was also performed (n = 19).
Coronal parameters
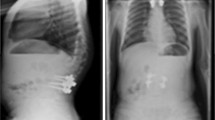
Cobb angle (Cobb), apex deviation and coronal plumbline (CorC7PL) (Fig. 1).
Sagittal parameters
Spinopelvic parameters [17]: pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), sagittal vertical axis (SVA, C7S1), T1 spinopelvic inclination (T1SPi), T9 spinopelvic inclination (T9SPi) and PI-LL mismatch (PI-LL) (Fig. 1).
Regional alignment: lumbar lordosis measured from L1 to S1 (LL), L1–L4 angle (L1L4), L4S1 angle (L4S1), thoracic kyphosis measured from T4 to T12 (TK), T1–T3 angle (T1T3), T1–T4 angle (T1T4), C1–C2 angle, C2–C7 angle (C2C7CL), C2–C7 sagittal vertical axis (cSVA, C2C7), C2 slope, T1 slope, T1–CL mismatch (Fig. 1). In terms of CL, TK and LL, negative values denote lordosis.
Axial rotation: apical vertebral rotation in thoracic spine (Raimondi 1 rotation angle), apical vertebral rotation in lumbar spine (Raimondi 2 rotation angle). Raimondi rotation angle is a reliable method for estimating vertebral rotation as projected on standard X‑rays of the spine in standing position ([18]; Fig. 1).
Patient stratification
Sagittal alignment was evaluated and compared with normative values of children and the adolescent population as published by Mac-Thiong et al. [19]. According to this normative data, patients were stratified by the thoracic alignment into a hypokyphotic (<33.1°) or kyphotic (33.1°–54.9°) group. Thoracic hyperkyphosis was defined as >54.9°. In this study population none of patients had thoracic hyperkyphosis. Secondly, the study population was divided in an anteriorly aligned group if SVA was >0 mm and a posteriorly aligned group when SVA ≤0 mm [20]. Coronal and sagittal alignments were compared in TK and SVA groups preoperatively to postoperatively. Sagittal alignment was compared between baseline and postoperative status.
Statistical analysis
Shapiro-Wilk test indicated normal distribution in all stratified groups. Descriptive statistics were reported as means and standard deviations. Preoperative to postoperative comparisons were conducted using Student’s t-test. The threshold of statistical significance was set at p < 0.05. The statistical software package SPSS 20.00 (IBM, Armonk, NY, USA) was used for statistical analysis.
Results
A total of 21 patients with a mean age at initial surgery of 9.2 ± 2.5 years (range 4–13 years) and 81% female were included in the study. Characteristics of the scoliotic curves with the respective upper and lower instrumented vertebrae are illustrated in Table 1.
Baseline and postoperative sagittal alignment parameters are reported in Table 2.
Coronal parameters
There was a significant correction of the primary, secondary and tertiary curves: primary curve Cobb angle 64.5° ± 19.9 vs. 36.1° ± 9.7; p < 0.001, secondary curve Cobb angle 44.9° ± 14.9 vs. 27.3° ± 12.6; p < 0.001 and tertiary curve Cobb angle 31.3° ± 9.4 vs. 22.7° ± 5.9; p < 0.001 (Fig. 2). Furthermore, in all groups a significant correction of apex deviation of the main curve (main curve apex deviation: 49.0 mm ± 16 vs. 28.5 mm ± 10.9; p < 0.001) was measured (Fig. 2). Before surgery, the coronal C7 plumbline was within the normal range and was not changed throughout the surgical procedure (11.1 mm ± 8.5 vs. 10.5 mm ± 8.9; p = 0.821).
Cobb angle (upper left), apex deviation (lower left), cSVA and SVA (upper right) and apical vertebral rotation (lower right) for all patients before and after surgery. Values measured in all stratified groups; p = statistical significance, p < 0.05. Vertebral rotation was estimated with Raimondi method. Raimondi 1 angle: apical vertebral rotation of thoracic curves, Raimondi 2 angle: apical vertebral rotation of lumbar curves
Axial parameters
Postoperatively, a significant derotation of apical vertebra in thoracic and lumbar curves was observed (Raimondi 1 thoracic rotation angle: 28.5° ± 9.4 vs. 16.1° ± 9.6; p < 0.001), (Raimondi 2 lumbar rotation angle: 14.3° ± 12.2 vs. 9.1° ± 7.1; p = 0.012) (Fig. 2).
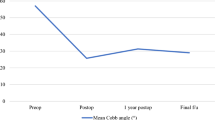
Sagittal parameters
Preoperatively to postoperatively, there was a significant decrease of TK and T9SPi (TK: 29.6° ± 11.3 vs. 19.9° ± 9.3; p < 0.001, T9SPi: −8.8° ± 5.3 vs. −5.2° ± 4.1; p = 0.002) with a simultaneous increase of T1T3 angle and T1T4 angle (T1T3 angle: 3.75° ± 3.8 vs. 6.9° ± 4.7; p = 0.015, T1T4 angle: 6.5° ± 6.7 vs. 12.8° ± 7.5; p = 0.015) (Fig. 3). Cervical, lumbar and global spinopelvic parameters were not significantly changed (Figs. 2 and 3; Table 2).
Thoracic normokyphotic group (TK ≥ 33.1°, n = 10): postoperatively, TK, LL and also T9SPi were significantly decreased (TK: 39.5° ± 5.2 vs. 25.3° ± 9.2; p < 0.001, LL: −54.0° ± 11.3 vs. −46.6° ± 12.0; p = 0.038, T9SPi: −12.6° ± 4.0 vs. −6.1° ± 4.0; p = 0.001) (Fig. 4). The segmental kyphosis of the upper thoracic part (T1T3 and T1T4) was not changed postoperatively (T1T3: 3.8° ± 5.3 vs. 7.4° ± 6.4; p = 0.298, T1T4: 8.4° ± 6.9 vs. 14.5° ± 9.3; p = 0.195) (Fig. 4). All other measured sagittal parameters of the thoracic and lumbar spine as well as pelvic parameters did not change after surgery (Fig. 4). There were also no significant changes of global balance (SVA) or sagittal parameters of the cervical spine (Table 2).
Thoracic hypokyphotic group (TK < 33.1°, n = 11): surgical procedure resulted in a decrease of TK, albeit without reaching level of significance (TK: 20.6° ± 6.6 vs. 14.9° ± 6.2; p = 0.075) (Fig. 5). Nevertheless, the segmental kyphosis of the upper thoracic part (T1T3 and T1T4) significantly increased (T1T3: 2.3° ± 3.7 vs. 6.2° ± 3.5; p = 0.037, T1T4: 4.9° ± 6.4 vs. 11.4° ± 5.7; p = 0.035) (Fig. 5). All other lumbar, thoracic and pelvic parameters did not change postoperatively (Fig. 5). Also, cervical parameters, cSVA and SVA were not changed after the surgical procedure (Table 2).
Posteriorly aligned group (SVA ≤ 0 mm) (n = 11): also this group had a significant flattening of TK, LL and changed T9SPi (TK: 34.3° ± 9.3 vs. 22.4° ± 10.8; p < 0.001, LL: −57.1° ± 9.0 vs. −50.6° ± 11.7; p = 0.046, T9SPi: −11.6° ± 4.8 vs. −7.4° ± 3.0; p = 0.004) postoperatively (Fig. 6). The T1T3 and T1T4 angles were not significantly changed (T1T3: 5.7° ± 3.1 vs. 7.4° ± 3.4; p = 0.278, T1T4: 10.4° ± 5.4 vs. 14.1° ± 5.7; p = 0.149) (Fig. 6). Corresponding to significant loss of LL, segmental lordosis L1L4 was significantly reduced (LL: −57.2° ± 9.0 vs. −50.6° ± 11.7; p = 0.046, L1L4: −26.6° ± 8.8 vs. −21.7° ± 10.5; p = 0.064) (Fig. 6). All other lumbar, thoracic and pelvic parameters were not changed preoperatively to postoperatively (Fig. 6). Also, cervical parameters cSVA and SVA did not change significantly through surgery (Table 2).
The anteriorly aligned group (SVA >0 mm) (n = 10) had postoperatively a tendency of decrease of TK without reaching the level of significance (TK: 24.5° ± 11.5 vs. 17.1° ± 6.6; p = 0.062) (Fig. 7). Interestingly, the baseline TK was notably lower than TK in the posteriorly aligned group (TK in SVA >0: 24.5° ± 11.5 vs. TK in SVA ≤0 mm: 34.3° ± 9.3). Furthermore, segmental angles T1T3 and T1T4 increased, but without reaching the level of statistical significance (T1T3: 0.3° ± 3.9 vs. 6.1° ± 6.2; p = 0.076, T1T4: 2.5° ± 5.6 vs. 11.5° ± 9.1; p = 0.055) (Fig. 7). All other estimated thoracic, lumbar and pelvic parameters did not reveal significant changes (Fig. 7). Cervical parameters, cSVA and SVA did not reveal any statistical changes pre- to postoperatively (Table 2).
Follow up evaluation
Among the 21 patients, 2 patients were excluded, 1 patient had to be excluded due to detachment of the upper thoracic screws and the other 1 because the follow-up was less than 1 year. Henceforth, 19 patients were included in this analysis. The X‑rays at 1‑year post-MCGR implantation could be evaluated and compared to X‑rays taken immediately after surgery. This analysis revealed that there was a significant increase of T1T3 angle (T1T3: 6.9° ± 4.7 vs. 10.5° ± 4.1; p = 0.001) and T1T4 angle (T1T4: 12.8° ± 7.5 vs. 17.2° ± 5.9; p = 0.003). In all stratified subgroups and for all other measured parameters of coronal, sagittal and axial planes there were no significant changes.
Discussion
The MCGR technique seems to be a potential therapeutic tool for severe scoliosis in pediatric and adolescent populations [8, 10, 11, 21,22,23,24,25,26,27]. In the literature there were some sporadic reports about complications rates post-MCGR implantation [5, 9, 28, 29] and long-term results [8, 24]; however, these reports lacked a well-founded assessment of spinal correction, especially in the sagittal and axial planes. Thus, this study attempted to address this gap to gain a deeper understanding of the impact of the MCGR procedure on spinal correction in the coronal, sagittal and axial planes.
The data show that implantation of MCGR leads to significant correction of the Cobb angle of structural and compensatory curves. In the preoperative to postoperative analysis a significant reduction of the structural curve by 45% (reduction of Cobb angle from 64.5° ± 14.9 to 36.1° ± 9.7) was observed by using the index surgery. These data are in line with the results of Dannawi et al. [30], Akbarnia et al. [21] and Cheung et al. [11] who also reported a significant Cobb angle correction in a range from 32% to 57%. A significant diminishing of apex deviation was noticed at least for primary curves which is in line with the coronal Cobb angle correction. Interestingly, axial vertebral rotation of apical vertebrae in the thoracic and lumbar spine was significantly reduced. Notably, this relevant correction in the coronal and axial planes could be achieved, although the implant system used is only composed of proximal and distal anchors (four pedicle screws proximally and four pedicle screws distally) and two MCGRs without any utilization of anchors at the apex of the scoliosis. This potential correction in the coronal and axial planes could be explained by the well-preserved flexibility of the spine in this young population. Furthermore, in all stratified groups no significant deviations from the coronal C7 plumbline were observed postoperatively. In terms of coronal correction, it can be concluded that scoliotic curves in this cohort can be well-controlled using MCGR implantation.
Previous studies of growing rod treatment for idiopathic scoliosis mainly focused on the coronal curves and only included few parameters relating to the sagittal profile, such as TK and LL [22, 31, 32]. Recently, Akbarnia et al. reported a significant flattening of TK (decrease from 50° to 35°) after growing rod implantation and first lengthening [22]; however, patients in that study were not stratified by the magnitude of TK, and hence the authors could not elucidate whether a difference existed in the evolutionary tendency of TK between patients with preoperative hypokyphosis or normokyphosis. In the present cohort, preoperative sagittal alignment was evaluated and compared with normative values of children and adolescents [19]. Therefore, the performed stratification sheds light on changes of the sagittal profile through surgery in respect to the preoperative status of TK and SVA (thoracic normokyphosis vs. thoracic hypokyphosis and anteriorly aligned SVA vs. posteriorly-aligned SVA).
Globally, the results of this study present a significant influence of MCGR implantation on the sagittal profile in terms of flattening of TK (p < 0.001) and decrease of T1SPi (p = 0.002). Furthermore, segmental compensatory mechanisms in the upper thoracic part above implanted MCGR could be observed (increase of T1T3 angle, p = 0.015 and T1T4 angle, p = 0.015). Interestingly, there was no need for compensation in the cervical spine, lumbar spine or pelvis. Secondly, the data show that MCGR implantation in normokyphotic patients causes a significant flattening of TK (p < 0.001) and a significant decrease of T9SPi (p = 0.001) and a tendency to decrease of T1SPi albeit without reaching statistical significance (p = 0.069). The change of TK has a direct influence on LL which is also decreased (p = 0.038). Furthermore, these patients are preoperatively and postoperatively still well-compensated regarding sagittal global alignment (SVA without significant changes and in normal range). In this group, the changes of regional profile of the thoracic spine would be compensated by the lumbar spine without taking any compensatory mechanisms of the pelvis (PT without significant changes and in normal range; p = 0.981). On the other hand, the thoracic hypokyphotic group revealed a postoperative tendency of further flattening but without reaching the level of significance. Similarly, no other regional parameters for the thoracic and lumbar spine were significantly changed. These patients were postoperatively slightly posteriorly aligned (SVA) but without reaching the level of significance. Hence, the pelvis in these patients was not recruited for compensation of the sagittal profile (PT without significant changes and in normal range).
To elucidate whether MCGR implantation has an impact on global sagittal alignment, the patients were stratified according to the SVA. For both groups (SVA ≤0 mm vs. SVA >0 mm) there was no significant change of SVA preoperatively to postoperatively. In other words, global alignment was not affected in this cohort; however, in the SVA ≤0 mm group a significant flattening of TK (p = 0.001), a significant decrease of T9SPi (p = 0.004) and consequently significant flattening of LL (p = 0.046) were noticed. In the SVA >0 mm group, TK was postoperatively flattened without reaching a level of significance (p = 0.062). All other regional parameter for the thoracic and lumbar spine were not changed. In both groups, no pelvic compensatory mechanisms were recruited as these parameters did not change postoperatively. These findings could suggest that there is a potential interdependence between regional thoracic and lumbar spine following MCGR implantation. Furthermore, surgery-induced changes of the thoracic spine (TK flattening, T9SPi decrease) are neutralized by compensatory flattening of the lumbar spine. Finally, SVA remained within the normal range without recruitment of pelvic compensatory mechanisms.
In addition, significant segmental compensation mechanisms of the upper thoracic part were observed in the thoracic hypokyphotic group. The MCGR implantation led to further flattening of the TK. Simultaneously, the subsequent upper thoracic segments reacted with a significant increase of segmental kyphosis angle (T1T3 and T1T4 angles). This phenomenon can be explained by the malleability of the spine and greater segmental range of motion in this young population.
Henceforth, it could be concluded that MCGR-induced changes of TK and global T9SPi inclination can be well-compensated by few spinal segments in the upper and lower segments. Through the sufficient compensation mechanisms in segments located in the vicinity to implanted MCGR (upper thoracic spine and lumbar spine (T1–T3, T1–T4, LL)), there was no need for recruitment of cervical or pelvic compensatory mechanisms to safeguard sagittal balance.
Coronal correction, system lengthening and complication rates post-MCGR treatment were preliminarily evaluated [8, 10, 11, 21, 28, 29, 33,34,35] without considering the sagittal profile. To our best knowledge, this is the first study that analyzed potential changes of regional and global sagittal profile of the spine in young patients in the context of MCGR. The present data revealed that MCGR implantation induces flattening of TK and may trigger a chain of reactions which influences upper and lower spinal segments (upper thoracic part and lumbar part). Consequently, it is believed that surgeons should contemplate potential sagittal profile changes during preoperative planning of MCGR implantation.
Previously, the problem of TK and LL flattening using Harrington’s instrumentation for scoliosis treatment was reported [36, 37]. In a meta-analysis by Lykissas et al. they evaluated 27 studies and 1613 patients with adolescent idiopathic scoliosis (AIS) who were treated with Harrington’s instrumentation [36]. They confirmed the negative effect of this system on sagittal alignment. Thoracic spine flattening post-MCGR treatment remains a challenge to using Harington’s instrumentation. This phenomenon might be caused by the structural condition of scoliosis and by the proximal anchoring screws which are predominantly implanted in the upper thoracic vertebra, and distally in the lower thoracic or upper lumbar vertebrae. Consequently, the rod’s internal lengthening mechanism is mostly implanted in the lower thoracic part. Internal lengthening mechanism is an intrinsic part of MCGR that cannot be bent. Normally, the lower thoracic part of the spine is kyphotic. The implantation of MCGR with distraction mechanism that is applied in lower thoracic spine part may automatically lead to loss of TK. Physiologically, the thoracolumbar junction is a part of spine that has almost no kyphosis. The implantation of MCGR with the rod lengthening mechanism in the thoracolumbar region might have less effect on the sagittal profile. Hence, it is suggested that the implantation of MCGR distraction mechanism should be performed in the thoracolumbar region to counteract flattening of TK. Secondly, the anchoring part of the implanted pedicle screws is located in the vicinity of the vertebral facet joints and transverse processes. To reduce autofusion rate, the rods of MCGR should be directly subfascially inserted. This condition may be surgically challenging while bending the rods. In cases of insufficiently bent rods, the subfascially inserted internal distraction mechanism may act as an additional fulcrum that consequently leads to loss of TK.
The analysis at 1‑year follow-up revealed a significant cranial increase in thoracic segmental kyphosis (T1T3 and T1T4) compared to immediate postoperative status. This phenomenon could be explained by the distraction of the MCGR, the flattening effect of the rod on the thoracic profile, the malleability of the spine and greater segmental range of motion in this young population; however, future studies are warranted to analyze the effect of MCGR distraction and its influence on the sagittal profile. Sagittal, coronal and axial parameters were unchanged. This could be explained by the fact that magnetic distraction was performed in concert with physiological growth.
One of the limitations of this study is the absence of a control group; however, ethical considerations about unnecessary X‑radiation in normal young volunteers (controls) were prohibitive. The retrospective design is acknowledge as another limitation. Furthermore, the follow-up analysis was performed only after 1 year, which could be considered a short examination period for substantiated conclusions. Hence, reporting the clinical and radiological follow-up of more than 1 year after MCGR implantation is still warranted. Finally, it is conceded that our study population could not be stratified based on the Lenke classification which would result in very small subgroups. Thus, the preoperative to postoperative TK and SVA are considered to be more appropriate for the study cohort. These limitations notwithstanding, the retrospective preoperative to postoperative analysis revealed important observations and enabled the complex relationships between different parts of the spine to be disentangled in the context of MCGR treatment.
Conclusion
This exploratory study revealed MCGR implantation to be effective in the management of EOS. Although implant-related changes of the regional thoracic and lumbar profiles could be noted, no further compensatory mechanisms of the cervical spine or pelvis had to be recruited to safeguard sagittal balance. Further longitudinal investigations with a minimum of 2 years follow-up are required to determine the influence of MCGR implantation on the sagittal profile whilst monitoring spinal growth.
Key points
-
MCGR is a potential therapeutic tool for severe scoliosis in patients with EOS.
-
MCGR has a significant influence on the sagittal profile in terms of flattening of TK and decrease of T9SPi.
-
At 1‑year follow-up, there was an increase of segmental kyphosis cranially (T1T3 and T1T4). All other sagittal, coronal and axial parameters did not exhibit a statistically significant change.
-
Segmental compensatory mechanisms in the vicinity of implanted MCGR excluded the need for recruitment of cervical or pelvic compensatory mechanisms to safeguard sagittal balance.
-
The implantation of the MCGR distraction mechanism should be performed in the thoracolumbar region to counteract flattening of TK.
Abbreviations
- C2–C7 CL:
-
Cervical lordosis from C2 to C7
- cSVA:
-
Cervical sagittal vertical axis
- DICOM:
-
Digital imaging and communications in medicine
- L1L4:
-
Angle measured from L1 to L4
- L4L5:
-
Angle measured from L4 to L5
- LL (L1-S1):
-
Lumbar lordosis measured from L1 to S1
- PACS:
-
Picture archiving and communication system
- PI:
-
Pelvic incidence
- PI-LL:
-
Mismatch PI-LL
- PT:
-
Pelvic tilt
- SS:
-
Sacral slope
- SVA:
-
Sagittal vertical axis
- T1-CL:
-
Mismatch T1-CL
- T1SPi:
-
T1 spinopelvic inclination
- T1T3:
-
Angle measured from T1 to T3
- T1T4:
-
Angle measured from T1 to T4
- T9SPi:
-
T9 spinopelvic inclination
- TK:
-
Thoracic kyphosis measured from T4 to T12
References
Moe JH, Kharrat K, Winter RB, Cummine JL (1984) Harrington instrumentation without fusion plus external orthotic support for the treatment of difficult curvature problems in young children. Clin Orthop Relat Res 185:35–45
Harrington PR (1973) The history and development of Harrington instrumentation. Clin Orthop Relat Res 93:110–112
Hasler CC (2013) A brief overview of 100 years of history of surgical treatment for adolescent idiopathic scoliosis. J Child Orthop 7(1):57–62
Campbell RM Jr., Smith MD, Hell-Vocke AK (2004) Expansion thoracoplasty: the surgical technique of opening-wedge thoracostomy. Surgical technique. J Bone Joint Surg Am 86-A(Suppl 1):51–64
Bess S, Akbarnia BA, Thompson GH et al (2010) Complications of growing-rod treatment for early-onset scoliosis: analysis of one hundred and forty patients. J Bone Joint Surg Am 92(15):2533–2543
Schroerlucke SR, Akbarnia BA, Pawelek JB et al (2012) How does thoracic kyphosis affect patient outcomes in growing rod surgery? Spine 37(15):1303–1309
Odent T, Ilharreborde B, Miladi L et al (2015) Fusionless surgery in early-onset scoliosis. Orthop Traumatol Surg Res 101(6 Suppl):S281–S288
Yilmaz B, Eksi MS, Isik S, Ozcan-Eksi EE, Toktas ZO, Konya D (2016) Magnetically controlled growing Rod in early-onset scoliosis: a minimum of 2‑year follow-up. Pediatr Neurosurg 51(6):292–296
Thakar C, Kieser DC, Mardare M, Haleem S, Fairbank J, Nnadi C (2018) Systematic review of the complications associated with magnetically controlled growing rods for the treatment of early onset scoliosis. Eur Spine J. https://doi.org/10.1007/s00586-018-5590-4
La Rosa G, Oggiano L, Ruzzini L (2017) Magnetically controlled growing rods for the management of early-onset scoliosis: a preliminary report. J Pediatr Orthop 37(2):79–85
Cheung KM, Cheung JP, Samartzis D et al (2012) Magnetically controlled growing rods for severe spinal curvature in young children: a prospective case series. Lancet 379(9830):1967–1974
Eltorai AEM, Fuentes C (2018) Magnetic growth modulation in orthopaedic and spine surgery. J Orthop 15(1):59–66
Scoles PV, Salvagno R, Villalba K, Riew D (1988) Relationship of iliac crest maturation to skeletal and chronologic age. J Pediatr Orthop 8(6):639–644
Sanders JO, Khoury JG, Kishan S et al (2008) Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am 90(3):540–553
Akbar M, Terran J, Ames CP, Lafage V, Schwab F (2013) Use of Surgimap Spine in sagittal plane analysis, osteotomy planning, and correction calculation. Neurosurg Clin N Am 24(2):163–172
Puvanesarajah V, Liauw JA, Lo SF, Lina IA, Witham TF (2014) Techniques and accuracy of thoracolumbar pedicle screw placement. World J Orthop 5(2):112–123
Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20(4):451–462
Weiss HR (1995) Measurement of vertebral rotation: Perdriolle versus Raimondi. Eur Spine J 4(1):34–38
Mac-Thiong JM, Labelle H, Berthonnaud E, Betz RR, Roussouly P (2007) Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J 16(2):227–234
Akbar M, Almansour H, Lafage R et al (2018) Sagittal alignment of the cervical spine in the setting of adolescent idiopathic scoliosis. J Neurosurg Spine 29(5):506–514
Akbarnia BA, Cheung K, Noordeen H et al (2013) Next generation of growth-sparing techniques: preliminary clinical results of a magnetically controlled growing rod in 14 patients with early-onset scoliosis. Spine 38(8):665–670
Akbarnia BA, Marks DS, Boachie-Adjei O, Thompson AG, Asher MA (2005) Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicenter study. Spine 30(17 Suppl):46–57
Akbarnia BA, Mundis GM Jr., Salari P, Yaszay B, Pawelek JB (2012) Innovation in growing rod technique: a study of safety and efficacy of a magnetically controlled growing rod in a porcine model. Spine 37(13):1109–1114
Akbarnia BA, Pawelek JB, Cheung KM et al (2014) Traditional growing rods versus magnetically controlled growing rods for the surgical treatment of early-onset scoliosis: a case-matched 2‑year study. Spine Deform 2(6):493–497
Bekmez S, Dede O, Yazici M (2017) Advances in growing rods treatment for early onset scoliosis. Curr Opin Pediatr 29(1):87–93
Cheung JP, Samartzis D, Cheung KM (2014) A novel approach to gradual correction of severe spinal deformity in a pediatric patient using the magnetically-controlled growing rod. Spine J 14(7):e7–e13
Hickey BA, Towriss C, Baxter G et al (2014) Early experience of MAGEC magnetic growing rods in the treatment of early onset scoliosis. Eur Spine J 23(Suppl 1):S61–S65
Choi E, Yaszay B, Mundis G et al (2017) Implant complications after magnetically controlled growing rods for early onset scoliosis: a multicenter retrospective review. J Pediatr Orthop 37(8):e588–e592
Kwan KYH, Alanay A, Yazici M et al (2017) Unplanned Reoperations in Magnetically Controlled Growing Rod Surgery for Early Onset Scoliosis With a Minimum of Two-Year Follow-Up. Spine 42(24):E1410–E1414
Dannawi Z, Altaf F, Harshavardhana NS, El Sebaie H, Noordeen H (2013) Early results of a remotely-operated magnetic growth rod in early-onset scoliosis. Bone Joint J 95-B(1):75–80
Thompson GH, Akbarnia BA, Kostial P et al (2005) Comparison of single and dual growing rod techniques followed through definitive surgery: a preliminary study. Spine 30(18):2039–2044
Acaroglu E, Yazici M, Alanay A, Surat A (2002) Three-dimensional evolution of scoliotic curve during instrumentation without fusion in young children. J Pediatr Orthop 22(4):492–496
Gilday SE, Schwartz MS, Bylski-Austrow DI et al (2018) Observed length increases of magnetically controlled growing rods are lower than programmed. J Pediatr Orthop 38(3):e133–e137
Ridderbusch K, Rupprecht M, Kunkel P, Hagemann C, Stucker R (2017) Preliminary results of magnetically controlled growing rods for early onset scoliosis. J Pediatr Orthop 37(8):e575–e580
Ahmad A, Subramanian T, Panteliadis P, Wilson-Macdonald J, Rothenfluh DA, Nnadi C (2017) Quantifying the ‘law of diminishing returns’ in magnetically controlled growing rods. Bone Joint J 99-b(12):1658–1664
Lykissas MG, Jain VV, Nathan ST et al (2013) Mid- to long-term outcomes in adolescent idiopathic scoliosis after instrumented posterior spinal fusion: a meta-analysis. Spine 38(2):E113–E119
Schlenzka D, Poussa M, Muschik M (1993) Operative treatment of adolescent idiopathic thoracic scoliosis. Harrington-DTT versus Cotrel-Dubousset instrumentation. Clin Orthop Relat Res 297:155–160
Funding
No funding was received in support of this work. Relevant financial activities outside the submitted work: consultancy, grants, royalties, stocks, patents.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to this article. MA, BD, WP contributed to the conception and design of the study. Data collection was performed by WP. Data analyses were performed by WP, HA, BD and MA. All authors contributed to the interpretation of the results, revision and correction of the report, which was drafted by WP, HA and MA. All named authors read, revised and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
W. Pepke, H. Almansour, B.G. Diebo and M. Akbar declare that they have no competing interests.
The ethics committee of the medical faculty of Heidelberg University approved this study. Vote no. S‑378/2016. Radiographs of the study cohort were conducted routinely, i.e. no additional radiographs were performed in the context of this study. These radiographs were retrospectively analyzed. Hence, no informed consent was required to perform this study.
Additional information
The manuscript submitted does not contain information about medical device(s)/drug(s).
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
FDA device/drug status
The implants used in this study are FDA approved.
Rights and permissions
About this article
Cite this article
Pepke, W., Almansour, H., Diebo, B.G. et al. Correction of the spine with magnetically controlled growing rods in early onset scoliosis. Orthopäde 49, 1086–1097 (2020). https://doi.org/10.1007/s00132-019-03801-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-019-03801-x