Abstract
Background
No previous epidemiological studies of child mental health have been conducted in Bangladesh, partly due to lack of suitable measures.
Methods
A Bangla translation of a standardised child psychiatric interview, the Development and Well-Being Assessment (DAWBA), was validated against routine clinical diagnoses on a consecutive series of 100 referrals to a child mental health service. A two-phase study of prevalence was applied to random samples of 5- to 10-year-olds (N=922) drawn from three contrasting areas: a rural area, a moderately prosperous urban area, and an urban slum.
Results
There was substantial agreement between the DAWBA and the independent clinic diagnosis (kappa=0.63–0.94). The estimated prevalence of any ICD-10 diagnosis was 15% (95% CI 11–21%). The rate of obsessive–compulsive disorder was higher than in previous studies. Children from the slum area were significantly more likely to have serious behavioural problems, and marginally more likely to have post-traumatic stress disorder.
Conclusion
A conservative extrapolation is that around 5 million Bangladeshi children and adolescents have psychiatric disorders. In a country with very few child mental health professionals, there is a vast gap between need and provision that must be addressed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Epidemiological studies of child and adolescent psychiatric disorders in the developing world have generated prevalence estimates ranging from 1 to 49% [18]. However, most of these studies lack one or more of the methodological features required for generating believable prevalence estimates, namely: an adequate sample size, a representative sampling frame, standardized assessment measures that are suitable for generating exact diagnoses (as opposed to use of screening questionnaires alone), explicit and internationally accepted diagnostic criteria, and assessment not just of symptoms but also of resultant distress and social impairment [8]. The studies that do meet these crucial methodological requirements report a range of prevalence ranging from 5 to 18% [4–6, 8, 19].
Bangladesh is a low-income nation with a total population of 124 million people, of whom 45% are under the age of 18 years [2]. Measures of poverty and deprivation include the following: an infant mortality rate of 53 per thousand live births; an adult literacy rate of 54 and 41% for males and females, respectively; and a per capita gross national income of US$444 [2, 3]. The country is very prone to floods and cyclones, reflecting the fact that it is largely made up of river deltas, with about 75% of the land being less than 3 m (10 ft) above sea level. There have been no epidemiological studies of the prevalence of child and adolescent psychiatric disorders in Bangladesh, and indeed there are no validated psychiatric measures in Bangla (Bengali) that could be used for this purpose. The present study translated and validated a standardised child psychiatric assessment and applied it to three contrasting community samples: a rural area, a moderately prosperous urban area, and an urban slum. The purposes of the study were: (1) to validate psychiatric measures in Bangla; (2) to generate approximate prevalence estimates as a guide to future research and service planning; (3) to explore differences in types and rates of psychopathology between rural, urban and slum areas; and (4) to provide methodological foundations for more extensive and representative epidemiological studies in Bangladesh in the future.
Subjects and methods
Overview
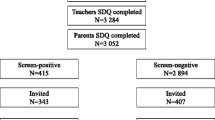
Two main measures of psychopathology were employed: the Strengths and Difficulties Questionnaire (SDQ), which is a brief screening measure, and the Development and Well-Being Assessment (DAWBA), which is a much more extensive suite of interviews, questionnaires and rating techniques for generating psychiatric diagnoses. Bangla versions of the SDQ have previously been validated [22]. In this study, a Bangla translation of the DAWBA was validated against routine clinical diagnoses on a consecutive series of referrals to a child mental health service. Test–retest reliability was established on a subset of this clinic sample. The SDQ and DAWBA were then applied in a two-phase design to random samples of 5- to 10-year-olds from three contrasting areas: a rural area, a moderately prosperous urban area, and an urban slum. In the first phase, SDQs were administered to parents and teachers, and parents were also asked about socio-demographic factors. Possession of consumer goods such as a refrigerator was used as an index of socioeconomic status, following precedents from other developing countries [1]. In the second phase, the DAWBA was applied to all screen-positive children and a random sample of screen-negative children. Ethical permission for the study was obtained from the Bangabadhu Sheikh Mujib Medical University in Dhaka and the Institute of Psychiatry in London.
Subjects
A clinical sample of one hundred 5- to 17-year-olds was obtained by approaching the families of consecutive new referrals to a child psychiatric clinic in Dhaka in 2002. A total of 116 families were approached in order to obtain a total of 100 participating families (participation rate 86%). The research team administered both screening and detailed measures of psychopathology for all 100 subjects, who were also independently assigned a diagnosis by the clinic blind to the research assessment. The mean age of the clinic sample was 11.3 years (SD 3.3 years); 59 of the subjects were male. Parents and teachers provided information on all 100 children. Of the 49 children who were 11 or older, 45 (92%) provided information about themselves. The research diagnostic assessment was repeated an average of 3 weeks later by a different interviewer on a randomly chosen 25 subjects.
Community samples were obtained in 2004 from three contrasting areas. The three areas have clear geographical and administrative boundaries, include between 14,000 and 37,000 inhabitants each, and were chosen after informal local consultation as representative exemplars of that sort of area (rural, urban, slum). The rural area is located 30 km (20 miles) outside of Dhaka, the capital city, but despite this apparent proximity to the city, it is fairly isolated with the journey by bus to the city taking about 3 h and involving a ferry crossing. The moderately prosperous urban area is a residential zone in Dhaka that was established about 50 years ago; most families are of medium socioeconomic status and literate. The urban slum was relatively recently established on the periphery of Dhaka, and consists of very crowded, low-quality dwellings without adequate sanitation; most of the adults in the slum moved to Dhaka because of unemployment, or after losing their homes due to flooding. Community samples of 5- to 10-year-olds in each of the three areas were obtained by random sampling from the electoral registers. The overall participation rate for families with 5- to 10-year-old children was 75%, ranging from 66% for the slum to 97% for the rural area (Table 1). There were no exclusion criteria. When a participating family included more than one 5- to 10-year-old, just one of these children was chosen at random. In the first phase of the study, screening questionnaires and socio-demographic measures were obtained on all subjects. Parents provided SDQs and socio-demographic information on all subjects, but teacher SDQs were only obtained on 88% of rural children, 98% of urban children, and 65% of slum children (chi-square=132.4, 2 df, p<0.001), partly reflecting differences in school attendance.
Limited resources meant that it was only possible to carry out DAWBA assessments on one in five subjects; the families invited to take part in the second phase were all those whose children were screen positive in the first phase, plus a random sample of those who were screen negative (adjusting the sampling fraction for the screen negative so as to achieve an overall sampling fraction of around 20% in each of the three areas). All families invited to take part in the second phase agreed to do so. Table 1 shows how many screen-positive and screen-negative subjects from each area were assessed in the second phase. The DAWBA assessment involved a parent interview in all cases, but teacher DAWBAs were only obtained on 94% of rural children, 97% of urban children, and 69% of slum children (chi-square=27.2, 2 df, p<0.001).
Measures
The screening measure of psychopathology was the Bangla translation of the Strengths and Difficulties Questionnaire (SDQ; [22]). The SDQ asks about 25 attributes, some positive and some negative. The items cover emotional symptoms, conduct problems, hyperactivity, peer problems, and prosocial behaviours. A brief impact supplement asks whether the respondent thinks that the child has a problem, and if so, inquires further about overall distress, social impairment, burden and chronicity [11]. The informant version of the SDQ can be completed in about 5 min by parents or teachers of children aged 4–16 [10]. The SDQ was shown to be of acceptable reliability and validity, performing at least as well as lengthier and longer-established alternatives [12]. The web site http://www.sdqinfo.com provides more information on SDQ plus downloadable versions of the questionnaires in many languages. The versions of the SDQ used in this study were the informant versions including impact supplements [10, 11]. The Bangla translation of the SDQ has been validated in Bangladesh [22]. Parents were seen by interviewers who gave respondents the choice of completing paper versions of the questionnaires or having them administered as structured interviews—the latter is an important option in a society with high levels of illiteracy. Teachers were sent paper versions of the questionnaires. It is common in Bangladesh for children to have home tutors as well as schoolteachers. The teacher questionnaire was sent to the school in the first instance, unless the family felt that the schoolteacher did not know the child as well as the home tutor. When teacher questionnaires were sent to the school but not returned, home tutors (if available) were asked to complete the questionnaires instead. Children were taken to be screen positive in the first phase of the study if they were classified as ‘probable’ psychiatric cases (as opposed to ‘possible’ or ‘unlikely’ psychiatric cases) by a computer algorithm based on the information from all available SDQs; this predictive algorithm has previously been shown to function well in a Bangladeshi child and adolescent mental health clinic [14].
The research assessment of psychiatric disorder was carried out using the Development and Well-Being Assessment (DAWBA; [13]). This uses a mixture of closed and open questions about child psychiatric symptoms and their impact (i.e. resultant distress and social impairment). It is administered as an interview to parents and as an abbreviated questionnaire to teachers. The interviews are administered by lay interviewers who also record verbatim accounts of any reported problems, but do not rate them. Experienced clinicians subsequently review both the verbatim accounts and the answers to structured questions before assigning Axis 1 diagnoses according to ICD-10 criteria [27]. Previous studies have provided evidence for the validity of the DAWBA in English [13, 9] and Portuguese [8]. The DAWBA was translated into Bangla by the first author (M.S.I.M.) and then independently back-translated into English by seven Bangladeshis with excellent proficiency in both English and Bangla. The back-translations were compared with the original English versions, identifying a small number of discrepancies that were then resolved by panel discussion. The translated assessments were piloted on 15 families of mixed social backgrounds attending a child and adolescent mental health service; feedback from the respondents and interviewers guided the final adjustments in wording to maximise comprehensibility and cultural appropriateness. Further information on the DAWBA is available at http://www.dawba.com—including downloadable versions of the measures in English and Bangla as well as on-line demonstrations of the clinical rating process. In this study, all open-ended comments were translated from Bangla into English, and DAWBA diagnoses were assigned by the second author (R.G.), an experienced child psychiatrist who has previously carried out or supervised over 20,000 clinical ratings using the DAWBA. In the case of the clinic sample, the research diagnoses made by the second author were assigned blind to the diagnoses assigned by the clinic (and were not discussed with the first author since he had generated the clinic diagnoses). In the case of the community samples, the research diagnoses made by the second author were subsequently discussed with the first author to ensure that cultural context had been adequately allowed for, and that diagnoses were not being assigned to culturally sanctioned variations within the normal range—a process particularly relevant to obsessive–compulsive disorder, post-traumatic stress disorder and behavioural disorders. To avoid small cell sizes for subsequent analyses, diagnoses were grouped into emotional disorders (including anxiety, depressive and obsessive–compulsive disorders), hyperkinesis, and behavioural disorders (including oppositional–defiant and other conduct disorders). Although children in developing countries may be referred to psychiatric clinics because they have learning difficulties or physical disorders such as epilepsy, the DAWBA diagnoses only extend to Axis 1 psychiatric disorders. Parents’ open-ended comments made it clear that some of the children included in the study did have physical or learning disabilities (their presence was not an exclusion criterion), but in the absence of any standardised measure of these additional disabilities, their rate cannot usefully be reported.
For the clinic sample, the clinic diagnoses were assigned by the first author (M.S.I.M.), who is the senior child psychiatrist in charge of that child and adolescent mental health outpatient clinic. All diagnoses were phenomenologically based, drawing on extensive information on symptoms and resultant impact reported by multiple informants. Clinic diagnoses were made according to the operational criteria of ICD-10 [27] and were allocated blind to the DAWBA assessment and diagnosis. Diagnoses were grouped into emotional disorders, hyperkinesis and behavioural disorders.
Statistical analysis
Whereas the first phase was a simple random sample and did not require weighting, the second phase did require weighting to adjust for the disproportionate sampling of screen positive children. Statistical analyses were performed using the Statistics/Data Analysis Program (STATA 8) survey program, which adjusts appropriately for weighting when calculating test statistics and 95% confidence intervals.
Results
Validity and reliability in the clinic sample
Of the 100 clinic patients, 93 were assigned a DSM-IV diagnosis by the clinic. Emotional, hyperkinetic and behavioural disorders were diagnosed by the clinic in 55, 32 and 21 children, respectively, with some children being assigned diagnoses from more than one group. The validity of the DAWBA diagnoses was assessed by examining their level of agreement with the clinic diagnoses—the DAWBA and clinic diagnoses were completely independent of one another, being based on separate assessments made by different interviewers and then rated by different clinicians. The results are shown in Table 2. For example, the second row of data shows the level of agreement for getting an ICD-10 emotional disorder: 55 children had an emotional disorder according to the clinic, of whom 53 were also diagnosed as having an emotional disorder by the DAWBA (sensitivity 96%); conversely, 45 children did not have an emotional disorder according to the clinic, of whom only one child had an emotional disorder according to the DAWBA (specificity 98%). Kappa values between 0.63 and 0.94 (fourth column of table) reflect a high level of agreement between DAWBA diagnoses and clinic diagnoses. Sensitivities ranged from 63 to 94% (third column of table) and specificities ranged from 81 to 100% (100% minus second column of table). The DAWBA was more likely to diagnose behavioural disorders than the clinic, whereas the reverse was true for hyperkinesis. The clinic sample of 100 children spanned the 5–17 age range of the DAWBA. Since the community sample came from the more restricted 5–10 age range, it is also relevant to present the kappa values (asymptotic standard error) for the 51 clinic children aged 5–10 years: 0.64 (0.19) for any disorder, 0.88 (0.07) for emotional disorders, 0.57 (0.11) for hyperkinesis, and 0.48 (0.12) for behavioural disorders.
Table 3 presents test–retest agreement for DAWBA diagnoses when the assessment was repeated an average of 3 weeks later by different interviewers. Kappa values between 0.50 and 0.91 reflect a moderately high level of agreement, although it is important to note that the standard errors are large because the repeated assessments were carried out on a random sample of only 25 children. With only 12 children aged 5–10 in the test–retest sample, it was not appropriate to generate kappa values for this age range separately.
Characteristics of the three community samples
As shown in Table 4, there were small but statistically significant differences in the mean ages of the three community samples, but no differences in the gender balance. The urban area was the most educationally and materially advantaged, as judged by literacy levels and the possession of a refrigerator. By contrast, the rural area had the highest rating for neighbourhood helpfulness and the lowest rating for neighbourhood danger. The slum area did worst in all respects.
Predictive validity of screening in the community samples
All 922 children in the community samples were assessed with the SDQ in the first phase of the study, but practical constraints only permitted about 20% of these to be assessed using the DAWBA in the second phase. All 59 children who were screen positive in the first phase were assessed with the DAWBA, of whom 90% (53) were assigned at least one ICD-10 diagnosis; 149 randomly selected children who were screen negative were also assessed with the DAWBA, of whom 10% (15) were assigned at least one ICD-10 diagnosis (chi-square=122.2, 1 df, p<0.001). If the SDQ screen-negative children were subdivided into those predicted to be ‘possible’ and ‘unlikely’ cases by the predictive algorithm [14], then at least one ICD-10 diagnosis was made for 16% (12/76) of the possible cases and 4% (3/73) of the unlikely cases. Examining all three community samples separately, there were highly significant differences between the rates of psychiatric diagnoses for screen positive and negative children in each area: 92 vs 12% for rural children (chi-square=33.0, 1 df, p<0.001); 92 vs 6% for urban children (chi-square=39.2, 1 df, p<0.001); 89 vs 12% for slum children (chi-square=46.0, 1 df, p<0.001).
Prevalence of psychiatric disorder in the three community samples
Table 5 summarises the prevalence estimates for ICD-10 psychiatric disorders in the three areas, with confidence intervals and test statistics adjusted for the two-phase design with weighting. Three specific features of the pattern of area differences and similarities warrant further comment.
Firstly, within the behavioural disorders, the association with area varied strikingly according to the type and severity of behavioural problem. Children from all three areas had similar rates of oppositional–defiant disorder, involving behaviours such as temper outbursts, arguing with adults, refusing to follow rules, annoying others on purpose, and irritability. By contrast, children from the slum were substantially more likely to have more serious conduct disorders, involving behaviours such as stealing, use of weapons, deliberate cruelty to people or animals, and repeatedly staying out late without permission.
Secondly, post-traumatic stress disorder was more likely to affect the children from the slum, although this was only marginally statistically significant. The relevant traumatic events for the six affected children (five from the slum, one from the rural area) were as follows. A 9-year-old boy from the slum witnessed neighbouring households set alight after an episode of gang violence. An 8-year-old girl from the slum was in a rickshaw with her mother when they were hit by a bus, leaving her mother unconscious. Another 8-year-old girl from the slum was present when a group tried to evict the family by force from their home. A 6-year-old boy from the slum escaped from the family home after it had deliberately been set on fire while they were all asleep. A 10-year-old girl from the slum witnessed a person being shot dead by a gang. An 8-year-old boy from the rural area was beaten up along with all the rest of the family as the result of a feud.
Thirdly, the prevalence of obsessive–compulsive disorder was high across all three areas. The obsessions and compulsions of the five children can be summarised as follows. A 9-year old girl from the slum engaged in excessive cleaning and washing, repetitive walking and counting, and had obscene thoughts, for which she feared punishment by God. A 6-year-old girl from the slum has obscene thoughts about God and prayed a lot for forgiveness. A 10-year-old girl from the rural area worried constantly that she, her siblings and her mother would die; she feared that God was angry with her and repeatedly crossed herself to avoid punishment; and she also engaged in excessive washing and cleaning, as well as repeated checking of her work. A 10-year-old girl from the urban area engaged in prolonged and repeated hand washing, only stopping when others forced her to do so, resulting in considerable teasing and distress at school. A 6-year-old from the urban area was very concerned about dirt and washed his hands, body and clothes a lot; he feared he was not properly clean for prayers and that God might be angry; and he also repeatedly checked his school bag and school work.
Discussion
This study generated both methodological and substantive findings of interest. Methodologically, the study provided the first evidence for the validity of the Bangla version of the Development and Well-Being Assessment (DAWBA), as well as confirming and extending previous validation studies of the Bangla version of the Strengths and Difficulties Questionnaire (SDQ; [14, 22]). Substantively, the study suggests that around 10–20% of Bangladeshi 5- to 10-year-olds have emotional and behavioural problems that are severe enough to result in substantial distress or social impairment, thereby warranting a psychiatric diagnosis, and probably warranting treatment, too. Children from the slum were substantially more likely than children from the other two areas to have serious conduct problems and the same might apply to post-traumatic stress disorder.
Psychometric properties of the Bangla translation of the DAWBA
Within the clinic sample, there was substantial agreement between the DAWBA diagnosis and the independent diagnosis made by clinicians. The DAWBA generated more diagnoses of behavioural disorders, whereas the clinicians generated more diagnoses of hyperkinesis. In the absence of a true ‘gold standard’, we currently have no way of telling whether the DAWBA or the clinic was more accurate in this respect. It was not possible to compare the DAWBA diagnoses with diagnoses generated with previously validated measures since no such measures exist in Bangla. In the longer term, it will be important to establish how well DAWBA diagnoses predict prognosis and response to treatment since this sort of predictive validity is of great practical relevance to clinicians. Test–retest reliability was satisfactory. On the basis of the available evidence from this study and from previous studies of the DAWBA in developed and developing countries [13, 8], the DAWBA would appear to be a suitable assessment tool for both clinical and research purposes in Bangladesh.
Psychometric properties of the Bangla translation of the SDQ
The first validation study of the SDQ in Bangla demonstrated in a clinic sample that there was substantial agreement between the SDQ ‘caseness’ predictions and an independent psychiatric diagnosis [14]. A second validation study demonstrated that mean SDQ scores differed markedly between clinic and community samples [22]. This study extends previous validation studies by demonstrating that SDQ ‘caseness’ predictions in diverse community samples are substantially confirmed by independent psychiatric assessments. Overall, the likelihood of being assigned a psychiatric diagnosis was 90% for children predicted to be ‘probable’ cases by the SDQ, compared to 16% for children predicted to be ‘possible’ cases, and 4% for children predicted to be ‘unlikely’ cases. The caseness predictions worked well in all three communities studied. These findings suggest that the multi-informant SDQ might have a useful role in community screening. In particular, since 90% of children with ‘probable’ caseness have a psychiatric disorder, referring these children for specialist evaluation would not waste a substantial amount of scarce clinical resources on the evaluation of false positives. In a society where child mental health resources are very scarce, it is appropriate to use a screening test with a high threshold. The fact that a high threshold will also increase the proportion of false negatives is probably a cost worth paying since the children missed by the screening process would almost certainly never have been referred to services in any case.
Overall prevalence of psychiatric disorder
The proportion of 5- to 10-year-old children who had at least one ICD-10 psychiatric diagnosis according to the DAWBA was 15% for the rural area, 10% for the relatively prosperous urban area and 20% for the slum. Combining all three samples, the 95% confidence interval for prevalence was 11–21%. This compares with DAWBA-based prevalences of 8% for British 5- to 10-year-olds [21]; 7% and 13% for two different surveys of Brazilian 7- to 14-year-olds [8, 15]; and 15% for Russian 7-to 14-year-olds [16]. Since we did not sample a variety of rural, urban and slum areas, let alone obtain a representative sample of the country as a whole, it would be rash to use our figures as the basis for a precise estimate for Bangladesh as a whole. Nevertheless, allowing for the relative proportion of Bangladeshis living in rural, urban and slum areas, it seems unlikely that the prevalence of psychiatric disorders among Bangladeshi children is lower than 10%, and it is probably closer to 15%. The prevalence is probably higher still in adolescents [9]. On the conservative assumption that 10% of Bangladeshi children and adolescents have a psychiatric diagnosis, this represents over 5 million individuals who are experiencing substantial distress and social impairment; their disorders will also be affecting family members, classmates and teachers. These childhood problems will have substantial long-term costs, including higher rates of adult psychiatric disorders, criminality, substance abuse and under-employment. There are currently only a handful of child mental health professionals with specialist training in Bangladesh. Bridging the vast gap between need and provision will probably need to involve three strands: increasing the number of child mental health professionals; disseminating assessment and treatment techniques to other professionals, including teachers, family doctors and paediatricians; and preventing disorders where possible by tackling identifiable risk factors. Approaches to meeting mental health needs in developing countries are discussed by Rahman et al. [25] and Patel [23].
The pattern of psychiatric disorders found in Bangladeshi 5- to 10-year-olds resembles that identified in other parts of the world, with a preponderance of behavioural and anxiety disorders (e.g. [9, 8]); hyperkinesis is less common, and depression in this age range is rare. As discussed in the section “Obsessive–compulsive disorder”, an apparently distinctive aspect of the pattern of psychiatric disorder in Bangladesh is the high rate of obsessive–compulsive disorder.
Obsessive–compulsive disorder
The prevalence of obsessive–compulsive disorder (OCD) among this sample of Bangladeshi 5- to 10-year-olds was 2.0% (95% confidence interval 0.7–5.9%). This compares with prevalence rates of 0.1% (95% CI 0–0.2%) for British 5- to 10-year-olds [9, 21] and 0.1% (95% CI 0–0.2%) for Brazilian 7- to 14-year-olds [8]. This 20-fold difference occurred despite the DAWBA being used for the psychiatric assessment in all three countries, and despite clinical ratings being made or supervised by the second author (R.G.) in all three countries.
Since the high Bangladeshi prevalence was based on just five cases, it would be a mistake to make too much of the finding. Nevertheless, it does warrant some comment. The two commonest themes (each occurring in four of the five children) were obsessional concerns of having offended God and compulsions related to cleanliness. Bangladesh is a religious country; about 90% of the population are Muslim, and there are also significant numbers of Hindus, Buddhists and Christians. In a religious society, it is unsurprising that religious concerns are more common; the occurrence of an OCD-like ‘scrupulosity’ has been noted for many centuries among practicing Christians [26]. Islam particularly emphasises the importance of cleanliness in preparation for prayer; the themes of cleanliness and religion were explicitly linked by one of the children with OCD in this study, and may implicitly have been linked by some of the others. Furthermore, since Bangladesh is a country with a high mortality from diarrhoeal diseases spread by poor hygiene, and since health promotion in Bangladesh emphasises this link, heightened concerns about the dangers of poor hygiene are understandable. In this context, is it possible that we assigned diagnoses of obsessive–compulsive disorder to what should have been regarded as culturally sanctioned variations within the normal range? It is certainly possible; however, three factors lead us to believe that diagnoses were culturally appropriate. Firstly, both authors agreed on the diagnoses, in particular the first author, who is a Bangladeshi living and working in Bangladesh. Secondly, the families of the five affected children reported that the obsessions and compulsions led to marked distress or social impairment. Finally, in the clinical experience of the first author, children and adolescents with similar symptoms, including religious obsessions, are brought to mental health professionals by parents who happen to be religious leaders or pious lay people.
Our favoured interpretation, therefore, is that children with a constitutional tendency to obsessions and compulsions are more likely to present with frank obsessive–compulsive disorder in societies (such as Bangladesh) that emphasise and link cleanliness and piety. If our interpretation is correct, then religious authorities in Bangladesh may potentially be well placed to reassure overanxious believers of any age who have taken things too far.
Area differences in psychiatric disorders
In the first screening phase of the study, 10% of the children from the slum were screen positive, as compared with just 4% in both the rural and urban samples—a highly significant difference (Table 1). For comparison, a study using the same screening measure in Brazil found that 22% of 7- to 14-year-old children from a favela (shanty town) were screen positive, as compared to 13% in a rural area and 12% in a mixed urban area [7]. The absolute percentages were higher in the Brazilian study than in the present study, although much of this may be attributable to differences in the screening properties of the SDQ in the two countries. Thus whereas 90% of screen-positive children in Bangladesh in the present study had a psychiatric diagnosis when assessed with the DAWBA, the corresponding figure was only 56% in Brazil [7], suggesting that the threshold for becoming screen positive is lower in Brazil than in Bangladesh. The fact that the Brazilian sample was older may also have been relevant, since the prevalence of psychiatric disorder rises in adolescence [9]. Setting aside the national differences in absolute percentages, the similarity in pattern is very striking. Thus, in each country, children from rural and urban areas had similar rates of probable psychiatric disorders, whereas the rates for children from the slum/favela were roughly twice as high. The present study suggests that one possible explanation is that the slum families are generally poorer in all respects. Although families in the rural area were less affluent and less well educated than families from the relatively prosperous urban area, rural life had compensatory advantages, as judged by high ratings for neighbourhood helpfulness and low ratings for neighbourhood danger (Table 4). By contrast, the slum families were poorer in all ways—experiencing even more financial and educational disadvantage than the rural families, but without compensatory neighbourhood benefits to offset this. The urban poor in developing countries may experience the worst of all worlds [20], missing out on the potential benefits of both rural and urban life, while experiencing a heightened sense of relative poverty as a result of daily reminders of how much less privileged they are then wealthy city dwellers. Rural to urban migration may have an adverse impact on the mental health of rural as well as urban children and adolescents. This is reported to be the case in Swaziland where children are left in the care of over-burdened grandparents in depopulated rural areas while parents migrate to cities to work [17]. Whether this effect is relevant in some rural areas of Bangladesh remains to be established.
The first phase of this study applied the screening measures to almost a thousand children, giving the study reasonable statistical power to detect area differences. By contrast, the second phase applied detailed psychiatric assessments to only a fifth of these children, with more limited statistical power. Despite this, two interesting differences emerged from the second phase. Whereas the rates of non-compliant and irritable behaviours warranting a diagnosis of oppositional–defiant disorder were similar in all three areas, the children from the slum had significantly higher rate of serious behavioural problems warranting a diagnosis of conduct disorder (6.8% as compared with 0.7 and 0.4% for rural and urban children, respectively). There are several plausible reasons for children from a slum being more likely to have serious behavioural problems. For example, stealing may sometimes be an economic necessity; the use of weapons and being cruel to others may be linked to high levels of ambient violence; and repeatedly staying out late without permission may reflect stressed parents who are too busy or depressed to provide adequate supervision or discipline. The higher rate of serious conduct problems in our slum sample is in keeping with the adverse impact of rapid urbanisation on child behaviour in Sudan [24] and the marked excess of conduct disorder among the urban poor in Brazil [8]. In Swaziland, rural to urban migration may have had an adverse impact on the mental health of children and adolescents growing up in the increasingly depopulated rural areas [17]; whether this applies in some rural areas of Bangladesh remains to be established.
A second area of difference that only reached marginal statistical significance was the excess of post-traumatic stress disorder among slum children (3.2% as compared with 0.3 and 0% for rural and urban children, respectively). This difference is plausibly attributable to the slum children being more frequently exposed to several types of trauma, e.g. gang warfare, attacks by neighbours.
Demonstrating area differences and then teasing out the proximal mediators of those differences are mostly tasks for the future, but this preliminary study suggests that undertaking these tasks will be worthwhile. For example, a future study that involved many randomly selected areas could investigate how area rates of child mental health problems correlate with the area averages for material, educational and social wealth.
Limitations
Although the three communities that we studied were chosen after informal local consultation as representative exemplars of rural, urban and slum areas, we cannot rule out the possibility that they may nevertheless be not representative. Thus our findings are necessarily provisional, awaiting confirmation by larger studies sampling from a greater number of randomly chosen areas. Although our study has validated screening and detailed measures that can be used in future studies, and has generated approximate prevalence estimates that can be employed in the power calculations for such studies, definitive studies have yet to be done. Researchers and policy makers should view our findings as provisional and approximate.
References
Associacao Nacional de Empresas de Pesquisa-ANEP (2000) Criterio de Classificacao Economica Brasil. URL http://www.anep.org.br/codigosguias/CCEB.pdf
Bangladesh Bureau of Statistics (2003) Bangladesh population census 2001: national report (Provisional). Bangladesh Bureau of Statistics, Dhaka
Bangladesh Bureau of Statistics (2004) Statistical pocket book of Bangladesh 2002. Bangladesh Bureau of Statistics, Dhaka
Bird HR, Canino G, Rubio-Stipec M, Gould MS, Ribera J, Sesman M, Woodbury M, Huertas-Goldman S, Pagan A, Sanchez-Lacay A, Moscoso M (1988) Estimates of the prevalence of childhood maladjustment in a community survey in Puerto Rico. Arch Gen Psychiatry 45:1120–1126
Bird HR, Yager TJ, Staghezza B, Gould MS, Canino G, Rubio-Stipec M (1990) Impairment in the epidemiological measurement of childhood psychopathology in the community. J Am Acad Child Adolesc Psychiatry 29:796–803
Canino G, Shrout, PE, Rubio-Stipec M, Bird HR, Bravo M, Ramírez R, Chavez L, Alegría M, Bauermeister JJ, Hohmann A, Ribera J, García P, Martínez-Taboas (2004) The DSM-IV rates of child and adolescent disorders in Puerto Rico. Arch Gen Psychiatry 61:85–93
Fleitlich B, Goodman R (2001) Social factors associated with child mental health problems in Brazil—a cross-sectional survey. BMJ 323:599–600
Fleitlich-Bilyk B, Goodman R (2004) The prevalence of child psychiatric disorders in Southeast Brazil. J Am Acad Child Adolesc Psychiatry 43:727–734
Ford T, Goodman R, Meltzer H (2003) The British child and adolescent mental health survey 1999: the prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry 42:1203–1211
Goodman R (1997) The Strengths and Difficulties Questionnaire: a research note. J Child Psychol Psychiatry 38:581–586
Goodman R (1999) The extended version of the Strengths and difficulties questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry 40:791–801
Goodman R (2001) Psychometric properties of the Strengths and Difficulties Questionnaire (SDQ). J Am Acad Child Adolesc Psychiatry 40:1337–1345
Goodman R, Ford T, Richards H, Meltzer H, Gatward R (2000a) The development and well-being assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry 41:645–657
Goodman R, Renfrew D, Mullick M (2000b) Predicting type of psychiatric disorder from Strengths and Difficulties Questionnaire (SDQ) scores in child mental health clinics in London and Dhaka. Eur Child Adolesc Psychiatry 9:129–134
Goodman R, Neves dos Santos D, Robatto Nunes AP, Pereira de Miranda D, Fleitlich-Bilyk B, Almeida Filho N (2005a) The Ilha de Maré study: a survey of child mental health problems in a predominantly African–Brazilian rural community. Soc Psychiatry Psychiatr Epidemiol 40:11–17
Goodman R, Slobodskaya H, Knyazev G (2005b) Russian child mental health: a cross-sectional study of prevalence and risk factors. Eur Child Adolesc Psychiatry 14:28–33
Guinness E (1992) Patterns of mental illness in the early stages of urbanization. Br J Psychiatry 160(Supplement 16):4–72
Hackett R, Hackett L (1999) Child psychiatry across cultures. Int Rev Psychiatry 11:225–235
Hackett R, Hackett L, Bhakta P, Gowers S (1999) The prevalence and associations of psychiatric disorder in children in Kerala, South India. J Child Psychol Psychiatry 40:801–807
Harpham T, Molyneux C (2001) Urban health in developing countries: a review. Prog Dev Stud 1:113–137
Meltzer H, Gatward R, Goodman R, Ford T (2000) Mental health of children and adolescents in Great Britain. The Stationery Office, London
M Mullick R Goodman (2001) ArticleTitleQuestionnaire screening for mental health problems in Bangladeshi children: a preliminary study Soc Psychiatry Psychiatr Epidemiol 36 94–99 Occurrence Handle10.1007/s001270050295 Occurrence Handle11355451
Patel V (2003) Where there is no psychiatrist. Gaskell, London
Rahim SIA, Cederblad M (1984) Effects of rapid urbanisation on child behaviour and health in a part of Khartoum, Sudan. J Child Psychol Psychiatry 25:629–641
Rahman A, Mubbashar M, Harrington R, Gater R (2000) Developing child mental health services in developing countries. J Child Psychol Psychiatry 41:539–546
Seuss L, Halpern MS (1989) Obsessive–compulsive disorder: a religious perspective. In: Rapoport JL (ed) Obsessive–compulsive disorder in children and adolescents. American Psychiatric Press, Washington DC, pp 311–325
World Health Organization (1993) The ICD-10 Classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization, Geneva
Acknowledgements
The study was supported by a grant from the Wellcome Trust.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mullick, M.S.I., Goodman, R. The prevalence of psychiatric disorders among 5–10 year olds in rural, urban and slum areas in Bangladesh. Soc Psychiat Epidemiol 40, 663–671 (2005). https://doi.org/10.1007/s00127-005-0939-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-005-0939-5