Abstract
Objectives
Valid screening tools are needed to identify Indian children and adolescents with mental health problems, both for clinical or research purposes. The present study validated the Strengths and Difficulties Questionnaire (SDQ) in Malayalam across different informants and sub-scales.
Methods
A sample of 150 children and adolescents seen in a psychiatric clinic for children in Kerala, India was compared to a community sample of 1984 children from six surrounding urban and rural districts. Children in clinic and community samples were screened with the parent-report SDQ; those over 11 y completed the self-report SDQ. The community sample was also screened with the teacher-report SDQ and the clinical sample received formal diagnoses from a child psychiatrist blind to SDQ scores. The discriminative validity of the SDQ was investigated using Receiver Operator Characteristic (ROC) curves and by assessing Area Under the Curve (AUC).
Results
The SDQ discriminated reliably between clinical and community samples for the SDQ total score and its subscales. Within the clinic sample, 49 % of patients qualified for more than one broad diagnostic grouping. The SDQ discriminated between diagnostic categories in the clinic sample, but did so most effectively for conduct disorders. Based on the cut-offs that generated the highest combined value of sensitivity and specificity, the estimated rate of psychiatric disorder in the community sample was 13.6 % (parent-report) and 7.3 % (self-report).
Conclusions
The SDQ is a useful screening tool for child and adolescent mental disorders for Malayalam speakers in Kerala, India.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More information is needed about rates of child psychiatric disorders in low and middle income countries. Studies in low and middle income countries mostly suggest a prevalence of 10 to 20 % in young people aged 18 y and below [1–5], although other estimates have been both lower [6] and higher [7].
International and intercultural studies can lead to a better understanding of the universality (or otherwise) of disorders as currently defined, e.g. , informing debate about the validity of attention deficit hyperactivity disorder (ADHD) [8]. Comparing findings from different cultures and global locations could contribute to thinking about biological and psychosocial etiologies.
Consistent measurement across cultures of children’s behavior from multiple informants can also elucidate how adult expectation of children’s behavior varies in different national and cultural groups [9]. It may additionally contribute to our understanding of the long-term consequences of child psychiatric disorders in different circumstances.
The use of widely differing methodologies and diagnostic criteria for measuring and classifying psychopathology limits meaningful comparison of the prevalence rates and risk factors associated with child mental disorders, both for comparisons between and across countries. There is an increasing demand for a “toolbox” of measures that can be validated and used across countries, languages and cultures [10, 11].
The Strengths and Difficulties Questionnaire (SDQ) is a tool that is easy and quick to administer and has been translated into around 80 languages. It could be useful as a free screening measure in the community to identify children whose behavior is of concern and prompt further assessment or intervention.
In Kerala, there has been a previous study of children’s mental health [5] which used a Malayalam version of the Isle of Wight Interview Schedule [12, 13]. This is the first validation study of the SDQ in this region, based on a comparison of SDQ findings for clinical and community samples.
Material and Methods
A multidisciplinary child mental health clinic at the Medical College Hospital in Thiruvananthapuram, the capital city of Kerala, administered SDQs to parents and young people (11–16 y) at the first psychiatric assessment; for logistical reasons, teacher SDQs were not obtained. Questionnaires were administered to a consecutive series of 153 new patients between April 2005 and February 2006. Three patients were excluded from further analysis because either the parent or self-report questionnaire had not been completed, which made it impossible to generate all scores. One hundred fifty patients remained in the sample after exclusions.
The community sample was collected from two urban councils and three rural panchayats within Thiruvananthapuram district. The schools within these councils and panchayats were selected using stratified random sampling, and five schools were included in the study. Two of the five schools were co-educational, the remainder were single-sex (two girls’ schools, one boys’ school); one of the five schools was private. All schools agreed to participate. Two thousand forty children were randomly selected from the class registers, mothers were visited at home and 1985 agreed to take part in the study. Parents, teachers and young people completed SDQs with questions being read out when respondents had literacy problems. The children and families were representative of the population in this area.
Ethical Permission was obtained from the ethics committee at the Institute of Psychiatry, Kings College London and from Thiruvananthapuram medical college. Participants joined voluntarily after giving written and verbal consent and were free to withdraw from the study at any point. Parental consent was sought before child/adolescent assent. Permission from the department of education, Kerala and head-teachers was granted.
The SDQ asks about 25 attributes, some positive and some negative. The items, which were selected on the basis of contemporary diagnostic criteria, as well as factor analyses, are divided between five scales of five items each, generating scores for Emotional Symptoms, Conduct Problems, Hyperactivity, Peer Problems, and Prosocial Behaviors. All items contributing to the first four subscales are summed to generate a Total Difficulties Score. The questionnaire can be completed in about 5 min by parents or teachers of children aged 4–16 y [14]. There is a self-report version for children aged 11 y and over [15]. An extended version rates the impact of psychiatric symptoms in terms of distress, social impairment or burden to others [16]. The SDQ has an acceptable reliability and validity, performing at least as well as the Rutter Questionnaire [14] and the Child Behaviour Checklist [17]. The website at www.sdqinfo.org provides more information on the SDQ, plus versions of the questionnaires in Bengali, Hindi, Kannada, Malayalam, Punjabi, Tamil and Urdu.
The versions of the SDQ were translated into Malayalam by a Malayali psychiatrist after clarifying possible ambiguities in English with the senior author (RG). KM made independent back translations. The discrepancies were resolved by discussion between authors. Care was taken to ensure that the translation was culturally sensitive, using only words and idioms understandable to all Malayali speakers irrespective of social and educational background. The versions of the SDQ used in this study were informant and self-report versions, including impact supplements, all being scored as in the standard manner [14–16]. In the community sample, Parent and Teacher SDQs were administered to the mothers and class teachers of all subjects aged 4–16 y; in the clinic sample, Parent SDQs were administered to the mothers of all subjects aged 4–16 y. In both community and clinical samples, self-report SDQs were administered to 11–16 y olds.
Children from the psychiatric clinic were assigned clinical diagnoses based on the operationalised criteria of ICD-10 [18]. These clinical diagnoses were made at the time of initial assessment by a Malayali child psychiatrist, the senior clinician involved in the assessment. These diagnoses were made blind to the child’s SDQ scores. Diagnoses were collapsed into three broad categories to provide cell sizes that would be sufficient for meaningful analysis. These were hyperkinesis; conduct disorders (including oppositional defiant disorder); and emotional disorders (including anxiety, depression, and obsessive compulsive disorder).
The ability of the different SDQ scales to distinguish between community and clinic subjects – or between different diagnostic categories within the clinic sample – was examined using receiver-operator characteristic (ROC) curves utilising the statistics/data analysis programme STATA 11. The area under the curve (AUC) indicated how well the SDQ or one of its subscales discriminated between clinic and community samples, or between cases with different diagnoses within the clinic sample. As a guide to interpretation, the area under the curve is 1.0 for a measure that discriminates perfectly, and 0.5 for a measure that discriminates no better than chance. While an AUC of just over 0.5 could be statistically significant in a large sample, this would be unlikely to be clinically significant. An AUC of 0.8 or more was used as a benchmark for clinically meaningful predictions.
ROC curves were generated for the SDQ Total Difficulties score, comparing the clinic and community samples. In addition ROC curves were generated for the SDQ subscores of Hyperactivity/Inattention, Conduct, Emotional and Impact scores, comparing the entire community sample with the clinic cases who had been diagnosed with a disorder conforming to the relevant scale. For example, for the emotional subscale of the SDQ, only those clinic cases diagnosed with an emotional disorder were compared with the community sample, in an effort to distinguish whether the subscale discriminated between high and low risk for emotional disorder. The ability of the SDQ to discriminate between disorders in the clinic sample was also investigated.
Results
Parent SDQs were available on 100 % of the 1985 subjects included in the community sample. Teacher SDQs were returned for 1543 subjects (78 %). A self-report was available on 100 % of community subjects between the ages of 11 and 16 y inclusive (n = 1289; 65 % of the sample were between 11 and 16 y). The mean age of the entire sample was 11.4 y (SD 3.0 y); 39.4 % were boys; 60 % of families were urban and religious belief as reported by parents was Hinduism for 68 %, Christianity for 21 % and Islam for 11 %. The mean SDQ score for the parent-report was 9.6, for the teacher-report 9.9 and for the self-report 12.2 (11–16 y).
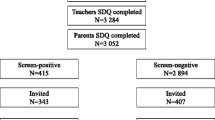
Of the 150 patients included in the clinic sample after exclusions, self report was available on 92 young people (61 %). The mean age of the sample was 11.3 y [SD 2.7 y, which was not significantly different from the community sample; 66 % of the clinic sample were boys, which was significantly different from the community sample (t = 6.44; p < 0.0001)]. Diagnoses as assigned by child psychiatrists were as follows: 71 patients had hyperkinesis (47.3 %), 40 patients had an emotional disorder (26.6 %), 102 patients had conduct disorder (68 %); 74 met criteria for more than one diagnosis (49 %); and 18 (12 %) were not diagnosable within the available categories (Fig. 1).
Table 1 summarizes the ability of the different SDQ scales to distinguish between community and clinical subjects as gauged by area under a receiver operating characteristic curve (AUC). Total Difficulties, Emotional, Conduct, and Hyperactivity subscales distinguished well between clinic and community samples. In each case the AUC was significantly greater than 0.5 (P < 0.001). The scales exceeded the benchmark of an AUC of 0.8, with the exception of an AUC of 0.76 for the parent-reported Impact score. Because Teacher SDQs were administered for the community, but not the clinic sample, it was not possible to compute AUCs for the Teacher SDQ.
Whether the Emotion, Conduct, and Hyperactivity subscales discriminate within the clinic sample between patients with different types of disorders was also examined using the area under ROC curves (Table 2).
The Conduct scale of the SDQ discriminated reliably between clinic patients with and without a diagnosis of conduct disorder (including oppositional-defiant disorder) with an AUC of 0.84 (parent report) and 0.81 (self-report). Emotional and Hyperactivity scales discriminated less well between those with and without emotional and hyperkinetic disorders respectively, with AUCs in the 0.70–0.73 range for both parent and self-report.
The authors used the clinic data to designate the band of SDQ scores likely to correspond with “abnormality”. The cut-off value was based on the total problem score and defined as the SDQ score that corresponded with the highest values of sensitivity and specificity combined.
For the parent SDQ, the score with the highest combined value of sensitivity and specificity was achieved by defining caseness (presumptive mental disorder) in terms of a total SDQ score of 15 points or more, corresponding to a sensitivity of 0.82 and a specificity of 0.83. In the community sample, 13.6 % of the sample met this criterion for caseness.
For the self-report SDQ, the score with the highest combined value of sensitivity and specificity was achieved by defining caseness in terms of a total SDQ score of 20 points or more, corresponding to a sensitivity of 0.92 and a specificity of 0.91. In the community sample, 7.3 % of the 11–16 y olds met this criterion for caseness.
According to all three types of informants, this Malayali sample has higher mean total difficulties scores than reported by previous SDQ studies carried out in Goa [6] and on British Indians [19] (Table 3). One interpretation is that children from Kerala have more problems and symptoms than their British and Goan counterparts. An alternative explanation may be response bias, with expectations relating to children’s behavior and well-being being higher in Kerala than in other Indian samples. A similar effect was shown by Leung et al’s [9] study of Hong Kong Chinese school boys, in which Rutter scores suggesting levels of hyperactivity significantly higher (double) that reported in the West;[20].
Another perspective on this difference in reporting levels of mental health symptoms is suggested by Sen [21]. He compared levels of health morbidity reported by a Malayali population both to India as a whole and the poorer state of Bihar. He noted that despite Kerala’s superior health facilities, longevity and general education, the level of morbidity was higher in Kerala than in India and far higher than that reported in poorer Indian states with low life expectancy, e.g., Bihar. Sen suggests that better access to health facilities and education results in greater recognition of health problems. This effect may help to explain the higher mean problem scores in Malayali children vs. Goan children, but does not provide a coherent interpretation for the Malayali children vs. British-Indian or White British children.
The authors explored the intra-class correlations for total difficulty scores between the different informants in the community sample – these are shown in Table 4 along with comparable data from a British SDQ study [22] and a meta-analysis of inter-rater agreement in a broad range of measures [23].
Discussion
This study indicates that the Strengths and Difficulties Questionnaire is useful in discriminating between child psychiatry clinic and school-based community samples. For both parent and self-report, the AUC exceeded the benchmark of 0.8, with just the parent impact score falling slightly lower (0.76). These results are in line with the AUCs in a number of other validation studies [24], and better than the AUCs in other similar validation designs [25]. These results indicate that the Strengths and Difficulties Questionnaire may be a useful screening tool in the community.
In the examination of how well the SDQ subscales could distinguish between different types of psychiatric disorders in the clinic sample, the conduct subscale discriminated with an AUC of 0.84 for parent-rating and 0.81 for self-rating, whereas the emotional and hyperactivity subscales did not exceed the benchmark AUC threshold of 0.80 (range 0.71 to 0.73). The greater difficulty predicting type, as opposed to presence, of disorder is in line with other studies using similar methods [25, 26]. Inter-rater reliabilities were consistently higher than those reported in Achenbach’s meta-analysis (Table 4).
Conclusions
The findings of this study would have been stronger had the authors been able to use a standardized measure of psychiatric diagnosis in the clinical sample, instead of relying on clinical diagnoses. Unfortunately, the resources were not available to conduct such a study. Nevertheless, the results do suggest that the Malayalam SDQ is a useful tool that discriminates well between children with and without mental disorders. Further studies should examine whether the use of parent, teacher and self- report SDQs can efficiently and economically identify children who benefit from more detailed assessment and, where appropriate, treatment. An estimated prevalence of child and adolescent mental health disorders of between 7 % (by self-report) and 14 % (by parent-report) suggests that there is much to do, incurring costs but potentially saving even more money in the longer term [27, 28].
References
Bird HR, Canino G, Rubio-Stipec M, et al. Estimates of the prevalence of childhood maladjustment in a community survey in Puerto Rico. The use of combined measures. Arch Gen Psychiatry. 1988;45:1120–6.
Canino G, Shrout PE, Rubio-Stipec M, et al. The DSM-IV rates of child and adolescent disorders in Puerto Rico: prevalence, correlates, service use, and the effects of impairment. Arch Gen Psychiatry. 2004;61:85–93.
Fleitlich-Bilyk B, Goodman R. Prevalence of child and adolescent psychiatric disorders in southeast Brazil. J Am Acad Child Adolesc Psychiatry. 2004;43:727–34.
Hackett R, Hackett L. Child psychiatry across cultures. Int Rev Psychiatry. 1999;11:225–35.
Hackett R, Hackett L, Bhakta P, Gowers S. The prevalence and associations of psychiatric disorder in children in Kerala, South India. J Child Psychol Psychiatry. 1999;40:801–7.
Pillai A, Patel V, Cardozo P, Goodman R, Weiss HA, Andrew G. Non-traditional lifestyles and prevalence of mental disorders in adolescents in Goa, India. Br J Psychiatry. 2008;192:45–51.
Belfer ML. Child and adolescent mental disorders: the magnitude of the problem across the globe. J Child Psychol Psychiatry. 2008;49:226–36.
Timimi S, Taylor E. ADHD is best understood as a cultural construct. Br J Psychiatry. 2004;184:8–9.
Leung PW, Luk SL, Ho TP, Taylor E, Mak FL, Bacon-Shone J. The diagnosis and prevalence of hyperactivity in Chinese schoolboys. Br J Psychiatry. 1996;168:486–96.
Polanczyk G, de Lima MS, Horta BL, Biedermann J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942–8.
Cortina MA, Sodha A, Fazel M, Ramchandani PG. Prevalence of child mental health problems in sub-Saharan Africa: a systematic review. Arch Pediatr Adolesc Med. 2012;166:276–81.
Rutter M, Graham P. The reliability and validity of psychiatric assessment of child: I. Interview with the child. Br J Psychiatry. 1968;114:563–79.
Graham P, Rutter M. The reliability and validity of psychiatric assessment of child: II. Interview with the parent. Br J Psychiatry. 1968;114:581–92.
Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. 1997;38:581–6.
Goodman R, Meltzer H, Bailey V. The strengths and difficulties questionnaire: a pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry. 1998;7:125–30.
Goodman R. The extended version of the strengths and difficulties questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry. 1999;40:791–9.
Goodman R, Scott S. Comparing the strengths and difficulties questionnaire and the child behavior checklist: is small beautiful? J Abnorm Child Psychol. 1999;27:17–24.
WHO, ICD-10, Vol. 3. International statistical classification of diseases and related health problems: Alphabetical index, 10th ed. Geneva, Switzerland: WHO{a}; 1994. p. iii + 750.
Goodman A, Patel V, Leon DA. Why do British Indian children have an apparent mental health advantage? J Child Psychol Psychiatry. 2010;51:1171–83.
Ho TP, Leung PWL, Luk ES, Taylor E, Bacon-Shone J, Mak FL. Establishing the constructs of childhood behavioral disturbances in a Chinese population: a questionnaire study. J Abnorm Child Psychol. 1996;24:417–31.
Sen A. Mortality as an indicator of economic success and failure. Econ J. 1998;108:1–25.
Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40:1337–45.
Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol Bull. 1987;101:213–32.
Alyahri A, Goodman R. Harsh corporal punishment of Yemeni children: occurrence, type and associations. Child Abuse Negl. 2008;32:766–73.
Mullick MS, Goodman R. The prevalence of psychiatric disorders among 5–10 year olds in rural, urban and slum areas in Bangladesh: an exploratory study. Soc Psychiatry Psychiatr Epidemiol. 2005;40:663–71.
Woerner W, Becker A, Rothenberger A. Normative data and scale properties of the German parent SDQ. Eur Child Adolesc Psychiatry. 2004;13:II3–10.
Beecham J. Annual research review: child and adolescent mental health interventions: a review of progress in economic studies across different disorders. J Child Psychol Psychiatry. 2014;55:714–32.
Snell T, Knapp M, Healey A, et al. Economic impact of childhood psychiatric disorder on public sector services in Britain: estimates from national survey data. J Child Psychol Psychiatry. 2013;54:977–85.
Acknowledgments
The authors wish to acknowledge the support and help of Mr. M.S.S Mohan, Miss Roshin Sudesh, and Dr. Sudeshni Mirza, Hopes and Dreams foundation, Kerala, India for their input into data collection, data entry and other logistic support.
Contributions
JPO and RG analysed the data and produced the manuscript. KAHM and RG designed the protocol, gained ethical approval, translated the SDQ and supervised data collection. KAHM reviewed the manuscript. RG will act as guarantor for this paper.
Conflict of Interest
RG is the owner of Youthinmind Ltd that produces no-cost and low-cost websites relating to the Strengths and Difficulties Questionnaire.
Source of Funding
Departmental funds.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jacqueline A. Phillips Owen and K. A. H. Mirza are joint first authors
Rights and permissions
About this article
Cite this article
Phillips Owen, J.A., Mirza, K.A.H. & Goodman, R. Validating Screening Tool in Malayalam for Mental Disorders. Indian J Pediatr 82, 595–600 (2015). https://doi.org/10.1007/s12098-015-1727-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-015-1727-1