Abstract
Unstable vertebral body fragility fractures of the thoracolumbar spine can occur with or without relevant trauma. Initially, a standardized diagnostic algorithm including magnetic resonance tomography is recommended to detect accompanied further vertebral body fractures, to interpret the individual fracture stability, and to screen for relevant traumatic intervertebral disc lesions. Aim of the therapy is to assure fast mobilization and to maintain spinal alignment. Unstable fracture morphology is defined by vertebral body fractures including a relevant defect of the posterior vertebral cortex as well as type B or C fractures. With respect of type A fractures, a combined anterior–posterior approach including a primary cement-augmented posterior stabilization and anterior spondylodesis is indicated in those patients with relevant intervertebral lesions or in those suffering from high-energy accidents resulting in unstable burst-type fractures. The others will benefit from hybrid stabilizations including cement-augmented posterior stabilizations and cement augmentation (kyphoplasty) of the fractured level to gain a ventral transosseous stability. In addition, individually adapted antiosteoporotic therapy is essential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The average age of patients suffering from vertebral body fractures is increasing over the last decades. Nowadays, a second peak is visible after the age of 65 [19, 20]. There are several possible explanations for that including longer life expectancy, increasing activity level, ongoing degenerative changes, sagittal malalignment, and impaired bone quality [11]. Thereby, the vertebral spine is the most prominent location of osteoporotic fractures [8]. Interestingly, more than 80% of trauma patients suffered from Vitamin D insufficiency possibly potentiating the effect of osteoporosis in the future [34]. The majority of osteoporotic vertebral body fractures are stable and can be treated conservatively. However, a considerable number of vertebral body fractures collapse after mobilization or offer instability criteria. Thus, an operative stabilization is mandatory [13]. Thereby, the biomechanics of the vertebral spine as well as the fracture situation have to be considered. The aim of this review is to analyze the biomechanical background of unstable osteoporotic vertebral body fractures, to present a diagnostic algorithm, to point out the indication for anterior–posterior stabilization, and to describe surgical techniques based on the individual patient.
Biomechanics
Fragility fractures of the vertebral body typically occur after low-energy accidents [13]. Furthermore, it is occasionally visible in patients without any trauma at all. In the majority, these fractures offer no signs of instability with intact posterior vertebral cortex and intact posterior ligament complex. Thus, a conservative treatment is indicated. However, this can change tremendously over the course. The repetitive force acting on a fractured vertebral body can be sufficient to promote regional kyphosis and/or posterior vertebral cortex insufficiency. This can be explained by several biomechanical considerations, such as the ongoing process of degeneration, impaired bony architecture caused by osteoporosis, and non-physiological force vectors acting on the vertebral bodies based on malalignment. Thereby, vertebral column degeneration is mainly based on ongoing intervertebral-disc sclerosis and subsequent loss of disc height [11]. Thus, the intervertebral disc loses the ability to transfer forces symmetrically leading to pressure peaks at the anterior and posterior vertebral bodies [2]. In addition, it was shown that a reduction of whole vertebral column flexibility reduces the ability of stress compensation [1, 12, 27, 30]. Thus, stress peaks that act on the posterior vertebral body and impaired bony stability in combination with osteoporotic fracture situation might overstrain the vertebral body. Furthermore, the local and regional alignment of the vertebral column is of great importance, concerning both the sagittal and coronal plane. On the one side, increasing kyphosis leads to an anterior shift of the force acting on the vertebral body (Fig. 1). On the other side, scoliotic malalignment will lead to one-sided lateral stress peaks of the affected vertebral bodies [8]. Thus, increasing risk of further vertebral can be expected [3]. It has been shown that the risk of adjacent fractures increases disproportionately in dependence on the number of vertebral bodies with kyphotic malalignment [17].
Schematic drawing of the axial force distribution (red arrows) at the vertebral body at the thoracolumbar junction in standing position in a balanced vertebral spine without fracture deformity (a). In contrast, a 10° wedge deformity of one vertebral body (b) leads to an anterior shift of the downward-directed force vector (b)
Classification
Historically, osteoporotic fractures were classified analogous to vertebral body fractures of patients with normal bone quality. One of the oldest fracture classifications was developed by Holdsworth [10] and Whitesides [32] using a two-column concept. Later, Louis [16] and Denis [5] introduced the three-column idea dividing the anterior column in two parts, the anterior two-thirds of the vertebral body on the one side and posterior third of the vertebral body including the posterior cortex and the posterior longitudinal ligament on the other side. In 1994, Magerl et al. [18] introduced the AO comprehensive fracture classification after analyzing a total of 1445 thoracolumbar vertebral fractures. Fractures of the compression type were classified as type A fractures, whereas type A1 and A2 fractures affected the anterior column only, and type A3 fractures additionally included the posterior cortex of the vertebral body. In 2013, this classification has been modified into the “AOSpine Thoracolumbar Spine Injury Classification System” [29]. Meanwhile, specific classifications for osteoporotic vertebral body fractures have been introduced, such as the Genant score. This classification is based on the vertebral body shape on conventional radiographs [15]. Just recently, the osteoporotic fracture (OF) classification has been developed [22]. This classification considers the fracture morphology as well as individual patient-specific parameters such as pain situation, mobility, bone quality, and kyphotic malignment.
Diagnostic imaging
Conventional radiography in two planes is the primary diagnostic tool in patients with suspicion of vertebral body fractures [11]. This should be performed in all patients with low- or moderate-energy traumas and in those patients without known accidents but therapy-resistant pain of no more than 6 weeks. In contrast, computed tomography (CT) is indicated in patients suffering high-energy accidents. An additional magnetic resonance imaging (MRI) is recommended in patients with visible or high suspicion of a vertebral body fracture(s) and an age of 60 years and older. In most patients, short-tau inversion recovery (STIR) sequences are sufficient. Thereby, Spiegl at al. [23] reported that in more than half of the patients, the therapy concept was changed based on the information obtained by MRI. In contrast, MRI with T1 and T2 sequences should be included in patients with a history of acute clinical signs of claudicatio spinalis or any radiculopathy [11]. In the majority of cases, the degree of posterior cortex lesion can be evaluated sufficiently by MRI and conventional radiographs. In doubt, an additional CT examination is necessary to interpret bony instability correctly. Furthermore, full-spine radiographs are recommended in those patients who tolerate standing position. Thereby, the local and global alignment can be analyzed.
360°-Stabilization
A posterior-only treatment concept is not advisable in patients suffering from an unstable osteoporotic thoracolumbar vertebral fracture based on the decreased implant fixation strength, the impaired healing potential of the fractured vertebral body, and the anterior shift of the downward-directed force vector [13]. In contrast, a ventral transosseous stabilization by kyphoplasty or vertebroplasty is a proper and suitable procedure in osteoporotic vertebral body fractures without vertebral disc lesions. The authors prefer kyphoplasty based on the reduced cement leakage and the improved reduction potential compared to vertebroplasty [26, 33]. The rigid cement acts well against axial forces making this an adequate technique for type A1 (OF 1) fractures or fractures without relevant posterior cortex lesion (OF 2 fractures). In contrast, the biomechanical properties of the cement against shear forces, particularly in osteoporotic bone situation, are questionable. Therefore, it is advisable to perform an additional dorsal stabilization (hybrid) to avoid shear forces in patients with posterior cortex lesion. The combination of posterior stabilization and the anterior intraosseous support (kyphoplasty) acts functionally as a 360°-stabilization. This can be performed minimally invasively by a posterior approach. Anatomic reduction can be successfully achieved in acute fractures by correct patient positioning in prone position and sag of the fractured vertebral body. Analogous to the authors of the OF classification, we believe that a 360°-stabilization is advisable in patients with a posterior cortex lesion of more than 20% [22]. Similarly, an additional dorsal stabilization has to be discussed in patients with type A1 fractures and severe kyphotic malalignement of more than 20° particularly in the upper and mid-thoracic spine. Kyphoplasty alone might result in higher risk of reduction loss and impaired clinical results, based on the biomechanics of this fracture condition shown in Fig. 2. Particularly, too far posterior cement positioning increases the risk of upper endplate fractures and consecutive recurrent kyphotic malalignment [7]. In contrast, this risk of implant failure can be minimized by a 360°-stabilization and adding a dorsal implant. Additionally, the technique of a 360°-stabilization can be done either by performing posterior stabilization in combination with an additional anterior spondylodesis using a cage. This has to be chosen properly.
Schematic drawing of severely wedge-shaped vertebral bodies including the force vectors (red arrows) while standing (a, b; superior images). Postoperative situation after kyphoplasty and anatomic reduction with anterior cement position (a, central image) and posterior cement position (b, central image) including the force vectors and counter-acting forces of the vertebral body (blue arrows). Whereas there is a symmetric force and counter-force configuration leading to no relevant morphologic changes when the cement is positioned anteriorly (a, inferior image), endplate fracture and reduction loss can be expected when the cement is positioned posteriorly based on the asymmetric force distribution (b, inferior image)
Hybrid stabilization
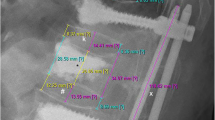
The hybrid stabilization including minimally invasive posterior cement-augmented stabilization and kyphoplasty of the ventral column is a well-established technique [4] (Fig. 3). It was shown that the intraoperative blood loss and complication rate could be reduced significantly using minimally invasive techniques [21]. In addition, no disadvantages in reduction potential are visible. Weiss et al. [31] proved the ability of anatomic fracture reduction using minimally invasive instrumentation systems. Cement augmentation of the screws is of great importance to reduce implant failure and reduction loss [4, 25]. Fenestrated screws facilitate the technique of screw augmentation tremendously. As a result of the intravertebral-disc sclerosis and the lower fracture threshold in osteoporotic bones, traumatic intervertebral disc lesions are rare in patients with osteoporotic vertebral fractures [11]. Thus, anterior transosseous stabilization using cement augmentation is sufficient in the majority of those patients. Whereas bisegmental instrumentation is sufficient in vertebral body fractures of the thoracolumbar junction and lumbar spine, longer dorsal constructs are necessary in fractures of the mid or upper thoracic spine [13]. Thereby, it is important to analyze the sagittal alignment correctly and to avoid ending the instrumentation at the apex of kyphosis [8].
69-year-old female patient who fell during an emergency stop during a bus ride suffering an incomplete burst fracture of the first lumbar vertebral body type AO A3, OF 3 (a–c). On the next day, minimally invasive bisegmental cement-augmented stabilization of Th 12 to L 2 including kyphoplasty of L1 was performed. Postoperative radiographs illustrated anatomic reduction (d, e). After 1 year, the patient had minimal pain (VAS: 2) with no limitations. There was no relevant reduction loss visible after 1 year (f, g)
In accordance with the literature, proper hybrid stabilization technique can lead to anatomic fracture reduction without relevant postoperative reduction loss [14]. In contrast, patients suffering from osteoporotic vertebral fracture treated with posterior stabilization without anterior support had significantly higher rates of reduction loss [28]. Similarly, patients treated by hybrid stabilization offered better long-term clinical and radiological outcomes compared to those treated by kyphoplasty alone [24]. Actually, there was no difference in reduction loss between patients with unstable osteoporotic vertebral fractures treated by an anterior–posterior approach including anterior cage implantation versus by hybrid stabilization [28].
Anterior–posterior approach
Nonwithstanding, vertebral fractures with osteoporotic bone quality can be caused by high-energy trauma leading to unstable fracture morphology with or without intervertebral disc lesion. Traditionally, these patients are treated by an anterior–posterior approach (Fig. 4). In those patients, cement-augmented screw implantation is recommended [25]. In addition, it was shown that a careful endplate preparation is of great importance to avoid reduction loss by cage subsidence. Hoffmann et al. [9] evaluated patients older than 60 years with unstable vertebral body fractures of the thoracolumbar junction after an adequate trauma treated by an anterior–posterior approach with implantation of a ventral cage. They found an average reduction loss in all patients with intraoperative endplate defect (17%) of 14.8°, whereas in all others, no relevant reduction loss was visible (average: 1.3° after 3 years). Generally, the outcome was promising with no or minimal limitations in the majority of patients (86%) and moderate limitations in the others. Alternatively, cement augmentation of the vertebral body accompanied to the anterior cage has been reported. Thus, relevant cage incidences with reduction loss could be avoided [6]. This technique is particularly recommended in those patients with intraoperative suspicion of endplate lesions accompanied to the cage.
69-year-old male patient who fell from a height of 3 m while cutting the tree. Initially, a polytrauma CT examination was performed showing a complete burst fracture of L2 type A4, OF 4 (a). Surgery was done on the same day, performing a posterior bisegmental cement-augmented stabilization from L1 to L3 (b, c). An additional anterior spondylodesis and partial corporectomy of L2 and implanting a cage was performed 8 weeks after trauma (d, e). The patient had only minimal pain after 1 year (VAS: 1) and had no limitations (ODI-score: 0). The radiographic control after 1 year showed no reduction loss and correct implant positioning (f, g)
Whereas the majority of our adult patients below the age of 60 years are treated by an anterior–posterior approach including cage implantation at the ventral column, our older patients, 70 years of age or older, are mainly treated by hybrid stabilization. Meanwhile, both techniques were used in our patients aged between 60 and 70 years. Therefore, we examined this patient collective between 60 and 70 years of age with unstable thoracolumbar fractures after acute trauma of moderate to high energy. All patients were treated surgically in 2013 and 2014. A total of 20 patients were treated by hybrid stabilization, whereas an anterior–posterior approach was done in 14 patients. After a minimum follow-up of 12 months, there was no significant difference regarding the average ODI score (hybrid: 24.9; anterior-posterior: 16.0). In addition, there was no significant difference in the pain situation, patients’ satisfaction level as well as the physical and mental summary score (SF 36 score). However, the anterior–posterior concept represents the more complex strategy, being associated with two surgeries and a significantly longer hospital stay. Based on those results, a 360°-stabilization using anterior transosseous stabilization (kyphoplasty) might be a sufficient therapy strategy in patients 60 years and older without traumatic vertebral disc lesion. On the other hand, patients with accompanying intervertebral disc lesion and those who are biologically young and very active might benefit from a more complex anterior–posterior approach.
Conclusions
An MRI should be part of the diagnostic workup prior to surgery, to rule out accompanying further lesions such as bone oedema and vertebral disc lesions.
A 360°-stabilization in osteoporotic vertebral fractures of the thoracolumbar spine is indicated in patients with acute or subacute fracture situation and relevant lesion of the posterior cortex and in patients with severe kyphotic malalignment (>20°).
Whereas an anterior–posterior approach including ventral spondylodesis is indicated in patients with accompanying relevant intervertebral disc lesion and biologically young and active patients, we see the indication for a hybrid stabilization in older patients without disc lesion and the above-mentioned fracture situation.
References
Ackland DC, Merritt JS, Pandy MG. Moment arms of the human neck muscles in flexion, bending and rotation. J Biomech. 2011;44(3):475–86. doi:10.1016/j.jbiomech.2010.09.036.
Adams MA, Dolan P. Biomechanics of vertebral compression fractures and clinical application. Arch Orthop Trauma Surg. 2011;131(12):1703–10. doi:10.1007/s00402-011-1355-9.
Aquarius R, Homminga J, Verdonschot N, Tanck E. The fracture risk of adjacent vertebrae is increased by the changed loading direction after a wedge fracture. Spine (Phila Pa 1976). 2011;36 (6):E408–412. doi:10.1097/BRS.0b013e3181f0f726.
Blattert TR, Katscher S, Josten C. Percutaneous techniques in the thoracic and lumbar spine. Unfallchirurg. 2011;114(1):17–25. doi:10.1007/s00113-010-1939-9.
Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983; 8 (8):817–831.
Geiger F, Kafchitsas K, Rauschmann M. Anterior vertebroplasty of adjacent levels after vertebral body replacement. Eur Spine J. 2011;20(8):1385–92. doi:10.1007/s00586-011-1766-x.
Glasmacher S, Glinsky A, Schmidt C, Jarvers JS, Josten C. Hat die Zementlage bei der Kyphoplastie Einfluss auf die Nachsinterung und den Korrekturverlust? Paper presented at the DKOU 2012, Berlin, Germany. 2012.
Heyde CE, Rohlmann A, Weber U, Kayser R. [Stabilization of the osteoporotic spine from a biomechanical viewpoint]. Der. Orthopade. 2010;39(4):407–16. doi:10.1007/s00132-009-1574-8.
Hoffmann C, Spiegl UJ, Hauck S, Buhren V, Gonschorek O. [What is the effect of ventral thoracoscopic spondylodesis (VTS) on elderly patients and what is the medium-term outcome?] Zeitschrift fur Orthopadie Unfallchirurgie. 2013;151(3):257–63. doi:10.1055/s-0032-1328522.
Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg. 1970;52(8):1534–51.
Josten C, Heyde CE, Spiegl UJ. Complex pathologies of the spine: trauma meets degeneration. Zeitschrift fur Orthopadie Unfallchirurgie. 2016. doi:10.1055/s-0042-108344.
Josten C, Jarvers JS, Glasmacher S, Heyde CE, Spiegl U. Anterior transarticular atlantoaxial screw fixation in combination with dens screw fixation for type II odontoid fractures with associated atlanto-odontoid osteoarthritis. Eur Spine J. 2016.
Josten C, Schmidt C, Spiegl U. Osteoporotic vertebral body fractures of the thoracolumbar spine: diagnostics and therapeutic strategies. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen. 2012;83 (10):866–874. doi:10.1007/s00104-012-2338-2.
Korovessis P, Hadjipavlou A, Repantis T. Minimal invasive short posterior instrumentation plus balloon kyphoplasty with calcium phosphate for burst and severe compression lumbar fractures. Spine (Phila Pa 1976). 2008;33 (6):658–667. doi:10.1097/BRS.0b013e318166e0bb.
Leidig-Bruckner G, Genant HK, Minne HW, Storm T, Thamsborg G, Bruckner T, Sauer P, Schilling T, Soerensen OH, Ziegler R. Comparison of a semiquantitative and a quantitative method for assessing vertebral fractures in osteoporosis. Osteoporos Int. 1994;4(3):154–61.
Louis R. Unstable fractures of the spine. III. Instability. A. Theories concerning instability. Revue de chirurgie orthopedique et reparatrice de l’appareil moteur. 1977;63(5):423–425.
Lunt M, O’Neill TW, Felsenberg D, Reeve J, Kanis JA, Cooper C, Silman AJ, European Prospective Osteoporosis Study G. Characteristics of a prevalent vertebral deformity predict subsequent vertebral fracture: results from the European Prospective Osteoporosis Study (EPOS). Bone. 2003;33(4):505–13.
Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3(4):184–201.
Pickett GE, Campos-Benitez M, Keller JL, Duggal N. Epidemiology of traumatic spinal cord injury in Canada. Spine (Phila Pa 1976). 2006;31(7):799–805. doi:10.1097/01.brs.0000207258.80129.03.
Reinhold M, Knop C, Beisse R, Audige L, Kandziora F, Pizanis A, Pranzl R, Gercek E, Schultheiss M, Weckbach A, Buhren V, Blauth M. Operative treatment of traumatic fractures of the thoracic and lumbar spinal column. Part I: epidemiology. Der Unfallchirurg. 2009;112(1):33–42, 44–35. doi:10.1007/s00113-008-1524-7.
Rodriguez-Vela J, Lobo-Escolar A, Joven-Aliaga E, Herrera A, Vicente J, Sunen E, Loste A, Tabuenca A. Perioperative and short-term advantages of mini-open approach for lumbar spinal fusion. Eur Spine J. 2009;18(8):1194–201. doi:10.1007/s00586-009-1010-0.
Schnake KJ, Blattert TR, Zimmermann V, Katscher S, Verheyden AP, Schinkel C, Scherer M. (2013) Entwicklung einer Klassifikation für osteoporotische Wirbelfrakturen und eines Scores zur therapeutischen Indikationsfindung (OF-Klassifikation und OF-Score) Paper presented at the DKOU 2013, Berlin.
Spiegl UJ, Beisse R, Hauck S, Grillhosl A, Buhren V. Value of MRI imaging prior to a kyphoplasty for osteoporotic insufficiency fractures. Eur Spine J. 2009;18(9):1287–92. doi:10.1007/s00586-009-1045-2.
Spiegl UJ, Hauck S, Merkel P, Buhren V, Gonschorek O. [Long-term results of kyphoplasty with additive dorsal instrumentation of incomplete burst fractures of the thoracolumbar spine in the elderly]. Zeitschrift fur Orthopadie Unfallchirurgie. 2012;150(6):579–82. doi:10.1055/s-0032-1327936.
Spiegl UJ, Jarvers JS, Heyde CE, Glasmacher S, Von der Hoh N, Josten C. [Delayed indications for additive ventral treatment of thoracolumbar burst fractures: what correction loss is to be expected]. Unfallchirurg. 2015. doi:10.1007/s00113-015-0056-1.
Taylor RS, Fritzell P, Taylor RJ. Balloon kyphoplasty in the management of vertebral compression fractures: an updated systematic review and meta-analysis. Eur Spine J. 2007;16(8):1085–100.
Toyone T, Ozawa T, Kamikawa K, Watanabe A, Matsuki K, Yamashita T, Shiboi R, Takeuchi M, Wada Y, Inada K, Aoki Y, Inoue G, Ohtori S, Tanaka T. Subsequent vertebral fractures following spinal fusion surgery for degenerative lumbar disease: a mean ten-year follow-up. Spine (Phila Pa 1976). 2010;35(21):1915–1918. doi:10.1097/BRS.0b013e3181dc846c.
Uchida K, Nakajima H, Yayama T, Miyazaki T, Hirai T, Kobayashi S, Chen K, Guerrero AR, Baba H. Vertebroplasty-augmented short-segment posterior fixation of osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine: comparisons with posterior surgery without vertebroplasty and anterior surgery. J Neurosurg Spine. 2010;13(5):612–21. doi:10.3171/2010.5.SPINE09813.
Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, Reinhold M, Aarabi B, Kandziora F, Chapman J, Shanmuganathan R, Fehlings M, Vialle L, Injury AOSC, Trauma Knowledge F. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 2013;38 (23):2028–2037. doi:10.1097/BRS.0b013e3182a8a381.
Watanabe M, Sakai D, Yamamoto Y, Sato M, Mochida J. Upper cervical spine injuries: age-specific clinical features. J Orthopaed Sci Off J Jpn Orthopaed Assoc. 2010;15(4):485–92. doi:10.1007/s00776-010-1493-x.
Weiss T, Hauck S, Buhren V, Gonschorek O. [Repositioning options with percutaneous dorsal stabilization : For burst fractures of the thoracolumbar junction.]. Unfallchirurg. 2013. doi:10.1007/s00113-013-2364-7.
Whitesides TE, Jr. (1977) Traumatic kyphosis of the thoracolumbar spine. Clin Orthopaed Relat Res. 128:78–92.
Yan D, Duan L, Li J, Soo C, Zhu H, Zhang Z. Comparative study of percutaneous vertebroplasty and kyphoplasty in the treatment of osteoporotic vertebral compression fractures. Arch Orthop Trauma Surg. 2011;131(5):645–50. doi:10.1007/s00402-010-1188-y.
Zellner BS, Dawson JR, Reichel LM, Schaefer K, Britt J, Hillin C, Reitman CA. Prospective nutritional analysis of a diverse trauma population demonstrates substantial hypovitaminosis D. J Orthop Trauma. 2014;28(9):e210–e215. doi:10.1097/BOT.0000000000000053.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
U. J. Spiegl, J.-S. Jarvers, C.-E. Heyde and C. Josten declare that they have no conflict of interest.
This article does not contain any studies with human or animal subjects performed by any of the authors.
Rights and permissions
About this article
Cite this article
Spiegl, U., Jarvers, JS., Heyde, CE. et al. Osteoporotic vertebral body fractures of the thoracolumbar spine: indications and techniques of a 360°-stabilization. Eur J Trauma Emerg Surg 43, 27–33 (2017). https://doi.org/10.1007/s00068-016-0751-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-016-0751-9