Abstract
Purpose
To evaluate the dose–volume parameters of the pericardium and heart in order to reduce the risk of radiation-induced pericardial effusion (PE) and symptomatic PE (SPE) in esophageal cancer patients treated with concurrent chemoradiotherapy.
Methods
In 86 of 303 esophageal cancer patients, follow-up CT was obtained at least 24 months after concurrent chemoradiotherapy. Correlations between clinical factors, including risk factors for cardiac disease, dosimetric factors, and the incidence of PE and SPE after radiotherapy were analyzed using Cox proportional hazard regression analysis. Significant dosimetric factors with the highest hazard ratios were investigated using zones separated according to their distance from esophagus.
Results
PE developed in 49 patients. Univariate analysis showed the mean heart dose, heart V5–V55, mean pericardium dose, and pericardium V5–V50 to all significantly affect the incidence of PE. Additionally, body surface area was correlated with the incidence of PE in multivariate analysis. Grade 3 and 4 SPE developed in 5 patients. The pericardium V50 and pericardium D10 significantly affected the incidence of SPE. The pericardium V50 in patients with SPE ranged from 17.1 to 21.7%. Factors affecting the incidence of SPE were the V50 of the pericardium zones within 3 cm and 4 cm of the esophagus.
Conclusion
A wide range of radiation doses to the heart and pericardium were related to the incidence of PE. A pericardium V50 ≤ 17% is important to avoid symptomatic PE in esophageal cancer patients treated with concurrent chemoradiotherapy.
Zusammenfassung
Ziel
Beurteilung der Dosis-Volumen-Parameter für Perikard und Herz zur Risikoreduzierung eines strahleninduzierten Perikardergusses (PE) und eines symptomatischen PE (SPE) bei mit kombinierter Strahlenchemotherapie behandelten Speiseröhrenkrebspatienten.
Methoden
Bei 86 von 303 Speiseröhrenkrebspatienten wurde mindestens 24 Monate nach der Strahlenchemotherapie ein Kontroll-CT angefertigt. Die Korrelationen zwischen klinischen Faktoren, einschließlich Risikofaktoren für Herzerkrankungen, dosimetrischen Faktoren und der Inzidenz eines PE und SPE nach Strahlentherapie wurden mittels proportionaler Cox-Regressionsanalyse analysiert. Signifikante dosimetrische Faktoren mit den höchsten Hazard Ratios wurden unter Verwendung des Bereichs, der entsprechend dem Abstand vom Ösophagus abgegrenzt wurde, untersucht.
Ergebnisse
Einen PE hatten 49 Patienten. Die univariate Analyse ergab einen signifikanten Einfluss von mittlerer Herzdosis, Herz V5–V55, mittlerer Perikarddosis und Perikard V5–V50 auf die PE-Inzidenz. Die multivariate Analyse zeigte eine Korrelation zwischen Körperoberfläche und PE-Inzidenz. Bei 5 Patienten trat ein SPE Grad 3 und 4 auf. Perikard V50 und D10 beeinflussten die Inzidenz eines SPE signifikant. Die Spanne von Perikard V50 bei SPE betrug 17,1–21,7 %. Beeinflussende Faktoren für die SPE-Inzidenz war V50 in den 3 und 4 cm von der Speiseröhre entfernten Perikardbereichen.
Schlussfolgerung
Eine breite Spanne von an Herz und Perikard abgegebenen Strahlendosen korrelierten mit der PE-Inzidenz. Ein Perikard V50 ≤ 17 % ist wichtig, um einen SPE bei Speiseröhrenkrebspatienten unter Strahlenchemotherapie zu vermeiden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Reported radiation-induced cardiac diseases include pericarditis, coronary artery disease, valvular disease, cardiomyopathy, and conduction abnormalities [1–3]. These different clinical manifestations have different latency periods, which range from months to decades [4–7].
Pericardial effusion (PE) occurs as the earliest radiation-induced cardiac complication. As the prognosis of esophageal cancer is poor, asymptomatic PE is a common late complication in patients with esophageal cancer treated with radiotherapy [8]. Although there have been several reports regarding PE, the following problems remained in evaluating their results: First, the definition of PE in computed tomography (CT) was not consistent. Second, the minimal follow-up periods or the minimal intervals between the radiotherapy and the obtained CT at the time of PE were short, which underestimated the true incidence of PE. Third, several PE patients developed symptoms. Differences in factors affecting the incidence of PE and symptomatic pericardial effusion (SPE) are not yet clear. Finally, of the reported pericardium (PC) and heart dosimetric factors , the most important predictor has not yet been clearly established.
The aim of this retrospective study is to investigate the dose–volume parameters of the PC and heart with the aim of reducing radiation-induced PE and SPE in esophageal cancer patients treated with concurrent chemoradiotherapy (CCRT). PE was diagnosed based on CT findings, and patients who underwent chest CT more than 2 years after radiotherapy were selected.
Methods
Patients
Between January 2000 and July 2013, 303 patients with newly diagnosed esophageal cancer were treated with CCRT without surgery. After the exclusions outlined in Fig. 1, 86 patients were used for the analysis.
Evaluation of pericardial effusion and symptomatic pericardial effusion
An enhanced CT scan with 5 mm slice thickness of the chest was obtained before and after CCRT. CT scans were performed every 3–6 months, and were individually scheduled according to clinical findings during the 5 years after completion of CCRT. As the thickness of the pericardial fluid at the base of the cardiac ventricles and apex of the cardiac atriums was difficult to measure using axial CT images, the largest thickness of pericardial fluid between 3 cm above the diaphragm and 3 cm below the left pulmonary artery was selected (Fig. 2a). The median thickness of the PC with and without pericardial fluid before CCRT was 0.2 cm (range: 0.1–0.6). The presence of PE was defined as a thickness of the pericardial fluid >0.6 cm. The time of PE onset was defined as the interval between radiotherapy and the first presence of PE on CT.
Representative axial CT images. a The longest distance measured at the pericardial space between 3 cm above the diaphragm and 3 cm below the left pulmonary artery shows the thickness of the pericardial fluid (between the two arrows). b The zone separated 3 cm from the esophagus. PC>3 cm E pericardium more than 3 cm away from the esophagus (yellow), HT >3 cm E heart more than 3 cm away from the esophagus (red), PC≤ 3 cm E pericardium within 3 cm of the esophagus (light blue), HT ≤ 3 cm E heart within 3 cm of the esophagus (blue)
The time to SPE was defined as the interval between radiotherapy and the first documented cardiac symptoms. The toxicity grading was reviewed by a single cardiologist using the Common Terminology Criteria for Adverse Events (CTCAE), version 4.0.
Dosimetric analysis
Planning CT was obtained using a CT scanner with a 2.5–5 mm slice thickness. The proposed Atlas was used to delineate the whole heart contour [9] and the surrogate PC, for which the contoured heart served as the inner boundary of the shell extending three-dimensionally outward by 0.5 cm in thickness [10]. The heart and PC dose–volume histograms (DVH) were calculated using Pinnacle3, version 9.2 (Philips Medical Systems, Hanover, MA, USA).
Treatment
The clinical target volume (CTV) encompassed the primary gross tumor volume (GTV) with 4 cm superior and inferior margins and regional lymph nodes. The planning tumor volume (PTV) was defined as the CTV + 1 cm. Anterior–posterior opposed treatment fields were typically used initially to deliver up to 40–45 Gy to the PTV. Dose inhomogeneities within the target volume had to be less than 5%.
The boost CTV included the GTV with 2 cm superior and inferior, and 0.5 cm radial margins, and also contained involved nodes with 0.5 cm margins. An additional dose was delivered to the boost PTV using oblique beams to avoid cords. Radiotherapy was delivered by using linear accelerators with 15 MV photons, with daily fractional doses of 1.8–2.0 Gy.
Combined 5‑fluorouracil (5-FU) and cisplatin was the most common regimen for patients with CCRT. Combined docetaxel and cisplatin was the most common regimen for adjuvant chemotherapy [11].
Statistics
The cumulative incidence of events was calculated using Kaplan–Meier survival analyses. Cox proportional hazard regression analysis was used for univariate and multivariate analyses. Correlations between clinical factors, including risk factors for cardiac disease, dosimetric factors, and the incidence of PE and SPE after radiotherapy, were analyzed [12]. Dosimetric factors were treated as continuous variables. Factors with a P-value of <0.05 were considered significant. All analyses were performed using SPSS version 24.0 (IBM Corp., Armonk, NY, USA). Of the percentage volumes receiving doses greater than 5–65 Gy (V5–V65), the significant factors with the highest hazard ratios (HR) were investigated using zones separated according to the distance from the esophagus.
Results
Pericardial effusion and symptomatic pericardial effusion
The median clinical follow-up of these 86 patients was 56.5 months (range: 25–125 months). The distribution of the clinical factors is shown in Table 1. There were 82 patients with squamous cell carcinoma, 2 with adenocarcinoma, and 2 with small cell carcinoma.
The overall and disease-free survival rates of the 86 patients at 5 years obtained by Kaplan–Meier product-limited methods were 80.6 and 52.8%, respectively. Of the 86 patients, 49 (57.0%) were diagnosed with PE using a CT scan. The actual incidence of PE was 45% at 5 years. PE developed 2–108 months after radiotherapy (median 6 months) and occurred within 24 months in 45 patients (91.8%).
Five patients developed SPE (grade 3 and 4). None of these patients had a history of heart disease before radiotherapy. Chest pain and dyspnea developed 8–41 months after radiotherapy (median 22 months). Two patients required urgent pericardial fluid drainage (grade 4). The other three patients did not have drainage, but required observation by cardiologists for 70–110 months (grade 3). Among these three patients, one was admitted twice for severe symptoms, but improved without treatment. Another patient was evaluated without pericardiocentesis because of thrombocytopenia. The other patient with SPE later developed paroxysmal atrial tachycardia and required catheter ablation.
Univariate analysis
Univariate analysis of the clinical factors possibly affecting the incidence of PE and SPE are presented in Table 1. No clinical factors, including risk factors for the development of cardiac disease, were associated with the incidence of PE and SPE.
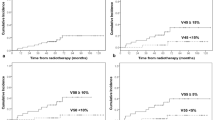
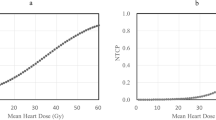
Univariate analysis of the heart and PC dosimetric factors possibly affecting the incidence of PE and SPE are shown in Table 2. The mean heart dose, heart V5–V55, mean PC dose, and PC V5–V50 were significantly correlated with the incidence of PE. The HRs for these factors were close to 1, because the HRs were calculated per 1% increase in the percentage volume of the heart and PC DVHs. The PC V50 and PC D10 (the minimum dose to the hottest 10%) significantly affected the incidence of SPE. The range of the PC V50 for patients with SPE was 17.1–21.7% (median 19.1). The cumulative incidence of SPE at 5 years was 32.1% in patients with a PC V50 > 17% (Fig. 3). The range of the PC V50 for all patients was 0–36.4% (median 9.1). Of these, 69 (80.2%) had V50 ≤ 17% and 17 (19.8%) had V50 > 17%. The range of the PC V50 for patients with PE was 0–36.4% (median 12.5%). Of these, 36 (73.5%) had V50 ≤ 17% and 13 (26.5%) had V50 > 17%.
Although the incidence of SPE was not significantly correlated with DVH factors for the heart, the P-value for incidence of SPE was the lowest (=0.05) for the heart V50.
Multivariate analysis
Dosimetric factors and body surface area (BSA), the other independent factor with a P-value <0.1 in univariate analysis, were analyzed in terms of the incidence of PE in multivariate analysis. The dosimetric parameters were correlated with each other. The heart and PC V50 values had the highest HR in univariate analysis. Therefore, the heart and PC V50 values were analyzed separately in multivariate analysis. In multivariate analysis, heart V50, PC V50, and BSA significantly affected the incidence of PE (Table 3).
Different zones
For the incidence of PE, the highest HR for the significant factors among V5–V65 was the V50. For the incidence of SPE, a significantly higher incidence of SPE was found for the PC V50, and the P-value was the lowest (=0.05) for the heart V50 among V5–V65. Therefore, the heart and PC V50 values were investigated by separating the zone near the esophagus into two zones: the zone that includes the most PTV and the zone that was mostly outside the PTV.
The V50 of the zones of the heart and PC separated from the esophagus by 3 and 4 cm (Fig. 2b) were considered. The results of a univariate analysis of these factors are presented in Table 4. For the heart, all zones of the V50 separated by 3 and 4 cm affected the incidence of PE. For the PC, the zones >3 and >4 cm away from esophagus did not affected the incidence of PE. The incidence of SPE was influenced by the V50 of the PC zones within 3 and 4 cm of the esophagus. No heart factors of the V50 zones affected the incidence of SPE.
Discussion
A wide range of incidence rates for PE have been reported in esophageal cancer patients [10, 13, 14]. A high incidence (52.2%) of PE was reported by Tamari et al. at a median follow-up of 37 months [14]. Whereas, a lower incidence (27.7%) of PE was reported by Wei et al. at a median follow-up of 8.4 months, although an actuarial incidence of 48% was reported at 18 months [10]. A long follow-up period is important for investigating the true incidence of PE. In the current study, patients were selected with CTs obtained at least 24 months after radiotherapy, and PE was found to occur within 24 months in 91.8%. Compared with other reports, the median follow-up in this study was longer (56.5 months) and the incidence of PE was higher (57.0%). The median observed time to onset of PE in these reports was 5.3–6 months, which was compatible with the current finding of 6 months. Although PE was assessed from the follow-up chest CT, previous reports did not describe the criteria used to diagnose abnormal pericardial fluid. A normal pericardial sac contains approximately 15–50 ml of fluid. PE occurs when there is a significant accumulation of fluid (>50 mL) within the pericardial space [15]. There is no consensus for the diagnosis of abnormal pericardial fluid detected by a CT scan. This study defined the criteria of PE by CT.
The incidence and median onset times of SPE after CCRT in recent reports were 4.3–9.7% and 19–22 months, respectively [13, 14, 16, 17]. This is compatible with the present results, in which the incidence was 5.8% and the median onset of symptoms was at 22 months. A longer follow-up period is required for investigating SPE than for PE.
In a multivariate analysis, Tamari et al. reported that a body mass index (BMI) ≥19 kg/m2 was significant correlated with the development of PE [14]. In the current study, BMI results strongly correlated with BSA (data not shown). Here, BSA was investigated for correlation with the incidence of PE and SPE, as it affects the dose of chemotherapy agents. Besides DVH factors, only BSA was associated with the incidence of PE. Although cisplatin and 5‑FU were associated with increased risks of thrombus formation [8], no chemotherapy regimens were found to be related to the incidence of PE or SPE.
Wei et al. reported that a wide range of DVH cutoff points for the PC were associated with a significant risk of PE, whereas there were fewer DVH cutoff points for the heart associated with the risk of PE. Additionally, the DVH parameters given to the PC were highly correlated to those of the heart, making it difficult to distinguish between the importance of the individual parameters and their effects [10]. The current study found that the V50 was the most important DVH parameter and investigated it in separate zones. Except the V50 at the PC >3 cm away from the esophagus and the PC >4 cm away from esophagus, all factors were significantly correlated with PE. Whether DVHs of the PC are more reliable than those of the heart for determining the risk of PE was difficult to conclude from this study.
Only the V50 at the PC ≤ 3 cm and ≤4 cm away from the esophagus was correlated with SPE in the separate zone analysis. PC D10 significantly affected the incidence of SPE in univariate analysis. SPE was affected the most by DVH parameters that irradiated the PC near the PTV at a high dose. There may be some differences in the mechanisms between the development of PE and SPE. It was not possible to find factors in PE that significantly influenced the development of SPE (no data shown).
Tayler et al. summarized subclinical vascular abnormalities observed within months of irradiation for breast cancer in myocardial perfusion imaging studies. They suggested that defects in the irradiated heart initially occur more frequently in patients that have received more than 25 Gy to the heart excessively for 6 months after radiotherapy, and that they are located preferentially in areas of expected high dose. They suggested that irreversible and reversible myocardial perfusion defects may result from dose-dependent damage to the microvascular myocardium or blockage of a coronary artery [18]. Hardenbergh et al. reported a radiation dose-dependent perfusion defect in left breast cancer seen at 6 months with minimal defects at 0–10 Gy, and a 20% decrease in regional perfusion at 41–50 Gy [19]. Although no any myocardial perfusion imaging studies were performed in the present study, and it is difficult to compare with these studies, the median interval of PE between CCRT was 6 months, which was on the same timescale as myocardial perfusion imaging studies. Chello et al. reported that the total collagen concentration was significantly increased in the ventricular tissue of patients undergoing pericardiectomy for post-irradiative constrictive pericarditis. They found the effect of fibrosis caused by radiotherapy for patients with pericarditis was not only in the PC, but also in the myocardium [20]. In the current study, the incidence of PE was significantly affected by both the heart and PC dose at a wide range from V5–V55, which may be related to both microvascular damage to the myocardium and PC.
The V30 of the PC was found to be a risk factor for PE [10, 14], whereas higher PC doses were relevant for the incidence of SPE. Fukuda et al. revealed a mean PC V45 of 58% to be the optimal threshold, as analyzed by a receiver operator characteristic curve, in which the time to event was not considered [13]. There is still no consensus as to which parameters of the PC and heart are the most important factors for radiotherapy treatment planning. All of the current patients with SPE suffered from severe cardiac symptoms, which may have had a significant medical impact. The reported ratio of grade 3 or more SPE assessed using the same criteria as CTCAE version 4.0 was 36.4–66.7% for all ≥grade 3 late cardiac disease, and 30–50% for all ≥grade 3 late complications [11, 17, 21, 22]. The range of the PC V50 in the current patients with SPE was 17.1–21.7%. A PC V50 ≤17% was thus considered to be the most important dosimetric factor and this should be used as threshold for avoiding SPE.
Intensification of the radiation dose did not increase survival or local/regional control in the RTOG 85-01 trial. For patients with esophageal cancer treated with 5‑FU/cisplatin-based combined-modality therapy, the standard radiation dose was concluded to be 50.4 Gy [23]. Regardless of these results, a recent advanced radiotherapy technique, which could deliver a dose above 50.4 Gy to tumors with decreased doses to critical organs, did not clarify whether a dose above 50.4 Gy is unable to improve the treatment outcomes [24–27].
Conclusion
In esophageal cancer patients treated with CCRT, it was found that a wide range of radiation doses to the heart and PC were related to the incidence of PE. It was also found that a high dose to the PC affected the development of SPE with severe cardiac symptoms and that a PC V50 ≤17% was an important dosimetric factor.
References
Adams MJ, Lipshultz SE, Schwartz C, Fajardo LF, Coen V, Constine LS (2003) Radiation-associated cardiovascular disease: manifestations and management. Semin Radiat Oncol 13(3):346–356. doi:10.1016/S1053-4296(03)00026-2
Hooning MJ, Botma A, Aleman BM, Baaijens MH, Bartelink H, Klijn JG, Taylor CW, van Leeuwen FE (2007) Long-term risk of cardiovascular disease in 10-year survivors of breast cancer. J Natl Cancer Inst 99(5):365–375. doi:10.1093/jnci/djk064
Carver JR, Shapiro CL, Ng A, Jacobs L, Schwartz C, Virgo KS, Hagerty KL, Somerfield MR, Vaughn DJ, Panel ACSE (2007) American Society of Clinical Oncology clinical evidence review on the ongoing care of adult cancer survivors: cardiac and pulmonary late effects. J Clin Oncol 25(25):3991–4008. doi:10.1200/JCO.2007.10.9777
Brusamolino E, Baio A, Orlandi E, Arcaini L, Passamonti F, Griva V, Casagrande W, Pascutto C, Franchini P, Lazzarino M (2006) Long-term events in adult patients with clinical stage IA-IIA nonbulky Hodgkin’s lymphoma treated with four cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine and adjuvant radiotherapy: a single-institution 15-year follow-up. Clin Cancer Res 12(21):6487–6493. doi:10.1158/1078-0432.CCR-06-1420
Hancock SL, Donaldson SS, Hoppe RT (1993) Cardiac disease following treatment of Hodgkin’s disease in children and adolescents. J Clin Oncol 11(7):1208–1215
Hull MC, Morris CG, Pepine CJ, Mendenhall NP (2003) Valvular dysfunction and carotid, subclavian, and coronary artery disease in survivors of hodgkin lymphoma treated with radiation therapy. JAMA 290(21):2831–2837. doi:10.1001/jama.290.21.2831
Kaplan BM, Miller AJ, Bharati S, Lev M, Grais MI (1997) Complete AV block following mediastinal radiation therapy: electrocardiographic and pathologic correlation and review of the world literature. J Interv Card Electrophysiol 1(3):175–188
Beukema JC, van Luijk P, Widder J, Langendijk JA, Muijs CT (2015) Is cardiac toxicity a relevant issue in the radiation treatment of esophageal cancer? Radiother Oncol 114(1):85–90. doi:10.1016/j.radonc.2014.11.037
Feng M, Moran JM, Koelling T, Chughtai A, Chan JL, Freedman L, Hayman JA, Jagsi R, Jolly S, Larouere J, Soriano J, Marsh R, Pierce LJ (2011) Development and validation of a heart atlas to study cardiac exposure to radiation following treatment for breast cancer. Int J Radiat Oncol Biol Phys 79(1):10–18. doi:10.1016/j.ijrobp.2009.10.058
Wei X, Liu HH, Tucker SL, Wang S, Mohan R, Cox JD, Komaki R, Liao Z (2008) Risk factors for pericardial effusion in inoperable esophageal cancer patients treated with definitive chemoradiation therapy. Int J Radiat Oncol Biol Phys 70(3):707–714. doi:10.1016/j.ijrobp.2007.10.056
Ogino I, Watanabe S, Iwahashi N, Kosuge M, Sakamaki K, Kunisaki C, Kimura K (2016) Symptomatic radiation-induced cardiac disease in long-term survivors of esophageal cancer. Strahlenther Onkol 192(6):359–367. doi:10.1007/s00066-016-0956-1
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB (1998) Prediction of coronary heart disease using risk factor categories. Circulation 97(18):1837–1847
Fukada J, Shigematsu N, Takeuchi H, Ohashi T, Saikawa Y, Takaishi H, Hanada T, Shiraishi Y, Kitagawa Y, Fukuda K (2013) Symptomatic pericardial effusion after chemoradiation therapy in esophageal cancer patients. Int J Radiat Oncol Biol Phys 87(3):487–493. doi:10.1016/j.ijrobp.2013.07.008
Tamari K, Isohashi F, Akino Y, Suzuki O, Seo Y, Yoshioka Y, Hayashi Y, Nishida T, Takehara T, Mori M, Doki Y, Ogawa K (2014) Risk factors for pericardial effusion in patients with stage I esophageal cancer treated with chemoradiotherapy. Anticancer Res 34(12):7389–7393
Kardon DE, Borczuk AC, Factor SM (2000) Mechanism of pericardial expansion with cardiac enlargement. Cardiovasc Pathol 9(1):9–15
Kawaguchi G, Sasamoto R, Abe E, Ohta A, Sato H, Tanaka K, Maruyama K, Kaizu M, Ayukawa F, Yamana N, Liu J, Takeuchi M, Kobayashi M, Aoyama H (2015) The effectiveness of endoscopic submucosal dissection followed by chemoradiotherapy for superficial esophageal cancer. Radiat Oncol 10:31. doi:10.1186/s13014-015-0337-4
Kumekawa Y, Kaneko K, Ito H, Kurahashi T, Konishi K, Katagiri A, Yamamoto T, Kuwahara M, Kubota Y, Muramoto T, Mizutani Y, Imawari M (2006) Late toxicity in complete response cases after definitive chemoradiotherapy for esophageal squamous cell carcinoma. J Gastroenterol 41(5):425–432. doi:10.1007/s00535-006-1771-8
Taylor CW, McGale P, Darby SC (2006) Cardiac risks of breast-cancer radiotherapy: a contemporary view. Clin Oncol (R Coll Radiol) 18(3):236–246
Hardenbergh PH, Munley MT, Bentel GC, Kedem R, Borges-Neto S, Hollis D, Prosnitz LR, Marks LB (2001) Cardiac perfusion changes in patients treated for breast cancer with radiation therapy and doxorubicin: preliminary results. Int J Radiat Oncol Biol Phys 49(4):1023–1028
Chello M, Mastroroberto P, Romano R, Zofrea S, Bevacqua I, Marchese AR (1996) Changes in the proportion of types I and III collagen in the left ventricular wall of patients with post-irradiative pericarditis. Cardiovasc Surg 4(2):222–226
Konski A, Li T, Christensen M, Cheng JD, Yu JQ, Crawford K, Haluszka O, Tokar J, Scott W, Meropol NJ, Cohen SJ, Maurer A, Freedman GM (2012) Symptomatic cardiac toxicity is predicted by dosimetric and patient factors rather than changes in 18F-FDG PET determination of myocardial activity after chemoradiotherapy for esophageal cancer. Radiother Oncol 104(1):72–77. doi:10.1016/j.radonc.2012.04.016
Morota M, Gomi K, Kozuka T, Chin K, Matsuura M, Oguchi M, Ito H, Yamashita T (2009) Late toxicity after definitive concurrent chemoradiotherapy for thoracic esophageal carcinoma. Int J Radiat Oncol Biol Phys 75(1):122–128. doi:10.1016/j.ijrobp.2008.10.075
Minsky BD, Pajak TF, Ginsberg RJ, Pisansky TM, Martenson J, Komaki R, Okawara G, Rosenthal SA, Kelsen DP (2002) INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy. J Clin Oncol 20(5):1167–1174
Munch S, Aichmeier S, Hapfelmeier A, Duma MN, Oechsner M, Feith M, Combs SE, Habermehl D (2016) Comparison of dosimetric parameters and toxicity in esophageal cancer patients undergoing 3D conformal radiotherapy or VMAT. Strahlenther Onkol 192(10):722–729. doi:10.1007/s00066-016-1020-x
Fleckenstein J, Kremp K, Kremp S, Palm J, Rube C (2016) IMRT and 3D conformal radiotherapy with or without elective nodal irradiation in locally advanced NSCLC: a direct comparison of PET-based treatment planning. Strahlenther Onkol 192(2):75–82. doi:10.1007/s00066-015-0900-9
Fakhrian K, Oechsner M, Kampfer S, Schuster T, Molls M, Geinitz H (2013) Advanced techniques in neoadjuvant radiotherapy allow dose escalation without increased dose to the organs at risk : planning study in esophageal carcinoma. Strahlenther Onkol 189(4):293–300. doi:10.1007/s00066-012-0297-7
Yu WW, Zhu ZF, Fu XL, Zhao KL, Mao JF, Wu KL, Yang HJ, Fan M, Zhao S, Welsh J (2014) Simultaneous integrated boost intensity-modulated radiotherapy in esophageal carcinoma: early results of a phase II study. Strahlenther Onkol 190(11):979–986. doi:10.1007/s00066-014-0636-y
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I. Ogino, S. Watanabe, K. Sakamaki, Y. Ogino, C. Kunisaki, and K. Kimura declare that they have no competing interests.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Ogino, I., Watanabe, S., Sakamaki, K. et al. Dosimetric predictors of radiation-induced pericardial effusion in esophageal cancer. Strahlenther Onkol 193, 552–560 (2017). https://doi.org/10.1007/s00066-017-1127-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-017-1127-8