Abstract
Purpose
To evaluate clinical and dosimetric factors retrospectively affecting the risk of symptomatic cardiac disease (SCD) in esophageal cancer patients treated with radiotherapy.
Patients and methods
A total of 343 patients with newly diagnosed esophageal cancer were managed with concurrent chemoradiotherapy or radiotherapy alone. Of these, 58 patients were followed at our hospital for at least 4 years. Median clinical follow-up was 79 months. Cardiac toxicity was determined by Common Terminology Criteria for Adverse Events (CTCAE) v. 4.0. The maximum and mean doses to the heart and percentage of the volume were calculated from the dose–volume histograms.
Results
SCD manifested in 11 patients. The heart diseases included three pericardial effusions, one pericardial effusion with valvular disease and paroxysmal atrial tachycardia, three atrial fibrillations, one sinus tachycardia, one coronary artery disease, one chest pain with strongly suspected coronary artery disease, and one congestive heart failure. The actual incidence of SCD was 13.8 % at 5 years. Univariate and multivariate analyses of continuous variables revealed that the risk of developing an SCD depended on the volume of the heart receiving a dose greater than 45 Gy (V45), 50 Gy (V50), and 55 Gy (V55). No other clinical factors were found to influence the risk of SCD. For V45, V50, and V55, the lowest significant cutoff values were 15, 10, and 5 %, respectively.
Conclusion
High-dose and large-volume irradiation of the heart increased the risk of SCD in long-term survivors. Using modern radiotherapy techniques, it is important to minimize the heart dose–volume parameters without reducing the tumor dose.
Zusammenfassung
Ziel
Beurteilung von klinischen und dosimetrischen Faktoren, die mit Risiken eines retrospektiven Auftretens von symptomatischen Herzerkrankungen (SCD) bei Patienten zusammenhängen, die aufgrund eines Ösophaguskarzinoms strahlentherapeutisch behandelt wurden.
Patienten und Methoden
Insgesamt 343 Patienten mit neu diagnostiziertem Ösophaguskarzinom wurden mit kombinierter Chemo- und Strahlentherapie oder nur strahlentherapeutisch behandelt. In dieser Gruppe wurden 58 Patienten über mindestens 4 Jahre beobachtet. Die mediane klinische Beobachtungsdauer betrug 79 Monate. Die kardiale Toxizität wurde mit CTCAE v.4.0 ermittelt. Anhand der Dosis-Volumen-Histogramme wurden maximale und mittlere Strahlendosis im Herzen und der Prozentsatz des Volumens berechnet.
Ergebnisse
Bei 11 Patienten trat eine SCD auf: 3 perikardiale Effusionen, 1 perikardiale Effusion mit Klappenfehler und paroxysmaler atrialer Tachykardie, 3 atriale Fibrillationen, 1 Sinustachykardie, 1 Koronararterienerkrankung, 1 Brustschmerz mit starkem Verdacht auf Koronararterienerkrankung, 1 kongestive Herzinsuffizienz. Die tatsächliche SCD-Inzidenz betrug nach 5 Jahren 13,8%. Uni- und multivariate Analysen mit den stetigen Variablen ergaben, dass das Risiko für eine SCD vom Volumen des Herzens abhängt, das Dosen von mehr als 45 Gy (V45), V50 und V55 erhielt. Keine anderen klinischen Faktoren zeigten Auswirkungen auf das Risiko für symptomatische Herzerkrankungen. Bei V45, V50 und V55 betrug der niedrigste signifikante Toleranzwert jeweils 15, 10 und 5%.
Schlussfolgerung
Hochdosierte, großvolumige Bestrahlungen des Herzens wirkten sich auf das SCD-Risiko bei Langzeitüberlebenden aus. Dosis-Volumen-Parameter für das Herz müssen mit modernen Strahlentherapiemethoden verringert werden, ohne die Tumordosis zu reduzieren.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The effect of radiation therapy on the heart has been well discussed for breast cancer and Hodgkin’s disease. Radiation dosage [1–3], volume of the heart involved in the radiation field [4–6], and fraction size [7] were identified as risk factors for cardiac toxicities. Long-term survivors of Hodgkin’s lymphoma have increased risks for cardiac mortality after delivered total tumor doses of 30–40 Gy, where large volumes of the heart were included in the field. Increased cardiac mortality is also seen in women irradiated for breast cancer. Breast doses are generally 40–50 Gy, but only a small part of the heart is included in the treatment fields, and mean heart doses rarely exceed 10–15 Gy. The relative risks of cardiac mortality are consequently lower than for Hodgkin’s lymphoma survivors [8].
For patients with distal esophageal cancer, the dose delivered to the heart is 50 Gy or more [9]. The maximum dose delivered to the heart for patients with esophageal cancer is usually higher than that for patients with Hodgkin’s disease. The irradiated volume of the heart in esophageal cancer patients is larger than for breast cancer.
The Eastern Cooperative Oncology Group study compared a radiation therapy alone arm to those in an arm who received concurrent chemoradiotherapy (CCRT), with 2- and 5-year survival rates of 12 and 7 % in the radiation alone arm and 27 and 9 % in the CCRT arm, respectively [10]. Because the prognosis of most patients with esophageal cancer is poor, data on long-term survivors are limited [11]. There are few reports available and late complications of the heart are not well understood in long-term survivors with esophageal cancer treated by radiotherapy.
We retrospectively analyzed long-term survivors with esophageal cancer who were followed at our hospital for ≥ 4 years, in order to investigate the risk factors for radiation-induced symptomatic cardiac disease (SCD).
Methods
Patients
Between January 2000 and June 2011, 343 patients with newly diagnosed esophageal cancer were managed with CCRT or radiation alone without surgery. Patients who had received intracavitary brachytherapy for the esophagus or esophagectomy as salvage treatment were excluded from the study. The study was carried out with the approval of the institutional review board, in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). To avoid underestimating the true incidence of cardiac disease, we selected patients with a follow-up time of ≥ 48 months. This resulted in a median clinical follow-up for the remaining 58 patients of 79 months (range 48–127 months), with an interquartile range of 60–96 months. Of these 58 patients, 11 developed SCD.
Treatment
Radiotherapy was delivered with 15-MV photons with daily doses of 1.8–2.0 Gy, 5 days per week. The clinical target volume (CTV1) contained the primary gross tumor volume (GTV) with 4-cm superior–inferior margins and regional lymph nodes. Supraclavicular nodes were included if the involved tumor was located in or extended to the upper thoracic esophagus. Celiac axis nodes were not routinely treated. The planning tumor volume (PTV1) was defined as the CTV plus 1 cm. Anterior–posterior opposed treatment fields were used initially and delivered at 40–45 Gy to PTV1. The boost PTV2 was defined as the CTV2 (GTV with 2-cm superior–inferior and 0.5-cm radial margins) plus 0–1 cm. Involved nodes with 0.5-cm margins were also included in CTV2. An additional dose was delivered to PTV2 using oblique off-cord beams.
Combined cisplatin and 5-flourouracil (5-FU) was the most common regimen for patients with CCRT (continuous infusion of 500 mg/m2/day 5-FU and 5 mg/m2/day cisplatin administered on days 1–5, 8–12, 15–19, and 22–26) [12]. Combined cisplatin and docetaxel was the most common regimen for adjuvant chemotherapy (60 mg/m2 docetaxel on days 1 and 21, and 60 mg/m2 cisplatin on days 1 and 21).
Analysis of heart disease
The hospital charts were thoroughly reviewed in all patients, and we confirmed that no patients had cardiac-related symptoms before radiotherapy. Any evidence of cardiac symptoms after radiotherapy, history of heart disease, and risk factors for the development of cardiac disease, such as diabetes mellitus, total cholesterol, hypertension, and smoking habits, was recorded for each patient [13].
Cardiologists evaluated all patients with cardiac symptoms. The cardiac status of symptomatic patients was reviewed using electrocardiography by a single cardiologist (MK) and echocardiography by a single cardiologist (NI) with comparison of the data before and after radiotherapy. The time of onset of cardiac toxicity was defined as the interval between radiotherapy and the clinical presentation with cardiac symptoms.
Dosimetric analysis
A planning computed tomography (CT) scan was obtained using a CT scanner with 5-mm slice thickness before June 2009 and 2.5-mm slice thickness after June 2009. To improve the dose-reporting accuracy of whole heart contours, we used the Atlas proposed by Feng et al. [14] and the whole heart contour was contoured by a physician (IO). Dose distributions for the heart were calculated using the Philips Pinnacle3 software program (version 9.2; Philips, Amsterdam, Netherlands). The maximum and mean doses to the heart, D10 (minimum dose to the hottest 10 % of the heart), and the percentage of the heart volume were calculated from the dose–volume histogram (DVH).
Toxicity scoring
The toxicity variable used in this study was cardiac disorders, for which the grading was determined using the Common Terminology Criteria for Adverse Events (CTCAE), version 4.0 (http://evs.nci.nih.gov/ftp1/CTCAE/About.html).
Statistical analyses
The cumulative incidence of SCD was calculated using Kaplan–Meier survival analyses. Cox proportional hazard regression analysis was used for both univariate and multivariate analyses. Univariate analysis was used to evaluate correlations between clinical factors, dosimetric factors, and the incidence of cardiac symptoms after radiotherapy. Dosimetric factors were treated as continuous variables. To generate hypotheses by identifying the dose/toxicity threshold, the log-rank test was used for recursive partitioning analysis. Factors with a difference at the 0.05 level were considered significant. All analyses were carried out using SPSS version 21.0 (IBM SPSS Statistics for Windows, IBM Corp., Armonk, NY, USA).
Results
Patients
The distribution of clinical factors including risk factors for cardiac disease is shown in Table 1. Large numbers of stage 1A patients were noted. Many of these patients, who had other malignancies and esophageal cancer, were detected by Lugol chromoendoscopy screening and avoided aggressive treatment. Forty-one (71 %) patients were heavy smokers, with their Brinkman index (cigarettes per day multiplied by years of smoking) before radiotherapy ranging from 48 to 2220. A total of 12 patients had a history of heart disease before radiotherapy: 7 with arrhythmia and 5 with coronary artery disease. In addition, 22 patients had another primary cancer before or at the time of radiotherapy. There were 53 (91 %) patients with squamous cell carcinoma, 3 (5 %) with adenocarcinoma, and 2 (3 %) with small cell carcinoma. Treatment and dosimetric characteristics of the 58 patients are listed in Table 2. The median volume of the heart was 712.2 cm3 (range 435.4–1188.5 cm3). The median total dose delivered to the central tumor was 60 Gy (range 40–68 Gy).
Symptomatic patients
The clinical data and results for the 11 patients with SCD (grade 2 or more) are shown in Table 3. Cardiac symptoms developed 7–70 months after radiotherapy (median 37 months). SCD included thress pericardial effusions, one pericardial effusion with valvular disease and paroxysmal atrial tachycardia, three atrial fibrillations, one sinus tachycardia, one coronary artery disease, one cardiac chest pain with strongly suspected coronary artery disease, and one congestive heart failure. One patient died of congestive heart failure due to severely impaired left ventricular function (patient number 11). One patient with valvular disease had mild to moderate arterial valve stenosis (patient number 4).
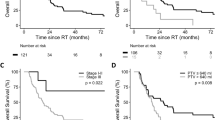
The actual incidence of SCD was 13.8 % at 5 years. Figure 1a shows the cumulative incidence of SCD by actuarial methods.
Univariate analysis
Factors affecting the incidence of SCD and univariate analyses are presented in Tables 1 and 2. Only dosimetric factors (V45, V50, and V55) with continuous variables were significantly correlated with the incidence of SCD in univariate analysis. Risk factors for the development of cardiac disease were not associated with the incidence of SCD.
Multivariate analysis
As the dosimetric parameters were highly correlated with each other, multivariate analysis included the dosimetric factors significant in univariate analysis analyzed separately. Factors in multivariate analysis also included gender, the other independent factor with a P-value < 0.1 in univariate analysis. In multivariate analysis, V45, V50, and V55 significantly affected the incidence of SCD compared with gender (Table 4).
Recursive partition analysis
Recursive partition analysis was used to derive hypotheses for the dose and volume parameters strongly affecting the incidence of SCD. The incidences of SCD were compared between the two groups using different cutoffs, and the P-value of the two groups is presented in Fig. 2. A dose range of 30–65 Gy in increments of 5 Gy, and the percent volume from heart DVHs were analyzed in the range of 5–85 % in increments of 5 %. For V45, V50, and V55—the continuous variable factors showing significant correlations with the incidence of SCD in univariate analysis—the most significant cutoff values were 45, 20, and 15 %, and the lowest but still significant cutoff values were 15, 10, and 5 %, respectively. The cumulative incidence of SCD for the lowest cutoff values are presented in Fig. 1b, c, and d.
Patients without a history of heart disease
We analyzed 46 patients without a history of heart disease. Because of a decreased number of total patients, only V55 (as a continuous variable) was a statistically significant risk factor of SCD in univariate analysis (P = 0.033; hazard ratio = 1.326, 95 % confidence interval = 1.020–1.708). Hazard ratio for these patients was similar to the original 58 patients. For V55, the lowest significant cutoff values were 5 % (P = 0.046).
Discussion
Radiation-induced cardiac diseases reported in the literature are pericardial effusion, pericarditis, coronary artery disease, valvular disease, cardiomyopathy, and conduction abnormalities [1–4, 15]. These different clinical manifestations have different latency periods which range from months to decades.
Acute pericarditis during radiotherapy is uncommon and pericarditis and pericardial effusion were reported to occur 1–42 months after radiotherapy [6, 16–18]. Although pericardial diseases are usually asymptomatic, Carmel et al. reported that 7.4 % of patients with Hodgkin’s disease had developed symptomatic radiation-induced pericarditis [2]. The incidence of symptomatic radiation-induced pericarditis was 6.9 % in our study, which is similar to the results of the latter study.
Coronary artery diseases were reported to occur 28–179 months after radiation therapy [1, 16, 17]. Hull et al. retrospectively studied 415 patients with Hodgkin’s disease with a median mid-mediastinal dose of 33 Gy. These authors found actual incidences of coronary artery disease of 3 % at 5 years, 6 % at 10 years, and 10 % at 20 years [4]. Swerdlow et al. reported that standardized mortality ratios decreased sharply with an older age at the initial treatment of Hodgkin’s disease, but absolute excess risks of death from myocardial infarction increased with an older age up to 65 years at initial treatment. The significantly increased risk of myocardial infarction mortality persisted through to 25 years after initial treatment [19]. The median age of patients in the current study was 68 years, and one definite case of coronary artery disease (1.7 %) was found at 5 years.
Hull et al. found actual incidences of clinically important valvular dysfunction of 1 % at 10 years, 4 % at 15 years, and 6 % at 20 years in 415 patients with Hodgkin’s disease. The most common valve lesion was aortic stenosis [4]. Heidenreich et al. recruited 294 asymptomatic patients treated with at least 35 Gy to the mediastinum for Hodgkin’s disease. Compared to those who had received irradiation within 10 years, patients who had received irradiation more than 20 years before evaluation had significantly more mild or greater aortic regurgitation (60 vs. 4 %, respectively), moderate or greater tricuspid regurgitation (4 vs. 0 %, respectively), and aortic stenosis (16 vs. 0 %, respectively) [20]. In our study, 1 patient (1.7 %) had mild to moderate aortic stenosis associated with pericardial effusion and paroxysmal atrial tachycardia.
There are a few reports regarding atrial fibrillation occurring after radiation therapy to the mediastinum. Gayed et al. reported on 2 patients (12.5 %) suffering from atrial fibrillation with an interval of 5.5–10.5 months after CCRT among 16 esophageal cancer patients [21]. In the present study, 3 (5.2 %) patients suffered atrial fibrillation 31–70 months after radiotherapy.
Congestive heart failure-related death was reported by Hancock et al. in Hodgkin’s disease patients with mediastinal radiation above 30 Gy. Congestive heart failure death was the second most common cause of cardiac disease death, arising in 24 (1.1 %) of 2232 patients, after 55 (2.4 %) cases of acute myocardial infarction [3]. Hooning et al. reported on radiotherapy using photon beams to either side of the internal mammary chain for breast cancer, which was associated with increased congestive heart failure compared with no radiotherapy. These authors stated that many cardiac events may be missed by restricting the study outcome to coronary artery disease only and not considering congestive heart failure [22]. In our results, one cardiac death (1.7 %) was caused by congestive heart failure.
Beukema et al. conducted a review of the current literature concerning cardiac toxicity in esophageal cancer patients treated with radiotherapy with or without chemotherapy. The overall crude incidence of SCD was as high as 10.8 % [23]. Among this literature, we selected studies of SCD for esophageal cancer and summarize them in Table 5 [5, 16, 17, 24]. The incidence of SCD increased with longer follow-up and our data include the greatest incidence in the list. Although our follow-up was 4 years or more, and this follow-up period may be too short to analyze the morbidity or mortality due to coronary artery disease and valvular disease; other radiation-induced cardiac diseases increased with a longer follow-up.
There are a few articles reporting on the correlation between the dose–volume parameters of the heart and SCD. Konski et al. evaluated 102 patients treated with CCRT for locally advanced esophageal cancer with a median prescribed dose of 50.4 Gy (range 45–57.6 Gy). These authors found the thresholds for symptomatic cardiac toxicity of V20, V30, and V40 to be above 70, 65, and 60 %, respectively. A total of 76 of the latter patients (74.5 %) underwent esophagectomy 4–6 weeks after completion of CCRT [5].
Intensity-modulated radiotherapy (IMRT) plans reduced unnecessary radiation to the heart compared with three-dimensional conformal radiotherapy (3DCRT) plans in esophageal cancer. Chen et al. found a heart V45 of less than 1 % with 50 Gy to the gross PTV and 45 Gy to the elective PTV treated by IMRT [25]. Lin et al. retrospectively studied stage II-IVA esophageal cancer typically treated with neoadjuvant CCRT to 50.4 Gy (range 6.6–66.6 Gy). These authors compared 413 3DCRT patients and 263 IMRT patients. Although they found that the rate of cardiac-related deaths was significantly lower after IMRT than after 3DCRT, and that there were no differences in the cumulative incidence of cancer-specific deaths, the authors did not propose a dose–volume parameter for the heart [26]. Despite the known associations of radiation with long-term cardiac toxicities, there is neither a consensus statement nor are there specific recommendations on a dose–volume parameter for the heart.
In INT 0123, a higher radiation dose (64.8 Gy) did not increase survival or local/regional control, and it was concluded that the standard radiation dose for patients treated with concurrent 5-FU and cisplatin chemotherapy is 50.4 Gy [9]. Regardless of these results, whether a dose above 50.4 Gy is unable to improve the treatment outcome is not clear. In the present study, V45, V50, and V55 were analyzed as continuous variables. A significantly higher incidence of SCD was seen in association with an increasing percentage of the volume in V45, V50, and V55. We selected a lower volume as a discriminator, with V45, V50, and V55 being above 15, 10, and 5 %, respectively. The implications of these results on dose reduction to the heart and identifying whether a tumor dose above 50.4 Gy can improve survival of patients treated with CCRT for esophageal cancer will require future long-term studies.
Conclusion
We generated hypotheses for future testing of V45, V50, and V55 of the heart being below 15, 10, and 5 % to reduce SCD. All multiple beams have recently been applied simultaneously during each treatment fraction, whereas most of our patients were treated with initial anterior–posterior beams followed by oblique off-cord beams. It is necessary to minimize the dose–volume parameter of the heart without reducing the tumor dose using modern radiotherapy techniques for esophageal cancer patients.
References
Brusamolino E, Baio A, Orlandi E, Arcaini L, Passamonti F, Griva V, Casagrande W, Pascutto C, Franchini P, Lazzarino M (2006) Long-term events in adult patients with clinical stage IA–IIA nonbulky Hodgkin’s lymphoma treated with four cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine and adjuvant radiotherapy: a single-institution 15-year follow-up. Clin Cancer Res 12:6487–6493. doi:10.1158/1078-0432.CCR-06-1420
Carmel RJ, Kaplan HS (1976) Mantle irradiation in Hodgkin’s disease. An analysis of technique, tumor eradication, and complications. Cancer 37:2813–2825
Hancock SL, Tucker MA, Hoppe RT (1993) Factors affecting late mortality from heart disease after treatment of Hodgkin’s disease. JAMA 270:1949–1955
Hull MC, Morris CG, Pepine CJ, Mendenhall NP (2003) Valvular dysfunction and carotid, subclavian, and coronary artery disease in survivors of hodgkin lymphoma treated with radiation therapy. JAMA 290:2831–2837. doi:10.1001/jama.290.21.2831
Konski A, Li T, Christensen M, Cheng JD, Yu JQ, Crawford K, Haluszka O, Tokar J, Scott W, Meropol NJ, Cohen SJ, Maurer A, Freedman GM (2012) Symptomatic cardiac toxicity is predicted by dosimetric and patient factors rather than changes in 18F-FDG PET determination of myocardial activity after chemoradiotherapy for esophageal cancer. Radiother Oncol 104:72–77. doi:10.1016/j.radonc.2012.04.016
Wei X, Liu HH, Tucker SL, Wang S, Mohan R, Cox JD, Komaki R, Liao Z (2008) Risk factors for pericardial effusion in inoperable esophageal cancer patients treated with definitive chemoradiation therapy. Int J Radiat Oncol Biol Phys 70:707–714. doi:10.1016/j.ijrobp.2007.10.056
Cosset JM, Henry-Amar M, Pellae-Cosset B, Carde P, Girinski T, Tubiana M, Hayat M (1991) Pericarditis and myocardial infarctions after Hodgkin’s disease therapy. Int J Radiat Oncol Biol Phys 21:447–449
Stewart FA, Seemann I, Hoving S, Russell NS (2013) Understanding radiation-induced cardiovascular damage and strategies for intervention. Clin Oncol 25:617–624. doi:10.1016/j.clon.2013.06.012
Minsky BD, Pajak TF, Ginsberg RJ, Pisansky TM, Martenson J, Komaki R, Okawara G, Rosenthal SA, Kelsen DP (2002) INT 0123 (Radiation Therapy Oncology Group 94–05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy. J Clin Oncol 20:1167–1174
Smith TJ, Ryan LM, Douglass HO Jr, Haller DG, Dayal Y, Kirkwood J, Tormey DC, Schutt AJ, Hinson J, Sischy B (1998) Combined chemoradiotherapy vs. radiotherapy alone for early stage squamous cell carcinoma of the esophagus: a study of the Eastern Cooperative Oncology Group. Int J Radiat Oncol Biol Phys 42:269–276
Ordu AD, Nieder C, Geinitz H, Kup PG, Deymann LF, Scherer V, Combs SE, Fakhrian K (2015) Radio(chemo)therapy for locally advanced squamous cell carcinoma of the esophagus: long-term outcome. Strahlenther Onkol 191:153–160. doi:10.1007/s00066-014-0779-x
Takagawa R, Kunisaki C, Makino H, Kosaka T, Ono HA, Akiyama H, Shimada H (2009) Efficacy of chemoradiotherapy with low-dose cisplatin and continuous infusion of 5-fluorouracil for unresectable squamous cell carcinoma of the esophagus. Dis Esophagus 22:482–489. doi:10.1111/j.1442-2050.2008.00935.x
Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB (1998) Prediction of coronary heart disease using risk factor categories. Circulation 97:1837–1847
Feng M, Moran JM, Koelling T, Chughtai A, Chan JL, Freedman L, Hayman JA, Jagsi R, Jolly S, Larouere J, Soriano J, Marsh R, Pierce LJ (2011) Development and validation of a heart atlas to study cardiac exposure to radiation following treatment for breast cancerl. Int J Radiat Oncol Biol Phys 79:10–18. doi:10.1016/j.ijrobp.2009.10.058
Kaplan BM, Miller AJ, Bharati S, Lev M, Martin Grais I (1997) Complete AV block following mediastinal radiation therapy: electrocardiographic and pathologic correlation and review of the world literature. J Interv Card Electrophysiol 1:175–188
Ishikura S, Nihei K, Ohtsu A, Boku N, Hironaka S, Mera K, Muto M, Ogino T, Yoshida S (2003) Long-term toxicity after definitive chemoradiotherapy for squamous cell carcinoma of the thoracic esophagus. J Clin Oncol 21:2697–2702. doi:10.1200/JCO.2003.03.055
Kumekawa Y, Kaneko K, Ito H, Kurahashi T, Konishi K, Katagiri A, Yamamoto T, Kuwahara M, Kubota Y, Muramoto T, Mizutani Y, Imawari M (2006) Late toxicity in complete response cases after definitive chemoradiotherapy for esophageal squamous cell carcinoma. J Gastroenterol 41:425–432. doi:10.1007/s00535-006-1771-8
Martel MK, Sahijdak WM, Ten Haken RK, Kessler ML, Turrisi AT (1998) Fraction size and dose parameters related to the incidence of pericardial effusions. Int J Radiat Oncol Biol Phys 40:155–161
Swerdlow AJ, Higgins CD, Smith P, Cunningham D, Hancock BW, Horwich A, Hoskin PJ, Lister A, Radford JA, Rohatiner AZ, Linch DC (2007) Myocardial infarction mortality risk after treatment for Hodgkin disease: a collaborative British cohort study. J Natl Cancer Inst 99:206–214. doi:10.1093/jnci/djk029
Heidenreich PA, Hancock SL, Lee BK, Mariscal CS, Schnittger I (2003) Asymptomatic cardiac disease following mediastinal irradiation. J Am Coll Cardiol 42:743–749
Gayed I, Gohar S, Liao Z, McAleer M, Bassett R, Yusuf SW (2009) The clinical implications of myocardial perfusion abnormalities in patients with esophageal or lung cancer after chemoradiation therapy. Int J Cardiovasc Imaging 25:487–495. doi:10.1007/s10554-009-9440-7
Hooning MJ, Botma A, Aleman BM, Baaijens MH, Bartelink H, Klijn JG, Taylor CW, van Leeuwen FE (2007) Long-term risk of cardiovascular disease in 10-year survivors of breast cancer. J Natl Cancer Inst 99:365–375. doi:10.1093/jnci/djk064
Beukema JC, van Luijk P, Widder J, Langendijk JA, Muijs CT (2015) Is cardiac toxicity a relevant issue in the radiation treatment of esophageal cancer? Radiother Oncol 114:85–90. doi:10.1016/j.radonc.2014.11.037
Morota M, Gomi K, Kozuka T, Chin K, Matsuura M, Oguchi M, Ito H, Yamashita T (2009) Late toxicity after definitive concurrent chemoradiotherapy for thoracic esophageal carcinoma. Int J Radiat Oncol Biol Phys 75:122–128. doi:10.1016/j.ijrobp.2008.10.075
Chen YJ, Liu A, Han C, Tsai PT, Schultheiss TE, Pezner RD, Vora N, Lim D, Shibata S, Kernstine KH, Wong JY (2007) Helical tomotherapy for radiotherapy in esophageal cancer: a preferred plan with better conformal target coverage and more homogeneous dose distribution. Med Dosim 32:166–171. doi:10.1016/j.meddos.2006.12.003
Lin SH, Wang L, Myles B, Thall PF, Hofstetter WL, Swisher SG, Ajani JA, Cox JD, Komaki R, Liao Z (2012) Propensity score-based comparison of long-term outcomes with 3-dimensional conformal radiotherapy vs intensity-modulated radiotherapy for esophageal cancer. Int J Radiat Oncol Biol Phys 84:1078–1085. doi:10.1016/j.ijrobp.2012.02.015
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I. Ogino, S. Watanabe, N. Iwahashi, M Kosuge, K. Sakamaki, C. Kunisaki, and K. Kimura state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Rights and permissions
About this article
Cite this article
Ogino, I., Watanabe, S., Iwahashi, N. et al. Symptomatic radiation-induced cardiac disease in long-term survivors of esophageal cancer. Strahlenther Onkol 192, 359–367 (2016). https://doi.org/10.1007/s00066-016-0956-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-016-0956-1