Abstract
Objective
Restoring stability after total knee arthroplasty (TKA) and improving joint function using a cemented rotating hinge system.
Indications
Ligament instability and/or osseous defects (including Anderson Orthopaedic Research Institute [AORI] classification type II defects) after primary TKA or TKA revision surgery.
Contraindications
Distal femoral or proximal tibial bowing requiring implant systems that provide femoral or tibial offset stems. Persistent periprosthetic infection. Poor therapeutic compliance. AORI type III defects.
Surgical technique
Medial arthrotomy. Femoral and tibial component removal with small saw blades and chisels. Intramedullary alignment for the tibial and femoral cuts. Debridement and removal of membranes and cement remnants. Reconstruction of joint line and correct TKA alignment. Trial reduction. Cement fixation.
Postoperative management
Unrestricted range of motion, partial weight bearing for 4 weeks.
Results
Between 2012 and 2013, 18 patients suffering from ligament insufficiency after TKA were revised using the described system and included in a prospective study protocol. The mean follow-up was 37 months (range 30–46 months). There was a significant improvement of the Oxford Knee Score (OKS) from 19 (range 7–29) preoperatively to 29 (range 10–45) postoperatively (p = 0.004). The Knee Society Score (KSS) knee assessment subscore improved from 35 (range 9–70) to 67 (range 35–97) (p = 0.002) and the pain score from 7 (range 0–50) to 24 (range 0–50) (p = 0.008).
Zusammenfassung
Operationsziel
Funktionsverbesserung und Behandlung der Knieprotheseninstabilität durch Wechsel auf eine vollständig zementierte, rotationsachsgeführte Knieprothese.
Indikationen
Bandinsuffizienz und/oder Knochenverlust (bis einschließlich AORI [Anderson Orthopaedic Research Institute] Typ-II-Defekte) nach primärer Knieprothesenimplantation oder Revision.
Relative Kontraindikationen
Höhergradige femorale oder tibiale Achsabweichungen, die ein stielgeführtes Revisionssystem mit Offset-Varianten notwendig machen. Persistierende periprothetische Infektion. Fehlende Compliance. Knochendefekt AORI Typ III.
Operationstechnik
Mediale Arthrotomie, Entfernung der einliegenden femoralen und tibialen Komponenten mit kleinen, flachen Sägeblättern und Meißeln. Intramedulläres Alignment für den tibialen und femoralen Sägeschnitt. Débridement und Entfernen von Membranen und Zementresten. Knochensparende Resektion für eine suffiziente Prothesenauflage. Rekonstruktion der Gelenklinie und korrektes Prothesenalignment. Probereposition. Vollständig zementierte Verankerung.
Nachbehandlung
Keine Bewegungseinschränkung. Teilbelastung für 4 Wochen.
Ergebnisse
In einer prospektiven Studie konnten 18 Patienten eingeschlossen werden, welche zwischen 2012 und 2013 aufgrund einer klinisch relevanten Instabilität nach Knieprothesenimplantation revidiert wurden. Das durchschnittliche Follow-up lag bei 37 Monaten (30–46). Es zeigte sich eine signifikante Verbesserung des OKS (Oxford Knee Score) von 19 (7–29) auf 29 (10–45) Punkte (p = 0,004), des KSS (Knie Funktion Scores) von 35 (9–70) auf 67 (35–97) Punkte (p = 0,002) und des Schmerz-Scores von 7 (0–50) auf 24 (0–50) Punkte (p = 0,008).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introductory remarks
Total knee arthroplasty (TKA) instability is one of the most frequent causes for TKA revision [2, 3]. It can be caused by a plethora of reasons including untreated intraoperative or postoperative ligament attenuation, wear, TKA loosening, component malpositioning, periprosthetic infection or implant failure. Revision of instable TKAs can be challenging due to ligament insufficiency, osseous defects, diminished bone quality, and lack of bony landmarks [1]. Restoration of the joint line and correct frontal, sagittal, and rotational alignment of the revision implant is crucial for postoperative knee function. Multiple pre- and intraoperative measurements have been proposed to determine the correct height of the joint line [9, 11, 13].
For correct component alignment, offset-stems or stem-extensions may be necessary to account for anatomic variants, which can be preoperatively anticipated by digital templating.
Reliable TKA fixation is crucial for sufficient long-term survival of the new implant. Spacers, wedges, cones, or sleeves enable surgeons to compensate for epiphyseal and metaphyseal bone loss. Multiple zone fixation can be achieved in an uncemented, fully cemented, or hybrid fashion [14].
Although treatment of TKA instability might be managed non-operatively with proprioceptive and muscle training, revision is indicated in most cases. Choosing the correct revision strategy may be challenging and is highly influenced by the underlying reason for instability and implant type. Finally, patient-specific factors such as comorbidities and body mass index, inter alia, need to be considered.
So far, there is no consensus on a classification system that allows derivation of the best treatment strategy with predictable results [4, 6, 8]. Thus, choice of therapy remains a case-by-case decision.
Rotating hinged prostheses offer a definite solution for high-grade TKA instability. The Link Endo-Model SL (Waldemar Link GmbH & Co. KG, Hamburg, Germany) is a rotating hinge knee, with a design inaugurated in the late 1970s, which has proven its clinical utility in multiple studies [1, 7]. Here, we describe a straightforward surgical approach using this system for TKA revision due to instability.
Surgical principle and objective
Restoring stability after TKA and improving joint function by TKA revision with a cemented rotating hinge prosthesis.
Advantages
-
Modular and monoblock system (no complex intraoperative assembly needed)
-
Distal femoral medial and lateral augments (ultra-high molecular weight polyethylene [UHMWPE] or Tilastan®, Waldemar Link GmbH & Co. KG, Hamburg, Germany; 25 mm height including the femoral component thickness) for reconstruction of the joint line
-
Half and complete tibial augments (in 5, 10, and 15 mm) and tibial cones (TrabecuLink®, Waldemar Link GmbH & Co. KG, Hamburg, Germany) to compensate for osseous defects
-
Centralizers to facilitate correct orientation of the stems
-
Intraoperative change from rotational to hinge knee possible with femur and tibia components in place
-
Simple coupling mechanism without the need for femoral soft tissue detachment or tissue distraction
-
Elastic titanium tibial cones (TrabecuLink®) available in four sizes and versions for additional metaphyseal cementless fixation
-
Conversion to distal femur/proximal tibia without femoral/tibial component removal (Megasystem C®, Waldemar Link GmbH & Co. KG, Hamburg, Germany)
-
Cemented or uncemented stems (CaP coating optional) Hypoallergenic TiNbN surface modification available (LINK PreEx®, Waldemar Link GmbH & Co. KG, Hamburg, Germany)
Disadvantages
-
No off-set options and anatomic stem extensions available
-
High stresses at the cement–bone–implant interface, especially for the hinge version
-
One size only femoral distal augments (to account for defects 25 mm proximal to the joint line)
Indications
-
Ligament instability and/or bone loss after primary or revision TKA
Contraindications
-
Distal femoral or proximal tibial bowing requiring implant systems that provide femoral or tibial offset stems
-
Persistent periprosthetic infection or active infection elsewhere
-
Poor therapeutic compliance
-
Anderson Orthopaedic Research Institute (AORI) classification type III osseous defects
-
Relative: Extensor mechanism defect
Patient information
-
General surgery related risks:
-
Infection
-
Neurovascular lesions
-
Blood loss
-
Thrombosis and embolism
-
Wound healing complications
-
-
Specific risks
-
Arthrofibrosis
-
Intraoperative fracture
-
Implant loosening
-
Malalignment
-
Prolonged rehabilitation period
-
Preoperative work up
-
History of giving-way symptoms
-
Clinical examination to check for mediolateral or global ligament insufficiency
-
Implants that need removal should be known and former surgical protocols should be made available
-
Standard radiographic workup (calibrated orthoroentgenogram standing, anteroposterior, lateral and Merchant view).
-
Joint aspiration to rule out infection
-
Preoperative digital templating. Especially small patients should undergo additional lateral imaging of the distal femur and knee joint to exclude a curvature misfit of nonanatomic femur stems within the medullary canal that might lead to perforation of the anterolateral femoral cortex during intramedullary reaming. Excessive tibial bowing (valgus) should also be excluded as tibial offset-stems are not available. This is particularly important in smaller patients where no compensation of the stem positioning is possible by reducing the tibial tray size. The height of the joint line and the height of the posterior femoral condylar offset should be anticipated preoperatively.
-
Patient education and discussion of patient expectations
-
Prior to admission, whole body and nasal decontamination with a lotion and gel based on octenidine dihydrochloride and allantoin
-
Patient blood management and allocation of erythrocyte concentrates
Instruments
-
Standard instruments for TKA revision surgery (i.e., chisels, flat saw blades)
-
Jet lavage
-
Instrument set for the Link Endo-Model SL
Anesthesia and positioning
-
General or spinal anesthesia
-
Supine position with leg holders (Fig. 1)
-
Perioperative administration of intravenous antibiotics; if procedure exceeds 2 h repeat administration
-
Thigh tourniquet; to be applied during the cementation process only.
Surgical technique
(Figs. 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14)
After medial arthrotomy, we first perform a radical synovectomy within the recessus suprapatellaris and all accessible joint spaces. Then the polyethylene liner is removed. Any wear debris has to be documented. Scar tissue around the patella and its tendon is meticulously removed and the femoral origins of the collateral ligaments are sacrificed. We try to perform a lateral patellafacettectomy at this stage to facilitate lateralization or even elevation of the patella by release of the lateral structures. In stiff joints, this might not be possible and further measures are necessary to gain adequate access to the implant without risking lesions of the extensor apparatus. In these cases, we first perform a quadriceps snip to decrease proximal lateral tightness and then remove the soft tissues at the anteromedial tibia during maximum external rotation of the tibia (“RanSall”-Manöver). In very contract joints, this subperiosteal elevation of soft tissues has to include the pes anserinus superficialis and profundus to achieve unimpeded visualization of the tibial tray. We then start to separate the femoral implant from the cement and bone using relatively short and fine saw blades. Care should be taken to preserve the underlying bone. Therefore, the blade should be inserted directly beneath the femoral component. Then the femoral implant is removed with gentle hammer blows
(a) The tibial component can now be accessed through maximum external rotation of the tibia. Using a straight Hohmann retractor the tibia can be moved forward. During this step, care should be taken not to damage the exposed cancellous bone of the distal femur by applying too much force to the Hohmann retractor. In case there is still too much tension to gain adequate access, we remove the soft tissues from the dorsal aspect of the distal femur. The tibial component is circumferentially freed of scar tissue and is loosened with a thin and fine saw blade and osteotome that is introduced between the tibial bone and the tray from medially during maximum external tibial rotation. (b) During this step, it is essential to carefully separate the bone under the dorsolateral tray from the implant and bone, respectively, in order to prevent iatrogenic defects of the dorsal tibial plafond during tibial tray removal. In rare cases and very contract knees, it might be difficult to lift the tibial tray. Then a small window is made at the anterior tibial cortex just under the tibial implant to push it out
After complete component removal, the tibial medullary cavity is opened using a trephine. Then, reamers with increasing diameters are inserted into the tibial medullary canal until firm diaphyseal grip is achieved for intramedullary alignment. The cutting block is assembled to the reamer, and the height of the tibial bone to be resected is measured with a stylus or angel wing to achieve a bone preserving cut perpendicular to the tibial shaft axis. We do not recommend removing cement remnants before the bone cuts are completed as this can result in large cavitary bone defects
The tibia is prepared first since the height of the tibial component affects both the flexion and extension gap. The trial baseplate with the best possible coverage of the tibial plateau is fixed with pins. We use several landmarks simultaneously to determine correct tibial tray rotation: The junction of the medial and middle third of the tibial tuberosity, the anterior tibial crest, the anterior cortex of the tibia, and the second metatarsal. Akagi’s line is not suitable in revision surgery as in many cases the tibial attachment of the posterior cruciate ligament cannot be identified anymore, nor is the posterior tibial condylar line which is interrupted in most revision cases due to bone loss after tibial tray removal. To improve patella tracking it is mandatory to avoid any medialization and internal rotation of the tibial tray. The medullary cavity is then prepared with reamers for the trial stem which should be 2 mm thicker than the final stem to allow for a sufficient cement mantle around the definitive implant. Preparation of the tibial plateau is completed with an impactor
The femoral medullary canal is opened with a trephine. The entry point depends on the preoperative templating and should be located on the mechanical axis in the coronal plane and on the anatomical shaft axis in the sagittal plane. Thus, the entry point is just below the anterior cortex in most cases. It is of utmost importance to adhere to this surgical guideline when using the described implant system as femoral offset stems are not available, thereby avoiding malalignment of the femoral stem and component. The stem will ultimately be placed more posteriorly and the femoral component will therefore be implanted in a flexed position, if the entry point for the intramedullary alignment rod is positioned too far posteriorly (a). The distal femoral cutting jig is assembled with 6° valgus to the reamer which has the firmest grip within the diaphyseal femoral canal (b). The height of the distal femoral resection is determined with an angel wing
Following distal femoral resection, the height of the anatomic joint line is estimated according to Servien et al. [13]: The transepicondylar width is divided by three. The result in mm indicates the location of the joint line measured from the lateral epicondyle. For reconstruction of the joint line, distal femoral augments are available (one size: 25 mm). Correct placement of the 4 in 1 block within the sagittal plane is achieved by anterior down referencing, placing an angel wing through the anterior cutting slot flush to the pre-existing femoral ventral cut—in case there is no significant damage to the anterior cortex. Alternatively, posterior up referencing can be performed using the femoral sizer and sliding its paddles under the dorsal condyles. Here it is important to account for any existing bone loss of the dorsal condyles in order to avoid any increase of the flexion gap. Correct external rotation can be determined using Whiteside’s and Insall’s line if applicable. In revision TKA and stiff knees, we aim for a slightly higher degree of external rotation compared to primary TKA to improve patella tracking. The cutting block is fixed with pins and the femoral cuts are performed. Here it is advisable to first perform the anterior cut to check for the presence of the “Grand Piano” or “Boot” sign indicating that the cut on the lateral side is deeper than on the medial side and confirming correct femoral rotational alignment [5, 10, 15]
After removal of the 4 in 1 cutting block, the femoral metaphysis has to be prepared for the uptake of the femoral box. Therefore, the last reamer with the firmest grip within the diaphyseal femoral canal is reinserted and mounted with a drilling jig followed by a two-step drilling procedure. During this step it is of utmost importance that the dorsal soft tissues are protected using a straight Hohmann retractor to lift the distal femur up thereby increasing the distance between the neurovascular structures and the cutting planes (Fig. 9)
After removal of the instruments, the femoral and tibial trial components are inserted and coupled. Range of motion and patella tracking (“rule of no thumb”) is tested. At this stage the patella can be prepared for resurfacing with a three peg polyethylene system-specific patella button. We perform patella resurfacing in a freehand technique. The patella button should be positioned as medial as possible to improve patella tracking. Then, the trial components are removed and an antiseptic lavage with polyhexanide followed by high pressure irrigation with ringer’s solution is performed. Prior to definitive implantation of the prosthesis we inflate the tourniquet and dry the bony surfaces. There should be no membranes or soft tissues left on the surfaces in order to ensure proper cement interdigitation
At this stage it is important to leave the tibial insert locking screw in place to prevent cement intrusion into the screw thread. At the same time the femoral transport secure element within the femoral box should be left in place until complete hardening of the cement (arrows). If the secure element is removed prior to hardening this will inevitably result in medial dislocation of the polyethylene (PE) inserts out of the medial and lateral condyles (a). After complete cement curing, the femoral box secure element and the tibial locking screw are removed and the rotating hinge peg is secured onto the tibial implant by locking the tibial insert with the locking screw (b). Then, the coupling mechanism is activated by removing the hinge secure screw (circle) which allows the hinge to be secured and fixed within the femoral condyles. Correct locking is indicated by positioning the holes in line with the arrows (circle) (c). Eventually, the coupled rotating hinge is secured with a locking screw (d)
Postoperative management
-
Sterile wound dressing and compressive bandaging
-
Intra-articular drain; removed 24–48 h postoperatively
-
Deep vein thrombosis prophylaxis until full weight bearing is possible
-
First 2 postoperative weeks 20 kg partial weight bearing, then 4‑point-gait with crutches for 2 weeks. Full weight bearing after 4 weeks. Weight bearing is restricted for soft tissue protection.
-
Regular postoperative clinical and radiographic follow-ups
Errors, hazards and complications
-
Fracture during intramedullary reaming: Preoperative templating is mandatory and particularly important in smaller patients to assess any femoral and tibial bowing and to determine the correct entry point into the femoral medullary canal. During reaming, it is important to notice reaming sound changes.
-
Rotational malalignment of the femoral and tibial components resulting in restricted range of motion and patella maltracking.
-
Insufficient joint line reconstruction resulting in patella alta or baja
-
Risk of damage to the popliteal artery or vein during femoral box preparation (Fig. 9).
Results
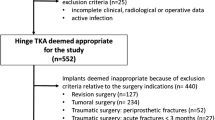
After obtaining approval by the University’s review board (approval no. 195/10), we started a prospective single-center clinical study analyzing the outcome of patients treated with TKA revision and implantation of the EndoModel Link SL after suffering from clinically significant TKA instability. Between 2012 and 2013, 25 consecutive patients were included. Three patients were lost to follow-up, 1 patient denied final follow-up examination and 2 patients died of reasons unrelated to revision surgery. Therefore, 18 patients were left for complete data acquisition with a minimum 24 month follow-up (patient demographics provided in Table 1). The mean follow-up of these patients was 37 months (range 30–46 months). One patient had to be revised due to periprosthetic infection. There were no other complications during the follow-up period. We observed a significant improvement of the Oxford Knee Score (OKS) from 19 (range 7–29) preoperatively to 29 (range 10–45) postoperatively (p = 0.004). The Knee Society Score (KSS) knee assessment subscore improved from 35 (range 9–70) to 67 (range 35–97) (p = 0.002) and the pain score from 7 (range 0–50) to 24 (range 0–50) (p = 0.008) (Table 2).
Only few studies can be found in the literature that analyzed outcomes after TKA revision with rotating hinge systems due to clinically relevant instability. Rodriguez-Merchan et al. reported results comparable to our study with an improvement of the KSS knee assessment subscore from 37 points preoperatively to 79 points at the latest follow-up. The KSS knee function subscore improved from 39 points preoperatively to 53 points at the latest follow-up, which ranged between 5 and 10 years [12].
Our study demonstrates that TKA revision with the EndoModel Link SL in patients suffering from clinically significant ligament insufficiency can lead to good clinical outcomes after a mid-term follow-up.
References
Boelch SP, Arnholdt J, Holzapfel BM et al (2018) Revision knee arthroplasty with rotating hinge systems in patients with gross ligament instability. Int Orthop. https://doi.org/10.1007/s00264-018-3982-z
Boelch SP, Jakuscheit A, Doerries S et al (2018) Periprosthetic infection is the major indication for TKA revision—experiences from a university referral arthroplasty center. BMC Musculoskelet Disord 19:395
Bozic KJ, Kurtz SM, Lau E et al (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468:45–51
Chang MJ, Lim H, Lee NR et al (2014) Diagnosis, causes and treatments of instability following total knee arthroplasty. Knee Surg Relat Res 26:61–67
Cui WQ, Won YY, Baek MH et al (2006) Variations of the ‘grand-piano sign’ during total knee replacement. A computer-simulation study. J Bone Joint Surg Br 88:1441–1447
Fehring TK, Baird R 3rd, Park B et al (2019) When polyethylene exchange is appropriate for prosthetic knee instability. J Am Acad Orthop Surg 3:e31
Guenoun B, Latargez L, Freslon M, Defossez G, Salas N, Gayet LE (2009) Complications following rotating hinge Endo-Modell (Link) knee arthroplasty. Orthop Traumatol Surg Res. 95(7):529–536. https://doi.org/10.1016/j.otsr.2009.07.013
Indelli PF, Giori N, Maloney W (2015) Level of constraint in revision knee arthroplasty. Curr Rev Musculoskelet Med 8:390–397
Laskin RS (2002) Joint line position restoration during revision total knee replacement. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-200211000-00029
Ohmori T, Kabata T, Kajino Y et al (2018) Usefulness of the “grand-piano sign” for determining femoral rotational alignment in total knee arthroplasty. Knee 25:15–24
Pereira GC, Von Kaeppler E, Alaia MJ et al (2016) Calculating the Position of the Joint Line of the Knee Using Anatomical Landmarks. Orthopedics 39:381–386
Rodriguez-Merchan EC, Gomez-Cardero P, Martinez-Lloreda A (2015) Revision knee arthroplasty with a rotating-hinge design in elderly patients with instability following total knee arthroplasty. J Clin Orthop Trauma 6:19–23
Servien E, Viskontas D, Giuffre BM et al (2008) Reliability of bony landmarks for restoration of the joint line in revision knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 16:263–269
Sheth NP, Bonadio MB, Demange MK (2017) Bone loss in revision total knee Arthroplasty: evaluation and management. J Am Acad Orthop Surg 25:348–357
Weißenberger M, Petersen N, Bölch S et al (2020) Revision of unicompartmental knee arthroplasty using the in situ referencing technique. Oper Orthop Traumatol. https://doi.org/10.1007/s00064-020-00656-w
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Arnholdt, S.P. Boelch, F. Dogan, M. Hoberg, B.M. Holzapfel and M. Rudert declare that they have no competing interests.
For this study, we received institutional review board approval (approval no. 195/10) from the university.
Additional information
Editor
D.C. Wirtz, Bonn
Illustrator
R. Himmelhan, Mannheim
Jörg Arnholdt and Sebastian P. Boelch have equally contributed as first author to this article.
Rights and permissions
About this article
Cite this article
Arnholdt, J., Boelch, S.P., Dogan, F. et al. Revision arthroplasty with rotating hinge systems for total knee arthroplasty instability. Oper Orthop Traumatol 32, 298–308 (2020). https://doi.org/10.1007/s00064-020-00663-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00064-020-00663-x