Abstract
Background
Heart failure with reduced ejection fraction is a common condition that has a poor prognosis. Accurate selection of patients with ischemic heart disease and idiopathic dilated cardiomyopathy, who are at risk of sudden cardiac death (SCD), remains a challenge. In these cases, current indications for implantable cardioverter-defibrillators (ICD) rely almost entirely on left ventricular ejection fraction. However, this parameter is insufficient. Recently, noninvasive imaging has provided insight into the mechanism underlying SCD using myocardial deformation on echocardiography and magnetic resonance imaging. The aim of this review article was to underline the emerging role of these novel parameters in identifying high-risk patients.
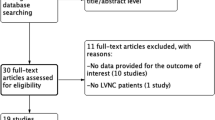
Methods
A literature search was carried out for reports published with the following terms: “sudden cardiac death,” “heart failure,” “noninvasive imaging,” “echocardiography,” “deformation,” “magnetic resonance imaging,” and “ventricular arrhythmia.” The search was restricted to reports published in English.
Results
The findings of this analysis suggest that cardiac magnetic resonance imaging and strain assessment by echocardiography, particularly longitudinal strain, can be promising techniques for cardiovascular risk stratification in patients with heart failure.
Conclusion
In future, risk stratification of arrhythmia and patient selection for ICD placement may rely on a multiparametric approach using combinations of imaging modalities in addition to left ventricular ejection fraction.
Zusammenfassung
Hintergrund
Die Herzinsuffizienz mit reduzierter Ejektionsfraktion ist eine häufige Erkrankung mit schlechter Prognose. Die genaue Auswahl von Patienten mit koronarer Herzkrankheit und idiopathischer dilatativer Kardiomyopathie, bei denen das Risiko des plötzlichen Herztods besteht, bleibt eine Herausforderung. In diesen Fällen basieren die aktuellen Indikationen für implantierbare kardiale Defibrillatoren (ICD) fast vollständig auf der linksventrikulären Ejektionsfraktion. Allerdings ist dieser Parameter unzureichend. In letzter Zeit hat die nichtinvasive Bildgebung anhand der myokardialen Deformation in der Echokardiographie und in der Magnetresonanztomographie (MRT) Einblicke in den Mechanismus eröffnet, der dem plötzlichen Herztod zugrunde liegt. Ziel der vorliegenden Übersichtsarbeit war es, die aufkommende Bedeutung dieser neuen Parameter für die Erkennung von Hochrisikopatienten hervorzuheben.
Methoden
Dazu wurde eine Literatursuche in Bezug auf Publikationen mit den folgenden Begriffen durchgeführt: „sudden cardiac death“, „heart failure“, „noninvasive imaging“, „echocardiography“, „deformation“, „magnetic resonance imaging“ und „ventricular arrhythmia“. Die Suche war begrenzt auf englischsprachig veröffentlichte Arbeiten.
Ergebnisse
Die Ergebnisse dieser Auswertung weisen darauf hin, dass die kardiale MRT und die Beurteilung des Strains mittels Echokardiographie, insbesondere des longitudinalen Strains, vielversprechende Ansätze für die kardiovaskuläre Risikostratifizierung bei Patienten mit Herzinsuffizienz sein können.
Schlussfolgerung
In Zukunft könnten die Risikostratifizierung für Arrhythmien und die Patientenauswahl für eine ICD-Implantation auf einem multiparametrischen Ansatz basieren, bei dem Kombinationen von Bildgebungsmodalitäten zusätzlich zur linksventrikulären Ejektionsfraktion verwendet werden.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Heart failure with reduced ejection fraction is a common condition associated with a poor prognosis and risk of sudden cardiac death (SCD; Fig. 1). Approximately 50% of deaths, especially in mild-to-moderate cases, are sudden.
Ischemic heart disease and idiopathic dilated cardiomyopathy (DCM) are two frequent structural heart diseases associated with heart failure and SCD. Ischemic heart disease is the anatomical substrate in 80% of SCD events. Idiopathic DCM, on the other hand, accounts for 10% of SCD cases in the adult population [1], and up to 30% of deaths in patients with DCM are sudden and likely mediated by arrhythmia [2].
In these patients, multiple randomized controlled trials (with > 6000 patients) demonstrated the superiority of implantable cardioverter-defibrillators (ICD) over antiarrhythmic agents for primary prevention of SCD [3].
The only indicator shown to have an association with increased risk of SCD in the setting of ischemic or nonischemic left ventricular (LV) dysfunction is LV ejection fraction (LVEF); [4,5,6,7]. Therefore, this parameter has been used as the major criterion for ICD implantation for primary prevention of SCD, often in combination with New York Heart Association (NYHA) class, and is still listed in recent guidelines [8].
However, only 35% of patients randomized to the ICD arm in the Multicenter Automatic Defibrillator Implantation Trial II (MADIT II) received appropriate therapy during 3 years of follow-up [9]. It was reported that LVEF had limited accuracy in identifying patients at high risk for SCD.
Recent studies have evaluated novel echocardiographic parameters of myocardial deformation and cardiac magnetic resonance (CMR) with late-gadolinium enhancement (LGE) for risk stratification of patients with ischemic and idiopathic cardiomyopathy. This noninvasive imaging facilitates the characterization of arrhythmogenic substrate explaining the mechanism of ventricular arrhythmia. Moreover, it helps in the assessment of the anatomical substrate (viable myocardium and scar tissue) and transient factors such as myocardial ischemia.
In the present review, we describe the emerging role of these novel imaging parameters in identifying high-risk patients.
Left ventricular ejection fraction as a predictor of increased risk
Although LVEF has some limitations related to reproducibility, geometric assumptions, and experience, current guidelines for SCD risk stratification emphasize the use of this parameter.
The calculation of LVEF can be improved by using contrast echocardiography or a three-dimensional (3D) approach, but the gold standard for 3D quantification of left ventricular volumes and ejection fraction is CMR [10, 11].
The Marburg Cardiomyopathy Study (MACAS), including 343 patients with nonischemic heart failure, revealed that the relative risk for major arrhythmic events was 2.28 for every 10% decrease in EF, in patients with sinus rhythm.
International guidelines consider an EF ≤ 35% as a criterion for ICD implantation in primary prevention for patients with nonischemic heart failure [12]. However, most patients who suffer SCD have a preserved LVEF, and many patients with poor LVEF do not benefit from ICD prophylaxis.
Data from the Maastricht study confirm these findings and indicate that, among patients for whom EF was measured before an episode of SCD, 52% had an EF > 30% and 32% had an EF > 40% [13].
The use of the criterion of LVEF < 35% alone has limited power in predicting SCD in patients with nonischemic heart failure. In the DEFINITE trial, the use of low LVEF alone as an indicator for ICD placement was associated with both a low event rate of SCD in the control and treatment groups and a significant number of inappropriate ICD shocks (49 inappropriate versus 91 appropriate ICD shocks) in the treatment group [14].
Recently, results from the DANISH Study [15] suggest that for many patients with DCM, ICDs do not increase longevity.
It is clear from these data that there is a need for a better assessment of arrhythmic risk using other parameters for improved characterization and selection of patients for ICD implantation [16].
Mechanisms of ventricular arrhythmia
The pathophysiology of ventricular arrhythmias is complex and involves the anatomical and functional substrate as well as transient factors altering the electrophysiology of the substrate.
In patients with structural heart disease such as ischemic cardiomyopathy (ICM) or DCM, re-entry is the most frequent mechanism of severe ventricular arrhythmia.
A central area of conduction block (functional or fixed), a unidirectional conduction block, and a zone of slow conduction are substrates for re-entry. In infarcted areas, scar tissue is the most common cause of fixed conduction block. Furthermore, the interposition of bundles of fibrous tissue within layers of viable myocytes is a model of spatial heterogeneity and creates electrical dispersion and areas of unidirectional conduction block and slow conduction.
Myocardial scar is less common in DCM, bundle branch re-entrant ventricular tachycardia and focal automaticity ventricular tachycardia have been proposed as other arrhythmogenic mechanisms in DCM.
Noninvasive imaging and risk stratification
Role of magnetic resonance imaging
Cardiac magnetic resonance imaging has developed into a powerful tool that allows for a comprehensive cardiac assessment of left ventricular structure, function, perfusion, and tissue characteristics, including the presence or absence of fibrosis [17].
Contrast-enhanced MRI is the preferred imaging modality for evaluating the extent of scar after myocardial infarction, which is known to be an independent predictor of ventricular arrhythmias [18]. Contrast-enhanced MRI can detect scar areas as small as 0.16 g. The contrast agent is trapped in the extracellular matrix, which is increased in the infarct areas, and the scar appears as hyperenhanced, white areas. The extent and characteristics of the scar area on contrast-enhanced MRI have been related to increased risk of ventricular arrhythmias and cardiac death [19]. Moreover, the myocardial scar burden on contrast-enhanced MRI was superior to LVEF for prediction of ventricular arrhythmias [20].
In the study by Klem et al., including 137 patients considered for ICD placement, myocardial scar detected by cardiac MRI was an independent predictor of death or appropriate ICD discharge for sustained ventricular tachyarrhythmia. This study included a wider range of LVEF and showed that in patients with LVEF > 30%, significant scarring (≥5% LV) identifies a high-risk group similar in risk to those with LVEF ≤ 30%; by contrast, those with EF ≤ 30% and minimal scar (<5%) had similar risk to those with EF > 30% [19].
Contrast-enhanced MRI, using different signal intensity thresholds, can differentiate and quantify the core infarct zone and the peri-infarct or border zone (bundles of viable myocardium intermingling with fibrous tissue; [22]).
The infarcted myocardium can be divided into the following zones: core infarct zone; gray or peri-infarct zone; and total infarct = core + peri-infarct zones. The core and peri-infarct areas have been defined as areas with LGE signal intensity (SI) ≥ 3 SD, and 2 SD ≤ SI < 3 SD, respectively [23, 24].
In the Roes et al. study, the extent of the peri-infarct zone was the only independent predictor of appropriate ICD therapy or cardiac mortality [19].
A recent meta-analysis [25] was performed to identify the predictive accuracy of LGE-CMR for SCD risk stratification. The extent of LGE on CMR was strongly associated with the occurrence of ventricular arrhythmias in patients with reduced LVEF (relative risk estimated at 4.33 for all, 4.63 for ICM and 3.79 for nonischemic cardiomyopathy). Core scar and the gray zone are predictors of ventricular arrhythmia events with a relative risk of 3.82 (2.19–6.66) and 5.94 (2.82–12.52), respectively.
In DCM, contrast-enhanced MRI has provided important information on the relationship between myocardial scar burden, scar location, and the risk of ventricular arrhythmias [26,27,28]. Scar tissue usually involves the midwall (Fig. 2) or shows a patchy distribution.
Nazarian et al. [29] demonstrated that the distribution of myocardial scar assessed with contrast-enhanced MRI was predictive of inducible sustained monomorphic ventricular tachycardia in 26 patients with DCM. In this study and after adjustment for LVEF, the presence of fibrosis covering 26–75% of the wall thickness was associated with a ninefold increase in the risk of ventricular arrhythmia according to an electrophysiological study.
In the study by Wu et al. [30], SCD or appropriate ICD discharge were detected in 22% of patients with CMR evidence of myocardial scar versus only 8% of patients without evidence of gadolinium enhancement (p = 0.03). In these patients, fibrosis of the midwall detected by LGE-CMR was associated with adverse cardiac events (hospitalization for heart failure, appropriate ICD firing, and cardiac death; [30, 31]).
Neilan et al. [32] determined the prognostic value of LGE in 162 patients with nonischemic cardiomyopathy, and found that cardiovascular death and appropriate ICD therapy were substantially higher in patients with LGE (24%) than in those without LGE (2%).
The presence and the extent of LGE have the strongest associations with cardiovascular death and appropriate ICD therapy: LGE presence, hazard ratio (HR): 14.5; p < 0.001; LGE extent, HR: 1.15 per 1% increase in volume of LGE; p < 0.0001.
However, in multivariate analyses, LGE extent was the strongest predictor of cardiovascular death and appropriate ICD therapy (a sevenfold hazard per 10% LGE extent after adjusting for patient age, sex, and LVEF; adjusted HR: 7.61; p < 0.0001).
Given the multiple small and single-center studies reporting on the prognostic data of LGE in patients with DCM, a systematic review and meta-analysis was performed. The meta-analysis [33] collected data from nine studies with a total of 1488 patients and a mean follow-up of 30 months. It was found that LGE was present in 38% of patients. Those with LGE had increased overall mortality (odds ratio, 3.27; p < 0.00001) and SCD/aborted SCD (odds ratio, 5.32; p < 0.00001) compared with those without LGE.
The largest study on this topic was recently published by Gulati et al. [34], including 472 patients with nonischemic heart failure examined with MRI and with a median follow-up of 5.3 years. Combined events of SCD and aborted SCD were observed in 29.6% patients with myocardial fibrosis and 7.0% patients without fibrosis. For this event, the presence of fibrosis represented an HR of 4.61 (95% CI, 2.75–7.74; p < 0.001).
Another recent study [21] enrolling patients with ischemic cardiomyopathy or nonischemic cardiomyopathy found that the presence of both LGE and LVEF < 30% increased the event rate of SCD or ICD discharge compared with event rates in patients with LVEF < 30% alone.
This additive prognostic value of LGE was also demonstrated in the large study by Gulati et al. [34]. After multivariate analysis with adjustment for EF and other prognostic factors, the presence of fibrosis represented an HR of 2.43 (95% CI, 1.50–3.92; p < 0.001), and the extent of fibrosis represented an HR of 1.11 (95% CI, 1.06–1.16; p < 0.001).
Disertori et al. analyzed data from 19 studies of SCD primary prevention, which included 2850 patients with 423 arrhythmic events over an average follow-up of 2.8 years. The patients had either ischemic cardiomyopathy (31%) or nonischemic cardiomyopathy and ventricular dysfunction; the composite arrhythmic outcomes included SCD, aborted SCD, ventricular tachycardia/fibrillation, and ICD therapy. Patients with negative LGE test results had a composite annualized event rate of 1.7% versus 8.6% for those positive LGE test results (p < 0.0001). In both the etiology-based and EF-based subgroups, LGE correlated with arrhythmic events. In the overall population, the pooled odds ratio was 5.62 (95% CI: 4.20–7.51; [35]).
The second recent meta-analysis, performed by Di Marco et al., included 29 studies (2948 patients). It was found that LGE was significantly associated with the arrhythmic endpoint both in the overall population (odds ratio: 4.3; p < 0.001) and when including only those studies that performed multivariate analysis (hazard ratio: 6.7; p < 0.001; [36]).
Magnetic resonance imaging can also be helpful for patients with DCM and mild or moderate reductions in LVEF (>35–40%), in which midwall LGE identifies a group of patients at increased risk of SCD. This finding is important because these patients are not currently offered ICDs for the primary prevention of SCD on the basis of guideline recommendations [36, 37].
The main studies evaluating the association between myocardial fibrosis assessed via CMR and the risk of arrhythmic and nonarrhythmic events are summarized in Table 1.
Current studies examining LGE by CMR in patients with DCM use varying definitions to define the presence and extent of LGE [42]. Different thresholds of signal intensity have been proposed to determine the presence of LGE, but there is a lack of consensus on an acceptable threshold for the diagnosis of LGE. This is more challenging in DCM where the intensity of the LGE is much more variable than in ischemic heart disease.
Assomull et al. [26] found that these patients with DCM and with LGE of ≥ 4.8% of LV mass were at higher risk of cardiovascular events than those with LGE < 4.8%.
In the study by Neilan’ et al. [32], patients with LGE involving > 6.1% of LV myocardium had the highest cardiovascular death and appropriate ICD therapy.
Different methods are also used to determine LGE extent as a percentage of LV mass or scar volume. Although current guidelines recommend using the 2‑SD method, data suggest that the use of this technique leads to an overestimation of the extent of LGE in comparison with other techniques [23]. There is so a need for homogeneity in the definition of both the presence and extent of LGE so as to improve reproducibility and standardize the technique.
The LGE border zone on CMR imaging has also been proposed as an independent predictor of ventricular arrhythmias, and a recent meta-analysis [43] found that the quantification of the LGE border zone is the strongest predictor of appropriate ICD therapy, as a surrogate for SCD, in ICM patients with primary prophylactic ICD at medium- to long-term follow-up.
Role of myocardial deformation on echocardiography
Speckle-tracking imaging is a relatively new approach for assessing myocardial deformation by detecting features on grayscale 2D images.
The assessment of LV global longitudinal strain with 2D speckle-tracking echocardiography has been shown to be an accurate marker of LV function. This technique is feasible and reproducible without geometric assumptions, and is independent of LV geometry.
Since global longitudinal strain measures pure longitudinal function, and it may provide other information than EF, which is strongly influenced by the radial motion of the myocardium [44]. Global longitudinal strain has been reported to provide superior prognostic information in the setting of ischemic heart disease [44, 45].
The Bertini et al. study was a larger one including a homogeneous population with chronic ischemic heart disease (1060 patients). In this study, global longitudinal strain was independently related to all-cause mortality (HR per 5% increase, 1.69; 95% CI, 1.33–2.15; p < 0.001) and combined end point (all-cause mortality and heart failure hospitalization; 1.64; 95% CI, 1.32–2.04; p < 0.001) and patients with an LV global longitudinal strain value of ≤ −11.5% had better outcome than those with LV global longitudinal strain > −11.5% [46].
Iacoviello et al. [47] studied a group of heart failure patients affected by ischemic or nonischemic DCM without a history of sustained ventricular arrhythmias. During a follow-up of 26 ± 13 months, 31 of 230 patients experienced ventricular tachycardia/fibrillation or SCD.
At multivariate analysis, global longitudinal strain remained significantly associated with ventricular arrhythmic events. The best global longitudinal strain cut-off value for the 1‑year occurrence of major ventricular arrhythmias was −10.0% (73% sensitivity and 61% specificity).
Longitudinal strain also adds incremental prognostic value to EF alone for the prediction of adverse outcomes in both ischemic and nonischemic cardiomyopathy [48]. This finding was also noted in a multicenter study that included 147 patients with heart failure with an LVEF ≤ 45% (ischemic in 42.8%).
Among prognostic factors obtained by echocardiography, global longitudinal strain was the best predictor of cardiac events, and a cut-off value of −7% predicted cardiac events at 12 months with high sensitivity and specificity [49].
In the study of Motoki et al. [50], which included 194 patients with chronic systolic heart failure, global longitudinal strain was an independent prognostic factor for cardiac events in heart failure regardless of age, LVEF, ischemic etiology and E/e’, and it had greater prognostic power than LVEF.
In ischemic cardiomyopathy, the functional properties of the peri-infarct zone have been evaluated with 2D speckle-tracking echocardiography (Fig. 3).
Usually, the infarct zone had the most impaired longitudinal strain, whereas the peri-infarct zones had more preserved longitudinal strain.
In 424 patients with ischemic cardiomyopathy considered for ICD implantation, the presence of impaired segmental longitudinal strain in the peri-infarct zone was independently associated with an increased risk of appropriate ICD therapy for ventricular tachycardia and fibrillation [51].
The relationship between the longitudinal peak systolic strain of the peri-infarct zone detected with speckle-tracking echocardiography and monomorphic ventricular tachycardia inducibility in patients with chronic ischemic cardiomyopathy was explored. Only longitudinal peak systolic strain of the peri-infarct zone was independently related to monomorphic ventricular tachycardia inducibility [52].
Mechanical dispersion, another strain parameter that reflects contraction heterogeneity, was recently used in a prospective, multicenter study of patients after myocardial infarction. This parameter predicted arrhythmic events independently of LVEF. A combination of mechanical dispersion and global longitudinal strain may improve the selection of patients after myocardial infarction for ICD therapy, particularly when LVEF is > 35% [53].
Conclusion
-
This review detailed the emerging role of the novel imaging parameters in identifying high risk patients with ischemic or nonischemic dilated cardiomyopathy.
-
Cardiac magnetic resonance imaging can be a useful technique for the risk stratification of these patients but there is a need for a homogeneous definition for both the presence and extent of late-gadolinium enhancement to improve reproducibility and to standardize the technique.
-
Strain assessment by echocardiography, particularly longitudinal strain, can also be used for cardiovascular risk stratification in patients with heart failure with greater accuracy than left ventricular ejection fraction (LVEF), but the cut-off values must be better defined.
-
Future risk stratification for arrhythmia and patient selection for implantable cardioverter-defibrillator placement may rely on a multiparametric approach using combinations of imaging modalities that may complement primary reliance on LVEF.
References
Zipes DP, Wellens HJ (1998) Sudden cardiac death. Circulation 98(21):2334–2351
Tamburro P, Wilber D (1992) Sudden death in idiopathic dilated cardiomyopathy. Am Heart J 124(4):1035–1045
Ezekowitz JA, Armstrong PW, McAlister FA (2003) Implantable cardioverter defibrillators in primary and secondary prevention: a systematic review of randomized, controlled trials. Ann Intern Med 138(6):445–452
Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R et al (2005) Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 352(3):225–237
Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS et al (2002) Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 346(12):877–883
Bauer A, Barthel P, Schneider R, Ulm K, Müller A, Joeinig A et al (2009) Improved Stratification of Autonomic Regulation for risk prediction in post-infarction patients with preserved left ventricular function (ISAR-Risk). Eur Heart J 30(5):576–583
Exner DV, Kavanagh KM, Slawnych MP, Mitchell LB, Ramadan D, Aggarwal SG et al (2007) Noninvasive risk assessment early after a myocardial infarction the REFINE study. J Am Coll Cardiol 50(24):2275–2284
Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M et al (2015) 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: the Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Europace 17(11):1601–1687
Moss AJ, Greenberg H, Case RB, Zareba W, Hall WJ, Brown MW et al (2004) Long-term clinical course of patients after termination of ventricular tachyarrhythmia by an implanted defibrillator. Circulation 110(25):3760–3765
Pennell DJ (2010) Cardiovascular magnetic resonance. Circulation 121(5):692–705
Iacoviello M, Monitillo F (2014) Non-invasive evaluation of arrhythmic risk in dilated cardiomyopathy: from imaging to electrocardiographic measures. World J Cardiol 6(7):562–576
Russo AM, Stainback RF, Bailey SR, Epstein AE, Heidenreich PA, Jessup M et al (2013) ACCF/HRS/AHA/ASE/HFSA/SCAI/SCCT/SCMR 2013 appropriate use criteria for implantable cardioverter-defibrillators and cardiac resynchronization therapy: a report of the American College of Cardiology Foundation appropriate use criteria task force, Heart Rhythm Society, American Heart Association, American Society of Echocardiography, Heart Failure Society of America, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. Heart Rhythm 10(4):e11–e58
Gorgels APM, Gijsbers C, de Vreede-Swagemakers J, Lousberg A, Wellens HJJ (2003) Out-of-hospital cardiac arrest--the relevance of heart failure. The Maastricht Circulatory Arrest Registry. Eur Heart J 24(13):1204–1209
Kadish A, Dyer A, Daubert JP, Quigg R, Estes NAM, Anderson KP et al (2004) Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med 350(21):2151–2158
Køber L, Thune JJ, Nielsen JC, Haarbo J, Videbæk L, Korup E, Jensen G, Hildebrandt P, Steffensen FH, Bruun NE, Eiskjær H, Brandes A, Thøgersen AM, Gustafsson F, Egstrup K, Videbæk R, Hassager C, Svendsen JH, Høfsten DE, Torp-Pedersen C, Pehrson S, DANISH Investigators (2016) Defibrillator Implantation in patients with nonischemic systolic heart failure. N Engl J Med 375:1221–1230
Halliday BP, Cleland JGF, Goldberger JJ, Prasad SK (2017) Personalizing risk stratification for sudden death in dilated cardiac the past, present, and future. Circulation 136:215–231
Gonzalez JA, Kramer CM (2015) Role of imaging techniques for diagnosis, prognosis and management of heart failure patients: cardiac magnetic resonance. Curr Heart Fail Rep 12(4):276–283
Cheong BYC, Muthupillai R, Wilson JM, Sung A, Huber S, Amin S et al (2009) Prognostic significance of delayed-enhancement magnetic resonance imaging: survival of 857 patients with and without left ventricular dysfunction. Circulation 120(21):2069–2076
Roes SD, Borleffs CJW, van der Geest RJ, Westenberg JJM, Marsan NA, Kaandorp TAM et al (2009) Infarct tissue heterogeneity assessed with contrast-enhanced MRI predicts spontaneous ventricular arrhythmia in patients with ischemic cardiomyopathy and implantable cardioverter-defibrillator. Circ Cardiovasc Imaging 2(3):183–190
Bello D, Fieno DS, Kim RJ, Pereles FS, Passman R, Song G et al (2005) Infarct morphology identifies patients with substrate for sustained ventricular tachycardia. J Am Coll Cardiol 45(7):1104–1108
Klem I, Weinsaft JW, Bahnson TD, Hegland D, Kim HW, Hayes B et al (2012) Assessment of myocardial scarring improves risk stratification in patients evaluated for cardiac defibrillator implantation. J Am Coll Cardiol 60(5):408–420
Yan AT, Shayne AJ, Brown KA, Gupta SN, Chan CW, Luu TM et al (2006) Characterization of the peri-infarct zone by contrast-enhanced cardiac magnetic resonance imaging is a powerful predictor of post-myocardial infarction mortality. Circulation 114(1):32–39
Flett AS, Hasleton J, Cook C, Hausenloy D, Quarta G, Ariti C et al (2011) Evaluation of techniques for the quantification of myocardial scar of differing etiology using cardiac magnetic resonance. JACC Cardiovasc Imaging 4(2):150–156
Gao P, Yee R, Gula L, Krahn AD, Skanes A, Leong-Sit P et al (2012) Prediction of arrhythmic events in ischemic and dilated cardiomyopathy patients referred for implantable cardiac defibrillator: evaluation of multiple scar quantification measures for late gadolinium enhancement magnetic resonance imaging. Circ Cardiovasc Imaging 5(4):448–456
Scott PA, Rosengarten JA, Curzen NP, Morgan JM (2013) Late gadolinium enhancement cardiac magnetic resonance imaging for the prediction of ventricular tachyarrhythmic events: a meta-analysis. Eur J Heart Fail 15(9):1019–1027
Assomull RG, Prasad SK, Lyne J, Smith G, Burman ED, Khan M et al (2006) Cardiovascular magnetic resonance, fibrosis, and prognosis in dilated cardiomyopathy. J Am Coll Cardiol 48(10):1977–1985
Bogun FM, Desjardins B, Good E, Gupta S, Crawford T, Oral H et al (2009) Delayed-enhanced magnetic resonance imaging in nonischemic cardiomyopathy: utility for identifying the ventricular arrhythmia substrate. J Am Coll Cardiol 53(13):1138–1145
Pimentel M, Zimerman LI, Rohde LE (2014) Stratification of the risk of sudden death in nonischemic heart failure. Arq Bras Cardiol 103(4):348–357
Nazarian S, Bluemke DA, Lardo AC, Zviman MM, Watkins SP, Dickfeld TL et al (2005) Magnetic resonance assessment of the substrate for inducible ventricular tachycardia in nonischemic cardiomyopathy. Circulation 112(18):2821–2825
Wu KC, Weiss RG, Thiemann DR, Kitagawa K, Schmidt A, Dalal D et al (2008) Late gadolinium enhancement by cardiovascular magnetic resonance heralds an adverse prognosis in nonischemic cardiomyopathy. J Am Coll Cardiol 51(25):2414–2421
Suzuki T, Nazarian S, Jerosch-Herold M, Chugh SS (2016) Imaging for assessment of sudden death risk: current role and future prospects. Europace 18:1491–1500
Neilan TG, Coelho-Filho OR, Danik SB, Shah RV, Dodson JA, Verdini DJ et al (2013) CMR quantification of myocardial scar provides additive prognostic information in nonischemic cardiomyopathy. JACC Cardiovasc Imaging 6(9):944–954
Kuruvilla S, Adenaw N, Katwal AB, Lipinski MJ, Kramer CM, Salerno M (2014) Late gadolinium enhancement on cardiac magnetic resonance predicts adverse cardiovascular outcomes in nonischemic cardiomyopathy: a systematic review and meta-analysis. Circ Cardiovasc Imaging 7(2):250–258
Gulati A, Jabbour A, Ismail TF, Guha K, Khwaja J, Raza S et al (2013) Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA 309(9):896–908
Disertori M, Rigoni M, Pace N, Casolo G, Masè M, Gonzini L, Lucci D (2016) Myocardial fibrosis assessment by LGE is a powerful predictorOf ventricular tachyarrhythmias in ischemic and nonischemic LV dysfunction: a meta-analysis. JACC Cardiovasc Imaging 9:1046–1055
Di Marco A, Anguera I, Schmitt M, Klem I, Neilan T, White JA (2017) Sramko Late gadolinium enhancement and the risk for ventricular arrhythmias or sudden death in dilated cardiomyopathy: systematic review and meta-analysis. JACC Heart Fail 5:28–38
Halliday BP (2017) Association Between Midwall Late Gadolinium Enhancement and Sudden Cardiac Death in Patients With Dilated Cardiomyopathy and Mild and Moderate Left Ventricular Systolic Dysfunction. Circulation 135:2106–2115
Iles L, Pfluger H, Lefkovits L, Butler MJ, Kistler PM, Kaye DM et al (2011) Myocardial fibrosis predicts appropriate device therapy in patients with implantable cardioverter-defibrillators for primary prevention of sudden cardiac death. J Am Coll Cardiol 57(7):821–828
Lehrke S, Lossnitzer D, Schöb M, Steen H, Merten C, Kemmling H et al (2011) Use of cardiovascular magnetic resonance for risk stratification in chronic heart failure: prognostic value of late gadolinium enhancement in patients with non-ischaemic dilated cardiomyopathy. Heart Br Card Soc 97(9):727–732
Li X, Chan C‑P, Hua W, Ding L, Wang J, Zhang S et al (2013) Prognostic impact of late gadolinium enhancement by cardiac magnetic resonance imaging in patients with non-ischaemic dilated cardiomyopathy. Int J Cardiol 168(5):4979–4980
Müller KAL, Müller I, Kramer U, Kandolf R, Gawaz M, Bauer A et al (2013) Prognostic value of contrast-enhanced cardiac magnetic resonance imaging in patients with newly diagnosed non-ischemic cardiomyopathy: cohort study. Plos One 8(2):e57077
Nahum J, Bensaid A, Dussault C, Macron L, Clémence D, Bouhemad B et al (2010) Impact of longitudinal myocardial deformation on the prognosis of chronic heart failure patients. Circ Cardiovasc Imaging 3(3):249–256
Jablonowski R (2017) Cardiovascular magnetic resonance to predict appropriate implantable cardioverter defibrillator therapy in Ischemicand nonischemic cardiomyopathy patients using late gadolinium enhancement border zone comparison of four analysis method. Circ Cardiovasc Imaging 10:e6105
Kalam K, Otahal P, Marwick TH (2014) Prognostic implications of global LV dysfunction: a systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart Br Card Soc 100(21):1673–1680
Antoni ML, Mollema SA, Delgado V, Atary JZ, Borleffs CJW, Boersma E et al (2010) Prognostic importance of strain and strain rate after acute myocardial infarction. Eur Heart J 31(13):1640–1647
Bertini M, Ng ACT, Antoni ML, Nucifora G, Ewe SH, Auger D et al (2012) Global longitudinal strain predicts long-term survival in patients with chronic ischemic cardiomyopathy. Circ Cardiovasc Imaging 5(3):383–391
Iacoviello M, Puzzovivo A, Guida P, Forleo C, Monitillo F, Catanzaro R et al (2013) Independent role of left ventricular global longitudinal strain in predicting prognosis of chronic heart failure patients. Echocardiography 30(7):803–811
Zhang KW, French B, Khan MA, Plappert T, Fang JC, Sweitzer NK et al (2014) Strain improves risk prediction beyond ejection fraction in chronic systolic heart failure. J Am Heart Assoc 3(1):e550
Mignot A, Donal E, Zaroui A, Reant P, Salem A, Hamon C et al (2010) Global longitudinal strain as a major predictor of cardiac events in patients with depressed left ventricular function: a multicenter study. J Am Soc Echocardiogr 23(10):1019–1024
Motoki H, Borowski AG, Shrestha K, Troughton RW, Tang WHW, Thomas JD et al (2012) Incremental prognostic value of assessing left ventricular myocardial mechanics in patients with chronic systolic heart failure. J Am Coll Cardiol 60(20):2074–2081
Ng ACT, Bertini M, Borleffs CJW, Delgado V, Boersma E, Piers SRD et al (2010) Predictors of death and occurrence of appropriate implantable defibrillator therapies in patients with ischemic cardiomyopathy. Am J Cardiol 106(11):1566–1573
Bertini M, Ng ACT, Borleffs CJW, Delgado V, Wijnmaalen AP, Nucifora G et al (2010) Longitudinal mechanics of the periinfarct zone and ventricular tachycardia inducibility in patients with chronic ischemic cardiomyopathy. Am Heart J 160(4):729–736
Haugaa KH, Grenne BL, Eek CH, Ersbøll M, Valeur N, Svendsen JH et al (2013) Strain echocardiography improves risk prediction of ventricular arrhythmias after myocardial infarction. JACC Cardiovasc Imaging 6(8):841–850
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I. Kammoun, E. Bennour, L. Laroussi, M. Miled, A. Sghaier, K. Rahma, B. Amine, S. Marrakchi and S. Kachboura declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Kammoun, I., Bennour, E., Laroussi, L. et al. Risk stratification for sudden cardiac death in patients with heart failure. Herz 46, 550–557 (2021). https://doi.org/10.1007/s00059-021-05032-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-021-05032-3
Keywords
- Cardiac failure
- Sudden cardiac arrest
- Echocardiography
- Myocardial deformation
- Magnetic resonance imaging