Abstract
We report the synthesis of phosphoramidate conjugates of 3′-azido-3′-deoxythymidine (AZT) glycerolipid derivatives and amino acid esters. For the synthesized compounds, 50% inhibition of the HIV-1 MvP-899 strain in human T lymphoid MT-4 cells is achieved at concentrations of 0.014–0.356 µM. Significantly, compound 3c (which contained ethyl ester of α-alanine) was found to be the most active with EC50 value 0.014 µM. We show that, among these glycerolipid derivatives of AZT, some compounds are less toxic than AZT, and also they possess a similar or higher selectivity index compared to AZT (SI = 11643).

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the data of the Joint United Nations Program on HIV/AIDS, the number of HIV-infected people in the world was 37.9 million at the beginning of 2019, and this number continues to grow [1]. AIDS is among the major causes of death, and the disease has a significant social and economic impact. Currently, the highly active antiretroviral therapy (HAART) remains an efficient method that employs classic drugs based on nucleoside reverse transcriptase inhibitors (NRTIs)—zidovudine, stavudine, abacavir. These drugs are very effective at suppressing HIV replication and stopping the disease progression. However, many drugs that are included in the HAART are highly toxic (CC50 (CEM cell line) >80 µM) and have a low bioavailability (64%–75%, >80%, 83%, respectively) [2,3,4,5]. Since 1999, the domestic drug phosphazide (NicavirTM) is used in Russia for HIV treatment. Since that time, the drug proved to be a potent and well-tolerated antiviral therapy [6]. A lifelong intake of these medications leads to a continuous intoxication of the patient and causes the evolution of drug-resistant viral strains. Eventually, the effectivity of the anti-HIV therapy decreases.
Currently, prodrugs are becoming more and more popular, as they play a significant role in the development of treatment strategy for complex diseases and can help overcome the drug resistance issues. The prodrugs are derived from existing medications through modification with biomolecule fragments. This approach is used for the modification of antiviral and antitumor nucleoside drugs in order to combat the drawbacks of these drugs [7,8,9]. Development of prodrugs from NRTIs has a pharmacological potential, as the new prodrugs could be designed to cross biological barriers and reach the target cells, thus exhibiting high selectivity and efficacy compared to the original drugs [10,11,12]. A promising tool for prodrug synthesis is the pseudotriglyceride approach, which can be used to design a nucleoside (connected with a derivative of 1,3-diacylglycerol) that could participate in lipid metabolism and reach the lymphatic system (HIV reservoir), thus getting absorbed together with lipids in the small intestine—avoiding primary degradation in the liver [13].
Here, we describe the synthesis and anti-HIV activity of conjugates of 3′-azido-3′-deoxythymidine (AZT) glycerolipid derivatives and amino acid esters. Our results make it possible to establish the relationship between the structure of the synthesized compounds and their inhibiting activity, with obtained date could be used to design lipophilic prodrugs with improved properties and higher efficacy.
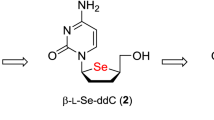
In our earlier work, we synthesized glycerolipid derivatives of AZT where the fragments of the molecules were connected via a functional phosphorous linkages [14]. Some of these molecules (Fig. 1) exhibited a high antiviral activity toward HIV-1 in vitro, but they are not stable enough in buffers that imitated biological media through which the drug delivery to target cells takes place.
In the present work, we describe the synthesis of phosphoramidate derivatives of glycerolipid conjugates of AZT with amino acid esters. This modification is thought to improve the stability of AZT conjugates to hydrolysis in various biological media and modulate the inhibitory activity of such compounds. The anti-HIV activity of the obtained substances was analyzed in an in vitro HIV model.
A possible advantage of such liponucleoside prodrugs is a higher activity in natural conditions, low toxicity, better delivery into the macrophages and other cells of the immune system, improved pharmacokinetics and long intracellular persistence. Also, these conjugates help release the nucleoside monophosphate during metabolism. The first step in the activation pathway consists of carboxylesterases hydrolyze the ether group in the amino acid part. The carboxyl ester group linked to the amino acid moiety has pronounced influence on the pharmacokinetics and stability of the phosphoramidate conjugate. Cleavage under the action of carboxyesterases is followed by a nucleophilic attack of the phosphorus by a carboxyl group to form a five-membered cyclic intermediate. The nature of the side chain of the amino acid and the nature of the sugar moiety do play an essential role in the formation of the amino acyl metabolite through the cyclic intermediate. This is followed by the conversion of the amino acyl metabolite to free AZT monophosphate (Fig. 2) [15].
This mechanism of drug release may allow to reduce the phosphorylation step in macrophages/monocytes—a significant HIV reservoir—where the thymidine kinase is less active [16]. Accumulation of the conjugates in the cells and subsequent hydrolysis by cellular enzymes (e.g., phosphatases) will result in a slower release of AZT monophosphate and lower the risk of developing drug resistance. It will also allow the patient to take the drug less frequently due to its prolonged action. As the conjugates are being degraded, diacylglycerols may be released, inhibiting the protein kinase C, thus lowering the endocytosis of CD4-HIV and the following viral infection of T cells [17]. PKC is involved in micropinocytosis and phagocytosis [18,19,20]. In cells where HIV-1 replicates efficiently, PKC must be activated. Various PKC isozymes, which are activated by interactions between CXCR4/CCR5 and HIV-1, play a major role in the rearrangement of the actin cytoskeleton, which is required for viral penetration [21, 22]. To this end, viral penetration could be partially inhibited because of the effect of glycerol derivatives on the protein kinase C.
Results and discussion
It was shown before that many phosphoramidate derivatives of AZT were active against viruses [23]. In this work, we report the synthesis of phosphoramidate conjugates of AZT and 1,3-diacylglycerol derivatives, modified with various amino acid esters. The design of such compounds facilitates their targeting at the enterocyte-mediated lymphatic transport and helps modulate different physico-chemical properties and the inhibitory activity of the molecules.
Glycerolipid H-phosphonates of AZT (1, 2) and their conjugates with methyl ether of α-alanine (α-Ala) (3а and 3b) were synthesized in our laboratory earlier [14]. The synthesis of the phosphoramidate conjugates 3с–g was carried out in the same manner: by interaction between H-phosphonates (1 or 2) with hydrochlorides of α-Ala or β-alanine (β-Ala) esters, at 0 °C in triethylamine–tetrachloromethane–water–acetonitrile (1:1:1:10 by volume) (Scheme 1).
The products were purified by column chromatography on silica gel, and yield was more than 70%. The structures were determined by nuclear magnetic resonance (NMR) spectroscopy: 1Н NMR and 31Р NMR. 31Р NMR spectra showed two characteristic peaks that indicated the formation of diastereomers with stereocenters at the phosphorus (PS and PR). The data of element analysis satisfactorily correlated with the structures of the synthesized compounds.
Next, compounds 3с–g were subjected to hydrolysis, because it is necessary to take into account chemical and enzymatic hydrolysis, which takes place during prodrug absorption and distribution, especially upon oral administration. For effective delivery, the pronucleotide derivatives should be resistant to these hydrolytic processes, but at the same time they should be sensitive to specific hydrolysis by the pancreatic lipase—for targeting the enterocyte-mediated lymphatic transport. We investigated with Thin-layer chromatography (TLC) monitoring the hydrolysis kinetics of compounds 3с–g in buffers that imitated physiological pH values of the intestine, blood, and lymphatic system. Our results showed that the hydrolysis half-time for these molecules exceeded 20 h.
Furthermore, we investigated the kinetics of enzymatic hydrolysis of these prodrugs by the porcine pancreatic lipase in vitro. To this end, they were incubated with the 375 U/mL enzyme at 37 °С in the PIPES buffer (pH 6.5) in the presence of sodium taurodeoxycholate. The kinetics were monitored by TLC. At the beginning of the reaction, we observed the formation of presumably 2-pseudomonoglycerides, products of the specific lipase activity. After 1 h, we did not detect significant degradation of these molecules. Even after 2 h, AZT was not released. Our data showed that the conjugates were highly sensitive to the pancreatic lipase; the hydrolysis half-time was 30 s, which can mimic the metabolic pathways of natural glycerolipid compounds.
At the next step of our study, we analyzed the cytotoxicity and anti-HIV efficacy of compounds 3a–g. We also investigated the relationship between the antiviral activity and the structure. AZT was used as a reference compound.
Compounds 3b–g exhibited low toxicity when applied to the МТ-4 cell line. The low CC50 for compound 3а (compared to the other conjugates) may be due to the methoxy group in the ester fragment. During metabolism, the methoxy group is transformed into methanol, which is toxic to the cells. AZT was rather toxic in our experiment (СС50 = 85 µM). Our data showed that modifications in certain conjugates 3b–g made them considerably less toxic compared to AZT: the СС50 ranged from 142 to 212 µM.
We analyzed the antiviral activity of compounds 3a–g in MT-4 cells infected with HIV-1. The antiviral activity was determined by two factors, amino acid residue and ester group, but did not depend on the length of the fatty acid of the lipophilic vector (R). Modifications with α-Ala were preferable over those with β-Ala. All compounds based on α-Ala were active. The EC50, obtained with our HIV model МТ-4/HIV-1 MvP-899 ranged from 0.014 to 0.053 µM (Table 1).
The microscopic analysis of the infected cells in the presence of the conjugates based on β-Ala, 3f (EC50 = 0.356 µM) and 3g (EC50 = 0.203 µM), showed the development of lytic infection leading to giant multinucleated cells: coenocytes and syncytia. This indicates that these substances did not inhibit the HIV. Our results showed that modifications with β-Ala did not produce active metabolites, in agreement with the previously published data [15].
At the first step of glycerolipid conjugates’ metabolism, carboxylesterases hydrolyze the ester group. Ether hydrolysis occurs in α- and β-amino acids with equal efficiency, but β-amino acids are biologically inactive. Moreover, the ethyl ester group linked to the amino acid moiety provides higher stability than the methyl group. The safety of the alcohol released by carboxylesterase is also important, with the ethyl derivative may seemed preferable over the methyl derivative. The antiviral activity of compounds with α-Ala, which contained various ester modifications as R′, decreased insignificantly in the row Et–Me–iPr–tBu. Compound 3c, which contained ethyl ester of α-Ala, was found to be the most active (ЕС50 = 0.014 µM). The conjugate 3e that contained tert-butyl ester of α-Ala had a lower activity (ЕС50 = 0.053 µM). This effect correlated with the high stability of the tert-butyl ester to the esterase.
In conclusion, our study on the bioactivity of AZT glycerolipid derivatives demonstrates that some of these molecules have advantages over AZT. In particular, they are less toxic and have a comparable or better selectivity index. The compounds described in this paper have the potential to be included in the conventional antiretroviral therapy.
Experimental
NMR spectra were recorded on a pulse Fourier transform NMR spectrometer Bruker DPX_300 (Germany). 1H NMR spectra (δ, ppm) were taken in deuterated solvents at operating frequency of 300 MHz with tetramethylsilane as an internal standard. 31P NMR spectra were taken in deuterated solvents at operating frequency 121.5 MHz with broad-band heteronuclear 31P-{1H} decoupling. Chemical shifts are given relative to 85% orthophosphoric acid (an external standard). Melting points were measured on a Boetius table (Germany). Element analysis was performed on an automated FLASH 1112 CHNS Analyzer (Italy). The following chemicals were used in this work: chloroform, dichloromethane, methanol, triethylamine, carbon tetrachloride, acetonitrile. Dichloromethane and acetonitrile were distilled over phosphorus pentoxide. Triethylamine was distilled over potassium hydroxide. Chloroform was distilled over calcium chloride. We used the following esters of amino acids: methyl ester of β-Ala; ethyl, isopropyl, tert-butyl esters of α-L-Ala (Aldrich, USA). The other substances used in this work were sodium taurodeoxycholate; 1,4-piperazinediethanesulfonic acid (PIPES) (Aldrich, Germany); porcine pancreatic lipase (EC 3.1.1.3), 30.1 U/mg (Fluka, USA).
TLC was performed on Sorbfil plates (Sorbpolimer, Russia) in the following solvent systems:
Chloroform:methanol (9.7:0.3, v/v) (a)
Chloroform:methanol (8.5:1.5, v/v) (b)
The spots on chromatograms visualized in UV light and by treatment with ammonium molybdate in 30% H2SO4 followed by heating at 150 °С. Column chromatography was performed on silica gel (0.040–0.063 mm) (Merck+, Germany).
Synthesis of phosphoramidate derivatives based on glycerolipid conjugates of AZT
H-phosphonate 1 or 2 (1 equivalent) dissolved in dichloromethane was added dropwise to amino acid hydrochloride (1.5 equivalent) dissolved in triethylamine–tetrachloromethane–water–acetonitrile (1:1:1:10 by volume), at 0 °C. The reaction mixture was stirred at room temperature for 10 min, and then the solvents were evaporated. The residual substance was purified by column chromatography on silica gel, and elution was performed with chloroform–methanol (0 → 1–2% methanol).
3′-Azido-3′-deoxythymidine-5′-yl-[6-(1,3-dipalmitoylglyceryl-2-succinyl)oxyhexyl]-(O-ethyl-L-alanino)phosphoramidate (3c)
Yield 80.5 %; amorphous; Rf 0.54 (а); 1Н NMR (CDCl3, 300 MHz) δ 8.54 (1Н, s, NH, Thy), 7.41 (1Н, s, H6, Thy), 6.11–6.31 (1Н, m, Н1′), 5.18–5.39 (1Н, m, СН, Gro), 3.91–4.44 (15Н, m, ωCH2, Hx–OP, CH2–О, Hx–OSuc, 2СН2, Gro, H3′, H4′, 2H5′, СН2, OEt, СН, Ala), 3.35–3.58 (1Н, m, NH, Ala), 2.55–2.77 (4Н, m, 2СН2, Suc), 2.38–2.52 (2Н, m, 2Н2′), 2.32 (4Н, t, J = 7.7 Hz, 2αСН2, Pal), 1.96 (3Н, s, СН3, Thy), 1.57–1.77 (13Н, m, 2βСН2, Pal, 3CH2, Hx, СН3, Ala), 1.21–1.42 (53Н, m, 24CH2, Pal, CH2, Hx, СН3, OEt), 0.89 (6Н, t, J = 6.9 Hz, 2СН3, Pal); 31Р NMR (CDCl3, 121.5 MHz) δ 7.55, 7.65; Anal. Calcd. for C60H105N6O16P: C, 60.18; H, 8.84; N, 7.02; P, 2.59. Found: C, 59.96; H, 8.80; N, 6.99; P, 2.56.
3′-Azido-3′-deoxythymidine-5′-yl-[6-(1,3-dipalmitoylglyceryl-2-succinyl)oxyhexyl]-(O-isopropyl-L-alanino)phosphoramidate (3d)
Yield 74.6 %; amorphous; Rf 0.61 (а); 1Н NMR (CDCl3, 300 MHz) δ 8.53 (1Н, s, NH, Thy), 7.41 (1Н, s, H6, Thy), 6.12–6.33 (1Н, m, Н1′), 5.20–5.39 (1Н, m, СН, Gro), 3.92–4.48 (14Н, m, ωCH2, Hx–OP, CH2–О, Hx–OSuc, 2СН2, Gro, H3′, H4′, 2H5′, СН, Ala, CH, iPr), 3.39–3.48 (1H, m, NH, Ala), 2.58–2.79 (4Н, m, 2СН2, Suc), 2.38–2.52 (2Н, m, 2Н2′), 2.32 (4Н, t, J = 7.7 Hz, 2αСН2, Pal), 1.96 (3Н, s, СН3, Thy), 1.59–1.80 (11Н, m, 2βСН2, Pal, 2CH2, Hx, СН3, Ala), 1.17–1.52 (58Н, m, 24CH2, Pal, 2СН2, Нх, (СН3)2, iPr), 0.89 (6Н, t, J = 6.9 Hz, 2СН3, Pal); 31Р NMR (CDCl3, 121.5 MHz) δ 9.73; Anal. Calcd. for C61H107N6O16P: C, 60.47; H, 8.90; N, 6.94; P, 2.56. Found: C, 60.21; H, 8.87; N, 6.91; P, 2.54.
3′-Azido-3′-deoxythymidine-5′-yl-[6-(1,3-dipalmitoylglyceryl-2-succinyl)oxyhexyl]-(O-tert-butyl-L-alanino)phosphoramidate (3e)
Yield 89.1%; amorphous; Rf 0.68 (а); 1Н NMR (CDCl3, 300 MHz) δ 8.53 (1Н, s, NH, Thy), 7.41 (1Н, s, H6, Thy), 6.12–6.33 (1Н, m, Н1′), 5.19–5.38 (1Н, m, СН, Gro), 3.95–4.45 (12Н, m, ωCH2, Hx–OP, CH2–О, Hx–OSuc, 2СН2, Gro, H3′, H4′, 2H5′), 3.72–3.91 (1Н, m, СН, Ala), 3.41–3.61 (1Н, m, NH, Ala), 2.58–2.79 (4Н, m, 2СН2, Suc), 2.32 (4Н, t, J = 7.7 Hz, 2αСН2, Pal), 2.34–2.42 (2Н, m, 2Н2′), 1.96 (3Н, s, СН3, Thy), 1.56–1.79 (11Н, m, 2βСН2, Pal, 2CH2, Hx, СН3, Ala), 1.17–1.51 (61Н, m, 24CH2, Pal, 2СН2, Нх, (СН3)3, tBu), 0.89 (6Н, t, J = 6.9 Hz, 2СН3, Pal); 31Р NMR (CDCl3, 121.5 MHz) δ 7.75, 7.85; Anal. Calcd. for C62H109N6O16P: C, 60.76; H, 8.96; N, 6.86; P, 2.53. Found: C, 60.46; H, 8.92; N, 6.83; P, 2.50.
3′-Azido-3′-deoxythymidine-5′-yl-[6-(1,3-dicapronoylglyceryl-2-succinyl)oxyhexyl]-(O-methyl-β-alanino)phosphoramidate (3f)
Yield 81%; amorphous; Rf 0.41 (а); 1Н NMR (CDCl3, 300 MHz) δ 8.53 (1Н, s, NH, Thy), 7.38 (1Н, s, 6H, Thy), 6.11–6.22 (1Н, m, Н1′), 5.18–5.30 (1Н, m, СН2, Gro), 4.23–4.41 (4Н, m, 2Н5′, H4′, H3′), 4.00–4.19 (8Н, m, ωСН2, Нх–ОР, СН2–О, Нх–ОSuc, 2СН2, Gro), 3.68 (3Н, s, СН3–О, β-Ala), 3.28–3.43 (1Н, m, NH, β-Ala), 3.12–3.25 (2Н, m, βСН2, β-Ala), 2.58–2.65 (4Н, m, 2СН2, Suc), 2.50 (2Н, t, J = 6.0 Hz, αСН2, β-Ala), 2.38–2.46 (2Н, m, 2Н2′), 2.32 (4Н, t, J = 7.7 Hz, 2αCH2, Cap), 1.91 (3Н, s, СН3, Thy), 1.52–1.72 (8Н, m, 2βСН2, Сар, 2СН2, Нх), 1.20–1.42 (12Н, m, 4СН2, Сар, 2СН2, Нх), 0.87 (6Н, t, J = 6.8 Hz, 2СН3, Cap); 31Р NMR (CDCl3, 121.5 MHz) δ 8.73, 8.76; Anal. Calcd. for C39H63N6O16P: C, 51.88; H, 7.03; N, 9.31; P, 3.43. Found: C, 51.68; H, 7.00; N, 9.27; P, 3.39.
3′-Azido-3′-deoxythymidine-5′-yl-[6-(1,3-dipalmitoylglyceryl-2-succinyl)oxyhexyl]-(O-methyl-β-alanino)phosphoramidate (3g)
Yield 87.6%; amorphous; Rf 0.46 (а); 1Н NMR (CDCl3, 300 MHz) δ 8.54 (1Н, s, NH, Thy), 7.41 (1Н, s, H6, Thy), 6.11–6.31 (1Н, m, Н1′), 5.18–5.39 (1Н, m, СН, Gro), 3.92–4.42 (12Н, m, ωCH2, Hx–OP, CH2–О, Hx–OSuc, 2СН2, Gro, H3′, H4′, 2H5′), 3.71 (3Н, s, ОСН3, β-Ala), 3.31–3.49 (1Н, m, NH, β-Ala), 3.11–3.29 (2Н, m, βСН2, β-Ala), 2.66–2.78 (4Н, m, 2СН2, Suc), 2.55–2.65 (2Н, m, αСН2, β-Ala), 2.36–2.49 (2Н, m, 2H2′), 2.31 (4Н, t, J = 7.7 Hz, 2αСН2, Pal), 1.96 (3Н, s, СН3, Thy), 1.56–1.79 (8Н, m, 2βСН2, Pal, 2CH2, Hx), 1.30–1.51 (4Н, m, 2CH2, Hx), 1.17–1.28 (48Н, m, 24CH2, Pal), 0.89 (6Н, t, J = 6.9 Hz, 2СН3, Pal); 31Р NMR (CDCl3, 121.5 MHz) δ 9.34, 9.38; Anal. Calcd. for C59H103N6O16P: C, 59.88; H, 8.77; N, 7.10; P, 2.62. Found: C, 59.66; H, 8.74; N, 7.08; P, 2.60.
Chemical hydrolysis in buffer solutions
The aqueous buffer (Na–phosphate, рН 7.3; Tris, рН 8.5; or Na_borate, рН 9.5) (3 mL) was equilibrated at 37 °С and mixed with solutions of the tested compounds 3c–g (2.0 mg) in DMSO (0.2 mL) also equilibrated at 37 °С. The hydrolysis course was monitored by TLC with UV detection, system (a). The approximate content of the starting compound and hydrolysis products in the mixture was estimated on the basis of the TLC data.
Enzymatic hydrolysis catalyzed by pig pancreatic lipase
A dispersion of prodrugs 3c–g (0.5 mL, a 1:4 mixture of 25 mM tested compound in ethanol and 25 mM sodium taurodeoxycholate in water) was equilibrated at 37 °С and mixed with the incubated mixture (pig pancreatic lipase, EC 3.1.1.3, 31.1 mg, 30.1 U/mg in 0.1 M PIPES buffer, 2 mL) also equilibrated at 37 °С. The prodrug concentration in the resulting solution was 1 mM, and enzyme activity, 375 U/mL. In certain time intervals aliquots (150 μL) were taken out of the hydrolysis mixtures and cooled to 0 °С. The kinetics of the process was monitored by TLC with UV detection (digestion of initial compounds 3c–g in system (a), accumulation of hydrolysis products, presumably 1,2-pseudomonoglycerides, in system (b)). The half-lives of the starting compounds as well as the dynamics of the formation of hydrolysis products were evaluated using time–concentration dependencies of the corresponding compounds. The approximate contents of the starting compound and hydrolysis products in the mixtures were evaluated by the TLC data.
Antiviral activity
Cells and viruses
MT-4 cells (AIDS Reagent Program) were maintained in RPMI 1640 medium supplemented with 10% FBS (fetal bovine serum; Sigma, USA), 1× penicillin–streptomycin, and 1× GlutaMAX (all from Gibco BRL Life Technologies, USA), in a humidified atmosphere with 5% СО2 at 37 °С. The HIV-1 strain MvP-899 (Russian State Collection of Viruses, D.I. Ivanovsky Institute of Virology), isolated in Germany in 1987, was used for infection of MT-4 cells.
Cytotoxicity assay
MT-4 cells, at a density of 3 × 104 cells/well, were mixed in 96-well plates with different dilutions of compounds. After 5 days of incubation at 37 °C, the cells were mixed with the MTT solution (final concentration 0.5 mg/mL). The microplates were incubated for 4 h. Then, the obtained formazan crystals were dissolved in DMSO. The optical density was measured at 590 nm. The drug concentration, at which the cell viability had been reduced by 50% (CC50), was determined by nonlinear regression analysis (GraphPad 6 Software Inc., USA).
HIV antiviral assay
Serial dilutions of compounds were added to MT-4 cells in 96-well plates in complete RPMI 1640 medium. For this, tenfold dilutions of the compound were used directly in 96-well plates. After 2-h incubation at 37 °C, the cells were infected with HIV-1 MvP-899 at 100 TCID50 (50% tissue culture infectious dose). After 72 h, the supernatants were collected and the virus production was measured using an HIV-1 p24 antigen ELISA (enzyme-linked immunosorbent assay; Vector-Best, Russia). The drug concentrations required to inhibit 50% of the viral spread were determined by regression analysis.
Abbreviations
- AIDS:
-
Acquired human immunodeficiency syndrome
- Ala:
-
Alanine
- AZT:
-
3′-azido-3′-deoxythymidine
- EC50:
-
Half maximal effective concentration
- HAART:
-
Highly active antiretroviral therapy
- HIV:
-
Human immunodeficiency virus
- NMR:
-
Nuclear magnetic resonance
- NRTI:
-
Nucleoside reverse transcriptase inhibitor
- SI:
-
Selectivity index
- TLC:
-
Thin-layer chromatography
- СС50:
-
Half maximal cytotoxic concentration
References
UNAIDS. Global HIV & AIDS statistics—2020 fact sheet. UNAIDS. 2020. https://www.unaids.org/en/resources/fact-sheet. Accessed 17 Feb 2020.
Gortmaker SL, Hughes M, Cervic J, Brady M, Johnson GM, Seage GR, et al. Pediatric AIDS clinical trials group protocol 219 team. Effect of combination therapy including protease inhibitors on mortality among children and adolescents unfected with HIV-1. NEJM. 2001;345:1522–28. https://doi.org/10.1056/NEJMoa011157.
Gumina G, Choi Y, Chu CK. Recent advances in antiviral nucleosides. Antivir Nucleosides. 2003;1:1–76. https://doi.org/10.1016/B978-044451319-9/50001-4.
Clercq E. Antiviral drug discovery and development: where chemistry meets with biomedicine. Antivir Res. 2005;67:56–75. https://doi.org/10.1016/j.antiviral.2005.05.001.
Wong A, Toth I. Lipid, sugar and liposaccharide based delivery systems. Curr Med Chem. 2001;8:1123–36. https://doi.org/10.2174/0929867013372535.
Galegov GA. Phosphazide (nikavir) is a highly effective drug for the treatment of HIV/AIDS infection. Vopr Virusol. 2017;62:5–11. https://doi.org/10.18821/0507-4088-2017-62-1-5-11.
Trznadel R, Singh A, Kleczewska N, Liberska J, Ruszkowski R, Celewicz L. Synthesis and in vitro anticancer activity of new gemcitabine-nucleoside analogue dimers containing methyltriazole or ester-methyltriazole linker. Bioorg Med Chem Lett. 2019;29:2587–94. https://doi.org/10.1016/j.bmcl.2019.08.003.
Seley-Radtke KL, Yates MK. The evolution of nucleoside analogue antivirals: a review for chemists and non-chemists. Part 1: early structural modifications to the nucleoside scaffold. Antivir Res. 2018;154:66–86. https://doi.org/10.1016/j.antiviral.2018.04.004.
Chudinov MV. Ribavirin and its analogs: can you teach an old dog new tricks? Fine Chem Technol 2019;14:7–23. https://doi.org/10.32362/2410-6593-2019-14-4-7-23.
Llibre JM, Sharon W, Gatell JM. Backbones versus core agents in initial ART regimens: one game, two players. J Antimicrob Chemother. 2016;71:856–61. https://doi.org/10.1093/jac/dkv429.
Yoshio H. Recent progress in prodrug design strategies based on generally applicable modifications. Bioorg Med Chem Lett. 2017;27:1627–32. https://doi.org/10.1016/j.bmcl.2017.02.075.
Smith N, Bade AN, Soni D, Gautam N, Alnouti Y, Herskovitz J, et al. A long acting nanoformulated lamivudine ProTide. Biomater. 2019;223:1–11. https://doi.org/10.1016/j.biomaterials.2019.119476.
Lambert DM. Rationale and applications of lipids as prodrug carriers. Eur J Pharm Sci. 2000;11:15–27. https://doi.org/10.1016/S0928-0987(00)00161-5.
Shastina NS, Maltseva TYU, D’yakova LN, Lobach OA, Chataeva MS, Nosik DN, et al. Synthesis, properties, and anti-HIV activity of new lipophilic 3’-azido-3’-deoxythymidine conjugates containing functional phosphoric linkages. Russ J Bioorg Chem. 2013;39:161–9. https://doi.org/10.1134/S1068162013020118.
Saboulard D, Naesens L, Cahard D, Salgado A, Pathirana R, Velazquez S, et al. Characterization of the activation pathway of phosphoramidate triester prodrugs of stavudine and zidovudine. Mol Pharm. 1999;56:693–704.
Mavromoustakos T, Calogeropoulou T, Koufaki M, Kolocouris A, Daliani I, Demetzos C, et al. Ether phospholipid-AZT conjugates possessing anti-HIV and antitumor cell activity. Synthesis, conformation analysis, and study of their thermal effects on membrane bilayer. J Med Chem. 2001;44:1702–9. https://doi.org/10.1021/jm001121c.
Piantadosi C, Marasco C, Morris-Natschke L, Meyer K, Gumus F, Surles J, et al. Synthesis and evalution of novel ether lipid nucleoside conjugates for anti-HIV-1 activity. J Med Chem. 1991;34:1408–14.
Amyere M, Payrastre B, Krause U, Smissen P, Veithen A, Courtoy PJ. Constitutive macropinocytosis in oncogenetransformed fibroblasts depends on sequential permanent activation of phosphoinositide 3-kinase and phospholipase C. Mol Biol Cell. 2020;11:3453–67. https://doi.org/10.1091/mbc.11.10.3453.
Doherty GJ, McMahon HT. Mechanisms of endocytosis. Annu Rev Biochem. 2009;78:857–902. https://doi.org/10.1146/annurev.biochem.78.081307.110540.
Swanson JA, Hoppe AD. The coordination of signaling during Fc receptor-mediated phagocytosis. J Leukoc Biol. 2004;76:1093–103. https://doi.org/10.1189/jlb.0804439.
Harmon B, Ratner L. Induction of the Gαq signaling cascade by the human immunodeficiency virus envelope is required for virus entry. J Virol. 2008;82:9191–205. https://doi.org/10.1128/JVI.00424-08.
Contreras X, Mzoughi O, Gaston F, Peterlin MB, Bahraoui E. Protein kinase C-delta regulates HIV-1 replication at an early post-entry step in macrophages. Retrovirology. 2012;9:37. https://doi.org/10.1186/1742-4690-9-37.
Xiao Q, Sun J, Ju Y, Zhao Y, Ciu Y. Novel approach to the synthesis of AZT 5‘-O-hydrogen phospholipids. Tetrahedron Lett. 2002;43:5281–3. https://doi.org/10.1016/S0040-4039(02)01045-6.
Acknowledgements
This study was supported by the Ministry of Science and Higher Education of the Russian Federation (Project No. 0706-2020-0019).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Darnotuk, E.S., Siniavin, A.E., Shulga, N.V. et al. Phosphoramidate conjugates of 3′-azido-3′-deoxythymidine glycerolipid derivatives and amino acid esters: synthesis and anti-HIV activity. Med Chem Res 30, 664–671 (2021). https://doi.org/10.1007/s00044-020-02672-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-020-02672-8