Abstract
In searching for better therapeutic alternatives to treat cutaneous leishmaniasis (CL), this study aimed to obtain and evaluate the efficacy and toxicity of new chroman-4-one hydrazones derivatives. Compounds were prepared and characterized, and then transformed into hydrazonas for molecular optimization. Their cytotoxicity was tested in different cell types using an in vitro MTT assay and the efficacy was evaluated using an in vitro macrophage intracellular amastigotes of Leishmania (Viannia) panamensis and L. (V) braziliensis by flow cytometry. The therapeutic effect of two formulations of chroman-4-one hydrazones on the CL induced by L. (V) braziliensis in golden hamsters was determined according to the size of lesions after treatment. The effect of these compounds in the production of inflammatory mediators and cell migration was also determined by in vitro assays using human fibroblasts models. Neither cytotoxicity nor genotoxicity was observed. The benzoic acid hydrazone derivative 2-(2,3-dihydro-4H-1-benzopyran-4-ylidene) hydrazide (4), produced a higher percentage of clinical cures, followed by benzoic acid, 2-(2,3-dihydro-4H-1-benzothiopyran-4-ylidene) hydrazide (3), while benzoic acid, 2-(2,3-dihydro-1,1-dioxide-4H-1-benzothiopyran-4-ylidene) hydrazide (5) and 4-pyridinecarboxylic acid, 2-(4H-1-benzopyran-4-ylidene) hydrazide (6) caused a poor therapeutic response. The compound 4 also showed an effect in the inflammatory and fibroblast migration processes. In conclusion, this is the first report of antileishmanial activity combined with inflammatory and wound healing properties. Results obtained here suggest that this strategy could be a good alternative for development of new drugs for the treatment of CL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Leishmaniasis is a tropical disease caused by parasites belonging to the Leishmania genus that is endemic in 98 countries, affecting 12 million people. There are about 2,000,000 new cases per year, of which 0.7–1.3 million cases are cutaneous leishmaniasis (CL) (Alvar et al. 2012). The massive displacement of populations, climatic change, growing resistance to drug treatment, lack of therapeutic alternatives and long treatments are creating a significant rise in this disease, with a resultant increase in public health problems. The pharmacological arsenal currently used to combat CL is limitated. Only five drugs are available (meglumine antimoniate—MA or sodium stibogluconate, miltefosine, amphotericin B—AMB and paromomycin), all of them displaying a series of drawbacks related to a decreased efficacy, moderate to severe adverse effects and high costs in-patient care (Den Boer et al. 2011). For that, there is an urgent need to find new and better drugs to treat CL.
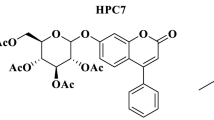
An useful strategy, commonly used in drug development, involves the use of bioactive molecule as a template to obtain more potent molecules with the best pharmacological properties (Mathur and Hoskins 2017). The benzopyran system is a valuable scaffold in medicinal chemistry, since it is found in many natural bioactive molecules, such as flavonoids, coumarins, chromenes, chromans, as well as some alkaloids (Fig. 1) (Saengchantara and Wallace 1986; Borges et al. 2005; Sharma et al. 2011; Gaspar et al. 2014; Ramendra et al. 2014). Therefore, this chemical moiety is considered a privileged structure, whose range of activity includes substances for human health, insecticides and other molecules for agriculture. Particularly, chroman and thiochroman also exhibit a wide range of biological activities such antiestrogenic (Kanbe et al. 2006), cytotoxic (Gaspar et al. 2019), antitumoral and antiepileptic (Rawat 2016). They also have Sirtuin 2 selective inhibition (Friden-Saxin et al. 2012). In addition, from the synthetic point of view, it is a very versatile molecule, relatively easy to synthesize (Borges et al. 2005; Ramendra et al. 2014; Nicolaou et al. 2000) and possess different sites for chemical transformations in the aromatic ring and the heterocycle or carbonyl systems. Moreover, the thiochroman analog is susceptible of oxidation to sulfoxide and sulfone.
Due to the high incidence of CL in tropical countries, a research program has been designed to look for molecules with antileishmanial activity and to identify candidate compounds to be submitted to CL animal assay and eventually to be converted into new medicines. In this work, we report the synthesis process to obtain several active molecules against CL, starting from a simple molecules like chroman and thiochroman, through a sequence of chemical transformations to the in vitro and in vivo antileishmanial evaluations. The effect of these compounds in the inflammatory and healing processes was also determined.
Materials and methods
Spectroscopy
All commercially available reagents and solvents were obtained from commercial suppliers and used without further purification. 4-Chromane (1) and 4-thiocromanone (2) were purchased from Sigma-Aldrich. The reaction progress was monitored using thin layer chromatography on silica gel TLC aluminum sheets (60F254, Merck). The melting points were determined using a Mel-Temp apparatus (Electrothermal, Staffordshire, UK) and were uncorrected. FTIR spectra were obtained on a Bruker Alpha FTIR spectrometer (Bruker Optic GmbH, Ettlingen, Germany). 1H- and 13C-nuclear magnetic resonance spectra were recorded using a Bruker Fourier 300 spectrometer (Bruker Bio-Spin GmbH), operating at 300 MHz for 1H and 75 MHz for 13C. Samples were dissolved in DMSO-d6 or CDCl3, using TMS as an internal standard. HRMS was obtained using Q-ToF quadrupole/orthogonal spectrometry (Waters) in either the negative (reported as [M + H]+) or positive mode (reported as [M + H]+) and a Bruker Impact II UHR-Q-TOF mass spectrometer (Bruker Daltonik) in the positive mode.
General procedure for the preparation of thiochroman-4-one or 4-chromanone
To a mixture of acrylic acid (700 mL, 720 mg, 10 mmol) and thiophenol or phenol (15 mmol), I2 (20% mol, 760 mg, 3 mmol) was added, and the mixture was stirred at 50 °C for 24 h. After the completion of the reaction (monitored by TLC), a cold saturated sodium thiosulfate solution (30 mL) was added and extracted with dichloromethane (2 × 25 mL). The combined organic layers were mixed with a saturated solution of sodium bicarbonate and extracted to remove the unreacted starting material layer, which was acidified with 10% HCl and extracted with dichloromethane (3 × 50 mL). The combined organic layers were dried over Na2SO4, and the evaporation of the solvent under reduced pressure afforded 64–66% of the desired additional product. The product was cooled down to 2 °C in an ice bath, 3 mL of concentrated sulfuric acid was added, and the reaction mixture was allowed to warm to room temperature for 2 h, with magnetic stirring. The reaction was quenched with ice, and the mixture was extracted with dichloromethane (3 × 50 mL). The combined organic layers were washed once with water, and then with saturated NaHCO3 solution. The combined organic layers were washed with brine, dried over Na2SO4, and concentrated under reduced pressure. The residue was purified by column chromatography over silica gel using hexane/EtOAc (9:1), as an eluent, to obtain thiochroman-4-one or 4-chromanone, as a white solid (90–85%).
Oxidation of sulfides to sulfones (5)
To a 25-mL glass tube, sulfide 5 (1.0 mmol), oxone® (0.9221 g, 1.5 mmol) and a water ethanol mixture (1:1) (3.0 mL) were added, and the mixture was stirred at 60 °C for 12 h. The mixture was then cooled to room temperature and extracted with dichloromethane (3 × 25 mL). The combined organic layers were dried over anhydrous Na2SO4 and concentrated under reduced pressure. The residue was purified by column chromatography over silica gel using mixtures of hexane and EtOAc as eluents.
General procedure for the preparation of Acyl hydrazone derivatives 3, 4, and 6
Thiochroman-4-ones or 4-Chromanone (0.5 mmol) was dissolved in anhydrous methanol (25 mL). The mixture was heated at reflux, and then with hydrazide (1.0 mmol, 2 equiv.), and 60 mL of glacial acetic acid was added. After 12 h at reflux, the resulting precipitate was collected through filtration and washed with methanol. After drying under a vacuum, the residue was passed through a small pad of silica gel with ethyl acetate, after the solvent acyl hydrazones were evaporated and obtained as white solids.
Spectroscopy of hydrazones
Benzoic acid, 2-(2,3-dihydro-4H-1-benzothiopyran-4-ylidene)hydrazide (3)
Yield: 82%, p.f: 160–161 °C. 1H RMN (300 MHz, DMSO), δ: 3.06 (m, 4H, H2, H3), 8.20 (sbr, 1H). (sbr, 1H, H4), 7.19 (sbr, 1H, 1H, H5), 7.27 (m, 2H, H6, H7), 7.90 (sbr, 2H, H2′–H6′), 7.52 (m, 2H, H3′–H5′), 7.54 (sbr, 1H, H4′), 10.87 (s, 1H, N–H). 13C-RMN δ: 25.7 (–C3), 28.4 (–C2), 121.8 (–C9), 125.7 (–C5), 126.0 (–C4), 128.4 (–C7), 128.4 (–C2′–C6′),128.8 (–C3′–C5′), 129.9 (–C6), 132.0 (–C4′), 134.5 (–C1′), 136.8 (–C8), 153.1 (–C3a), 164.5 (–C=O). m/z 282.0827 for C16H14N2OS [M+H]+, calculated 282.0821.
Benzoic acid, 2-(2,3-dihydro-4H-1-benzopyran-4-ylidene) hydrazide (4)
Yield: 93%, p.f: 190–191 °C. 1H RMN (300 MHz, DMSO), δ: 2.97 (t, J = 6.3, 2H, H3), 4.27 (t, J = 6.3, 2H, H2), 8.02 (sbr, 1H, H4), 7.02 (sbr, 1H, 1H, H5), 6.94 (seudo t, J = 7.5, 1H, H6), 6.91 (d, J = 7.5, 1H, H7), 7.88 (sbr, 2H, H2′–H6′), 7.51 (m, 2H, H3′–H5′), 7.56 (sbr, 1H, H4′), 10.88 (s. 1H, N–H). 13C-RMN δ: 26.4 (–C3), 65.2 (–C2), 117.9 (–C7), 120.8 (–C9), 121.7 (–C5), 125.4 (–C4), 128.3 (–C2′–C6′),128.8 (–C3′–C5′), 132.0 (–C4′), 134.5 (–C1′), 150.8 (–C3a), 157.6 (–C8), 164.3 (–C=O). m/z 266.1055 for C16H14N2O2 [M+H]+, calculated 266.1049.
Benzoic acid, 2-(2,3-dihydro-1,1-dioxido-4H-1-benzothiopyran-4-ylidene)hydrazide (5)
Yield: 78%, p.f: 216–217 °C. 1H RMN (300 MHz, DMSO). δ: 3.75 (t, J = 5.7, 2H, H2), 3.45 (t, J = 5.7, 2H, H3), 8.26 (sbr, 1H, H4), 7.93 (d, J = 8.6, 1H, H5), 7.61 (m, 1H, H6), 7.77 (m, 1H, H7), 7.93 (d, J = 8.6, 2H, H2′–H6′), 7.54 (m, 2H, H3′–H5′), 7.72 (m, 2H, H4′), 11.09 (s. 1H, N–H). 13C-RMN δ 25.0 (–C3), 46.4 (–C2), 123.2 (–C5), 126.7 (–C4), 128.7 (–C2′–C6′), 128.8 (–C3′–C5′), 130.9 (–C6), 132.3 (–C4′), 133.3 (–C8), 133.6 (–C7), 133.9 (–C9), 134.1 (–C1′), 147.3 (–C3a), 166.6 (–C=O). m/z 315.0790 for C16H15N2O3S [M+H]+, calculated 315.0797.
4-Pyridinecarboxylic acid, 2-(4H-1-benzopyran-4-ylidene)hydrazide (6)
Yield: 80%, p.f: 198–199 °C. 1H RMN (300 MHz, DMSO), δ: 3.13 (t, J = 6.0, 2H, H3), 4.44 (t, J = 6.0, 2H, H2), 7.10 (seudo t, J = 7.5, 1H, H6), 7.19 (d, J = 7.5, 1H, H7), 7.55 (seudo t, J = 7.7, 1H, H5), 8.24 (d, J = 7.5, 1H, H4), 7.97 (d, J = 4.8, 2H, H2′–H6′), 8.94 (m, 2H, H3′–H5′), 7.56 (sbr, 1H, H4′), 11.30 (s. 1H, N–H). 13C-RMN δ 26.3 (–C3), 65.3 (–C2), 117.9 (–C7), 120.1 (–C9), 121.7 (–C5), 122.2 (–C2′–C6′), 125.4 (–C4), 132.3 (–C6), 142.0 (–C1′), 150.5 (–C3′–C5′), 152.1 (–C3a), 157.2 (–C8), 163.2 (–C=O). m/z 268.1080 for C15H14N3O2 [M+H]+, calculated 268.1080.
Biological study
Cells and culture conditions
Human U937 (CRL-1593-2TM) macrophages, human Detroit 551 (CCL-110TM) fibroblast and golden hamster BHK-21 (CCL-10TM) kidney fibroblast were purchased from the American Type Culture Collection. Cells were cultured in the corresponding medium, according to the manufacturer’s instructions. The primary cultures of macrophages and fibrocytes, derived from human monocytes (huMDM and huMDF, respectively), were obtained from anticoagulated venous blood from healthy donors, after signing informed consent. The huMDM and huMDF were obtained, according to the methodology described by others (Robledo et al. 1994; Montoya et al. 2015).
In vitro cell toxicity
U937, Detroit 551, BHK-21, huMDM, and huMDF in suspension in the corresponding culture media were dispensed in 96-well plates, at a concentration of 1 × 105 or 2.5 × 105 or 3 × 105 or 2.5 × 106 cells/mL. Then, 100 µL/well of each compound at concentrations of 200–100–50–25–12.5–6.25 µL/mL were added. Plates were incubated at 37 °C, 5% CO2 for 72 h. Then, 20 μL of (3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) solution (0.5 mg/mL) (Sigma) was added to each well, and the plates were incubated at 37 °C, 5% CO2 for 3 h. The reaction was stopped by adding 100 μL/well of 50% isopropanol solution, with 10% sodium dodecyl sulfate and 30 min of incubation. The concentration of formazan was determined at 570 nm in a Varioskan Flash multimode reader (Thermo Scientific), and the intensity of the color was registered as optical densities (O.D) (Mesa et al. 2015). Cells treated with antileishmanial drugs, AMB, and the cytotoxic drug, doxorubicin (DOXO), were used as controls for the cytotoxicity (positive control), while the cell incubated in cell culture media, with no compound or drug, was used as a growth cell control (negative control). All determinations were conducted in triplicate in at least two independent experiments.
Leishmania (Viannia) panamensis and L. (V) braziliensis in vitro culture conditions
Promastigotes of L. (V) panamensis and L. (V) braziliensis, transfected with green fluorescent protein (MHOM/CO/87/UA140-EGFP and M/HOM/CO/88/301-EGFP, respectively), were maintained in a modified Novy-MCNeal-Nicolle medium, with phosphate buffer saline (PBS), plus glucose, pH 6.9 at 26 °C (Limoncu et al. 1997).
In vitro antileishmanial activity
The U937 cells were induced to differentiate to macrophage by exposing the cells (3 × 105 cells/mL) to 3 ng/mL of phorbol 12-myristate 13-acetate (Sigma) and incubation at 37 °C. Forty-eight hours afterwards, the cells were infected with the promastigotes of L. (V) panamensis and L. (V) braziliensis in a stationary growth phase (day 5 or 6) at a parasite:cell ratio of 30:1 or 15:1 for L. (V) panamensis or L. (V) braziliensis, respectively. The cells and parasites were incubated at 34 °C, 5% CO2 atmosphere. After 3 h of incubation, the cells were washed twice with PBS, and a 1 mL fresh RPMI 1640 medium was added into each well. The plates were incubated again at 34 °C, 5% CO2 for 24 h (Pulido et al. 2012).
After 24 h of the infection of U937 cells, the culture medium was replaced by a fresh RPMI medium, containing each compound at 100–25–6.25–1.78 μg/mL. Infected and treated cells were maintained at 34 °C and 5 % CO2. Then, 72-h cells were removed from the bottom plate with a trypsin/EDTA (250 mg) solution, and the removed cells were centrifuged at 1100 rpm for 10 min at 4 °C. The supernatant was discarded, and cells were washed with 1 mL of cold PBS and centrifuged at 1100 rpm for 10 min at 4 °C, and then the supernatant was discarded, and cells were suspended in 500 μL of cold PBS and analyzed in an argon laser Cytomics FC 500MPL flow cytometer (Beckman Coulter), reading at 488 nm of excitation and 525 nm of emission and counting 10,000 events. Infected cells were determined according the positive events for green fluorescence (parasites). Infected cells exposed to AMB or MA were used as controls for the antileishmanial activity (positive control), while infected cells incubated in a fresh RPMI 1640 medium were used as controls for infection (negative control). Each concentration was tested in triplicate in two independent experiments.
In vivo antileishmanial activity
Male and female golden hamsters (Mesocricetus auratus), at 6 or 7 weeks old, were infected with 5 × 107 stationary growth phase promastigotes of L. (V) braziliensis in the dorsum, following the method established elsewhere (Robledo et al. 2012). After the full development of skin lesions, they were distributed randomly into nine groups (n = 5 animals per group). Four groups were treated topically with 100 μL of each compound in PBS solution (3-S, 4-S, 5-S, or 6-S), at 1.5 mg/kg/day, for 10 days. The other four groups were treated with an ointment formulation at 4% of each compound (3-O, 4-O, 5-O, or 6-O), at 40 mg/day, for 28 days. A ninth and ten group of hamsters were treated with MA, administered intralesional, at 200 μg/three times per week for 10 days (MA-10) or 28 days (MA-28). After the end of treatment, animals were kept under observation for a period of 90 days. The effectiveness of each compound was determined according to the evolution of the size of the lesion in response to the treatment.
The size (width and length) of the ulcer and the body weight were obtained at the end of the treatment and then every 2 weeks, until the end of the study (90 days after the end of the treatment), for each individual. The evaluation time points were: pretreatment day (TD0), end of treatment (TD28), and posttreatment days (PTD) 30, 60, and 90. The effectiveness of each treatment was assessed, comparing the lesion sizes, prior to and after treatment, for each individual. The outcome at the end of study was recorded as a cure (epithelial healing and emergence of fur); improvement (reduction of the lesion size by at least >20%); relapse (reactivation of the lesion after an initial improvement or cure); or failure (increase of the lesion size).
The Ethics Committee for Animal Experimentation at the Universidad de Antioquia approved all of the experiments conducted with the hamsters (Act No. 53 of May 8, 2009 and Act No. 91 of September 25, 2014). The Procedures for obtaining donor cells were endorsed by the Human Ethics Committee at University of Antioquia (CIBH).
Quantification of inflammatory mediators CCL2/MCP-1, TGF-β1, IFN-γ and cyclooxygenase-2 activity in huMDM exposed to compounds 3–6
The production of MCP-1, TGF-β1, and IFN-γ by huFDM was quantified at 6 and 48 h after exposure to each compound at a maximum concentration of 20 μg/mL by the ELISA technique using the Quantikine® kits (R & D Systems, USA) and following the manufacturer’s instructions. The intensity of the color was determined at 540 nm in a Multiscan Flash Multimode reader (Thermo Scientific) and registered as O.D.
The cyclooxygenase-2 (COX-2) activity was determined from the cell lysates of huFDM co-cultures after 6 and 48 h of exposure to a maximum concentration of 20 μg/mL of each compound by the COX Fluorescent Activity Assay Kit (Cayman Chemicals, USA), following the manufacturer’s instructions.
The intensity of the fluorescence was determined at 530–540 nm in a Varioskan Flash multimode reader (Thermo Scientific) and registered as Arbitrary Units of fluorescence (AFU).
In vitro wound healing (scratch) assay
The effect of compounds 3–6 on fibroblast migration and closure of the scratch was investigated with a CytoSelect™ Wound Healing Assay Kit (Cell Biolabs, Inc.) and following the method described by others (Montoya et al. 2015). In brief, a Detroit 551 fibroblast (2.5 × 105/mL) in DMEM, containing 5% FBS, were seeded into a 24-well tissue culture plate, containing proprietary treated inserts in the plate wells, with their “wound field” aligned in the same direction, and incubated for 24 h to allow the cells adhere and reach a confluence of 60–80%. After removing the inserts from the wells, the medium was carefully aspired, and the wells were washed with DMEM, containing 2% FBS, to remove dead cells and debris. Finally, the cells were treated with 20 μg/mL of each tested compound and incubated for a further 8, 16, and 24 h at 37 °C, 5% CO2. The migration of the fibroblast into the wound field was determined by microscopic imaging of the wound closure. Two sets of experiments were performed in duplicate. The influence of compounds on wound closure was compared with an untreated control (0 h). As a positive control, DMEM, with 20% FBS, was used. The density of the cells in the wells, without a created wound area (confluent area), was used as a 100% wound closure.
In vitro genotoxicity
Chromosome alterations, induced by 3 and 4, were evaluated by the chromosome aberration test, using human lymphocytes from healthy donors. Cells cultured in an RPMI 1640 medium, supplemented with 2 mM l-glutamine, 10% FBS, and 1% penicillin–streptomycin (10,000 U–10 mg/mL) (complete medium), were stimulated with 200 μL phytohemagglutinin and incubated at 37 °C, 5% CO2. After 36 h, the cells were treated with each of the sublethal concentrations (46–23 and 12 μg/mL) and incubated for 24 h. Colcemid (0.1 pg/mL) was added, and cells were incubated again for 1 h. The cells were centrifuged, resuspended in 0.075 M KCl, and incubated at 37 °C for 7 min. Then, they were fixed for 10 min with a Carnoy solution, washed and dripped. Slides were dried and stained with 5% Giemsa, pH 6.8. One hundred metaphase cells (46 chromosomes) were analyzed. Structural chromosome aberrations were classified as chromatid breaks (B), chromosome breaks (BB), dicentric chromosomes (DC), ring chromosomes (R) and multiradial chromosomes (MR) (OECD 2016). Each treatment was performed in two separate experiments, using RPMI as a negative control and mitomycin-C (10 μM) as a positive control.
Data analysis
The cytotoxicity was determined according to mortality (%) for each condition (compound and concentration) using Eq. (1), where the O.D of the control corresponds to 100% viability.
The % of mortalities obtained in each concentration were used to calculate the half-maximal lethal concentration (LC50) using the Probit analysis (Finney 1978).
The antileishmanial activity was determined according to the infection (number of parasites in the infected cells), obtained for each experimental condition according to dotplot analysis by infected cells and histograms by the mean fluorescence intensity (MFI) in fluorescent parasites (Pulido et al. 2012). The parasite inhibition was calculated by Eq. 2, where the MFI in the control was 100% of parasites.
As above, the % of the inhibition of infection was used to calculate the half-maximum effective concentration (EC50), as determined by the Probit analysis (Finney 1978).
To compare the level of cytotoxicity and antileishmanial activity, the cytotoxicity of each compound was graded, according to the LC50 values, as high (LC50 < 100 μg/mL), moderate (LC50 > 100 to <200 μg/mL) and low (LC50 > 200 μg/mL). In turn, the activity was graded as high when EC50 < 25 μg/mL, moderate with EC50 values > 25 and <50 μg/mL, and low when EC50 was >50 μg/mL. The Index of Selectivity was calculated using the equation: IS = LC50/EC50.
The in vivo efficacy of the compound was expressed as the percentage of healing, improvement or failure and compared with the efficacy observed in the group treated with meglumine antimoniate. Parametric and nonparametric tests were carried out in order to compare the percentages and frequencies. Variances were expressed as standard errors, and the statistical significance was determined, using the analysis of variance (ANOVA) to compare the groups.
The quantification data of the inflammatory mediators were expressed as the mean of the results ± SD. Significant statistical differences between the treated groups and the control group were determined by means of a one-way ANOVA and the application of Dunnett’s multiple comparison test using GraphPad Prism 6.0.
Effect on healing was calculated according to the percentage of the wound closure using Eq. (3).
Monolayer wound healing assay data were analyzed by a two-way ANOVA, with an independent factor experiment and treatment, followed by Bonferroni post hoc tests. Differences were considered significant if p < 0.05. Statistical analysis was performed with GraphPad Prism 6.0.
Results and discussion
The different drugs that are recommended treatment for CL are associated with several side effects, such as arthralgia, hepatotoxicity, myalgia, fever, and several weeks of painful injection site, which limit their usage (WHO 2010). Therefore, the development of novel antileishmanial drugs, which are more effective, safer and more affordable, is urgently required. The strategy employed in the present work started with the selection of an abundant and chemically modifiable scaffold based on a benzopyran structure, such as a chroman and thiochroman. Thus, hydrazones were prepared from the active chromans and thiochromans, since this type of substance has antiparasitic activity due to its inhibitory effects in parasite proteases (Muñoz et al. 2006). After characterization, their cytotoxicity was evaluated using an in vitro MTT assay. Subsequently, the efficacy was evaluated using an in vitro macrophage intracellular amastigotes of Leishmania (Viannia) panamensis and L. (V) braziliensis systems by flow cytometry.
Considering that topical treatment are recommended by the World Health Organization for the treatment of noncomplicated CL (Muñoz et al. 2006), the efficacy of chroman hydrazones formulated in a phosphate buffer solution (PBS), pH 7.2, or in an ointment was validated in in vivo studies. Both formulations were assayed topically in the hamster model of CL caused by L. (V) braziliensis. Simultaneously, other biological properties related to antiparasite activity, such as cicatrizing and anti-inflammatory activities, were also studied. The ointment was the most effective against the CL hamster model, because this pharmaceutical preparation permits a high adherence in the skin lesion, with long drug delivery in addition to other beneficial effects, like emollient, occlusive and antiseptic effects (Tsatsop et al. 2017).
Molecular optimization of chroman and thiochroman
In this work, chromanone (1) and thiochromanone (2), commercially available, were selected to be optimized, since they have a wide spectrum of activity, are relatively hydrophobic small heterocycles and susceptible to further modifications (Scheme 1), and their preparation is relatively easy, with high yields. On the other hand, hydrazones were selected since they have shown protease inhibitory effects in some parasites (Desai et al. 2004; Cywin et al. 2003) and therefore could have a complementary activity to that already exhibited by chromans. Nevertheless is difficult to control the oxidation of sulfones and sulfoxides, a fact enables their production at a scale sufficient for more advanced clinical trials.
The compounds 1 and 2 were prepared from phenol and thiophenol, instead of being obtained commercially (Scheme 1). Then, the thiochroman was selectively oxidized to the respective sulfone but after the hydrazone formation.
The synthesized compounds were: benzoic acid, 2-(2,3-dihydro-4H-1-benzothiopyran-4-ylidene) hydrazide (3), benzoic acid, 2-(2,3-dihydro-4H-1-benzopyran-4-ylidene) hydrazide (4), Benzoic acid, 2-(2,3-dihydro-1,1-dioxido-4H-1-benzothiopyran-4-ylidene) hydrazide (5), and 4-Pyridinecarboxylic acid, 2-(4H-1-benzopyran-4-ylidene) hydrazide (6) (Scheme 1). Compound 5 was made directly from the oxidation of hydrazone 3.
Cytotoxicity and antileishmania effect of chroman-4-one hydrazone derivatives in L. (V) panamensis and L. (V) braziliensis
The four new aryl hydrazones were evaluated in L. (V) panamensis and L. (V) braziliensis, the two most prevalent species in Colombia that cause CL. It was previously established that a substance would be considered to have potential antileishmania activity if it exhibited a mean effective concentration (EC50) < 50 μg/mL. Compounds 3 and 4 exhibited high and moderate cytotoxicity, respectively, for U937 cells, with EC50 values of 62.2 and 112.9 μg/mL, while 5 and 6 were not cytotoxic at the evaluated concentrations (Table 1). As expected, AMB and DOXO exhibited high cytotoxicity for this cell line, with EC50 values of 26.8 and <1.0 μg/mL, respectively. On the other hand, compounds 3 and 4 were effective against intracellular amastigotes of L. (V) braziliensis, with an EC50 of <25 μg/mL, but were inactive for L. (V) panamensis, with an EC50 of >50 μg/mL. Compounds 5 and 6 showed a low activity for both Leishmania species (Table 2). Both MA and AMB were highly active for L. (V) panamensis and L. (V) braziliensis, with an EC50 of 5.0 and 6.7 μg/mL. Nevertheless, AMB was more active, with EC50 values of <1.0 μg/mL. Compounds 3 and 4 showed SI ranging from 3.1 to 7.3, while compounds 5 and 6 showed a SI < 4.0. These results suggest that the lipophilicity of the molecule is essential in the activity, considering the side ring and the chroman or thiochroman system.
These results suggest that compounds 3 and 4 can be considered molecules with an antileishmania potential, L. (V) braziliensis being more sensitive than L. (V) panamensis to the action of these compounds.
None of the compounds was cytotoxic for human fibroblasts (Detroit 551) and macrophage-derived fibrocytes (huMDF), hamster kidney epithelial cells (BHK21) and macrophages derived from peripheral blood monocytes (huMDM). For all these cells the LC50 was >200 μg/mL (Table 2). As expected, DOXO showed LC50 values of <1.0 μg/mL.
In vivo antileishmanial effect of chroman-4-one hydrazones 3–6
Because L. (V) braziliensis is the species with the highest virulence and infectivity, and shows the poorest therapeutic response among Leishmania species, the tests in the animal models were made only with this Leishmania species. After experimental infection with L. (V) braziliensis hamsters were treated with each compound prepared as aqueous solution in PBS, pH 7.2 (coded 3-S, 4-S, 5-S, and 6-S) and ointments containing 4% of each chroman-4-one hydrazones in experimental ointment formulation (coded 3-O, 4-O, 5-O, and 6-O). Products were applied topically every day for 10 or 28 days for aqueous solution or ointment, respectively. The effect of the treatment was periodically monitored by measuring the diameter of the ulcer.
In vivo response was correlated to the activity observed in the in vitro studies (Table 1). Both formulations of compounds 3 and 4 showed similar results when administered as pure compounds dissolved in PBS or formulated as 4% ointment, being 3 and 4 more effective than 5 and 6. At the end of the study, treatment with compound 4-S and 4-O produced cure in 4/5 hamsters (80%), and improvement of the ulcer in the remained hamsters of these groups, with a reduction of more than 80% in the ulcer sizes (Fig. 2a, b). With compounds 3-S and 3-O healing was observed in 3/5 hamsters (60%); in the remained two hamsters (40%) of 3-S groups there were improvement (reduction in 16 and 24%) while in the 3-O group there was failure to this treatment. Treatment with intralesional MA every two days for 10 days (MA-10) produced cure in 3/5 hamsters (60%) and failure and improvement each in the remained two hamsters (Fig. 2a) while treatment with MA during 28 days cured four of five hamsters at the end of the assay and failure in one of five hamsters (20%) (Fig. 2b).
Efficacy of chroman-4-one hydrazones in a 1.5% buffer solution and ointment vs. meglumine antimoniate in a L. braziliensis- hamster model of cutaneous leishmaniasis. a Hamsters were treated topically with 100 μL of compounds in PBS (3-S, 4-S, 5-S, or 6-S) at 1.5 mg/kg/day, 10 days, topically and MA-10 (200 μg every 3 days, 10 days, intralesional). b: Hamsters were treated topically with 40 mg of the ointment formulation containing 4% (3-O, 4-O, 5-O, or 6-O) every day for 28 days or intralesional MA (200 μg every 3 days, 28 days) (MA-28). The effectiveness of each treatment was assessed, comparing the lesion sizes prior to and after treatment for everyone. The lesion size was measured before treatment (TD0), at end of treatment (TD10 or TD28) and every 15 days for three months, corresponding to the posttreatment days (PTD) 15, 30, 45, 60, 75, and 90. The outcome at the end of the study (PTD90) was recorded as a cure (epithelial healing and emergence of fur, ●); improvement (reduction of the lesion size by at least >20%, ▲); or failure (increase of the lesion size, ■)
At contrary, treatment with both 6-S and 6-O produced cure in 1/5 (20%) and 2/5 (40%), respectively (Fig. 2a, b). The rest of the hamsters in the group treated with 6-S showed a reduction of the ulcer in a 50% in one hamster and failure in the last hamster in this group and 3/5 hamsters in the group treated with 6-O. In the case of the treatment with compound 5, pure compound was slightly better than ointment since with 5-S there was cure in 20% and with 5-O no cures were observed. The other 3/5 hamsters treated with (5-O) in ointment showed an improvement, with a reduction of 46.99, 76.13, and 80.6% in the size of the lesion. The remaining hamster of this group displayed a failure with this compound (Fig. 2b).
A representative clinical outcome of the lesions of a hamster that was cured with hydrazone compounds in a buffer solution or 4% ointment is shown in the Figs 3 and 4, respectively.
Treatment progress of cutaneous leishmaniasis, caused by L. braziliensis hamsters, with hydrazones in 1.5% buffer solutions (3-S, 4-S, 5-S, or 6-S). The photos represent one hamster from each treatment group: Before the treatment (TD0); on day 10 of the treatment (TD10); and on day 90 post treatment (PTD90). The numbers in mm2 are indicative of the size of the ulcers
Treatment progress of cutaneous leishmaniasis caused by L. braziliensis hamsters, with hydrazones (3-O) and (4-O) formulated as 4% ointment. The photos represent one hamster from each treatment group: before treatment (TD0), on day 28 of the treatment (TD28); and on day 90 post treatment (PTD90). The numbers in mm2 on the right are indicative of the size of the ulcers
In short, both pharmaceutical preparations are equally effective against L. braziliensis (Figs 5 and 6), but in the case of aqueous solution, moisture probably represent a risk of microbial contamination. Therefore, almost all the compounds were active, especially compound 4, which produced a higher percentage of clinical cures, and to a lesser degree, compound 3, followed by 6. The sulfone derivative 5, produced a poor therapeutic response, because although only 1/5 hamster was cured the ulcer relapsed weeks later.
Comparison of the therapeutic response to formulated hydrazones in 1.5% aqueous solution and 4% ointment. Bars represent the percentage of hamsters with cure ( ), improvement (
), improvement ( ) and failure (
) and failure ( ) in each group of treatment. Asterisk denotes that similar results are observed in hamsters treated with 22-O and meglumine antimoniate (MA) during 28 days
) in each group of treatment. Asterisk denotes that similar results are observed in hamsters treated with 22-O and meglumine antimoniate (MA) during 28 days
Effect of the treatment on body weight. a Golden hamsters (n = 5 each group) were treated with 100 μL of each compound in PBS (3-S, 4-S, 5-S, or 6-S) at 1.5 mg/kg/day, 10 days, topically) and MA-10 (200 μg every 3 days, 10 days, intralesional). b Hamsters were treated topically with 40 mg of the ointment formulation containing 4% (3-O, 4-O, 5-O, or 6-O) every day for 28 days or intralesional MA (200 μg every 3 days, 28 days) (MA-28). The data represent the mean value ± SD of the weight in grams of the hamsters in each experimental group. p > 0.05. Body weight was measured before the treatment (TD0), at end of the treatment (TD10 or TD28) and every 15 days for 3 months, corresponding to posttreatment days (PTD) 15, 30, 45, 60, 75, and 90
Based on the findings of in vivo model in golden hamsters infected with L. (V) braziliensis, a significant posttreatment reduction was observed in lesion size in hamsters which were treated with compounds 4 and 3 compared with 5 and 6 groups. After applying the topical buffered solution or ointments on the lesions, compounds 4 and 3 apparently could pass across the subcutaneous tissues and reach the epidermal and dermal areas where infected macrophages could take up these compounds and then, were released by lysosomal degradation of the active ingredients as seen for other drugs.
In vivo toxicity of the aqueous solution and ointment hydrazones
Treatment with both formulations of hydrazone-derivative compounds 3–6 did not produce any detrimental effect on body weight in most hamsters, but rather a slight weight gain was observed in most of them. The evolution of the body weight in the treatment group is shown in Fig. 6.
Effect of chroman-4-one hydrazones 3–6 on the expression of inflammatory mediators, MCP-1, TGF-β, INF-γ, and COX-2 by huMDF
During the infection by Leishmania species, there are the expression of many different cytokines by the host, leading to chronic inflammation and tissue necrosis, which magnify the signs and symptoms of the disease. Therefore, it is necessary not only find new drugs that control the parasite but also that improve the inflammation processes. For this reason, the effect of the all compounds on the mediators of inflammation as well as cell migration were analyzed.
The selected inflammatory mediators were the Monocyte Chemotactic Protein, 1 (MCP-1), the Transforming Growth Factor-beta 1 (TGF-β1), and the Interferon gamma (IFN−γ), which are associated with Leishmania infections and, depending on the levels of expression, have been suggested as biomarkers of exacerbation or cure of Leishmania infection (TGF-β1 and IFN−γ, respectively) (Bogdan and Nathan 1993; Wyler et al. 1987). On the other hand, the enzyme, COX-2, is a mediator of the proinflammatory pathway of prostaglandins and is expressed in low concentrations of physiological stress (Kapoor et al. 2005). The levels of each of these inflammatory mediators were determined in supernatants of huDMF co-cultures at 6 and 48 h after exposure to each of the hydrazones, 3–6, at 20 μg/mL in PBS, corresponding to a concentration that is considered to be active to Leishmania amastigotes.
The main production of MCP-1 was induced by compound 5 after 6 h of incubation, with 440.2 ± 83.7 pg/mL, while for 6 and 3, the levels were 235.7 ± 112.0 and 251.6 ± 24.7 pg/mL, respectively. In turn, a smaller amount of MCP-1 was produced by compound 4, with 131.1 ± 33. 6 pg/mL. An increase in the concentration of MCP-1 was observed at 48 h, relative to that at 6 h, for all the compounds. The concentration of MCP-1 induced by 5 were 940.2 ± 29.9, 854.8 ± 106.5 pg/mL for 4, 844.0 ± 158.4 pg/mL for 6, and 624.9 ± 47.5 pg/mL for 3. In contrast to observed in the stimulated cells by the compounds, in the unstimulated control cells, the concentration of MCP-1 was much higher at 48 h than that at 6 h (996.7 ± 57.5 vs. 729.8 ± 170.4 pg/mL). While no statistically significant differences were found for any of the compounds regarding the control, all the compounds had an opposite effect to that shown by the nonstimulated cells, decreasing the production of MCP-1 at 6 h and increasing its production at 48 h (Fig. 7).
In the nonexposed cells, the concentration of TGF-β1 at 6 h of incubation was 480.6 ± 29.4 pg/mL. Similar levels were observed for cells exposed to the chroman-4-one hydrazones. Thus, for 3, the amount of TGF-β1 was 431.8 ± 23.3 pg/mL, while with compounds 4, 5, and 6, these values were 438.0 ± 3.4, 444.8 ± 54.1, and 446.3 ± 38.3 pg/mL, respectively.
After 48 h of incubation, the concentration of TGF-β1 showed slight increases for the unexposed cells and those exposed to 3, 4, and 5, except for those exposed to 6, in which the levels were decreased. In the unexposed cells, the amount of TGF-β1 was 663.6 ± 15.7 pg/mL; for 3, it was 652.0 ± 22.6 pg/mL; for 4, it was 560.0 ± 78.7 pg/mL; for 5, it was 628.8 ± 3.4 pg/mL; and for 6, it was 557.1 ± 62.3 pg/mL. No statistically significant differences were found between the levels of TGF-β1 in the stimulated cells, relative to the control of nonstimulated cells. For TGF-β1, all the compounds increased the production of TGF-β1 at 48 h, relative to that at 6 h, except for compound 24, which inhibited the production of TGF-β1 (Fig. 7).
On the other hand, the concentration of INF-γ at 6 h of incubation in nonexposed cells was 74.5 ± 5.4 pg/mL; for 3, it was 140.3 ± 76.0 pg/mL; for the 4, it was 68.5 ± 6.2 pg/mL; for 5, it was 90.3 ± 6.2 pg/mL; and for 6, it was 64.4 ± 9.6 pg/mL (Fig. 8). The concentration of INF-γ at 48 h of incubation for the control was 65.5 ± 9.7 pg/mL; for compound 3, it corresponded to 77.9 ± 34.2 pg/mL; for 4, it was 151.3 ± 8.0 pg/mL; for 5, it was 135.4 ± 23.6 pg/mL; and for compound 6, it was 95.5 ± 23.5 pg/mL. While compounds 4, 5, and 6 increased the levels of IFN−γ at 48 h, relative to that at 6 h, the levels of the said cytokine decreased in response to exposure to compound 3, and in the unexposed cells, the levels showed no change.
Light microscope images of the wound closure in vitro using a confluent monolayer of Detroit 551 fibroblasts. Microphotographs show one representative experiment of the cell migration into the created wound area in response to the treatment. (left) Wound area at 0 h (a) and after 8 h (b) or 16 h (c), for the untreated control (−C) (set to 0%), positive control (+C), and 20 μg/mL of 3, 4, 5, or 6. The wound closure (indicated in as %) was normalized to the untreated control
After 6 h of incubation, some compounds induced COX-2 concentrations higher than those found in the control of nonexposed cells. Thus, in the absence of compounds, the COX-2 levels were 0.54 ± 0.4 μM (Fig. 8), and for compound 5, they were 2.25 ± 1.1 μM. This result was statistically significant, relative to the control. On the other hand, for compound 6, the levels were 1.4 ± 0.2 μM, and for 3, they were 1.1 ± 0.4 μM. With 4, the levels were similar to the control. After 48 h of incubation, the activity of the enzyme was maintained at levels similar to those presented at 6 h of incubation for control (0.6 ± 0.1 μM), as well as for cells exposed to 4 (0.62 ± 0.4 μM), 5 (0.522 ± 0.2 μM), and 6 (0.516 ± 0.0 μM). Only compound 3 (0.174 ± 0.6 μM) significantly inhibited COX-2 activity, showing that the concentrations of this enzyme are well below the concentration of non-stimulated cells.
To quantify the effect of the compounds, the percentage of increase or decrease in the levels of MCP-1, TGF-β1, IFN−γ, and COX-2 in the cells exposed to each compound, with respect to the exposed cells, was calculated. As shown in Table 3, at 6 h all the compounds decreased the levels of MCP-1, in percentages ranging between 55 and 86%, with compound 4 producing the greatest decrease. On the contrary, at 48 h, all the compounds induced a moderate increase in the levels of MCP-1, with percentages between 15 and 28%, except for compound 3, which produced a decrease of 14% in the levels of MCP-1. For TGF-β1, all the compounds induced a slight decrease in the levels of this cytokine, with values between 1 and 16%. On the other hand, for INF−γ, at 6 h, compounds 3 and 5 increased the INF-γ production by 21% and 88%, respectively, with respect to the values without stimulus (Table 3); At contrary, at 48 h, all the compounds increased the production of IFN−γ, indicating that 4 and 5 will increase the levels by more than 100%, with respect to the levels in the absence of the compounds (Table 3). Compound 4 inhibited the production of COX-2 by 24% at 6 h, but on the other hand, the other products, 3, 5, and 6, increased the levels, especially 5, with an increase of more than 100% (Table 3). At 48 h, compound 4 slightly increased the levels of COX-2, while the other compounds decreased it. However, although the COX-2 levels try to increase at 48 h in cells stimulated with compound 4, this increase is very slight and therefore is not significant. The preferential increase of COX-2, observed after exposure to compound 4, confers to this compound anti-inflammatory properties that are very useful for the resolution of the inflammatory process, occurring during active CL.
Compound 4 seems to have an impact on the anti-inflammatory response by inducing an increase in the levels of IFN−γ at 48 h post treatment, and the fact that it has activity against the Leishmania species places it as a candidate as an antileishmanial agent. In addition, it has a potential as a scarring factor, favoring the migration of fibroblasts, with a closing of the gap similar to that of the positive control. Compounds 3, 5, and 6 have the capacity to stimulate the production of the COX-2 at 6 h post treatment, and 4, at 48 h, which could favor the production of the derivatives of arachidonic acid, such as prostaglandin E2, enhancing the inflammatory response which may potentiate the final cure (Kalinski 2012).
With the increase in the levels of IFN−γ, induced by compound 4, it could be deduced that the mechanism by which this compound acts against Leishmania parasite could be through the activation of macrophages, which would eventually lead to the death of the parasite at the intracellular level. This would also explain the effectiveness of the compound in intracellular amastigotes and in infected hamsters. These results also correlate with the decrease in the production levels of TGF-β1, a cytokine that modulates macrophage activation, favoring the survival of Leishmania and therefore the development of CL (Bogdan and Nathan 1993) but also treatment failure (Elmekki et al. 2016). In turn, compound 4 increases the levels of COX-2, so it could be said to have an anti-inflammatory potential (Das et al. 2014). The other two compounds, 5 and 6, do not have significant activity in relation to the parasite, as already mentioned before, and they also do not decrease the enzymatic levels of COX-2. However, they have an anti-inflammatory potential by inducing the production of MCP-1 and INF-γ, so they can be used as adjuvants with treatments already available and be part of a combined antileishmanial therapy.
Effect of chroman-4-one hydrazones 3–6 on the stimulation of the healing process by fibroblast migration
In cells unexposed to the stimulus, a closing of the gap was observed in 18% (Fig. 8), while in the cells incubated in the presence of DMEM and 20% FBS (+C), the migration of the cells produced a reduction of the gap in 80%. Culturing fibroblasts in the presence of 4 induced cell migration, in such a way that the gap was reduced by 78%, whereas with compounds 3, 5, and 6, the gap was reduced by 40%.
Reepithelialization after cutaneous injury is a complex and multifaceted process that incorporates numerous cellular components interacting in a myriad of pathways. One of the most crucial aspects of this process is the initiation of fibroblast migration to fill the wound bed. The chroman-4-one hydrazones, especially compound 4 favored the migration of huMDF reducing the gap in the cell monolayer. These results suggest that these hydrazones could have potential as healing agents. This is the first report of this type of biological effect with this class of compounds.
Chromosome aberration—genotoxicity effect
Both compounds did not exhibit chromosomal aberrations at any of the tested concentrations, compared with the negative control (Table 4). No statistically significant differences between the negative control and 3 or 4 were found (p = 0.527).
Because genotoxicity analysis based only on chromosomal aberration studies and with low compound concentrations is not sensitive to genotoxicity and mutagenicity, other tests, such as Comet, Ames and Vitotox, which would be more sensitive, should be performed to identify the significant dose-dependent genotoxicity and mutagenicity of 3 or 4.
Our findings demonstrated that from molecules with relatively simple structure, and through chemical transformations and bioguided leishmanicidal in vitro tests, several active chroman analogs could be obtained. Moreover, transformation into hydrazones, optimized their antiparasite activity. Two of the four chroman-4-one hydrazone derivatives obtained, the benzoic acid, 2-(2,3-dihydro-4H-1-benzothiopyran-4-ylidene) hydrazide (3), and the benzoic acid, 2-(2,3-dihydro-4H-1-benzopyran-4-ylidene) hydrazide (4), caused high cure rates when were applied topically as a 4% ointment in a L. braziliensis hamster model of CL. Although these efficacy was similar when administered as buffered solution, the ointment permits a high adherence in the skin lesion, with long drug delivery in addition to other beneficial effects, like emollient, occlusive and antiseptic effects. At contrary, the moisture in the wound can affect the healing process and increase the risk of microbial contamination.
The benzoic acid, 2-(2,3-dihydro-1,1-dioxide-4H-1-benzothiopyran-4-ylidene) hydrazide (5) was less effective than 3 and 4, and compound 4-pyridinecarboxylic acid, 2-(4H-1-benzopyran-4-ylidene) hydrazide (6), was practically inactive.
On the other hand, the antileishmanial potential of compounds 4 and 3 is complemented by their healing property, since they also modulate the production of inflammatory mediators involved in the activation of the microbicidal response of the macrophage. The early production of IFN−γ and decreasing of TGF−β1 levels may favor the resolution of the disease. Besides, these compounds lack genotoxic and cytotoxic effects.
Conclusions
In this work is reported for first time new synthesized compounds having combined antileishmanial, anti-inflammatory and healing activities. The overall results obtained with hydrazone-derivative compounds 4 and 3 demonstrate at least qualitatively comparable with (or even somewhat better than) MA, the drug used against this disease. The strategy used here could be postulated as a suitable alternative in the search for new drugs to treat CL. These compounds can be produced from simple chemical precursors such as phenol and thiophenol in high yields, which may provide large amounts to further assays, to evaluate their efficacy in controlled clinical trials in human and canine CL.
References
Alvar J, Vélez ID, Bern C, Herrero M, Desjeux P, Cano J, Jannin J, den Boer M, WHO Leishmaniasis Control Team (2012) Leishmaniasis worldwide and global estimates of its incidence PLoS ONE 7:e35671. https://doi.org/10.1371/journal.pone.0035671
Bogdan C, Nathan C (1993) Modulation of macrophage function by transforming growth factor beta, interleukin-4, and interleukin-10. Ann N Y Acad Sci 685:713–739. https://doi.org/10.1111/j.1749-6632.1993.tb35934.x
Borges F, Roleira F, Milhazes N, Santana L, Uriarte E (2005) Simple coumarins and analogues in medicinal chemistry: occurrence, synthesis and biological activity. Curr Med Chem 12:887–916. https://doi.org/10.2174/0929867053507315
Cywin CL, Firestone RA, McNeil DW, Grygon CA, Crane KM, White DM, Kinkade PR, Hopkins JL, Davidson W, Labadia ME, Wildeson J, Morelock MM, Peterson JD, Raymond EL, Brown ML, Spero DM (2003) The design of potent hydrazones and disulfides as cathepsin S inhibitors. Bioorg Med Chem 6:733–740. https://doi.org/10.1016/S0968-0896(02)00468-6
Den Boer M, Argaw D, Jannin J, Alvar J (2011) Leishmaniasis impact and treatment access. Clin Microbiol Infect 17:1471–1477. https://doi.org/10.1111/j.1469-0691.2011.03635.x
Das P, De T, Chakraborti T (2014) Leishmania donovani secretory serine protease alters macrophage inflammatory response via COX-2 mediated PGE-2 production. Indian J Biochem Biophys 51:542–551. http://nopr.niscair.res.in/handle/123456789/30506
Desai PV, Patny A, Sabnis Y, Tekwani B, Gut J, Rosenthal P, Shivastava A, Avery M (2004) Identification of novel parasitic cysteine protease inhibitors using virtual screening. 1. The ChemBridge database. J Med Chem 47:6609–6615. https://doi.org/10.1021/jm0493717
Elmekki MA, Elhassan MM, Ozbak HA, Mukhtar MM (2016) Elevated TGF-beta levels in drug-resistant visceral leishmaniasis. Ann Saudi Med 36:73–77. https://doi.org/10.5144/0256-4947.2016.7310.5144/0256-4947.2016.73
Finney JD (1978) Statistical method in biological assay, 3rd edn. Charles Griffin & Co, London, UK, p 508. https://doi.org/10.1002/bimj.4710210714
Friden-Saxin M, Seifert T, Ryden Landergren M, Suuronen T, Lahtela-Kakkonen M, Jarho EM, Luthman K (2012) Synthesis and evaluation of substituted chroman-4-one and chromone derivatives as sirtuin 2-selective Iinhibitors. J Med Chem 55:7104–7113. https://doi.org/10.1021/jm3005288
Gaspar A, Matos MJ, Garrido J, Uriarte E, Borges F (2014) Chromone: a valid scaffold in medicinal chemistry. Chem Rev 114:4960–4992. https://doi.org/10.1021/cr400265z
Gaspar A, Mohabbati M, Cagide F, Razzaghi-Asl N, Miri R, Firuzi O, Borges F (2019) Searching for new cytotoxic agents based on chromen-4-one and chromane-2,4-dione scaffolds. Res Pharma Sci 14:74–83. https://doi.org/10.4103/1735-5362.251855
Kalinski P (2012) Regulation of immune responses by prostaglandin E2. J Immunol 1(188):21–28. https://doi.org/10.4049/jimmunol.1101029
Kanbe Y, Kim MH, Nishimoto M, Ohtake Y, Kato N, Tsunenari T, Taniguchi K, Ohizumi I, Kaiho S, Morikawa K, Jo JC, Lim HS, Kim HY (2006) Discovery of thiochroman and chroman derivatives as pure antiestrogens and their structure-activity relationship. Bioorg Med Chem 14:4803–4819. https://doi.org/10.1016/j.bmc.2006.03.020
Kapoor M, Shaw O, Appleton I (2005) Possible anti-inflammatory role of COX-2-derived prostaglandins: implications for inflammation research. Curr Opin Investig Drugs 6:461–466
Limoncu ME, Balcioğlu IC, Yereli K, Ozbel Y, Ozbilgin A (1997) A new experimental in vitro culture medium for cultivation of Leishmania species. J Clin Microbiol 35(9):2430–2431
Mathur S, Hoskins C (2017) Drug development: Lessons from nature. Biomed Rep 6:612–614. https://doi.org/10.3892/br.2017.909
Mesa C, Blandón GA, Muñoz DL, Muskus CE, Flórez AF, Ochoa R, Vélez ID, Robledo SM (2015) In silico screening of potential drug with anti-leishmanial activity and validation of their activity by in vitro and in vivo studies. J Chem Chem Eng 9:375–402. https://doi.org/10.17265/1934-7375/2015.06.002
Montoya A, Daza A, Muñoz D, Ríos K, Taylor V, Cedeño D, Vélez ID, Echeverri F, Robledo SM (2015) Development of a novel formulation with hypericin to treat cutaneous leishmaniasis based on photodynamic therapy in in vitro and in vivo studies. Antimicrob Agents Chemother 59:5804–5813. https://doi.org/10.1128/AAC.00545-15
Muñoz DL, Cardona D, Cardona A, Carrillo LM, Quiñones W, Echeverri F, Vélez ID, Robledo SM (2006) Efecto de hidrazonas sobre amastigotes intracelulares de Leishmania panamensis y una proteasa de cisteína parasitaria. Vitae 13:5–12
Nicolaou KC, Pfefferkorn JA, Roecker AJ, Cao G-Q, Barluenga S, Mitchell HJ (2000) Natural Product-like combinatorial libraries based on privileged structures. 1. General principles and solid-phase synthesis of benzopyrans. J Am Chem Soc 122:9939–9953. https://doi.org/10.1021/ja002033k
OECD (2016) Test No. 473: in vitro mammalian chromosomal aberration test, OECD guidelines for the testing of chemicals, section 4. OECD Publishing, Paris. https://doi.org/10.1787/9789264264649-en
Pulido SA, Muñoz DL, Restrepo AM, Mesa CV, Alzate JF, Vélez ID, Robledo SM (2012) Improvement of the green fluorescent protein reporter system in Leishmania spp. for the in vitro and in vivo screening of anti-leishmanial drugs. Acta Trop 122:36–45. https://doi.org/10.1016/j.actatropica.2011.11.015.
Ramendra P, Vishnu P, Ram J (2014) Natural and synthetic chromenes, fused chromenes, and versatility of dihydrobenzo[h]chromenes in organic synthesis. Chem Rev 114:10476–10526. https://doi.org/10.1021/cr500075s
Rawat P, Manaswita Verma S (2016) Design and synthesis of chroman derivatives with dual anti-breast cancer and antiepileptic activities. Drug Des Devel Ther 10:2779–2788. https://doi.org/10.2147/DDDT.S111266
Robledo S, Wozencraft A, Valencia AZ, Saravia N (1994) Human monocyte infection by Leishmania (Viannia) panamensis. Role of complement receptors and correlation of susceptibility in vitro with clinical phenotype. J Immunol 152:1265–1276
Robledo SM, Carrillo LM, Daza A, Restrepo AM, Muñoz DL, Tobón J, Murillo JD, López A, Ríos C, Mesa CV, Upegui YA, Valencia-Tobón A, Mondragón-Shem K, Rodríguez B, Vélez ID (2012) Cutaneous leishmaniasis in the dorsal skin of hamsters: a useful model for the screening of antileishmanial drugs. J Vis Exp (62). 3533. https://doi.org/10.3791/3533
Saengchantara ST, Wallace TW (1986) Chromanols, chromanones, and chromones. Nat Prod Rep 3:465–475. https://doi.org/10.1039/NP9860300465
Sharma SK, Kumar S, Chand K, Kathuria A, Gupta A, Jain R (2011) An update on natural occurrence and biological activity of chromones. Curr Med Chem 18:3825–3852. https://doi.org/10.2174/092986711803414359
Tsatsop RK, Djiobie GE, Regonne K, Bama VS, Mbawala A, Benoît NM (2017) Optimization of rheological properties in the formulation of an ointment base from natural ingredients. Inter J Sci Tech Res 2017(6):113–121
WHO Expert Committee on the Control of the Leishmaniases and World Health Organization (2010) Control of the leishmaniases: report of a meeting of the WHO Expert Commitee on the Control of Leishmaniases. World Health Organization, Geneva, 22–26 March. http://www.who.int/iris/handle/10665/44412
Wyler DJ, Beller DI, Sypek JP (1987) Macrophage activation for antileishmanial defense by an apparently novel mechanism. J Immunol 138:1246–1249
Acknowledgements
This work was a cooperative activity within the Temporal Union “Estrategia Integral para el control de la Leishmaniasis en Colombia” (EICOLEISH-UT) with financial support from Colciencias (CT695-2014). Authors also thanks to I. Ortiz, Facultad de Salud, Universidad Pontificia Bolivariana for technical support with the genotoxicity test.
Author contributions
FE and SMR devised the study and wrote the paper. WQ, GE, FT, and RA performed the chemical analyses. YU, KR, IDV, and SMR performed the in vitro and in vivo experiments.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Upegui, Y., Rios, K., Quiñones, W. et al. Chroman-4-one hydrazones derivatives: synthesis, characterization, and in vitro and in vivo antileishmanial effects. Med Chem Res 28, 2184–2199 (2019). https://doi.org/10.1007/s00044-019-02446-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-019-02446-x