Abstract
Objectives
Turkey is facing increasing rates of cardiovascular disease (CVD). The study is designed to meet the growing need to obtain information about the recent status and trends of CVD risk factors and their impact on mortality.
Methods
Balcova heart study (BHS) is a prospective cohort study, focusing on reducing the CVD risk factors of people over 30 years old living in Balcova District, Izmir, Turkey. Information about risk factors, anthropometric and biochemical measurements was collected in community centers. Interventions were planned, based on the 10-year coronary heart disease (CHD) risk and lifestyle characteristics with the collaboration of university and municipality.
Results
Mean age of the 16,080 participants was 52 years. The percentage of current smoking was 41.6 in men and 31.1 in women. One-third of the men were physically inactive. Hypertension was reported as 25% in men and 33% in women.
Conclusions
The project is unique for being the first community-based cohort on CVD risk factors in a Turkish setting. This project will have a valuable contribution on not only determining CVD risks, but also incorporating interventions for prevention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The global burden of non-communicable diseases has been increasing rapidly over the years and started to be a major concern for low- and middle-income countries. Mainly cardiovascular diseases, diabetes, cancers, and chronic respiratory diseases caused an estimated 35 million deaths in 2005. Deaths related to these causes are projected to increase by 17% over the next 10 years (WHO 2005). Since these deaths are predominantly preventable, a huge amount of effort is being allocated for the prevention and control. Mainly high-income countries have started programs to reduce the burden in the past years (WHO 2005). World Health Organization (WHO) has prepared an action plan to guide member states (WHO 2008). CVD is the main cause of death in the European Region of WHO, nearly half (48%) of all deaths are from CVD (54% of deaths in women and 43% of deaths in men) (WHO 2004).
One of the most reliable sources for CVD morbidity data is the WHO Monitoring Trends and Determinants in Cardiovascular Disease (MONICA) project (WHO 2003). Researchers concluded that coronary-event rates contributed two-third and case fatality to one-third of the decrease in CVD mortality (Tunstall Pedoe 1999). Using data from this project, Rayner et al. (2009) estimated that in Europe 23% of all disability adjusted life years (DALYs) lost are because of CVD—more than any other cause.
According to Turkish Statistical Institute (TurkStat), 40% of deaths over 35 years old were attributed to CVD in 2008 in Turkey, which are based on only urban area mortality data (TurkStat 2008). In fact, National Burden of Disease and Cost Effectiveness Study (NBD-CE) covered both rural and urban area reports and predicted that 47.7% of deaths were caused by CVD (52.3% of deaths in women and 43.9% of deaths in men) in 2004. In the risk factor analysis, it was estimated that controlling high systolic blood pressure, prevention of smoking and high cholesterol would prevent 212,196 deaths in Turkey (Ministry of Health-MoH 2004). It has been estimated that the aging population and high prevalence of CVD risk factors including hypertension 31.8% (Altun et al. 2005), hyperlipidemia 28–35% (Mahley et al. 1995), diabetes 11.9% (Satman et al. 2002), smoking 33.4% (TurkStat 2006), and obesity 21.9% (Yumuk 2005) will increase the risk of death from CVD by 2.7-fold in men and 1.8-fold in women by 2030 in Turkey (MoH 2004).
Turkish Ministry of Health also prepared an action plan to prevent and control cardiovascular diseases. This plan aimed to control smoking through legislation and mass media campaigns. Preventing obesity, ensuring healthy nutrition, and positive effects of physical activity were other targets of the Strategic Plan (MoH 2009).
There is substantial evidence that lifestyle interventions can reduce CVD deaths, and prolong life for CVD patients (Graham et al. 2007). In the recent systematic review of community interventions for the prevention of CVD, it was concluded that these interventions achieved favorable changes in overall CVD risk (Pennant et al. 2010).
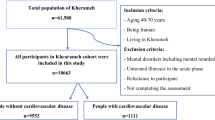
For an effective control of CVD, a comprehensive program is needed toward healthy people and high-risk populations, as well as already ill individuals. With this insight, Balcova heart study (BHS) was designed to reduce and prevent CVD, to address the inequalities in social determinants, and to reduce the disparities in risk factors and develop health policy recommendations based on evidence. The logic model of the project is shown in Fig. 1.
The logic model of Balcova heart study, Turkey, 2007 (adapted from Kark (1989))
Methods
Study population
Balcova is one of the central districts of Izmir city on the Aegean coast of Turkey. The total population of Izmir is ~3.8 million with considerable number of immigrants from the Eastern regions of Turkey. Balcova District is where the Dokuz Eylul University (DEU) Medical Campus is located. The target population of the project is the residents of Balcova District over the age of 30 without sampling, which was a total of 36,187 people (TurkStat 2006). Every house within the borders of district was visited at least three times and an invitation note was sent if household could not be reached during visits.
Organizational structure
The project is a joint effort of Dokuz Eylul University Medical School and Balcova District Municipality. The project is lead by the Department of Public Health and there are three committees for the operation of the project, namely Executive, Scientific and Administrative committees, and a Field Coordination Unit. The Executive Committee comprises five members from the Department of Public Health and the Municipality, headed by the mayor of Balcova District. The scientific committee consists of the faculty members of the Public Health Department, members from Cardiology and Biochemistry departments. The project is jointly funded by the Balcova Municipality and DEU Research Fund.
Implementation points
Balcova Municipality has set up Community Centers to develop the community members through skills courses on arts and crafts, computer, and language. These centers created a useful setting with its friendly environment for the project. Although they were not designed as health facilities, they were organized to welcome individuals for their biochemical and physical measurements throughout the project.
First, a baseline cross-sectional study was conducted to determine the coronary heart disease (CHD) risk status of the individuals according to Framingham risk equation (Wilson 1998). The population was then categorized as: individuals who already have CHD, high-risk individuals, and healthy individuals. Population-based intervention programs planned to be implemented to reduce incidence for the majority of individuals, not only those with high risk (Rose 1992). Three areas of intervention were planned: reducing smoking or prevention of starting smoking, increasing physical activity and developing healthy eating habits.
The individuals in the cohort, who already have CHD, will be followed-up to reduce mortality from CHD-related causes. They will be given counseling to change into healthier lifestyle and habits and will be directed for appropriate treatment options if necessary.
The midterm outcomes of the project will be the increase in the number of people who are physically active, decrease in the prevalence of diabetes, hypertension, obesity, as well as decrease in smoking and blood lipid levels. The main outcome would be the decrease in CVD incidence and mortality.
Time frame
This project was planned as a 10-year follow-up. It is anticipated that the project continues much longer than that. The baseline study which has started in Oct 2007 was completed in May 2009. In total, 16,080 interviews were conducted and 12,915 blood samples were collected. Participants of this baseline survey will consist of the largest population cohort study for chronic diseases in Turkey.
Preparation activities
The preparation activities started 4 months before the signing of the protocol between the Medical School and the Municipality. The two parties have met to decide on the goals, the methods, the work plan, division of tasks, and organization chart. The community center workers were given information on the aims and background of the project. Interviewers were trained on communication skills, basics of CVD diseases, and a training video film was also prepared by our department including examples from real life scenarios.
Activities were planned to raise the awareness of the community in the district by wall charts and newsletters sent to houses. Additionally, a TV commercial was prepared to be shown on the local TV.
Data collection
The questionnaire included questions on the demographics, socioeconomic status, and self-assessed health of the participants. There were two types of questionnaires used in this project: the short version including questions on the main risk factors such as smoking, diet and physical activity and the long version which included these risk factors more in detail. The interviews were conducted at homes after getting an informed consent. After their interview, the participants were given an appointment to visit their community center for physical and biochemical measurements.
The medical history section of the questionnaire was filled by a physician when the participant came to the community center. Daily used medications by individuals were recorded. Standard blood pressure measurements were taken by skilled physicians and nurses by using a validated mercury sphygmomanometer from patients at rest (5–10 min) in the sitting position as recommended by the guidelines (Alpert et al. 2006). Blood pressures of the participants were taken twice and the mean values were recorded. Hypertension was defined as a systolic blood pressure of ≥140 mmHg and/or a diastolic blood pressure of ≥90 mmHg or use of any antihypertensive drugs (Mancia et al. 2007). Anthropometric measurements (height, weight, waist, and hip circumference) were taken by the community center volunteers who were also trained and standardized by the field teams. Weight was measured, while subjects were minimally clothed without shoes, using digital scales. Waist and hip circumference was measured with a non-stretchable standard tape as defined in the measurements protocol of the project. “High-risk” waist circumference was defined as a waist circumference of >102 cm in men and >88 cm in women (Lean et al. 1995). Height was measured in a standing position without shoes, using a tape meter with shoulders in normal alignment. Body mass index (BMI) was calculated as weight (kg) divided by square of height (m2). Obesity was defined as BMI of 30 and above (WHO 2004). Blood samples were taken after at least 8 h of overnight fasting between 8:30 and 10:30 a.m. The blood samples were transported to DEU Hospital Laboratory, and total cholesterol (TC), low-density lipoprotein cholesterol (LDL), high-density lipoprotein cholesterol (HDL), triglyceride (TG), and fasting blood sugar tests were carried out with Abbott Architect c16000 system on the day of blood collection. After the biochemical analysis, remaining sera were frozen and stored in the form of two aliquots at −80°C for further analysis when needed. To increase the participation rates especially in the individuals who are working during week, blood sampling and interviews were conducted on Sundays.
Individuals were classified as moderately active if they undertake activity on at least 5 days/week and do at least 30 min of moderate-intensity activity and/or walking (Craig et al. 2003). Smoking status was defined as never smoker/current smoker/ex-smoker. Current smokers were those reported smoking every day or some days at the time of interview. Nonsmokers were defined as those who never had smoked. Ex-smokers were those who reported smoking during their lifetime, but currently did not smoke. At least five portions of fruit and vegetable intake was defined as the limit for healthy nutrition (WHO 1990).
The Heart Risk Report Card was specially developed for the project (Online resource 1). Report provided information about patients’ 10-year risk of developing CHD, identified risk factors, medical history, and lifestyle factors. The report was generated after combining the data from the questionnaire and the values from biochemical measurements. CHD risk was estimated using the Framingham risk equation. Data on age, gender, smoking status, total cholesterol, high-density lipoprotein, blood pressure, and diagnosis of diabetes were used to estimate the risk of developing CHD in the following 10 years. Individuals were grouped based on risk scores <10% as low, 10–20% as medium and >20% as high risk (Wilson 1998). Report was designed as a single page for practical usage. The report gave information about the current status of the modifiable risk factors and the target levels as recommended in guidelines. Absolute risk of a patient, absolute risk of a “normal” patient of the same age and sex, and absolute risk of an individual with minimum risk were estimated and presented in the report. We used Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (NCEP-ATPIII 2002), Joint National Committee (Lenfant et al. 2003), American Diabetes Association (ADA 2010) recommendations for thresholds. Alongside giving target levels for both lifestyle and biochemical risk factors by formulizing data, we made recommendations based on individuals CHD risk and medical history. For example, if an individual had a diabetes mellitus (DM) history, or CHD risk >20%, or have a CHD history, his target low-density lipoprotein (LDL level was defined as <100 mg/dl, otherwise target was (LDL) <130 mg/dl. Report card was given to all individuals with 10 min of counseling regarding healthy diet, smoking cessation, and regular physical activity by the doctors. Patients were referred to a hospital when necessary.
Data management
A database was created to enter the data from different units on a web-based design. Data collected through the interview from the laboratory and physical measurements would be entered and stored in the same database, as well as the follow-up information. A report on heart disease risk was prepared by combining the information at the server. Data were available through a remotely accessible web browser. All study data are managed through a secure server at the DEU, and it can only be used by authorized members of the project.
Community interventions and follow-up
Community interventions were planned specifically targeting three main risk factors: smoking, unhealthy diet, and physical inactivity. Various interventions for high-risk groups are diet and PA intervention for the individuals with impaired glucose, where those individuals will be contacted and called to participate in the program. Similarly, PA intervention will be conducted for the population with medium cardiovascular risk. A smoking cessation clinic will start and invite the participants with medium- and high-risk primarily, as well as serving the general community. The clinic will also plan activities for prevention of starting smoking. There will be other interventions throughout the course of the project targeted for specific risk groups and the community in general.
Participants will be followed-up for important health events and death in a schedule according to their risk category. These follow-ups will be done by a physician and a nurse in the project coordination unit at the municipality. The people with medium- and high-risk will be given appropriate counseling to reduce or at least maintain their risk status. They will be steered toward various interventions according to their risk factor.
Evaluation of the project
The project will be evaluated using program review procedure. Data will be collected on program activities, inputs, and outputs. Major outputs of the project are incidence and mortality rates of CVD. The baseline survey will be repeated in the year 2012 and 2017 on selected population samples to evaluate the changes in risk factor trends. The baseline survey population will also be followed-up to estimate incidence and mortality rates of non-communicable diseases including CHD, stroke, and cancer. Morbidity data will be identified by means of the social security records, hospital registries and questionnaires on occurrence of MI, stroke, and cancer. In Turkey, family physicians and municipal health units and hospitals in each district submit death certificates to the Provincial Health Directorate (PHD) and TurkStat. Causes of death are coded based on ICD-10. The ICD related with CHD (I20–25, I46–50, Z95) and stroke (G45–46, I60–69) will be tracked for mortality and morbidity data. We will validate the cause of death by checking the hospital records and a verbal autopsy questionnaire, which will be applied to family members. We will also evaluate the observed CHD events with the ones predicted by Framingham risk equation at the 5th and 10th year of the project. Inequalities in mortality and distribution of risk factors in different socio-economic groups will be evaluated.
Dokuz Eylul University Ethical Committee has reviewed and approved the study protocol 337/2007. Verbal and written consent was obtained from all participants.
Statistical analysis
SPSS for Windows (version 15.0; SPSS Inc., Chicago, IL, USA) was used for data analysis. For comparison of baseline characteristics among men and women, t test was used for continuous variables. Results were expressed as means ± standard errors or as percentages.
Results
In this section, characteristics of the study population and some of the baseline behavioral variables were presented. Of these 16,080 people participated in the study, 34.5% were men and mean age was 52 years. Participation rates were lower in men and in the younger age groups. Majority of the population were primary school graduates, but more men had higher education than women. Most of the population was covered by health insurance; the uninsured population was 7.6% in men and 6.9% in women (Table 1).
Some of the key lifestyle characteristics of the population are given in Table 2. Current smoking was quite high among both men and women (41.6, 31.1%, respectively). Almost one-third of the men were physically inactive compared with 14% of the women. One of the main elements of Turkish diet is white bread daily prepared in the bakeries. It was seen that there has been a shift to wholemeal bread in a considerable percent of the population. Olive oil and vegetables and fruits were also frequently consumed reflecting the Mediterranean style of nutrition in accordance with the geographical location of the study.
When participants were asked about their medical conditions that were either diagnosed by a doctor or that they were using a medication for hypertension was reported 25% in men and 33% in women, and the second prevalent condition was hypercholesterolemia (Table 3).
The biochemical and anthropometric measurements of population were presented in Table 4.
While TG, systolic and diastolic blood pressure, waist circumference and waist to hip ratio, and Framingham risk score values were higher in men than in women; TC, HDL-C, BMI, and hip circumference were significantly higher in women than in men. There was not a significant difference in mean LDL-C value between men and women.
Discussion
The study describes the BHS brought to life with the University and local municipality collaboration. This is a community-based CVD control programme that uses primary prevention interventions for the whole population and high-risk individuals. As most of the prospective studies in cardiovascular disease epidemiology, our study has been inspired from the Framingham Heart Study (Oppenheimer 2005) and the North Karelia Project (Pekka Puska 2002). Both projects contributed to the knowledge base of CVD and also set examples in community partnerships for a long-term success (Oppenheimer 2005).
Balcova is located at the western and more developed part of Turkey with a population of higher level of education and lower uninsurance. Although olive oil and vegetables and fruits were frequently consumed and physical inactivity was lower compared with former studies (MoH 2004), the smoking rates of women and mean blood lipid levels in both genders were higher than Turkish average (Mahley et al. 1995; Onat 2001). BMI values were also higher compared with results of nationwide studies (Sanisoglu et al. 2006; Satman et al.2002; Oğuz et al. 2008; MoH 2010). These findings suggest that there is a room for community-based health promoting interventions targeting mainly life style change and healthy diet to decrease long-term CVD risks in Balcova.
One of the strengths of this project is the timing of this study being in accordance with raised public awareness that cardiovascular disease is a widespread illness in the adult age group and also the leading mortality cause. However, people are not aware of their individual risk factors and their cardiovascular disease risk. Through this project, all participants will recognize their risk status and that this can be changed. This was also the first time for risk-based approach and a heart risk report card was used for treatment recommendations in Turkey.
There is also a supportive environment for some of the major interventions such as smoking cessation. Turkey has signed the Framework of Tobacco Convention and has enforced one of the most powerful legislations in the world for banning smoking in all public places, including bars, traditional coffee houses, and restaurants since 2009 (WHO 2009). Balcova Municipality has been building sports facilities in the district, where citizens can do physical exercise free of charge. There are also exercise equipments at the parks and bicycle roads were built along the coast line of the district.
This study gained a wide recognition and support from the public health community of the country. We have won the “excellent presentation” award in the National Public Health Congress and the mayor of Balcova Municipality has won the “Best Administrator in Supporting Public Health” award of the Turkish Public Health Association.
Main limitation of the project is lack of secure funding for an extended period. Most of the personnel come from the university. In fact, there is a considerable need for permanent staff for the interventions and follow-up. The health system in Turkey is in a transformation process. Therefore, a good collaboration with family physicians in the district has not been established yet, which would be a great support, especially for follow-up activities. Another major limitation of this project is the lack of a control group. Best evidence can be obtained from controlled studies; however, it is also a quite expensive design. Finding a comparable population within a close proximity which will not as well be contaminated by the interventions was quite impossible. Nevertheless, it is planned to use mortality and morbidity data for Izmir in the evaluation of the follow-up results.
The participation rate was rather low (44%), which might limit the generalization of our findings. However, low participation is typical of surveys and participation rates are declining worldwide. The magnitude of the nonparticipation bias is not proportional to the percentage of nonparticipants (Galea and Tracy 2007) and a study on representativeness observed that people with risky behaviors participated in the same proportions as people without risk factors (Taylor et al. 2006). In our case, some of the individuals with chronic diseases such as CHD or DM did not want to participate in project as they were already under control by their health facility. Participation rates were lower among men because most of them were working during blood sampling hours.
Loss to follow-up is the major concern of the cohort studies. Our district has a relatively high rate of migration in the younger adults (<45); however, the older age groups are more stable. The use of national ID numbers will make it possible to track individuals for their changing addresses. The neighborhood networks of the municipality will also be an important support in the follow-up of the population.
CHD risk estimations were based on Framingham risk equations and it can be argued whether it is suitable for Turkish settings. According to the only cohort (TEKHARF) on cardiovascular diseases in Turkey (Onat et al. 2010), Framingham risk score accurately predicted the low risk groups, but underestimated the ratio of high-risk individuals. Authors think that the variables such as obesity not included in Framingham risk scoring system caused this difference. We also anticipate validating or creating our own CVD risk scoring system in the future.
As most of the intervention studies are mostly conducted in high-income countries of the Western Europe and North America, our study may set an example for countries which are similar in economic and cultural aspects. The low-budget interventions could be accomplished with the participation of volunteers. Local municipality administrations could be encouraged to be engaged in health promotion activities.
The most prominent feature of this project is being the first community cohort on CVD in Turkey and it also incorporates interventions for controlling and preventing the CVD. Furthermore, it is designed with the collaboration of a University and a local municipality, where in Turkey health care and health promotion are under the responsibility of Ministry of Health. This is also a first approach from a municipality to take responsibility in health with a long-term investment. The project will reach individuals who do not seek for medical help, thus reduce the inequalities in utilization of services. We hope that the results of this study as the first community-based cohort and intervention study in Turkey will accelerate health promotion activities of the local and national governments of the country.
References
ADA (2010) American diabetes association standards of medical care in diabetes. Diabetes Care 33(Suppl 1):S11–S61
Alpert B, McCrindle B, Daniels S, Dennison B, Hayman L, Jacobson M, Mahoney L, Rocchini A, Steinberger J, Urbina E, Williams R (2006) Atherosclerosis, hypertension, and obesity in the young, Committee of the American Heart Association Council on Cardiovascular Disease in the Young, recommendations for blood pressure measurement in human and experimental animals; part 1: blood pressure measurement in humans. Hypertension 48(1):e3 (author reply e5. Epub)
Altun B, Arici M, Nergizoglu G et al (2005) Prevalence, awareness, treatment and control of hypertension in Turkey (the PatenT study) in 2003. J Hypertens 23(10):1817–1823
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395
Galea S, Tracy M (2007) Participation rates in epidemiologic studies. Ann Epidemiol 17:643–653
Graham I, Atar D et al (2007) European Guidelines on Cardiovascular Disease Prevention in Clinical Practice: fourth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Prevention in Clinical Practice (Constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil 14 (Suppl 2): S1–S113 (Executive summary: Eur J Cardiovasc Prev Rehabil 2007;14 (Suppl 2):E1–E40; Eur Heart J 28:2375–2414)
Kark SL (1989) The practice of community-oriented primary health care. The Hebrew University of Jerusalem, The Faculty of Medicine, Jerusalem
Lean MEJ, Han TS, Morrison CE (1995) Waist circumference as a measure for indicating need for weight management. BMJ 311:158–161
Lenfant C, Chobanian AV, Jones DW, Roccella EJ (2003) Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): resetting the hypertension sails. Hypertension 41(6):1178–1179
Mahley RW, Palaoglu KE, Atak Z, Dawson-Pepin J, Langlois AM, Cheung V, Onat H, Fulks P, Mahley LL, Vakar F et al (1995) Turkish heart study: lipids, lipoproteins, and apolipoproteins. J Lipid Res 36(4):839–859
Mancia G, De Backer G et al (2007) 2007 Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 28(12):1462–1536
MoH (2004) National burden of disease and cost effectiveness project burden of disease final report. http://www.tusak.saglik.gov.tr/pdf/nbd/raporlar/hastalikyukuTR.pdf. Accessed 07 Jan 2011
MoH (2009) Republic of Turkey Ministry of Health, Prevention and Control Program for Cardiovascular Diseases Strategic Plan and Action Plan for the Risk Factors. http://www.tkd-online.org/PDFs/StrategicActionPlan.pdf. Accessed 08 Jan 2011
MoH (2010) Global Adult Tobacco Survey Turkey Report. http://www.who.int/tobacco/surveillance/en_tfi_gats_turkey_2009.pdf. Accessed 15 June 2011
NCEP-ATP III (2002) National cholesterol education program expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult treatment panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 106(25):3143–3421
Oğuz A, Temizhan A, Abaci A, Kozan O, Erol C, Ongen Z, Celik S (2008) Obesity and abdominal obesity: an alarming challenge for cardio-metabolic risk in Turkish adults. Anadolu Kardiyol Derg 8(6):401–406
Onat A (2001) Risk factors and cardiovascular disease in Turkey. Atherosclerosis 156(1):1–10
Onat A, Can G, Hergenç G, Küçükdurmaz Z, Uğur M, Yüksel H (2010) High absolute coronary disease risk among Turks: involvement of risk factors additional to conventional ones. Cardiology 115:297–306. doi:10.1159/000312009
Oppenheimer G M (2005) Becoming the Framingham Study 1947–1950. Am J Public Health 95(4):602–610
Pennant M, Davenport C, Bayliss S, Greenheld W, Marshall T, Hyde C (2010) Community programs for the prevention of cardiovascular disease: a systematic review. Am J Epidemiol 172:501–516
Puska P (2002) Successful prevention of non-communicable diseases: 25 year experiences with North Karelia Project in Finland. Public Health Med 4(1):5–7
Rayner M, Allender S, Scarborough P, British Heart Foundation Health Promotion Research Group (2009) Cardiovascular disease in Europe. Eur J Cardiovasc Prev Rehabil 16(Suppl 2):S43–S47
Rose G (1992) The strategy of preventive medicine. Oxford University Press Inc., Oxford
Sanisoglu SY, Oktenli C, Hasimi A, Yokusoglu M, Ugurlu M (2006) Prevalence of metabolic syndrome-related disorders in a large adult population in Turkey. BMC Public Health 10(6):92
Satman I, Yilmaz T, Sengül A, Salman S, Salman F, Uygur S, Bastar I, Tütüncü Y, Sargin M, Dinççag N, Karsidag K, Kalaça S, Özcan C, King H (2002) Population-based study of diabetes and risk characteristics in Turkey. Results of the Turkish Diabetes Epidemiology Study (TURDEP). Diabetes Care 25(9):1551–1556
Taylor AW, Grande ED, Gill T, Chittleborough CR, Wilson DH, Adams RJ, Grant JF, Phillips P, Ruffin RE, The North West Adelaide Health Study Team (2006) Do people with risky behaviours participate in biomedical cohort studies? BMC Public Health 6:11
Tunstall Pedoe H, Kuulasmaa K, Mahonen M, Tolonen H, Ruokokoski E, Amouyel P, WHO MONICA project (1999) Contribution of trends in survival and coronary-event rates to changes in coronary heart disease mortality: 10 year results from 37 MONICA project populations. Lancet 353:1547–1557
TurkStat (2006) Aile Yapısı Araştırması. http://www.aile.gov.tr/files/Aileyapısı2006.pdf. Accessed 07 Jan 2011
TurkStat (2008) Turkish Statistical Institute Death Report. http://tuikrapor.tuik.gov.tr/reports/rwservlet?demografidb2=&report=OLUM10.RDF&p_yil1=2008&p_dil=1&p_kod=1&desformat=spreadsheet&ENVID=demografiEnv. Accessed 07 Jan 2011
WHO (2003) MONICA Project. MONICA monograph and multimedia sourcebook: world’s largest study of heart disease stroke, risk factors and population trends 1979–2002. http://www.ktl.fi/monic/public/monograph.html. Accessed 07 Jan 2011
WHO (2004) Deaths by cause in WHO Regions. http://www.who.int/healthinfo/global_burden_disease/DTH6%202004.xls. Accessed 07 Jan 2011
WHO (2005) Preventing chronic diseases: a vital investment: WHO global report. http://www.who.int/chp/chronic_disease_report/full_report.pdf . Accessed 07 Jan 2011
WHO (2005) Chronic diseases and their common risk factors, facing the facts. www.who.int/entity/chp/chronic_disease_report/media/Factsheet1.pdf. Accessed 07 Jan 2011
WHO (2008) 2008–2013 action plan for the global strategy for the prevention and control of noncommunicable diseases, World Health Assembly Document A61/8. www.who.int/entity/nmh/publications/ncd_action_plan_en.pdf. Accessed 07 Jan 2011
WHO (2009) Report on global tobacco epidemic, implementing smoke free environments. http://whqlibdoc.who.int/publications/2009/9789241563918_eng_full.pdf. Accessed 07 Jan 2011
Wilson PWF (1998) D’Agostino RB, Levy D, Belanger AM., Silbershatz H, Kannel WB Prediction of coronary heart disease using risk factor categories. Circulation 97(18):1837–1847
Yumuk VD (2005) Prevalence of obesity in Turkey. Obes Rev 6(1):9–10
Acknowledgments
This project is supported jointly by Balçova Municipality and Dokuz Eylül University Research Fund.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ergör, G., Soysal, A., Sözmen, K. et al. Balcova heart study: rationale and methodology of the Turkish cohort. Int J Public Health 57, 535–542 (2012). https://doi.org/10.1007/s00038-011-0309-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-011-0309-x