Abstract
Kashin-Beck disease (KBD), a particular type of osteoarthritis (OA), and an endemic disease with articular cartilage damage and chondrocytes apoptosis, can affect many joints, and the most commonly affected joints are the knee, ankle, and hand. KBD has traditionally been classified as a non-inflammatory OA. However, recent studies have shown that inflammation has played an important role in the development of KBD. Nowadays, clinical KBD is not only an endemic disease, but also a combined result of many other non-endemic factors, which contains age, altered biomechanics, joint trauma and secondary OA. The characteristics of the developmental joint failure of advanced KBD, because of the biochemical and mechanical processes, are tightly linked with the interaction of joint damage and its immune response, as well as the subsequent state of chronic inflammation leading to KBD progression. In this review, we focus on the epidemiology, pathology, imaging, cytokines and transduction pathways investigating the association of inflammation with KBD; meanwhile, a wide range of data will be discussed to elicit our current hypotheses considering the role of inflammation and immune activation in KBD development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kashin-Beck disease (KBD), known as an endemic disease, mainly occurs in the regions from Northeast China to Sichuan-Tibet Plateau, Russia and North Korea. Unlike other bone and joint diseases, for example, rheumatoid arthritis (RA), osteoarthritis (OA), reactive arthritis, and even septic arthritis, KBD showed obvious geographical features [1]. The characteristics of KBD are articular cartilage damage and chondrocytes apoptosis. KBD can affect many joints, and the most commonly affected joints are the knee, ankle, and hand [1, 2]. Early investigations of KBD etiology and pathogenesis mainly focused on the effects of the endemic factors, such as selenium deficiency, cereal contamination by mycotoxin, and high humic acid levels in drinking water [2].
The investigation of KBD as a non-inflammatory disease is a consequence of the long-term epidemiologic study of KBD. However, 20 years ago, the synovial inflammation in KBD patients was observed [3]. Subsequently, the inflammatory cytokines in articular synovial fluid [4–6] and serum [7–10] from KBD patients were investigated. Given greater appreciation for inflammatory response in patients with KBD, inflammation has been highly emphasized in the study of KBD progression recently. This is not to suggest that KBD pathogenesis is a result of inflammation, but rather that the inflammation maybe a secondary process initiated by immune activation following cartilage damage, which ultimately leads to a state of chronic joint inflammation that drives progression toward the phenotype recognized as clinical KBD.
For the prevention or treatment of KBD, sodium selenite [11, 12], pain killers and anti-inflammatory drugs [13], vitamins [14], hyaluronic acid [15], chondroitin sulfate and glucosamine [16] have been used. Thanks to these measures, KBD in children is under control and has almost disappeared today. However, KBD in adults is still a serious problem because of its high incidence in China during the last century. Due to the poor self-renewal ability of cartilage, tissue engineering and gene therapy have not been applied to the treatment of cartilage damages in KBD patients; meanwhile no effective clinical measures were carried out to repair the cartilage damages or defects of KBD at present. Considering the high disability and economic burdens among the patients with KBD in endemic regions, increased understanding of the inflammation function, which leads to the progression of KBD could enable development of targeted therapies.
Review
Understanding clinical KBD as an inflammatory disease
KBD, occurred in endemic regions and induced by endemic environmental factors, is long-term considered as an endemic disease, thus, it's not easy to consider that KBD is also an inflammatory disease. Whereas, the clinical KBD, a combination of chondrocytes apoptosis, cartilage damage, aging, and immune response, is quite similar to clinical OA in which inflammation plays a driving role in its progression [17]. Hence it can be estimated that inflammation occurs in clinical KBD too. We should recognize that inflammation is not exclusive to RA and other classical inflammatory disease. Some early studies in KBD with the comparisons of RA and OA tissues, observed dramatically increased levels of inflammatory cytokines and proteins in KBD tissues [4, 18–21]. Although the inflammatory expression was largely overshadowed by more pronounced histological and biochemical abnormalities in RA and OA, elevated levels of inflammatory cytokines and proteins in both the serum and synovial fluid of patients with KBD were reported early this century [4–10]; from then on, more and more reports data of the inflammatory studies on KBD were provided. Unfortunately, because of the common use of RA and OA tissues and fluids as comparators in KBD investigations, the inflammatory effect of KBD has been underestimated. Actually, the KBD tissues and fluids, when compared with normal tissues or fluids, are highly enriched with inflammatory cytokines [5–10, 22, 23]. Therefore, it should be noticed that inflammation occurs in KBD.
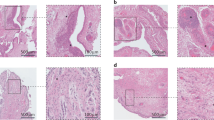
Cartilage damage
KBD predominantly affects children from 3 to 12 years old, resulting in chondrocyte growth stagnation, degeneration and necrosis, dissolve and disappear [24]. As a result, the growth and developmental disorders of cartilage and bone, joint enlargement, joint space narrowing, pain and impaired joint mobility could be observed in adult KBD (Fig. 1). Even more serious, the phenomena of early closure of metaphyseal, ossification disorders and developmental arrest of tubular bone in length diameter, which are observed in KBD children, can eventually lead to short stature and permanent disability (short fingers, extremity disability) of KBD-affected adults [25].
Characteristics of KBD patients. a Deformed joints in two knees and b flexion of the terminal finger joints or deformed fingers of grade III KBD adult (male, 58 years age). Radiographic findings in the right knee and right hand of a patient with grade II KBD (female, 60 years age). c Obvious joint space narrowing and loosened bodies in knee and d wrist joint crowded and space narrowing, phalanx thickening and osteophyte formation
The distinction of KBD from OA or other bone and joint diseases is the damage of epiphyseal cartilage and hyaline cartilage. Although the lesion of hyaline cartilage is crucial in KBD diagnosis based on X-ray detection, the change is not specific but quite similar to the pathological changes of OA. Therefore, the damage of epiphyseal plate cartilage is the most important characteristic in the diagnosis of KBD [25]. Besides, chondrocyte dedifferentiation, deep zone chondronecrotic changes and abnormal type-X collagen, TGF-β, PTHrP, bFGF and VEGF staining patterns have been noticed in KBD cartilage [26].
Extracellular matrix degradation
Degradation of extracellular matrix (ECM) is detected at sites of inflammation in the joints of KBD patients. Decreased content of proteoglycans is observed in the deep zone of cartilage, particularly in the necrotic areas [27], which means that the proteoglycan metabolism is affected in KBD. Aggrecanase-generated epitopes in KBD cartilage are present [28]. The percentages of chondrocytes staining for MMP-1/-13 and MMP-generated DIPEN neoepitope, aggrecanase-generated ITEGE neoepitope in aggrecan in KBD children were significantly higher than those in control. The percentage of chondrocytes staining for the TIMP-2 was significantly higher in the superficial and middle zones of KBD samples than that in control; however, the TIMP-1 was significantly lower than that in control [29].
ECM degradation products might promote inflammation and cartilage loss. It was observed that cartilage damage occurred by loss of proteoglycans when the fragments, derived from the breakdown of fibronectin were injected into knees of adolescent rabbits [30]. It was also noticed that the proinflammatory cytokines, such as, tumor necrosis factor α (TNF-α) and interleukin-1β (IL-1β), as well as matrix metalloproteinases (MMP-1/-3) mediators known to be implicated in chondrolysis, could be induced by the production of fibronectin fragments [31]. Based on the observations above, we propose a hypothesis for the KBD progress: ECM breakdown by cartilage damage results in the production of fragments, cytokines and molecules, which could initiate local inflammatory responses leading to further chondrolysis and release of additional ECM breakdown products. Notably, e.g., chondroitin sulfate, glucosamine and hyaluronic acid, known as additional ECM breakdown products, have been implied as DAMPs in mediating joint damage of KBD.
Synovial inflammation
The synovial inflammation attracted more attention in OA than it did in KBD. As reported in OA, although the synovium is notable lack of inflammatory cells, hyperplasia of the synovial lining cells in OA is often observed with an infiltration of inflammatory cells consisting primarily of macrophages, T and B cells [32], mast cells [33] and natural killer cells [34]. One study with the comparison of early and late OA by Benito and his colleagues demonstrated that the overexpression of inflammatory mediators and increased mononuclear cell infiltration were present in early disease [35]. In addition, synovial inflammation was present in 43 % of OA patients who were undergoing arthroscopic meniscectomy to repair traumatic meniscal injury and was associated with worse preoperative pain and function scores [36].
It is high time that we should pay more attention to the formation of synovitis in KBD and study its influence on KBD progression. Even though synovium is not the only tissue involved in KBD-related inflammation, it is a major site of inflammatory change. Despite the thickness of synovium is an about two to three cell layer with notable lack of inflammatory cells, synovial inflammation in KBD patients may precede cartilage structural change as well. In 1992, synovitis in KBD was first reported by Zhu and his colleague [3]. Later studies were focused on the expression of inflammatory cytokines in synovium and demonstrated significant synovial inflammation in KBD [4, 21], which suggested that interventions targeting synovial inflammatory processes might be efficacious for the treatment of KBD.
Inflammatory mediators involved in KBD
Soluble inflammatory factors such as cytokines are central to most inflammatory processes, and several cytokines have been implicated in KBD (Table 1). One previous study showed a significantly higher expression of IL-6 in the serum of KBD and OA patients than in the healthy adults, meanwhile, there was no significant difference on IL-6 level between KBD and OA patients [10]. Investigation from Cui and his colleagues identified higher levels of TNF-α and IL-1β in serum of patients with KBD than that in healthy control [9]. Similarly, study by Sun and his colleagues showed the expressions levels of IL-1β and TNF-α in the synovium and synovial fluid were significantly higher in patients with KBD and OA than in patients with meniscus injury [4]. Another study performed by Tong and Yang demonstrated that elevated levels of TNF and IL-1 were found in synovial fluid of KBD compared with healthy control [5]. Furthermore, significantly higher serum levels of IL-1β, TNF-α, cartilage oligomeric matrix protein (COMP), and type II collagen (CTX-II) were observed in the KBD and OA group than those in the healthy adult group; there were no significant differences on the levels of IL-1β and TNF-α in the KBD and OA groups [8]. Moreover, the staining for IL-6, IL-1β and TNF-α were elevated in articular cartilage from phalanges of hands of KBD children than that from normal children [37]. Besides, excessive apoptosis and abnormal expression of apoptosis regulating factors which might interacted with inflammation response, such as Bcl-2, Bax, Fas and inducible NO synthase (iNOS) were observed in KBD cartilage [38]. The results were consistent with the increased serum levels of NO and iNOS in KBD patients [7].
In a rat model of KBD, the serum levels of IL-6 were significantly elevated in rats fed with selenium-deficient, T-2 toxin, and T-2 toxin plus selenium-deficient diets in contrast to those with the normal diet, while the serum levels of IL-1β and TNF-α were significantly increased only in the rats group fed with T-2 toxin plus selenium-deficient diet [37]. In another rat model, the levels of IL-1β, IL-6 and TNF-α in the serum were found with no significant differences between the KBD-affected feed group (feed with the wheat and corn samples from a KBD-affected family located in Xiaojin county of the A’ba region, Sichuan, China) and the low protein plus T-2 toxin feed group. However, a significant increased serum level of IL-1β, IL-6 and TNF-α was noticed in the above-mentioned two groups when compared with normal feed plus the T-2 toxin group [39].
Although the functions of these cytokines in KBD were still unclear, there were numerous studies providing a catabolic role of elevated cytokines in the OA joint. As reported in OA, IL-1β and TNF-α signaling, culminating in the activation of activator protein transcription factors and nuclear factor-κB (NF-κB), could induce expression of IL-1β, TNF-α, IL-6, NO, MMP1, MMP9, MMP13 and prostaglandin E2 (PGE2) [40]. Many inflammatory cytokines can influence cartilage homeostasis with inducing cartilage catabolism and inhibiting anabolic processes. For example, it is reported that IL-1β can inhibit the production of cartilage ECM components, including aggrecan [41], types II and IX collagen [42]. It also showed that the elevated IL-6 at sites of inflammation in OA can activate T cells, B cells, and mediate the recruitment of inflammatory cells to sites of inflammation [43]. Besides, the inhibitor of IL-6 receptor was effective for the treatment of RA [44].
Inflammatory pathways activated in KBD
As the observation of the higher expression of TNF-α, VEGF, TGF-β and IL-1 in KBD cartilage [22], inflammation may be both a primary event in KBD and/or a secondary event in the disease. The KBD is characterized by chondrocyte apoptosis and pathological changes after cartilage necrosis, inflammation response maybe or may activate the up-stream of the chondrocytes apoptosis. For example, p38 protein kinase and c-Jun N-terminal kinase (JNK) pathways, two major pathways of mitogen-activated protein kinase (MAPK) inflammation-associated signal transduction, play a driving role in the stimulation of apoptotic signaling as well as inflammatory response. As reported in previous studies, the apoptotic function of ATF2, especially the elevated phosphate type of ATF2 in KBD cartilage is mainly enhanced through JNK signal pathway compared with p38 pathway. Thus, the activation of ATF2 through JNK pathway might be a possible target in the prevention and treatment of KBD [45].
By comparison of articular chondrocytes gene expression profile between KBD and OA, 195 up-regulated and 38 down-regulated genes was identified in KBD, such as PIM2, EFNA1, CSGALNACT, SMAD9, AQP, STK11, APCDD, T cell factor/LEF, and PTN [19]. Some of the above differentially expressed genes, linked to chondrocytes apoptosis, ion channel proteins and cartilage metabolism, were reported to have interaction with inflammation [46, 47]. Besides, by Gene Set Enrichment Analysis (GSEA) of cartilage from KBD and OA, apoptosis-related and NO-related pathways were significantly up-regulated in KBD cartilage [20]. These results are consistent with the increased levels of NO and iNOS [7] in KBD serum and abnormal expression of Bax, Fas, Bcl-2, iNOS in KBD cartilage [39]. In general, the development of KBD was greatly contributed to chondrocyte apoptosis, which was mediated by NO-related pathways.
Innate immunity: a perceive of damage and inflammation in KBD
Innate immunity implies that the host immune responses are induced by invariable pattern-recognition receptors (PRRs), which respond to conserved patterns in nature, such as bacteria, viruses, and fungi [48]. PRRs also identify multiple endogenous “danger signals” resulting tissue damage, including pathogen associated molecular patterns (PAMPs) and (DAMPs), which composed of potentially even more diverse group of molecules [17]. A protective response of either combat infection or initiate repair processes by immune system was the consequence of signals from both PAMPs and DAMPs.
As known, unlike RA, although KBD showed little association with a robust adaptive immune response, activation of the innate immune system was critical for both diseases. Markers of autoimmune response were also elevated in KBD patients. Arthritis-related autoantibodies and inflammatory factors, including types II, IX, and XI collagen, cyclic citrullinated peptide (CCP), immunoglobulin (Ig)-G and IgM in plasma from KBD patients were examined and compared with RA patients, OA patients and healthy controls. It has been notified that the plasma levels of IgG-RF, collagen IX antibodies and NO were obviously higher in KBD patients compared with that in the other groups. Meanwhile, collagen XI antibodies, CCP antibodies and IgM-RF were higher in the plasma of the KBD group than that in the control group. These results further confirmed that autoimmunity and inflammation might involve in the development of KBD, especially in the advanced stage of KBD [18].
Chronic inflammation: second stage in clinical KBD
The formation of cartilage loosen bodies and early cartilage degradation may play a driving role in the development of inflammation within the KBD joint and specifically the KBD synovium. In fact, chronic inflammation is ubiquitous present in KBD patients and should be considered as a driving force of progressive degeneration in clinical KBD joints. The KBD joint might be likened to a chronic wound, as a result of cartilage injury affected by environmental factors, induces a local pathologic inflammatory response that results in further cartilage loss and progressive joint injury over time. Therefore, the development of chronic inflammation in KBD might be understood as a vicious, self-perpetuating cycle of local tissue damage, inflammation, and repair. This hypothesis is depicted in Fig. 2. Biomechanics are central to the development of KBD, since cartilage damage from prior mechanical derangement by interaction of gene-environmental factor, can produce ongoing chronic inflammation and its immune response.
Schematic representation of chronic inflammation as a mediator of clinical KBD. Following cartilage damage by environmental factors, results in the production of damage-associated molecular patterns (DAMPs), including cartilage extracellular matrix (ECM) breakdown products and plasma proteins that signal through pattern recognition receptors on synovial macrophages, fibroblast-like synoviocytes, or chondrocytes to induce the local production of inflammatory mediators. Acute and chronic production of inflammatory mediators promotes further cartilage degradation either directly or indirectly through their induction of proteolytic enzymes, amplifying a vicious cycle of innate immune activation in KBD
Inflammation as a target for treatment of KBD
Although synovitis is observed in a part of clinical KBD patients, the relationship between KBD and synovitis is still uncertain. The impact of synovitis on KBD onset and progression needs further study. Thus, the increasing recognition of environmental risk factors for the development of clinical KBD and the advent of highly sensitive imaging modalities for visualizing cartilage damage, as well as early synovitis may greatly enhance the appreciation of early anti-inflammatory interventions. Current therapies, such as selenium, intra-articular hyaluronic acid injections, nonsteroidal anti-inflammatory drugs (NSAID), COX-2 selective agents, vitamins and chondroitin sulfate showed efficiency for relieving discomfort of KBD patients [11–18]. Although several studies have demonstrated that the efficacy of meloxicam [13, 49], a COX-2-specific inhibitor, is effective in the treatment of knee pain due to KBD, no agent has been shown to have disease modifying effects on the structural progression of KBD. Since the role of inflammation in KBD process is still a mystery waiting to be unveiled. There are fewer trials of potent anti-inflammatory therapies targeted very early KBD by using anti-inflammatory intervention, might be more effective, including use of systemic and intra-articular biologic agents to inhibit IL-1β and TNF-α. Clinical KBD is a result of progressive damage of cartilage and bone after affected by endemic environmental factors, thus therapeutics may have limitations. The challenges for the development of KBD target drugs include the improved understanding of the activated inflammation function in KBD and the disease stage for intervention, as well as the need for improved measures of cartilage structural damage (beyond the use of X-rays).
Conclusions
In summary, understanding KBD not only as an endemic disease, but also as an inflammation disease, may help us investigate the function of inflammation in the occurrence and development of KBD, and seek for a possible explanation of the interaction between environmental factors and the environment response genes and proteins in the progression of KBD as well. Owing to the latest findings, a set of abnormally expressed genes, proteins and pathways in KBD has been identified mainly involved in chondrocyte structure, cartilage metabolism, ion channels, oxidative stress, mitochondrial function and apoptosis. Thus, understanding KBD as an inflammation disease may help us to better study the role of inflammatory cytokines and pathways in the lesions of articular cartilage and growth plate cartilage in KBD. This will further help researchers and clinical doctors to find effective genes, proteins and pathways, targeted and modified-disease therapies for the prevention and treatment of KBD.
Abbreviations
- APCDD:
-
Adenomatosis polyposis coli down-regulated
- AQP:
-
Aquaglyceroporin
- CCP:
-
Cyclic citrullinated peptide
- COX:
-
Cyclooxygenase
- CSGALNACT:
-
Chondroitin sulfate N-acetylgalactosaminyltransferase
- CTX-II:
-
Type II collagen
- DAMPs:
-
Damage (or danger) associated molecular patterns
- ECM:
-
Extracellular matrix
- EFNA1:
-
Ephrin-A1
- FGF:
-
Fibroblast growth factor
- IGF:
-
Insulin-like growth factor
- IL:
-
Interleukin
- JNK:
-
c-Jun N-terminal kinase
- KBD:
-
Kashin-Beck disease
- LEF:
-
Lethal factor
- MAPK:
-
Mitogen-activated protein kinase
- MMP:
-
Matrix metalloproteinase
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- NSAID:
-
Nonsteroidal anti-inflammatory drugs
- OA:
-
Osteoarthritis
- PAMPs:
-
Pathogen associated molecular patterns
- PIM2:
-
Pim-2 proto-oncogene
- PTHrP:
-
Parathyroid hormone-related peptide
- PTN:
-
Pleiotrophin
- RA:
-
Rheumatoid arthritis
- SMAD9:
-
SMAD family member 9
- STK11:
-
Serine/threonine kinase 11
- TGF-β:
-
Transforming growth factor β
- TIMP:
-
Metallopeptidase inhibitor
- TNF-α:
-
Tumor necrosis factor α
- VEGF:
-
Vascular endothelial growth factor
References
Guo X, Ma WJ, Zhang F, Ren FL, Qu CJ, Lammi MJ. Recent advances in the research of an endemic osteochondropathy in China: Kashin-Beck disease. Osteoarthr Cartilage. 2014;22:1774–83.
Allander E. Kashin-Beck disease: an analysis of research and public health activities based on a bibliography 1849–1992. Scand J Rheumatol Suppl. 1994;99:1–36.
Zhu SD, Shao YX, Luo ZL. A case report of pigmented nodular villous synovitis in knees with KBD. Med J Natl Defending Forces Northwest China. 1992;4:67–8 (in Chinese).
Sun ZM, Ling M, Liu M, Zhang YG. Expression of interleukin-1β and tumor necrosis factor-α in the synovium and synovial fluid of patients with Kashin-Beck disease and osteoarthritis. J South Med Univ. 2009;29:5–8 (in Chinese).
Tong WS, Yang TF. IL-1 and TNF bioassay in synovial fluid of patients with Kashin-Beck disease. Chin J Ctrl Enden Dis. 2000;15:71–2 (in Chinese).
Yang T, Wang GL, Tong WS, Gong Q, Chen YQ. Measurement of the bioactivity of interleukin and tumour necrosis factor in synovial fluid of Kashin-Beck disease. Int Orthop. 2001;25:162–3.
Zhang BD, Guo X, Bai GK, Ping ZG, Zuo H, Ren FL, Xu GY, Geng D. The changes of nitric oxide, NO synthase, and sFas/Apo-1 in serum among the patients with Kashin-Beck disease. Chin J Endemiol. 2004;31:172–5 (in Chinese).
Tang X, Zhou Z, Shen B, Yang J, Kang P, Li J, Crook N, Li Q, Min L, Pei FX. Serum levels of TNF-alpha, IL-1beta, COMP, and CTX-II in patients with Kashin-Beck disease in Sichuan, China. Rheumatol Int. 2012;32:3503–9.
Cui CL, Yu HY, Yue YT, Yang GX, Shang WC, Yuan ZM. Detection of serum interleukin-β and tumor necrosis factor-α of patients with Kashin-Beck disease. J Zhengzhou Univ. 2008;43:656–8 (in Chinese).
Tang X, Zhou ZK, Shen B, Yang J, Kang PD, Li J, Li Q, Huang Q, Pei XF. Detection of serum levels of interleukin-6 in patients with Kashin-Beck disease and osteoarthritis in Kashin-Beck disease prevalent area. Chin J Bone Jt Surg. 2012;5:429–32 (in Chinese).
Jirong Y, Huiyun P, Zhongzhe Y, Birong D, Weimin L, Ming Y, Yi S. Sodium selenite for treatment of Kashin-Beck disease in children: a systematic review of randomised controlled trials. Osteoarthr Cartilage. 2012;20:605–13.
Zou K, Liu G, Wu T, Du L. Selenium for preventing Kashin-Beck osteoarthropathy in children: a meta-analysis. Osteoarthr Cartilage. 2009;17:144–51.
Luo R, Liu G, Liu W, Pei FX, Zhou ZK, Li J, Shen B, Kang PD, Xie QB, Ma X. Efficacy of celecoxib, meloxicam and paracetamol in elderly Kashin-Beck disease (KBD) patients. Int Orthop. 2011;35:1409–14.
Li CZ. A roentgenological observation of the effect of selenium and vitamin E treatment on children with early-stage Kashin-Beck disease. Chin Med J. 1979;59:169–71 (in Chinese).
Yu FF, Xia CT, Fang H, Han J, Younus MI, Guo X. Evaluation of the therapeutic effect of treatment with intra-articular hyaluronic acid in knees for Kashin-Beck disease: a meta-analysis. Osteoarthr Cartilage. 2014;22:718–25.
Yue J, Yang M, Yi S, Dong B, Li W, Yang Z, Lu J, Zhang R, Yong J. Chondroitin sulfate and/or glucosamine hydrochloride for Kashin-Beck disease: a cluster-randomized, placebo controlled study. Osteoarthr Cartilage. 2012;20:622–9.
Sokolove J, Lepus CM. Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Ther Adv Musculoskel Dis. 2013;5:77–94.
Tian L, Wang W, Hou W, Tian J, Zhong N, Sun J, Guo DW, Yao JF, Xu P, Su PH, He L, Lu SM. Autoimmune and inflammatory responses in Kashin-Beck disease compared with rheumatoid arthritis and osteoarthritis. Hum Immunol. 2011;72:812–6.
Duan C, Guo X, Zhang XD, Yu HJ, Yan H, Gao Y, Ma WJ, Gao ZQ, Xu P, Lammi MJ. Comparative analysis of gene expression profiles between primary knee osteoarthritis and an osteoarthritis endemic to Northwestern China, Kashin-Beck disease. Arthritis Rheum. 2010;62:771–80.
Zhang F, Guo X, Duan C, Wu S, Yu H, Lammi M. Identification of differentially expressed genes and pathways between primary osteoarthritis and endemic osteoarthritis (Kashin-Beck disease). Scand J Rheumatol. 2013;42:71–9.
Chen GH. The experimental study on functioning mechanism of MMP-13 and IGF-1 in the synovium of Osteoarthritis and Kashin-Beck Disease. Lanzhou Univ. 2009; Master Thesis (in Chinese).
Wang WZ, Guo X, Duan C, Ma WJ, Zhang YG, Xu P, Gao ZQ, Wang ZF, Yan H, Zhang YF, Yu YX, Chen JC, Lammi MJ. Comparative analysis of gene expression profiles between the normal human cartilage and the one with endemic osteoarthritis. Osteoarthr Cartilage. 2009;17:83–90.
Zhu CS, Feng QH, Yu YX, Wang DL, Chen M, Wang XY, Jin BQ. Detection of proinflammatory cytokine levels in sera from patients with Kaschin-Beck disease. Chin J Cell Mol Immunol. 2006;22:84–5 (in Chinese).
Zhang GQ, Liu JX, Yu JY, Shi YX, Zhang SJ. Ultrastructure of chondrocytes in articular cartilage of Kashin-Beck disease. Chin J Endemiol. 1989;8:27–30 (in Chinese).
Guo X. Diagnostic, clinical and radiological characteristics of Kashin-Beck disease in Shaanxi Province, PR China. Int Orthop. 2001;25:147–50.
Guo X, Zuo H, Cao CX, Zhang Y, Geng D, Zhang ZT, Zhang YG, von der Mark K, von der Mark H. Abnormal expression of Col X, PTHrP, TGF-beta, bFGF, and VEGF in cartilage with Kashin-Beck disease. J Bone Miner Metab. 2006;24:319–28.
Li SY, Cao JL, Caterson B, Hughes CE. Proteoglycan metabolism, cell death and Kashin-Beck disease. Glycoconj J. 2012;29:241–8.
Cao JL, Li SY, Shi Z, Yue Y, Sun J, Chen JH, Fu Q, Hughes CE, Caterson B. Articular cartilage metabolism in patients with Kashin-Beck disease: an endemic osteoarthropathy in China. Osteoarthr Cartilage. 2008;16:680–8.
Chen JH, Luo MX, Wang W, Zhang ZT, He Y, Duance VC, Hughes CE, Caterson B, Cao JL. Altered proteolytic activity and expression of MMPs and aggrecanases and their inhibitors in Kashin-Beck disease. J Orthop Res. 2014;33:47–55.
Homandberg G, Meyers R, Williams J. Intraarticular injection of fibronectin fragments causes severe depletion of cartilage proteoglycans in vivo. J Rheumatol. 1993;20:1378–82.
Homandberg G, Hui F. Association of proteoglycan degradation with catabolic cytokine and stromelysin release from cartilage cultured with fibronectin fragments. Arch Biochem Biophys. 1996;334:325–31.
Bondeson J, Blom AB, Wainwright S, Hughes C, Caterson B, van den Berg W. The role of synovial macrophages and macrophage-produced mediators in driving inflammatory and destructive responses in osteoarthritis. Arthritis Rheum. 2010;62:647–57.
Dean G, Hoyland J, Denton J, Donn R, Freemont A. Mast cells in the synovium and synovial fluid in osteoarthritis. Br J Rheumatol. 1993;32:671–5.
Scanzello C, Umoh E, Pessler F, Diaz-Torne C, Miles T, Dicarlo E, Potter HG, Mandl L, Marx R, Rodeo S, Goldring SR, Crow MK. Local cytokine profiles in knee osteoarthritis: elevated synovial fluid interleukin-15 differentiates early from end-stage disease. Osteoarthr Cartilage. 2009;17:1040–8.
Benito M, Veale D, FitzGerald O, van den Berg W, Bresnihan B. Synovial tissue inflammation in early and late osteoarthritis. Ann Rheum Dis. 2005;64:1263–7.
Scanzello C, McKeon B, Swaim B, DiCarlo E, Asomugha E, Kanda V, Nair A, Lee DM, Richmond JC, Katz JN, Crow MK, Goldring SR. Synovial inflammation in patients undergoing arthroscopic meniscectomy: molecular characterization and relationship to symptoms. Arthritis Rheum. 2011;63:391–400.
Zhou XR, Wang ZL, Chen JH, Wang W, Song DQ, Li SY, Yang HJ, Xue SH, Chen C. Increased levels of IL-6, IL-1b, and TNF-α in Kashin-Beck disease and rats induced by T-2 toxin and selenium deficiency. Rheumatol Int. 2014;34:995–1004.
Wang SJ, Guo X, Zuo H, Zhang YG, Xu P, Ping ZG, Zhang ZT, Geng D. Chondrocyte apoptosis and expression of Bcl-2, Bax, Fas, and iNOS in articular cartilage in patients with Kashin-Beck disease. J Rheumatol. 2006;33:615–9.
Yan DL, Kang PD, Shen B, Yang J, Zhou ZK, Duan LJ, Pei FX. Serum levels of IL-1b, IL-6 and TNF-α in rats fed with Kashin-Beck disease-affected diet. Int J Rheum Dis. 2010;13:406–11.
Attur M, Patel I, Patel R, Abramson S, Amin A. Autocrine production of IL-1 beta by human osteoarthritis-affected cartilage and differential regulation of endogenous nitric oxide, IL-6, prostaglandin E2, and IL-8. Proc Assoc Am Phys. 1998;110:65–72.
Pfander D, Heinz N, Rothe P, Carl H, Swoboda B. Tenascin and aggrecan expression by articular chondrocytes is influenced by interleukin 1beta: a possible explanation for the changes in matrix synthesis during osteoarthritis. Ann Rheum Dis. 2004;63:240–4.
Goldring M, Birkhead J, Sandell L, Kimura T, Krane SM. Interleukin 1 suppresses expression of cartilage-specific types II and IX collagens and increases types I and III collagens in human chondrocytes. J Clin Invest. 1988;82:2026–37.
Gabay C. Interleukin-6 and chronic inflammation. Arthritis Res Ther. 2006;8:S3.
Jones G, Sebba A, Gu J, Lowenstein M, Calvo A, Gomez-Reino J, Siri DA, Tomsic M, Alecock E, Woodworth T, Genovese MC. Comparison of tocilizumab monotherapy versus methotrexate monotherapy in patients with moderate to severe rheumatoid arthritis: the AMBITION study. Ann Rheum Dis. 2010;69:88–96.
Han J, Guo X, Tan WH, Zhang F, Liu JT, Wang WZ, Xu P, Lammi MJ. The expression of p-ATF2 involved in the chondeocytes apoptosis of an endemic osteoarthritis, Kashin-Beck disease. BMC Musculoskel Dis. 2013;14:209–18.
Bansal K, Kapoor N, Narayana Y, Puzo G, Gilleron M, Balaji KN. PIM2 Induced COX-2 and MMP-9 expression in macrophages requires PI3K and Notch1 signaling. PLoS One. 2009;4:e4911.
Yao Y, Ding C, Fang Y. Combination of MTX and LEF attenuates inflammatory bone erosion by down-regulation of receptor activator of NF-kB ligand and interleukin-17 in type II collagen-induced arthritis rats. Rheumatol Int. 2013;33:1845–53.
Kawai T, Akira S. The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat Immunol. 2010;11:373–84.
Tang X, Pei FX, Zhou ZK, Liu G, Shen B, Kang PD, Li J, Zhao XD, Li Q, Li Y. A randomized, single-blind comparison of the efficacy and tolerability of hyaluronate acid and meloxicam in adult patients with Kashin-Beck disease of the knee. Clin Rheumatol. 2012;31:1079–86.
Acknowledgments
This work was supported by the National Natural Scientific Foundation of China (81402639, 81472924), Shaanxi Province Natural Science Basic Research Program for Youths (2015JQ8310) and the China Postdoctoral Science Fund (2014M562423).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Responsible Editor: John Di Battista.
Rights and permissions
About this article
Cite this article
Han, J., Wang, W., Qu, C. et al. Role of inflammation in the process of clinical Kashin-Beck disease: latest findings and interpretations. Inflamm. Res. 64, 853–860 (2015). https://doi.org/10.1007/s00011-015-0861-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-015-0861-6