Abstract
The objective of this study was to compare the efficacy and tolerability of celecoxib, meloxicam and paracetamol in late Kashin-Beck disease. Adults (n = 168) with Kashin-Beck disease were randomised in clusters to receive six week courses of celecoxib 200 mg once daily, meloxicam 7.5 mg once daily or paracetamol 300 mg three times daily. Efficacy assessments included overall joint pain intensity and Western Ontario and McMaster Universities Osteoarthritis Index subscales; tolerability was evaluated by adverse event and physician reporting. Celecoxib and meloxicam were efficacious in relieving pain and improving stiffness, but unable to improve physical function after six weeks. Paracetamol was efficacious in relieving pain, but unable to improve morning stiffness and physical function after six weeks. Celecoxib and meloxicam provide predictable and sustained relief from pain and stiffness. Paracetamol can relieve the pain. None of the treatments improved impaired physical function in Kashin-Beck disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kashin-Beck disease (KBD) is a chronic, endemic, degenerative osteoarthropathy with severe skeletal deformation and dwarfism; its cause is unknown [1, 2]. Aetiological hypotheses include mycotoxins in stored barley grains [3, 4], selenium deficiency [5, 6] and excess of fulvic acid in drinking water [7]. Three million people are affected in an endemic area from east Siberia to north and west of China [8].
Initial pathological changes are multiple degenerative and necrotic lesions within the growth plate cartilage and articular cartilage, which are associated with disturbed mineralisation and malformation. The secondary pathological findings, visible on radiographs, are repairing and remodelling around the necrotic foci of the cartilage of the metaphysis, bone end, epiphysis and carpal bones [2]. The most frequently affected sites are the distal limb joints [9–11], especially the hands [2]. Although its aetiology differs from osteoarthritis (OA) and rheumatoid arthritis (RA), the central pathological feature of KBD is still a degradation of cartilage, similar to OA.
KBD usually afflicts children between the ages of five and 13 years at the onset and usually involves the metaphysis in growing bone. Clinically, the disease manifests in arthritic pain, morning stiffness, enlarged and shortened fingers, and deformed, enlarged joints with limited motion in the extremities. In seriously affected patients, this disease leads to shortened stature or dwarfism and disability in their daily life [2]. The physical environment will aggravate the evolution of the disease accelerating the OA lesions [12]. For some severely affected patients surgery will be needed to reconstruct the affected joints [9, 13].
The functional disability that partly results from the pain of KBD is one of the most common disabilities in the elderly population. Relieving the pain is an important intervention for those patients.
Based upon the experience for OA treatment, we tried to use non-steroidal anti-inflammatory drugs (NSAID) and analgesics to relieve the pain and other symptoms of KBD. This study was conducted to observe the efficacy and safety of celecoxib, meloxicam and paracetamol in treating the symptoms and improving the dysfunction of elderly KBD patients.
Methods
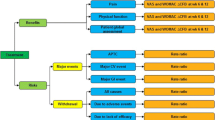
The study was conducted as a cluster randomised, mono-blind, parallel-group, mono-centre trial over six weeks in the Jala village, Bashen village and Rongmuda village of Rangtang county, Sichuan province, China. The primary objective was to determine the efficacy of celecoxib, meloxicam and paracetamol in the treatment of KBD as evaluated by the change in overall pain intensity in the most severely affected joint. Secondary objectives included the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index subscales, patients’ and physicians’ global assessment of disease activity and the assessment of the safety and tolerability profiles of celecoxib, meloxicam and paracetamol.
The study protocol was approved by the Institutional Review Boards at our medical college and was conducted according to Good Clinical Practice guidelines and in accordance with the Declaration of Helsinki (1964 and subsequent revisions). Patients provided informed consent before undergoing any study procedures.
Patients
Adult patients (aged 18–75 years) were eligible to participate in the study if they had a clinical or radiographic diagnosis of KBD. The clinical diagnosis of KBD was made by the orthopaedic surgeons and physicians of the Rheumatology Department of West China Hospital, West China Medical School, Sichuan University on the basis of clinical criteria previously described [10] and when patients had been symptomatic for at least three months prior to enrolment and had not received an NSAID or other analgesic therapy on a regular basis. Patients were required to have experienced a pain intensity of at least 40 mm on a 100-mm visual analogue scale (VAS; 0 mm representing no pain and 100 mm representing very severe pain) in the most severely affected joint during the 24 hours prior to randomisation. Patients were excluded from the trial if they had a history of, or evidence of, specified confounding disorders (e.g. septic arthritis, inflammatory joint disease or articular fracture). Significant medical problems that would, in the opinion of the investigators, influence outcomes were also grounds for exclusion, as were a history of open knee or hip surgery within one year prior to study entry, anaemia or hepatic, renal or blood coagulation disorders, prior intolerance of any NSAID or cyclooxygenase 2 (COX-2)-specific inhibitors, analgesic or antipyretic or presence of aspirin hypersensitivity. Patients with a history of upper gastrointestinal (GI) tract perforations, ulcers or peptic ulcer bleeding were not excluded unless the event had occurred within the six months prior to enrolment.
After a washout period of three to seven days, during which no NSAID therapy was permitted, eligible patients were randomised in clusters to receive celecoxib 200 mg once daily (qd), meloxicam 7.5 mg qd or paracetamol 300 mg three times daily (t.i.d.) for six weeks.
Variables
The primary efficacy comparison was between baseline and at week six of the overall joint pain intensity experienced in the most severely affected joint over the previous 24 hours, using a 100-mm VAS (0, no pain; 100, worst pain) for each drug. The joint assessed to be the most severely affected at screening was evaluated for the baseline and at week six.
Secondary efficacy measures were patients’ and physicians’ global assessment of disease activity also using the 100-mm VAS and assessment of pain, stiffness and physical function using the WOMAC Osteoarthritis Index (WOMAC 3.1 Likert questionnaire) [14]. All measures were applied at baseline and week six.
Safety variables included adverse events (AEs), serious AEs (SAEs), laboratory evaluations, vital signs and physical examinations conducted at each visit. AEs were graded based on qualitative assessment of the extent or intensity of the AE by the investigator, or as reported by the patients. SAEs were defined as any fatal or immediately life-threatening clinical experience or disabling event, or one that required prolonged inpatient hospitalisation, whether or not it was judged to be related to treatment.
Statistical analyses
All statistics were determined by using SPSS 15.0 software for Windows. The t test was used to analyse repeated measures such as primary efficacy variable and secondary efficacy variables. The incidence of AEs and the rates of patient withdrawals (overall and due to AEs) were compared between the groups using a χ2 test or Fisher’s exact test when appropriate. All statistical tests were two sided and performed at the 5% significance level.
Results
Study population
A total of 168 patients were divided into three groups by the cluster randomisation method to receive celecoxib 200 mg qd (n = 52), meloxicam 7.5 mg qd (n = 72) or paracetamol 300 mg t.i.d. (n = 44). The treatment groups were matched with no significant differences in baseline demographics and disease characteristics (Table 1) and most of the patients were of Tibetan nationality. In total, 12 (7.1%) patients discontinued treatment prior to the end of the study. The main reasons for withdrawal were the emergence of AEs (n = 8) and lack of efficacy (n = 4).
The involvement of joints is bilateral in most of the cases. The details of the frequency and sites of the lesion distribution are shown in Table 2. Except for the interphalangeal joint involvement, the lower limb is more frequently and more severely affected than the upper limb.
Overall joint pain intensity
Celecoxib, meloxicam and paracetamol were found to be effective in the confirmatory analysis of the primary efficacy variable, the overall joint pain intensity. The mean ± SD for baseline (mm) and week 6 (mm) was 59.42 ± 13.35 and 43.263 ± 17.65 for the celecoxib group, 56.76 ± 13.5 and 34.56 ± 15.59 for the meloxicam group and 50.24 ± 17.74 and 30.71 ± 16.59 for the paracetamol group, respectively. All values at week six were lower than baseline value (all P ≤ 0.01).
Global assessment of disease activity
For the secondary endpoint, patients’ global assessment of disease activity, all three treatments (celecoxib, meloxicam and paracetamol) were significantly improving disease activity at week six (all P ≤ 0.001) (Table 3). Similarly, all three of the active treatments were significantly improving physicians’ global assessment of disease activity at week six (all P ≤ 0.001) (Table 3).
WOMAC subscale assessments
The three WOMAC subscales were assessed as secondary efficacy measures.
The WOMAC pain subscale score demonstrated that the celecoxib, meloxicam and paracetamol treatment regimens were all effective. At week six, all of the treatment groups were statistically superior to the baseline (all P < 0.01) (Fig. 1).
On the WOMAC physical function subscale, none of the treatment groups achieved statistically superior results at week six compared with baseline score (all P > 0.05) (Fig. 2).
On the WOMAC stiffness subscale, the celecoxib and meloxicam treatment groups achieved statistically superior scores compared with baseline (both P < 0.01) , but the paracetamol treatment group did not achieve statistically superior scores compared with baseline (P > 0.05) (Fig. 3).
Safety and tolerability
The majority of AEs reported were mild to moderate in intensity in all treatment groups. The incidence of any AE (i.e. including mild to severe, treatment-related and non-treatment-related) was similar across the three groups (Table 4). The most frequently reported treatment-related AEs across all treatment groups were diarrhoea, nausea, dyspepsia, oedema and skin rash. The proportion of patients experiencing at least one GI-related AE was higher among patients treated with meloxicam (27.7%) compared with celecoxib (21.1%) and paracetamol (18.1%), but the difference was not statistically significance. Oedema was generally mild in degree. No SAEs were reported in any of the three treatment groups. In general, notable abnormal laboratory test results did not follow any clinically relevant pattern in any treatment group.
Discontinuations due to AEs were similar among each of the celecoxib, meloxicam and paracetamol groups accounting for two, four and two, respectively. The number of discontinued treatment for lack of efficacy was one, one and two, respectively.
Discussion
At present, there are very little data about the treatment for KBD. Some authors use physical therapy in the treatment of patients suffering from KBD. It can relieve pain, improve mobility and thus improve the socio-economic status of patients. The physical therapy treatment uses simple techniques, is easy to learn, but needs the physiotherapist to work on a long-term basis to achieve the effects [15]. Some advanced cases had undergone surgery to improve their joint function [13]. Up to now, in the endemic area of KBD, one of the problems is pain relief for most of the patients with KBD. Patients with KBD need pain relief as well as improvement of functional disability over the short- and long-term.
The study demonstrates that celecoxib 200 mg qd is efficacious in treating the signs and symptoms of KBD and the efficacious results are consistent with the published data on the COX-2-specific inhibitor. Although non-selective NSAID can be effective for managing the pain and other symptoms of OA, the elevated risk of GI toxicity associated with these agents, due to their inhibition of the COX isoenzyme COX-1, often limits their use [16]. The discovery of a second COX isoenzyme (COX-2) and the subsequent knowledge of its tissue distribution, regulation, expression and function led to the COX-2 hypothesis: specific inhibitors of COX-2 will provide equivalent efficacy to traditional NSAID (which inhibit both COX-1 and COX-2 isoenzymes) but will result in greater GI safety [16]. Several studies have shown the efficacy of COX-2-specific inhibitors to be comparable with that of non-specific NSAID such as naproxen and diclofenac in the treatment of OA and the greater GI safety of celecoxib [17–19].
One of the objectives of this study was to evaluate the safety and efficacy of meloxicam 7.5 mg qd in patients with KBD. It proved to be effective, safe and well tolerated for the treatment of KBD and was superior to paracetamol in remission stiffness and similar to celecoxib for the primary and secondary efficacy parameters. Moreover, the uniform incidence of GI AEs was similar to that for celecoxib. Meloxicam has been approved for the treatment of OA, RA and ankylosing spondylitis. In vitro and in vivo tests have shown that meloxicam is a COX inhibitor that demonstrates more COX-2 inhibition than COX-1 inhibition at therapeutic concentrations [20, 21].
The study demonstrated the clinical efficacy of paracetamol in the treatment of pain in KBD at a three times daily dose and over 42 days. Paracetamol is the initial drug recommended for systemic treatment of symptomatic OA of the hip and knee by the American College of Rheumatology [22, 23]. It was therefore the most appropriate drug to use for comparison with other drugs in an efficacy and safety study of KBD pain control. Further treatment recommendations will have to take into account the present data, linked to the better efficacy/tolerability ratio compared with other drugs, to elaborate a more widely based treatment strategy for KBD pain. Paracetamol provided effective relief of pain from KBD, but not of stiffness. We hope the dosage of 900 mg t.i.d. will be used in the next work and that we can look forward to better results in the future.
The results presented here demonstrate the efficacy of celecoxib, meloxicam and paracetamol in relieving the symptoms from KBD [15]. In terms of overall joint pain intensity, celecoxib, meloxicam and paracetamol afforded significant pain relief over six weeks of treatment. Throughout the study, celecoxib, meloxicam and paracetamol were effective in lowering pain intensity. The secondary efficacy endpoints supported these observations. Each of the WOMAC pain subscale scores demonstrated significant differences between baseline and endpoint for the active agents. Similarly, changes in patient and physician global assessments of disease activity showed consistent significant differences. No consistent significant differences in the pain endpoints were observed among celecoxib, meloxicam and paracetamol. They were comparable in terms of efficacy to patients’ global assessment of disease activity and physicians’ global assessment of disease activity in the study.
The results support the once-daily dosing option with celecoxib and meloxicam, which has important implications for convenience and compliance with therapy. This is particularly important among elderly patients who often find multiple daily dosing regimens difficult to adhere to [24, 25].
In this study, the overall number of AEs was small in all treatment groups, and discontinuations were primarily related to AEs associated with the GI system and skin rash. There was no evidence of a relationship between the regimens and the frequency of AEs. In this study, patients were generally elderly (approximately 25% of the patients were at least 65 years of age). Therefore, this population is at high risk for GI AEs. The result is consistent with previous reports of the low rate of GI AEs with other COX-2-specific inhibitors [19, 26–29].
It is noteworthy that the proportion of patients withdrawing due to an AE were similar in the three groups receiving active treatment. This may be a random finding, but it highlights the mild severity of the symptoms experienced by patients. In general, the AE and laboratory findings were similar to those in previous studies of similar length in which similar dosages were used [18, 19]. Also the restriction of this study was that it applied to elderly patients with secondary OA lesions and not during the active phases of the disease between five and 13 years.
In summary, over the six week period of this study, celecoxib 200 mg qd, meloxicam 7.5 mg qd or paracetamol 300 mg t.i.d. provided effective relief from the symptoms of KBD (celecoxib and meloxicam for pain and stiffness, paracetamol for pain), but they all did not improve overall physical function. Additional studies of longer duration with larger patient populations evaluating the three regimens are warranted both to confirm the efficacy data from this trial as well as obtaining additional information regarding the safety of celecoxib, meloxicam and paracetamol.
References
Yang C, Niu C, Bodo M, Gabriel E, Notbohm H, Wolf E, Müller PK (1993) Fulvic acid supplementation and selenium deficiency disturb the structural integrity of mouse skeletal tissue. An animal model to study the molecular defects of Kashin-Beck disease. Biochem J 289(Pt 3):829–835
Wang Y, Yang Z, Gilula LA, Zhu C (1996) Kashin-Beck disease: radiographic appearance in the hands and wrists. Radiology 201:265–270
Chasseur C, Suetens C, Nolard N, Begaux F, Haubruge E (1997) Fungal contamination in barley and Kashin-Beck disease in Tibet. Lancet 350:1074
Haubruge E, Chasseur C, Debouck C, Begaux F, Suetens C, Mathieu F, Michel V, Gaspar C, Rooze M, Hinsenkamp M, Gillet P, Nolard N, Lognay G (2001) The prevalence of mycotoxins in Kashin-Beck disease. Int Orthop 25:159–161
Moreno-Reyes R, Suetens C, Mathieu F, Begaux F, Zhu D, Rivera MT, Boelaert M, Nève J, Perlmutter N, Vanderpas J (1998) Kashin-Beck osteoarthropathy in rural Tibet in relation to selenium and iodine status. N Engl J Med 339:1112–1120
Moreno-Reyes R, Mathieu F, Boelaert M, Begaux F, Suetens C, Rivera MT, Nève J, Perlmutter N, Vanderpas J (2003) Selenium and iodine supplementation of rural Tibetan children affected by Kashin-Beck osteoarthropathy. Am J Clin Nutr 78:137–144
La Grange M, Mathieu F, Begaux F, Suetens C, Durand MC (2001) Kashin-Beck disease and drinking water in Central Tibet. Int Orthop 25:167–169
Zhai SS, Kimbrough RD, Meng B, Han JY, LeVois M, Hou X, Yin XN (1990) Kashin-Beck disease: a cross-sectional study in seven villages in the People’s Republic of China. J Toxicol Environ Health 30:239–259
Moerman J, Uyttendaele D, Van den Broecke W, Claessens H (1992) Kashin-Beck’s disease. Acta Orthop Belg 58:227–230
Mathieu F, Begaux F, Lan ZY, Suetens C, Hinsenkamp M (1997) Clinical manifestations of Kashin-Beck disease in Nyemo Valley, Tibet. Int Orthop 21:151–156
Hinsenkamp M, Ryppens F, Begaux F, Mathieu F, De Maertelaer V, Lepeire M, Haubruge E, Chasseur C, Stallenberg B (2001) The anatomical distribution of radiological abnormalities in Kashin-Beck disease in Tibet. Int Orthop 25:142–146
Hinsenkamp M, Mathieu F, Claus W, Collard JF, de Maertelaer V (2009) Effects of physical environment on the evolution of Kashin-Beck disease in Tibet. Int Orthop 33:1085–1088
Liu FD, Wang ZL, Hinsenkamp M (1998) Osteotomy at the knee for advanced cases of Kashin-Beck disease. Int Orthop 22:87–91
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Mathieu F, Suetens C, Begaux F, De Maertelaer V, Hinsenkamp M (2001) Effects of physical therapy on patients with Kashin-Beck disease in Tibet. Int Orthop 25:191–193
FitzGerald GA, Patrono C (2001) The coxibs, selective inhibitors of cyclooxygenase-2. N Engl J Med 345:433–442
Bensen WG, Fiechtner JJ, McMillen JI, Zhao WW, Yu SS, Woods EM, Hubbard RC, Isakson PC, Verburg KM, Geis GS (1999) Treatment of osteoarthritis with celecoxib, a cyclooxygenase-2 inhibitor: a randomized controlled trial. Mayo Clin Proc 74:1095–1105
Williams GW, Ettlinger RE, Ruderman EM, Hubbard RC, Lonien ME, Yu SS, Zhao W, Geis GS (2000) Treatment of osteoarthritis with a once-daily dosing regimen of celecoxib: a randomized, controlled trial. J Clin Rheumatol 6:65–74
McKenna F, Borenstein D, Wendt H, Wallemark C, Lefkowith JB, Geis GS (2001) Celecoxib versus diclofenac in the management of osteoarthritis of the knee. Scand J Rheumatol 30:11–18
Patrignani P, Panara MR, Sciulli MG, Santini G, Renda G, Patrono C (1997) Differential inhibition of human prostaglandin endoperoxide synthase-1 and -2 by nonsteroidal anti-inflammatory drugs. J Physiol Pharmacol 48:623–631
Pairet M, van Ryn J, Schierok H, Mauz A, Trummlitz G, Engelhardt G (1998) Differential inhibition of cyclooxygenases-1 and -2 by meloxicam and its 4′-isomer. Inflamm Res 47:270–276
Hochberg MC, Altman RD, Brandt KD, Clark BM, Dieppe PA, Griffin MR, Moskowitz RW, Schnitzer TJ (1995) Guidelines for the medical management of osteoarthritis. Part I. Osteoarthritis of the hip. American College of Rheumatology. Arthritis Rheum 38:1535–1540
Hochberg MC, Altman RD, Brandt KD, Clark BM, Dieppe PA, Griffin MR, Moskowitz RW, Schnitzer TJ (1995) Guidelines for the medical management of osteoarthritis. Part II. Osteoarthritis of the knee. American College of Rheumatology. Arthritis Rheum 38:1541–1546
Eisen SA, Miller DK, Woodward RS, Spitznagel E, Przybeck TR (1990) The effect of prescribed daily dose frequency on patient medication compliance. Arch Intern Med 150:1881–1884
Salzman C (1995) Medication compliance in the elderly. J Clin Psychiatry 56(Suppl 1):18–22, discussion 23
Simon LS, Lanza FL, Lipsky PE, Hubbard RC, Talwalker S, Schwartz BD, Isakson PC, Geis GS (1998) Preliminary study of the safety and efficacy of SC-58635, a novel cyclooxygenase 2 inhibitor: efficacy and safety in two placebo-controlled trials in osteoarthritis and rheumatoid arthritis, and studies of gastrointestinal and platelet effects. Arthritis Rheum 41:1591–1602
Silverstein FE, Faich G, Goldstein JL, Simon LS, Pincus T, Whelton A, Makuch R, Eisen G, Agrawal NM, Stenson WF, Burr AM, Zhao WW, Kent JD, Lefkowith JB, Verburg KM, Geis GS (2000) Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. Celecoxib Long-term Arthritis Safety Study. JAMA 284:1247–1255
Deeks JJ, Smith LA, Bradley MD (2002) Efficacy, tolerability, and upper gastrointestinal safety of celecoxib for treatment of osteoarthritis and rheumatoid arthritis: systematic review of randomised controlled trials. BMJ 325:619
Mamdani M, Rochon PA, Juurlink DN, Kopp A, Anderson GM, Naglie G, Austin PC, Laupacis A (2002) Observational study of upper gastrointestinal haemorrhage in elderly patients given selective cyclo-oxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory drugs. BMJ 325:624
Acknowledgements
The authors gratefully acknowledge the contribution made by Bing Li (secretary).
Disclosures
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was partially supported by a grant from NSFC (Natural Science support project Item of China) 2007BA125B04 to Dr. Fuxing Pei ChiCTR-TCR-000000395.
Appendix
Appendix
Investigators
In the Medical College of Sichuan University, West China Hospital: Gang Liu, Luo Rui, Wei Liu, Yongtao Cheng, Dan Hu, Jiangang Wang, Li Li, Xin Ma, (rheumatologist), Fuxing Pei, Zongke Zhou, Jian Li, Bin Shen, Pengde Kang (orthopaedist); in the North Sichuan Medical College: JianPing Liu (rheumatologist); in the People’s Hospital of Sichuan province: JIanxin Zhu, Liuyi Tang, Chongxin Huang (orthopaedist); in the Chengdu Medical University of Chinese Medicine: Qun Gao (orthopaedist).
Rights and permissions
About this article
Cite this article
Luo, R., Liu, G., Liu, W. et al. Efficacy of celecoxib, meloxicam and paracetamol in elderly Kashin-Beck Disease (KBD) patients. International Orthopaedics (SICOT) 35, 1409–1414 (2011). https://doi.org/10.1007/s00264-010-1062-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1062-0