Abstract
Objectives
This study compares the expression levels of tumor necrosis factor ligand superfamily member 4 (TNFSF4) and TNF-R-associated factor 2 (TRAF2) mRNAs in peripheral blood mononuclear cells (PBMCs) of patients with systemic lupus erythematosus (SLE) against healthy controls. The association of SLE disease activity index (SLEDAI) and clinical features of SLE with altered expression levels of TNFSF4 and TRAF2 mRNAs were also evaluated.
Design
We used real-time reverse transcription polymerase chain reaction to measure TNFSF4 and TRAF2 mRNAs expression levels in peripheral blood mononuclear cells of 57 SLE patients and 57 healthy controls.
Results
The expression level of TNFSF4 mRNA was significantly higher in SLE patients than in the control group. Overexpression of TNFSF4 was correlated with arthritis, atherosclerosis and lupus nephritis. TRAF2 mRNA was underexpressed in PBMCs of SLE patients, and its lower expression was associated with atherosclerosis and lupus nephritis. The altered expression levels of TNFSF4 and TRAF2 mRNAs was significantly correlated with SLEDAI.
Conclusion
Our results suggest that changes in the expression levels of TNFSF4 and TRAF2 mRNAs may significantly correlate with the pathogenesis of SLE, the disease activity and different clinical features of lupus, particularly lupus nephritis, atherosclerosis and arthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by acute and chronic inflammation of multiple organs [1]. Loss of tolerance to nuclear antigens, impaired B- and T-cell signaling pathways and subsequent production of auto-reactive antibodies lead to multiple tissue and organ damage in lupus patients [2, 3]. Although the specific cause of SLE is unknown, numerous genetic, environmental and hormonal factors that contribute to the pathogenesis of this disease have been identified [4]. So far, involvement of at least 35 genes has been defined as risk factors for development of SLE [5]. Most of these genes can be categorized into three main biological processes: (1) defective immune complex processing, (2) Toll-like receptor function and induced type I interferon production and (3) impaired immune signal transduction in lymphocytes [6].
One of the powerful tools used for identification of lupus susceptibility genes is genome-wide association studies (GWAS), which suggested TNFSF4 gene regions as lupus susceptibility loci [7, 8]. Tumor necrosis factor ligand superfamily member 4 (TNFSF4), also known as OX40L, is a ligand for TNFRSF4 (OX40). It has been shown that the OX40/OX40L system is associated with the regulation of T-cell proliferation [9]. TNFSF4 is a T-cell activator that seems to promote the survival of CD4+ T cells at sites of inflammation. Also, it possibly prolongs the immune response and triggers naïve CD4+ T cells to produce pro-inflammatory cytokines including interleukin (IL)-4, IL-5 and IL-13 [10, 11]. Moreover, TNFSF4 negatively regulates the generation and function of IL-10-secreting T-regulatory cells, and thus has a pivotal role in peripheral tolerance [12]. Previous studies have shown that TNFSF4 is expressed in activated macrophages and mononuclear cells and directly activates the intracellular signaling cascades and induces cytokine production [13, 14]. Furthermore, TNFSF4 enhances B-cell proliferation and differentiation and is expressed on the surface of activated B cells. It may enhance B-cell proliferation, which leads to the cell hyperactivity found in autoimmune diseases [15]. Considering the extensive role of TNFSF4 in the immune system, it is hypothesized that impaired expression of TNFSF4 may participate in the pathogenesis of SLE.
As an accepted concept, the disturbed T-cell homeostasis has been defined as a fundamental contributor to autoimmunity. On the other hand, programmed cell death (apoptosis) has been shown to have a critical role in maintenance of homeostatic balance of the immune system. One of the key players in lymphocyte apoptosis during immune regulation is the tumor necrosis factor (TNF) superfamily [16] and the tumor necrosis factor ligands (TNF-L) and receptors (TNF-R) [17]. Regulation of TNF-R signal transduction is mediated by a range of signaling proteins, among which members of the TNF-R-associated factor (TRAF) family can be mentioned. In this family, TRAF2 is an adaptor protein and ubiquitin ligase, which mediates signal transduction of various TNF-Rs including TNFR2, CD30, CD40 and TACI [18]. It should be noted that the role of CD40-expressing T cells in peripheral tolerance and autoimmunity [19] has long been confirmed, particularly in SLE [20, 21]. Furthermore, it has been shown that TRAF2 is also involved in TNF-α-mediated activation of the non-canonical NF-κB pathway [22]. Inappropriate NF-κB activity has long been linked to various autoimmune and inflammatory diseases [23]. TNFSF4 potentially interacts with TRAF2 in order to regulate apoptosis via the NF-κB pathway [24].
Although TNFSF4 loci have been identified as a lupus susceptibility gene in recent GWASs, to the best of our knowledge no study has yet investigated the expression levels of TNFSF4 mRNA in peripheral blood mononuclear cells (PBMCs) and their correlation with disease activity and clinical manifestations in lupus patients. In the case of TRAF2, there is no report on the correlation of TRAF2 mRNA expression levels with different clinical features of lupus. In the present study, we used the real-time reverse transcription polymerase chain reaction (RT-PCR) technique to assess alterations of the expression levels of TNFSF4 and TRAF2 mRNAs in peripheral blood mononuclear cells in SLE patients and healthy controls. We also explored the correlation of expression levels of the aforementioned genes with disease activity and different clinical features of systemic lupus erythematosus.
Patients and methods
Participants
Fifty-seven patients who had been clinically confirmed to suffer from SLE were enrolled into this study and were classified according to the revised American College of Rheumatology criteria [25]. SLE activity status was evaluated by using the SLE disease activity index (SLEDAI) [26]. SLEDAI > 8 was considered as the cut-off score for active SLE.
The patients’ medication regimens were as follows: 30 individuals were on prednisolone alone and 12, seven and eight individuals were on prednisolone plus methotrexate, azathioprine or cyclosporine, respectively. The patients were compared with 57 healthy subjects with no history of autoimmune diseases. All participants signed an informed consent according to the Declaration of Helsinki. The demographic and clinical features of healthy and SLE patients are shown in Table 1.
Laboratory assessments
Samples from SLE patients were collected 6 h before they received any immunosuppressive medication. Monocytes, lymphocytes, leukocytes and neutrophils were counted in peripheral blood samples. Serum levels of IgA, IgG, IgM, C3 and C4 and erythrocyte sedimentation rate were measured in all patients. In addition, the presence of anti-nuclear antibodies was evaluated by ELISA in all SLE patients.
PBMC isolation
Whole blood (10 mL) was collected in tubes containing sodium citrate. PBMCs were isolated by density gradient centrifugation with Ficoll-Paque PREMIUM (GE Healthcare, South Korea).
Total RNA extraction
Total RNA was isolated from freshly prepared buffy coats using the QIAamp RNA Blood Mini Kit (Qiagen, Germany) according to the manufacturer’s instructions. In order to eliminate genomic DNA contamination, the RNase-free DNase set (Qiagen, Germany) was used for on-column digestion of DNA during RNA purification. The absorbance of each sample was determined at 260 nm by spectrophotometry and the OD260/OD280 ratio was calculated. The amount of RNA isolated was determined by using aNanoDrop 2000c spectrophotometer (Thermo Scientific).
Real-time reverse transcription polymerase chain reaction
Isolated RNA was reverse-transcribed into complementary DNA using the Roche transcriptor high fidelity cDNA synthesis kit as described in the manufacturer’s manual (Roche Applied Science, Germany). The expression levels of TNFSF4 and TRAF2 were quantified in SLE patients and healthy controls using a LightCycler carousel-based system (Roche Diagnostic). β-Actin was used as an internal control.
The sequences of specific forward and reverse primers used for SYBR Green real-time PCR are shown in Table 2. Polymerase chain reaction was performed using LightCycler FastStart DNA Masterplus SYBR Green I following the manufacturer’s protocol (Roche Applied Science). Samples were amplified by a 45-cycle three-step temperature profile after a single-step 10-minute denaturation at 95 °C. The complete thermal cycling condition is shown in Table 3. Each sample was run in duplicate and a negative control was run in parallel with the duplicate samples.
Melting curve analysis was performed for evaluation of specificity of the amplified PCR products and, for each sample, a single peak was detected. Relative quantification assessment was carried out using LightCycler software (Roche Diagnostic) and the results were normalized to the expression level of β-actin.
Statistical analysis
The statistical analysis was performed using SPSS software, version 19 (Chicago, IL, USA). Data were expressed as mean ± standard deviation (SD). Variables were assessed by Student’s t test. The difference between TNFSF4 and TRAF2 mRNA expression levels were determined by the Mann–Whitney test. Spearman’s rank correlation coefficient was used as a measure of the relationship between parameters. A P value less than 0.05 was considered statistically significant.
Results
The expression levels of TNFSF4 and TRAF2 mRNAs in PBMCs of SLE patients and normal controls
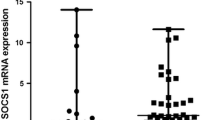
TNFSF4 and TRAF2 gene expression levels in peripheral blood cells from 57 SLE patients and 57 normal controls were assessed by real-time RT-PCR. The results revealed that the mean TNFSF4 mRNA expression level in SLE patients was significantly higher (2.639) than in healthy controls (0.526) (P < 0.001) (Fig. 1a). On the other hand, the TRAF2 gene was down-regulated in lupus patients compared to healthy controls, i.e., the mean expression level of TRAF2 mRNA in SLE patients was substantially lower (0.120) than in normal controls (0.995) (P < 0.001) (Fig. 1b).
a Expression levels of TNFSF4 mRNA in PBMCs from SLE patients (n = 57) and healthy controls (n = 57). TNFSF4 mRNA expression levels were increased in lupus patients compared with control subjects (P < 0.001). b Expression levels of TRAF2 mRNA in PBMCs from SLE patients (n = 57) and healthy controls (n = 57). TRAF2 mRNA expression levels were decreased in lupus patients compared with control subjects (P < 0.001)
Correlation of the expression levels of TNFSF4 and TRAF2 mRNAs with clinical characteristics of SLE patients
In active SLE patients, higher expression of TNFSF4 was significantly correlated with lupus nephritis (r s = 0.631), arthritis (r s = 0.342) and atherosclerosis (r s = 0.486) (P < 0.01). No substantial correlation was observed between the expression levels of TNFSF4 mRNA and other clinical features of SLE. On the other hand, in patients with active SLE, a strong correlation was detected between the decreased expression level of TRAF2 mRNA and renal dysfunction (r s = −0.497, P < 0.01). Moreover, a robust association was observed between lower levels of TRAF2 mRNA and atherosclerosis (r s = −0.367, P < 0.01).
Correlation of the expression levels of TNFSF4 and TRAF2 mRNAs with disease activity
A positive correlation was found between the mean SLEDAI score of the lupus group and the expression levels of TNFSF4 (r s = 0.316, P < 0.01) (Fig. 2a). However, the correlation of TRAF2 expression and mean SLEDAI was negative (r s = −0.279, P < 0.01) (Fig. 2b).
Discussion
In this study, using real-time RT-PCR, we explored the expression levels of TNFSF4 and TRAF2 mRNAs in PBMCs of SLE patients and compared them to those of healthy controls. TNFSF4 and TRAF2 are both involved in the same immune signaling pathway. TNFSF4 is expressed in activated T cells [27], activated B cells [28], dendritic cells [29] and endothelial cells [30]. TNFSF4 enhances the proliferation and differentiation of T lymphocytes and has a crucial role in regulating the development and survival of CD4+ T cells at sites of inflammation [31, 32]. TNFSF4 sustains the proliferation of Th1 and Th2 effector cells, and so promotes the development of the Th2 response, which in turn causes inflammation and organ-specific autoimmunity. It has been shown that impaired peripheral T-cell tolerance is a mechanism which contributes to autoimmunity [33]. Other studies have suggested the critical role of TNFSF4 in differentiation of B cells and antibody production [34]. Lastly, it has been shown that plasmacytoid dendritic cells regulate the expression of TNFSF4 and type I interferon, and so may regulate T-helper responses [35]. All these findings suggest that TNFRSF4/TNFSF4 interactions are of great importance in the immunoregulatory checkpoints and any alterations in the expression levels of TNFSF4 may result in autoimmunity. Accordingly, a previous study reported that overexpression of TNFSF4 in transgenic mice led to the spontaneous development of organ-specific inflammation [36]. In another study, targeted blockade of TNFRSF4/TNFSF4 interactions prevented the ongoing development of autoimmune diabetes and encephalomyelitis [37].
The TNFRSF4/TNFSF4 system directly stimulates TRAF2, is associated with TRAF3 and TRAF5, and has been shown to activate the NF-κB signaling pathway. NF-κB transcription factor regulates the expression of numerous genes involved in the immune response and has a central role in inflammation and apoptosis [38]. Taken together, it can be concluded that TNFSF4 and TRAF2 interaction plays a critical role in the development of T-cell-mediated autoimmunity.
In the present study, we demonstrated that TNFSF4 mRNA expression levels in PBMCs of SLE patients were higher than those in healthy controls. This is in accordance with the recent GWASs, which have shown the association of single nucleotide polymorphisms (SNPs) in the TNFSF4 gene and lupus susceptibility [7, 8, 39]. The association of the TNFSF4 gene and SLE has been shown in other studies as well. For example, Chang et al. [7] reported the association of two different SNPs of rs844648 and rs2205960 in the TNFSF4 gene locus with SLE susceptibility in the Chinese population. They also showed that TNFSF4 rs2205960 was associated with the production of anti-Ro antibodies in these patients. In another report, Zhang et al. [8] demonstrated that the association of SNP rs1234315 and the risk of development of SLE. This SNP is about 15 kb away from the 5′ end of the TNFSF4 gene and it may have potential regulatory effects on the expression levels of TNFSF4. However, due to the small sample size, they could not show any association between the levels of mRNA expression of TNFSF4 and the variant of rs1234315. In another study performed by Sanchez et al. [40] they uncovered the association of TNFSF4 rs2205960 with SLE susceptibility in American ancestors. According to the review performed by Ramos et al. [41], a few studies showed that the SNPs in TNFSF4 loci are associated with SLE susceptibility and it has been hypothesized that these SNPs might contribute to the increased expression of TNFSF4 leading to augmented T-cell activation via the TNFRSF4/TNFSF4 system.
To date, no studies have been conducted to determine the expression levels of TNFSF4 mRNA in the PBMCs of SLE patients. For the first time, in the current study we showed that the expression levels of TNFSF4 mRNA increase 2.113-fold in SLE patients compared to normal controls.
In our study, higher expression levels of TNFSF4 were correlated with atherosclerotic manifestations in SLE patients. TNFSF4 mediates T-cell adhesion to endothelial cells and varied SNPs in TNFSF4 loci have been linked to the development of atherosclerosis [42]. A previous study has shown that mice overexpressing TNFSF4 develop more atherosclerotic lesions than the normal group [43].
It was shown that in-vivo blockade of TNFRSF4/TNFSF4 in murine models not only suppressed different inflammatory symptoms, but also alleviated collagen-induced arthritis [44]. In addition, a recent GWAS found that there was a possible association between SNPs in TNFSF4 loci and arthritis in lupus patients [8]. Consistent with these findings, we also clarified that increased expression levels of TNFSF4 mRNA were strongly associated with arthritis symptoms in SLE patients.
For the first time, in the current study a robust positive correlation has been described between renal dysfunction in lupus patients and higher expression levels of TNFSF4 mRNA in PBMCs. Previously, another study reported that serum-soluble TNFSF4 was significantly higher in SLE patients with lupus nephritis, but, in contrast to our results, they could not find any association between increased serum levels of TNFSF4 and disease activity [45].
In their report, Faress et al. [45] revealed that TNFRSF4/TNFSF4 plays a critical role in the pathogenesis of SLE. They evaluated the role of TNFSF4 and its receptor as a marker of disease activity and nephritis in SLE patients. According to the results of flow cytometry, the percentage of of CD4+ T lymphocytes expressing TNFRSF4 was significantly higher in SLE patients than in controls and the higher expression of TNFRSF4 had a positive correlation with SLEDAI. It has also been reported that the expression levels of TNFRSF4 were higher in SLE patients suffering from lupus nephritis. In the same study, the serum levels of TNFSF4 were also assessed and were proven to be significantly higher in SLE patients than in healthy controls, and in patients with lupus nephritis compared with those without this complication. However, they found no significant correlation between the SLEDAI and the serum levels of TNFSF4 [45].
The association between lupus nephritis and TNFSF4 has also been investigated in a few other studies. For instance, in mice, anti-TNFSF4 treatment was successful in suppressing immune complex formation in kidney [46]. Another study reported that TNFSF4 is largely localized along the epithelial side of the glomerular capillary wall in patients with lupus [47].
Engagement of the TNFRSF4/TNFSF4 system initiates interaction with the adaptor molecules of TNF receptor associated factors (TRAFs) for downstream signaling [48]. It has been shown that the recruitment of TRAF2 mediates anti-apoptotic anti-inflammatory responses [49]. TRAF2 has long been linked to the activation of the NF-κB pathway in TNFRSF4/TNFSF4 signaling [38]. Several studies have demonstrated that the activation of the NF-κB pathway blocks apoptosis [50, 51]. It is therefore possible that the TNFRSF4-mediated NF-κB activation in T cells contributes to the prevention of T-cell apoptosis, which leads to prolonged immune responses and a variety of inflammatory and autoimmune diseases. Accordingly, the down-regulation of TRAF2 in different autoimmune diseases such as multiple sclerosis, rheumatoid arthritis and type I diabetes has been reported by performing gene assay analysis [52]. In the present study we have demonstrated that PBMCs of SLE patients expressed a TRAF2 mRNA level 0.875-fold lower than healthy controls. Underexpression of TRAF2 will lead to the disturbance of programmed cell death, and impaired apoptosis is considered to contribute to the generation of autoantibody and tissue damage in SLE patients [53].
We also observed a strong correlation between lower levels of TRAF2 mRNA in SLE patients and renal dysfunction and atherosclerosis, for which further studies are needed to explore the specific mechanisms. Our study shows that in the more severe cases of the disease, the expression levels of TRAF2 mRNA were lower. This indicates a strong negative correlation between the SLEDAI and the down-regulation of TRAF2. On the other hand, we observed a positive correlation between SLE disease activity and overexpression of TNFSF4 mRNA. It should be noted that the limited number of patients with other clinical manifestations who entered into this study rendered us unable to further explore the association of the expression levels of TRAF2 and TNFSF4 mRNAs with other clinical features of SLE.
In conclusion, our real-time RT-PCR analysis has revealed that TNFSF4 and TRAF2 mRNAs were over- and underexpressed in PBMCs of SLE patients, respectively. The expression levels of TNFSF4 and TRAF2 mRNAs were significantly correlated with lupus nephritis and atherosclerosis in lupus patients. Moreover, a robust association was detected between arthritis and up-regulation of TNFSF4 in SLE subjects. In the current study, we also demonstrated that the altered expression levels of TNFSF4 and TRAF2 mRNAs were correlated with SLEDAI. In a nutshell, these results support the possibility that TNFSF4 and TRAF2 have pivotal roles in the pathogenesis of systemic lupus erythematosus.
References
Rahman A, Isenberg DA. Systemic lupus erythematosus. N Engl J Med. 2008;358:929–39.
Weckerle CE, Franek BS, Kelly JA, Kumabe M, Mikolaitis RA, Green SL, et al. Network analysis of associations between serum interferon-alpha activity, autoantibodies, and clinical features in systemic lupus erythematosus. Arthritis Rheum. 2011;63:1044–53.
Heinlen LD, McClain MT, Merrill J, Akbarali YW, Edgerton CC, Harley JB, et al. Clinical criteria for systemic lupus erythematosus precede diagnosis, and associated autoantibodies are present before clinical symptoms. Arthritis Rheum. 2007;56(7):2344–51.
Niewold TB, Hua J, Lehman TJ, Harley JB, Crow MK. High serum IFN-alpha activity is a heritable risk factor for systemic lupus erythematosus. Genes Immun. 2007;8:492–502.
Sestak AL, Fürnrohr BG, Harley JB, Merrill JT, Namjou B. The genetics of systemic lupus erythematosus and implications for targeted therapy. Ann Rheum Dis. 2011;70(Suppl 1):i37–43.
Harley IT, Kaufman KM, Langefeld CD, Harley JB, Kelly JA. Genetic susceptibility to SLE: new insights from fine mapping and genome-wide association studies. Nat Rev Genet. 2009;10:285–90.
Chang YK, Yang W, Zhao M, Mok CC, Chan TM, Wong RW, et al. Association of BANK1 and TNFSF4 with systemic lupus erythematosus in Hong Kong Chinese. Genes Immun. 2009;10(5):414–20.
Zhang SQ, Han JW, Sun LD, Lu WS, Yin XY, Zhang XJ, et al. A single-nucleotide polymorphism of the TNFSF4 gene is associated with systemic lupus erythematosus in Chinese Han population. Rheumatol Int. 2011;31(2):227–31.
Weinberg AD, Wegmann KW, Funatake C, Whitham RH. Blocking OX-40/OX-40 ligand interaction in vitro and in vivo leads to decreased T cell function and amelioration of experimental allergic encephalomyelitis. J Immunol. 1999;162:1818–26.
Godfrey WR, Fagnoni FF, Harara MA, Buck D, Engleman EG. Identification of a human OX-40 ligand, a costimulator of CD4+ T cells with homology to tumor necrosis factor. J Exp Med. 1994;180:757–62.
Ito T, Wang YH, Duramad O, Hori T, Delespesse GJ, Watanabe N, et al. TSLP-activated dendritic cells induce an inflammatory T helper type 2 cell response through OX40 ligand. J Exp Med. 2005;202(9):1213–23.
Barrios CS, Johnson BD, Henderson DJ Jr, Fink JN, Kelly KJ, Kurup VP. The costimulatory molecules CD80, CD86 and OX40L are up-regulated in Aspergillus fumigatus sensitized mice. Clin Exp Immunol. 2005;142:242–50.
Ohshima Y, Tanaka Y, Tozawa H, Takahashi Y, Maliszewski C, Delespesse G. Expression and function of OX40 ligand on human dendritic cells. J Immunol. 1997;159:3838–48.
Lanzavecchia A, Sallusto F. Antigen decoding by T lymphocytes: from synapses to fate determination. Nat Immunol. 2001;2:487–92.
Linton PJ, Bautista B, Bierderman E, Bradley ES, Harbertson J, Kondrack RM, et al. Costimulation via OX40L expressed by B cells is sufficient to determine the extent of primary CD4 cell expansion and Th2 cytokine secretion in vivo. J Exp Med. 2003;197:875–83.
Chan KF, Siegel MR, Lenardo JM. Signaling by the TNF receptor superfamily and T cell homeostasis. Immunity. 2000;13(4):419–22.
Locksley R, Killeen N, Lenardo M. The TNF and TNF receptor superfamilies integrating mammalian biology. Cell. 2001;104:487–501.
Aggarwal BB. Signaling pathways of the TNF superfamily a double-edged sword. Nat Rev Immunol. 2003;3:745–56.
Giuliani C, Napolitano G, Bucci I, Montani V, Monaco F. NF-kB transcription factor: role in the pathogenesis of inflammatory, autoimmune, and neoplastic diseases and therapy implications. Clin Ter. 2001;152(4):249–53.
Toubi E, Shoenfeld Y. The role of CD 40–CD 154 interactions in autoimmunity and the benefit of disrupting this pathway. Autoimmunity. 2004;37:457–64.
Quezada SA, Eckert M, Adeyi OA, Schned AR, Noelle RJ, Burns CM. Distinct mechanisms of action of anti-CD 154 in early versus late treatment of murine lupus nephritis. Arthritis Rheum. 2003;48:2541–54.
Bradley JR, Pober JS. Tumor necrosis factor receptor-associated factors (TRAFs). Oncogene. 2001;20(44):6482–91.
Hayden MS, West AP, Ghosh S. NF-κB and the immune response. Oncogene. 2006;25(51):6758–80.
Arch RH, Thompson CB. 4–1BB and Ox40 are members of a tumor necrosis factor (TNF)-nerve growth factor receptor subfamily that bind TNF receptor-associated factors and activate nuclear factor kappa B. Mol Cell Biol. 1998;18(1):558–65.
Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40:1725.
Gladman DD, Ibanez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol. 2002;29:288–91.
Takasawa N, Ishii N, Higashimura N, Murata K, Tanaka Y, Nakamura M, et al. Expression of gp34 (OX40 ligand) and OX40 on human T cell clones. Jpn J Cancer Res. 2001;92:377.
Stüber E, Strober W. The T cell-B cell interaction via OX40-OX40L is necessary for the T cell-dependent humoral immune response. J Exp Med. 1996;183:979.
Murata K, Ishii N, Takano H, Miura S, Ndhlovu LC, Nose M, et al. Impairment of antigen-presenting cell function in mice lacking expression of OX40 ligand. J Exp Med. 2000;191:365.
Imura A, Hori T, Imada K, Ishikawa T, Tanaka Y, Maeda M, et al. The human OX40/gp34 system directly mediates adhesion of activated T cells to vascular endothelial cells. J Exp Med. 1996;183:2185.
Maxwell JR, Weinberg A, Prell RA, Vella AT. Danger and OX40 receptor signaling synergize to enhance memory T cell survival by inhibiting peripheral deletion. J Immunol. 2000;164:107.
Gramaglia I, Jember A, Pippig SD, Weinberg AD, Killeen N, Croft M. The OX40 costimulatory receptor determines the development of CD4 memory by regulating primary clonal expansion. J Immunol. 2000;165:3043.
Bansal-Pakala P, Gebre-Hiwot Jember A, Croft M. Signaling through OX40 (CD134) breaks peripheral T-cell tolerance. Nature Med. 2001;7:907–12.
Kato H, Kojima H, Ishii N, Hase H, Imai Y, Fujibayashi T, et al. Essential role of OX40L on B cells in persistent alloantibody production following repeated alloimmunizations. J Clin Immunol. 2004;24(3):237–48.
Ito T, Amakawa R, Inaba M, Hori T, Ota M, Nakamura K, et al. Plasmacytoid dendritic cells regulate Th cell response through OX40 ligand and type I IFNs. J Immunol. 2004;172(7):4253–9.
Murata K, Nose M, Ndhlovu LC, Sato T, Sugamura K, Ishii N. Constitutive OX40/OX40 ligand interaction induces autoimmune-like diseases. J Immunol. 2002;169(8):4628–36.
Pakala SV, Bansal-Pakala P, Halteman BS, Croft M. Prevention of diabetes in NOD mice at a late stage by targeting OX40/OX40 ligand interactions. Eur J Immunol. 2004;34(11):3039–46.
Kawamata S, Hori T, Imura A, Takaori-Kondo A, Uchiyama T. Activation of OX40 signal transduction pathways leads to tumor necrosis factor receptor-associated factor (TRAF) 2- and TRAF5-mediated NF-kappaB activation. J Biol Chem. 1998;273(10):5808–14.
Zhou XJ, Lu XL, Nath SK, Lv JC, Zhu SN, Yang HZ, et al. Gene-gene interaction of BLK, TNFSF4, TRAF1, TNFAIP3, and REL in systemic lupus erythematosus. Arthritis Rheum. 2012;64(1):222–31.
Sanchez E, Webb RD, Rasmussen A, Kelly JA, Riba L, Kaufman KM, et al. Genetically determined Amerindian ancestry correlates with increased frequency of risk alleles for systemic lupus erythematosus. Arthritis Rheum. 2010;62(12):3722–9.
Ramos PS, Brown EE, Kimberly RP, Langefeld CD. Genetic factors predisposing to systemic lupus erythematosus and lupus nephritis. Semin Nephrol. 2010;30(2):164–76.
Olofsson PS, Söderström LA, Jern C, Sirsjö A, Ria M, Sundler E, et al. Genetic variants of TNFSF4 and risk for carotid artery disease and stroke. J Mol Med. 2009;87(4):337–46.
Wang X, Ria M, Kelmenson PM, Eriksson P, Higgins DC, Samnegard A, et al. Positional identification of TNFSF4, encoding OX40 ligand, as a gene that influences atherosclerosis susceptibility. Nat Genet. 2005;37:365–72.
Yoshioka T, Nakajima A, Akiba H, Ishiwata T, Asano G, Yoshino S, et al. Contribution of OX40/OX40 ligand interaction to the pathogenesis of rheumatoid arthritis. Eur J Immunol. 2000;30:2815.
Farres MN, Al-Zifzaf DS, Aly AA. Abd Raboh NM. OX40/OX40L in systemic lupus erythematosus: association with disease activity and lupus nephritis. Ann Saudi Med. 2011;31(1):29–34.
Foell J, Strahotin S, O’Neil SP, McCausland MM, Suwyn C, Haber M, et al. CD137 co-stimulatory T cell receptor engagement reverses acute disease in lupus-prone NZB x NZW F1 mice. J Clin Invest. 2003;111:1505–18.
Aten J, Roos A, Claessen N, Schilder-Tol EJ, ten Berge IJ, Weening JJ. Strong and selective glomerular localization of CD134 ligand and TNF receptor-1 in proliferative lupus nephritis. J Am Soc Nephrol. 2000;11:1426–38.
Xie P, Hostager BS, Munroe ME, Moore CR, Bishop GA. Cooperation between TNF receptor-associated factors 1 and 2 in CD40 signaling. J Immunol. 2006;176:5388–400.
Baud V, Karin M. Signal transduction by tumor necrosis factor and its relatives. Trends Cell Biol. 2001;9(11):372–7.
Van Antwerp DJ, Martin SJ, Kafri T, Green DR, Verma IM. Suppression of TNF-alpha-induced apoptosis by NF-kappa B. Science. 1996;274(5288):787–9.
Beg AA, Baltimore D. An essential role for NF-kappaB in preventing TNF-alpha-induced cell death. Science. 1996;274(5288):782–4.
Maas K, Chan S, Parker J, Slater A, Moore J, Olsen N, et al. Cutting edge: molecular portrait of human autoimmune disease. J Immunol. 2002;169:5–9.
Gordon C, Salmon M. Update on systemic lupus erythematosus: autoantibodies and apoptosis. Clin Med. 2001;1:10–4.
Acknowledgments
This research was supported by a research grant from Tehran University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: John Di Battista.
P. Rajabi and M. Alaee contributed equally to this work.
Rights and permissions
About this article
Cite this article
Rajabi, P., Alaee, M., Mousavizadeh, K. et al. Altered expression of TNFSF4 and TRAF2 mRNAs in peripheral blood mononuclear cells in patients with systemic lupus erythematosus: association with atherosclerotic symptoms and lupus nephritis. Inflamm. Res. 61, 1347–1354 (2012). https://doi.org/10.1007/s00011-012-0535-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-012-0535-6