Abstract
Allergic rhinitis (AR) is an IgE-mediated inflammation which causes olfactory dysfunction. Antihistamines have been widely used to treat AR while few studies have investigated the effect of antihistamines on improving the sense of smell. In addition, the underlying mechanisms are not well elucidated. We established the ovalbumin (OVA)-induced allergic rhinitis rat model and administrated desloratadine to AR rats. The AR symptoms, serum level of OVA-specific IgE and IL-17, and expression of IL-4, IL-5 and IL-13 in nasal mucosa were measured. The olfactory dysfunction was monitored by buried food test and the expression of GluR1 was measured. Desloratadine treatment alleviated AR symptoms, decreased serum level of OVA-specific IgE and IL-17 in AR rats. Desloratadine decreased IL-4, IL-5, and IL-13 expression in nasal mucosa of AR rats. Desloratadine ameliorated olfactory dysfunction in AR rats and decreased GluR1 expression in AR rats. Desloratadine treatment alleviated AR symptoms and ameliorated olfactory dysfunction in AR rats. The expression of AMPA receptor subunit GluR1 in olfactory bulb was associated with olfactory disorder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Allergic rhinitis (AR), also known as hay fever, is a type of nasal inflammation which occurs when the immune system overreacts to environmental allergens such as pollen, dust, mold or pet hair. The symptoms of AR include sneezing, nasal pruritus, airflow obstruction, and mostly clear nasal discharge (Bousquet et al. 2008).
AR is one of the most common diseases and represents a global health problem, currently affecting up to 30% of the population and with a continuously increasing prevalence and significant comorbidities and complications (Licari et al. 2014). The underlying mechanisms involve IgE-mediated reactions against inhaled allergens and mucosal inflammation driven by type 2 helper T (Th2) cells. Th2 lymphocytes secrete several cytokines including IL-4, IL-5, IL-19 and IL-13. IL-4 is essential to induce the isotype switch from IgM to IgE in B cells while IL-5 stimulates the production and survival of eosinophils in nasal tissue, and induces eosinophilic inflammation (Greiner et al. 2011; Greiner and Meltzer 2011). Drug treatment is the major cornerstone of AR management which is mainly based on antihistamines and intranasal corticosteroids (INCSs).
AR is also the main cause of olfactory dysfunction (Guilemany et al. 2009). Olfactory disorder is very common and 1.2% of patients with olfactory disorder have a permanent loss and 62.4% have a temporary loss of the sense of smell (Wang et al. 2017). The α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (also known as AMPA receptor, AMPAR, or quisqualate receptor) is an ionotropic transmembrane receptor for glutamate that mediates fast synaptic transmission in the central nervous system. GluR-A to D, four AMPAR constituents, form tetrameric channel with different binary subunit combinations. Among them, GluR-B is contained in the majority of AMPARs (Petralia et al. 2004). The AMPA receptors have been identified in olfactory bulb and the contribution of AMPAR to olfactory processing in the olfactory bulb has been described (Blakemore et al. 2006). Shimshek et al. (2005) also reported that modification of AMPARs affected olfactory memory and discrimination. However, there is no previous report about the potential effects of AMPARs on olfactory disorder in AR.
Antihistamines have been widely used to treat AR while few studies have investigated the effect of antihistamines improving the sense of smell. In addition, the underlying mechanisms are not well elucidated (Guilemany et al. 2012; Marino-Sanchez et al. 2018). In current study, we utilized the well-established ovalbumin (OVA)-induced allergic rhinitis rat model and evaluated the effects of the antihistamines desloratadine on allergic rhinitis and olfactory disorder.
Materials and Methods
Animals
Ten weeks Sprague–Dwaley rats weighing 220–280 g were purchased from Beijing Vital River Laboratory Animal Technology Co., Ltd. (Beijing, China). The rats were housed in animal facility with automatically adjusted day–night cycle, temperature (24 ± 2 °C), and humidity (45 ± 3%) values. Food and water were available ad libitum in home cages. This experiment was performed according to the guidelines in Affiliated Hospital of Qingdao University and approved by the Ethics of the Institutional Animal Care and Use Committee in Affiliated Hospital of Qingdao University.
AR Model and Experimental Design
The AR model was established using an OVA sensitization method. Rats were divided into five groups. To induce model of AR, rats were sensitized via intraperitoneal (i.p.) injection of 0.3 mg OVA emulsified in 30 mg AL(OH)3 (OVA/alum) every other day for 2 weeks. Following the i.p. immunization, the rats were challenged by intranasal dripping of 20 μl of 0.1 mg/mL OVA daily for 2 weeks (Group B) or 6 weeks (Group C). For Group D, rats were challenged daily for total 10 weeks. After 6 weeks challenge, Group D rats were i.p. injected with desloratadine (3 mg/kg, daily) for 4 weeks. Rats in Group E were rats were challenged daily for total 6 weeks and then treated with desloratadine for 4 weeks. Control group (Group A) rats were received i.p. and intranasal administration of phosphate-buffered saline (PBS) solution. All animals were closely observed for development of any nasal responses of sneezing, nasal rubbing events for 10 min.
ELISA
Blood samples were collected. The serum level of OVA-specific IgE was measured using anti-ovalbumin IgE (mouse) ELISA Kit (Cayman Chemical, Ann Harbor, MI, USA), and IL-17 was measured using mouse IL-17 DuoSet ELISA kit (R&D Systems, Inc. Minneapolis, MN, USA) according to manufacturer’s protocol.
Western Blot
Nasal mucosa was removed and the total protein was extracted using M-PER mammalian protein extraction reagent (Thermo Fisher, Waltham, MA, USA). The olfactory bulb was isolated and total proteins were extracted using Total Protein Extraction Kit (Novus biologicals, Centennial, CO, USA). After measuring protein concentration using Bradford Protein Assay (Bio-rad, Hercules, CA, USA), total 25 µg protein was loaded on 12% SDS–PAGE and then transfer to PVDF membrane. After blocking with 5% non-fat milk (Bio-Rad, USA) for 1 h at room temperature, the membranes were incubated with different primary antibodies: anti-IL-4 (Abcam, Cambridge, MA, USA), anti-IL-5 (R&D Systems, USA), anti-IL-13 (R&D Systems, USA), anti- Anti-Glutamate Receptor 1 (Abcam, USA) and anti-β actin (Sigma, St Louis, MO, USA). The primary antibodies were incubated at 4 °C for overnight. Next day, horseradish peroxidase (HRP)-conjugated corresponding secondary antibodies were incubated at room temperature for 1 h. Peroxidase reaction was visualized by the SuperSignal West Pico Chemiluminenscent Substrate Kit (Thermo Scientific, USA). The signal intensities were quantified using software ImageJ.
Buried Food Test
The buried food test (BFT) was performed to examine olfactory disorder as described previously (Wang et al. 2017). Food pellets were randomly buried in the litter at depths of 1–2 cm. The food-deprived rats from different treatment groups were placed into the location of the experiment. The time from when the rat was put into the location until it grasped the food pellet was recorded.
Real-Time PCR
Total RNA of olfactory bulb was isolated using RNeasy mini kit (Qiagen, Germantown, MD, USA). The Quatitect reverse transcription kit (Qiagen, USA) was used to synthesize the subsequent cDNA. Real-time PCR (RT-PCR) was performed using SYBR Green Master Mix (Qiagen, USA) following manufacturer’s instructions and on a QuantStudio 3 Real-Time PCR System (Thermo Fisher, USA). GAPDH was used as the internal control. Primer sequences used for RT-PCR were: GluR1 Forward: 5′-GAGCAACGAAAGCCCTGTGA-3′, Reverse: 5′-CCCTTGGGTGTCGCAATG-3′. GAPDH forward 5′-TGATTCTACCCACGGC AAGTT-3′. Reverse 5′-TGATGG GTTTCCCATTGATGA-3′.
Statistical Aanalysis
One-way ANOVA analysis followed a Tukey’s post hoc test was used for statistical analysis. Statistical difference was considered as significant only if p < 0.05.
Results
Establishment of the AR Rat Model Using OVA
To carefully evaluate the protective effects of desloratadine on RA and explore the underlying mechanisms, we first established the AR rat model as described previously using OVA (Aswar et al. 2015). The administration of desloratadine to the AR rat was described in detail in Materials and Methods and shown in Fig. 1.
Schematic representation of the experimental protocol. To induce model of allergic rhinitis (AR), rats were sensitized via intraperitoneal injection of 0.3 mg ovalbumin (OVA) emulsified in 30 mg AL(OH)3 (OVA/alum) for 2 weeks (every other day). And then the rats were challenged by instilling a 20 μL droplet of OVA (0.1 mg/mL) into each nostril using a micropipette daily for 2 weeks (group B) or 6 weeks (Group C). For Desloratadine treatment, AR rats were intraperitoneal injected with desloratadine (3 mg/kg, daily) for 4 weeks with (Group D) or without continuous OVA challenge (Group E). Rats received intraperitoneal and intranasal administration of PBS solution were set as control group (Group A). The symptom of AR in different groups was examined on predetermined days
Desloratadine Decreased the Sneezing and Nasal Rubbing Events in AR Rats
Next, we monitored the sneezing and nasal rubbing events among different group of rats. As shown in Fig. 2, rats sensitized and challenged with OVA for 4 and 8 weeks had greatly increased frequencies of sneezing (Fig. 2a) and nasal rubbing (Fig. 2b) events when compared to normal rats. In contrast, rats sensitized and challenged with OVA for 12 weeks with desloratadine treatment in the last 4 weeks (AR 12 week group), and rats sensitized and challenged with OVA for 8 weeks and then treated with desloratadine for 4 weeks (AR 8-week group) displayed significantly decreased frequencies of both sneezing (Fig. 2a) and nasal rubbing (Fig. 2b) when compared to rats sensitized and challenged with OVA for 8 weeks. Interestingly, rats sensitized and challenged with OVA for 8 weeks and then treated with desloratadine for 4 weeks (AR 8-week group) had significantly lower frequencies of sneezing and nasal rubbing events than rats sensitized and challenged with OVA for 12 weeks with desloratadine treatment in the last 4 weeks (AR 12-week group), indicating longer challenge of OVA diminished the desloratadine-mediated prevention of sneezing and nasal rubbing events in AR rats.
Desloratadine Decreased Serum Levels of OVA-Specific IgE and IL-17 in AR Rats
We next measured the serum levels of OVA-specific IgE and IL-17 in AR rats after desloratadine treatment. As shown in Fig. 3a, rats sensitized and challenged with OVA for 4 and 8 weeks had greatly increased OVA-specific IgE in serum when compared to normal rats. In contrast, rats sensitized and challenged with OVA for 12 weeks with desloratadine treatment in the last 4 weeks (AR 12-week group), and rats sensitized and challenged with OVA for 8 weeks and then treated with desloratadine for 4 weeks (AR 8-week group) had significantly decreased serum level of OVA-specific IgE. Longer challenge of OVA diminished the dampened of serum OVA-specific IgE by desloratadine in AR rats as we detected significantly increased serum OVA-specific IgE level in rats sensitized and challenged with OVA for 12 weeks with desloratadine treatment in the last 4 weeks (AR 12-week group) when compared to rats sensitized and challenged with OVA for 8 weeks and then treated with desloratadine for 4 weeks (AR 8-week group). Similar result could be obtained for serum IL-17 level (Fig. 3b). Taken together, our data demonstrated that desloratadine decreased serum levels of OVA-specific IgE and IL-17in AR rats.
Desloratadine Decreased Expressions of IL-4, IL-5 and IL-13 in Nasal Mucosa of AR Rats
The expressions of IL-4, IL-5 and IL-13 in nasal mucosa of AR rats were measured. As shown in Fig. 4a, b, there was obviously increased IL-4 expression in nasal mucosa of rats sensitized and challenged with OVA for 4 and 8 weeks. In contrast, we detected greatly decreased IL-4 expression in nasal mucosa of rats sensitized and challenged with OVA for 12 weeks with desloratadine treatment in the last 4 weeks (AR 12-week group), and rats sensitized and challenged with OVA for 8 weeks and then treated with desloratadine for 4 weeks (AR 8-week group). Rats sensitized and challenged with OVA for 8 weeks and then treated with desloratadine for 4 weeks (AR 8-week group) had obviously significantly less IL-4 expression in nasal mucosa than rats sensitized and challenged with OVA for 12 weeks with desloratadine treatment in the last 4 weeks (AR 12-week group). We obtained similar results for IL-5 (Fig. 4c, d) and IL-13 (Fig. 4e, f) expression. Collectively, our data demonstrated that desloratadine decreased expression of IL-4, IL-5 and IL-13 in nasal mucosa of AR rats.
Desloratadine Enhanced Olfactory Function in AR Rats
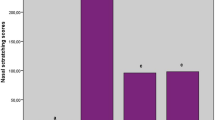
We performed the BFT to determine the effects of desloratadine on the olfactory function of AR rats. As shown in Fig. 5, normal rats in the control group could find buried food pellets within 200 s. In contrast, rats sensitized and challenged with OVA for 4 and 8 weeks spent longer time to find buried food pellets when compared to normal rats, indicating the impaired olfactory function in AR rats. Rats sensitized and challenged with OVA for 12 weeks with desloratadine treatment in the last 4 weeks (AR 12-week group), and rats sensitized and challenged with OVA for 8 weeks and then treated with desloratadine for 4 weeks (AR 8-week group) spent significantly shorter time to find buried food pellets than rats sensitized and challenged with OVA for 8 weeks. Interestingly, the time rats sensitized and challenged with OVA for 8 weeks and then treated with desloratadine for 4 weeks (AR eight-week group) spent to find buried food pellets was significantly shorter than that AR 12-week group rat spent, indicating desloratadine had better effects in rats with shorter OVA challenge.
Performance of different rats on buried and visible pellet tests. Food pellets were randomly buried in the litter at depths of 1–2 cm. Next, the rats were placed into the location of the experiment and the time spent finding the balls was recorded. Data represent means ± SD. n = 8, **p < 0.01, ***p < 0.001
Desloratadine Decreased GlutR1 Expression in Olfactory Bulbs of AR Rats
Finally, we measured the Glutamate receptor 1 (GlutR1) expression in olfactory bulbs of AR rats after desloratadine treatment. As shown in Fig. 6a, significantly increased mRNA levels of GlutR1 were detected in olfactory bulbs of rats sensitized and challenged with OVA for 4 and 8 weeks. In contrast, significantly decreased GlutR1 mRNA expressions were detected in olfactory bulbs of rats sensitized and challenged with OVA for 12 weeks with desloratadine treatment in the last 4 weeks (AR 12-week group), and rats sensitized and challenged with OVA for 8 weeks and then treated with desloratadine for 4 weeks (AR 8-week group). In addition, the mRNA level of GlutR1 in olfactory bulbs of rats sensitized and challenged with OVA for 8 weeks and then treated with desloratadine for 4 weeks (AR 8-week group) was significantly lower than that of rats in AR 12-week group. Consistently, we obtained similar profile of GlutR1 protein expression (Fig. 6b, c). Taken together, our data demonstrated that desloratadine decreased GlutR1 expression in olfactory bulbs of AR rats.
a The mRNA levels of Glut R1 in olfactory bulbs from mice of different groups were detected via real-time PCR. The levels of GluR1 were normalized to Control mice. Western blotting (b) and densitometric analysis (c) of GluR1 in olfactory bulbs from mice of different groups. β-Actin was used as a loading control. The signal intensities were quantified using software ImageJ (version 1.47). Data are shown as means ± SD, n = 3 independent replicates from a single experiment. **p < 0.01, ***p < 0.001
Discussion
AR, characterized by rhinorrhea, nasal itching, nasal congestion, sneezing and itching, has become increasingly prevalent over the world. Olfactory dysfunction is a key symptom in patients with AR. However, few researches have tested olfactory function in AR and the efficacy of AR treatment in restoring the sense of smell. In current study, we evaluated the effects of desloratadine, an antihistamine commonly used to treat AR, on AR as well as olfactory dysfunction in OVA-induced allergic rhinitis rat. The underlying mechanisms were further explored. We demonstrated that desloratadine significantly alleviated the AR symptoms, decreased the serum level of OVA-specific IgE and IL-17, and decreased the protein level of IL-4, IL-5 and IL-13 in nasal mucosa. More important, desloratadine alleviated olfactory dysfunction in AR rats as desloratadine-treated rats had less latency in buried pellet tests. We further demonstrated that desloratadine decreased the GlutR1 expression, suggesting the correlation of GlutR1 expression and olfactory dysfunction.
H1 antihistamines and INCSs are the major pharmacological agents used in AR treatment (Licari et al. 2014). There are more than 45 H1 antihistamines available worldwide. Antihistamines function to block receptors and downregulate allergic inflammation by interfering with histamine action at H1-receptors on sensory neurons and small blood vessels. H1-antihistamines also decrease antigen presentation, expression of proinflammatory cytokines and cell adhesion molecules and chemotaxis. Desloratadine is a tricyclic H1 antagonist and widely used to treat allergic rhinitis (Bachert 2009; Bachert and van Cauwenberge 2007; DuBuske 2005). In current study, we confirmed the protective effects of desloratadine on AR. The frequencies of sneezing and nasal rubbing were significantly decreased after desloratadine treatment in AR rats.
AR is partially mediated by the innate immune system, and inflammatory cytokines play important role in innate immune (Gao et al. 2017; Huang et al. 2018; Zhang et al. 2019). Importantly, AR is an IgE-mediated inflammatory disease. In AR, cross-linking of IgE molecules upon allergen contact induces degranulation of mast cells and basophils, and results in the release of typical mediators and finally causes the well-known symptoms (Verbruggen et al. 2009). In current study, we demonstrated that desloratadine treatment significantly decreased the serum level of OVA-specific IgE, which could contribute to the protective effects of desloratadine. Targeting IgE has been proved to be an effective approach to treat allergic diseases including AR (Corsico et al. 2017; Galli and Tsai 2012; Verbruggen et al. 2009). Omalizumab (rhuMAb-E25) is a recombinant humanized IgG1 monoclonal antibody which specifically binds to the high affinity FcR1 domain of free circulating IgE and prevents binding of free serum IgE to mast cells and other effector cells. Studies have described the efficacy of omalizumab to treat AR (Masieri et al. 2016; Tsabouri et al. 2014).
IL-17 is produced by Th17 cells and known to induce activation of allergen-specific Th2 cell, accumulation of eosinophil and neutrophil, and production of serum IgE in AR. Neutralization of IL-17 markedly reduced AR symptoms, decreased eosinophil and neutrophil infiltration and increased Treg response (Gu et al. 2017). IL-4 and IL-5 are Th2-type cytokines and are believed to be important in nasal inflammation through the recruitment of eosinophils. Similar to IL-4, IL-13 induced IgE switching and upregulation of vascular cell adhesion molecule-1 (Ghaffar et al. 1997). Elevated expressions of IL-4, IL-5 and IL-13 have been detected to be associated with AR. In current study, we also detected increased expressions of all three cytokines while desloratadine treatment inhibited the expressions of these cytokines.
Hyposmia is a common condition associated with allergic rhinitis. It is likely due to both a mechanical component (i.e., blockage of the nasal airways through mucosal congestion) and an inflammatory component (Guss et al. 2009; Klimek and Eggers 1997). In current study, we found impaired olfactory function in AR rats while desloratadine treatment ameliorated the olfactory dysfunction in AR rats. The mechanism of action of desloratadine in the treatment for olfactory dysfunction is not fully understood yet. The AMPA receptors are composed of four types of subunits, designated as GluA1 (GluR1), GluA2 (GluR2), GluA3 (GluR3), and GluA4 (GluR4). Most AMPARs are heterotetrameric, consisting of symmetric “dimer of dimmers” of GluA2 and either GluA1, GluA3 or GluA4 (Greger et al. 2007). Interestingly, our study identified the increased GluA1 expression in AR rats while desloratadine treatment significantly decreased the GluA1 level in AR rats. This correlation suggested the potential role of GluA expression in olfactory function. However, the underlying mechanisms need to be further explored. The regulation of GluA expression in AR is never described before. It is worthy of detecting expression of other three subunits in AR rats and in drug-treated AR rats. In addition, besides AMPARs, the N-methyl-d-aspartate (NMDA) receptors and kainate receptors mediate the glutamate transmission in excitatory synaptic circuits. The regulatory role of NMDA receptor and kainite receptors on olfaction has been described (Blakemore et al. 2018; Lee et al. 2016; Lethbridge et al. 2012). Therefore, it is worthy to evaluate their role in AR too. Desloratadine treatment alleviated AR symptoms and ameliorated olfactory dysfunction. The expression of AMPA receptor subunit GluR1 in olfactory bulb was associated with olfactory disorder.
References
Aswar U, Shintre S, Chepurwar S et al (2015) Antiallergic effect of piperine on ovalbumin-induced allergic rhinitis in mice. Pharm Biol 53:1358–1366
Bachert C (2009) A review of the efficacy of desloratadine, fexofenadine, and levocetirizine in the treatment of nasal congestion in patients with allergic rhinitis. Clin Ther 31:921–944
Bachert C, van Cauwenberge P (2007) Desloratadine treatment for intermittent and persistent allergic rhinitis: a review. Clin Ther 29:1795–1802
Blakemore LJ, Resasco M, Mercado MA et al (2006) Evidence for Ca(2 +)-permeable AMPA receptors in the olfactory bulb. Am J Physiol Cell Physiol 290:C925–C935
Blakemore LJ, Corthell JT, Trombley PQ (2018) Kainate receptors play a role in modulating synaptic transmission in the olfactory bulb. Neuroscience 391:25–49
Bousquet J, Khaltaev N, Cruz AA et al (2008) Allergic rhinitis and its impact on asthma (ARIA) 2008 update (in collaboration with the world health organization, GA(2)LEN and AllerGen). Allergy 63(Suppl 86):8–160
Corsico AG, De Amici M, Ronzoni V et al (2017) Allergen-specific immunoglobulin E and allergic rhinitis severity. Allergy Rhinol 8:1–4
DuBuske LM (2005) Review of desloratadine for the treatment of allergic rhinitis, chronic idiopathic urticaria and allergic inflammatory disorders. Expert Opin Pharmacother 6:2511–2523
Galli SJ, Tsai M (2012) IgE and mast cells in allergic disease. Nat Med 18:693–704
Gao Z, Li Y, Wang F et al (2017) Mitochondrial dynamics controls anti-tumour innate immunity by regulating CHIP-IRF1 axis stability. Nat Commun 8:1805
Ghaffar O, Laberge S, Jacobson MR et al (1997) IL-13 mRNA and immunoreactivity in allergen-induced rhinitis: comparison with IL-4 expression and modulation by topical glucocorticoid therapy. Am J Respir Cell Mol Biol 17:17–24
Greger IH, Ziff EB, Penn AC (2007) Molecular determinants of AMPA receptor subunit assembly. Trends Neurosci 30:407–416
Greiner AN, Meltzer EO (2011) Overview of the treatment of allergic rhinitis and nonallergic rhinopathy. Proc Am Thorac Soc 8:121–131
Greiner AN, Hellings PW, Rotiroti G et al (2011) Allergic rhinitis. Lancet 378:2112–2122
Gu ZW, Wang YX, Cao ZW (2017) Neutralization of interleukin-17 suppresses allergic rhinitis symptoms by downregulating Th2 and Th17 responses and upregulating the Treg response. Oncotarget 8:22361–22369
Guilemany JM, García-Piñero A, Alobid I et al (2009) Persistent allergic rhinitis has a moderate impact on the sense of smell, depending on both nasal congestion and inflammation. Laryngoscope 119:233–238
Guilemany JM, García-Piñero A, Alobid I et al (2012) The loss of smell in persistent allergic rhinitis is improved by levocetirizine due to reduction of nasal inflammation but not nasal congestion (the CIRANO study). Int Arch Allergy Immunol 158:184–190
Guss J, Doghramji L, Reger C et al (2009) Olfactory dysfunction in allergic rhinitis. ORL J Otorhinolaryngol Relat Spec 71:268–272
Huang T, Gao Z, Zhang Y et al (2018) CRL4(DCAF2) negatively regulates IL-23 production in dendritic cells and limits the development of psoriasis. J Exp Med 215:1999–2017
Klimek L, Eggers G (1997) Olfactory dysfunction in allergic rhinitis is related to nasal eosinophilic inflammation. J Allergy Clin Immunol 100:158–164
Lee JH, Wei L, Deveau TC et al (2016) Expression of the NMDA receptor subunit GluN3A (NR3A) in the olfactory system and its regulatory role on olfaction in the adult mouse. Brain Struct Funct 221:3259–3273
Lethbridge R, Hou Q, Harley CW et al (2012) Olfactory bulb glomerular NMDA receptors mediate olfactory nerve potentiation and odor preference learning in the neonate rat. PLoS One 7:e35024
Licari A, Ciprandi G, Marseglia A et al (2014) Current recommendations and emerging options for the treatment of allergic rhinitis. Expert Rev Clin Immunol 10:1337–1347
Marino-Sanchez F, Valls-Mateus M, Haag O et al (2018) Smell loss is associated with severe and uncontrolled disease in children and adolescents with persistent allergic rhinitis. J Allergy Clin Immunol Pract 6(1752–1755):e3
Masieri S, Cavaliere C, Begvarfaj E et al (2016) Effects of omalizumab therapy on allergic rhinitis: a pilot study. Eur Rev Med Pharmacol Sci 20:5249–5255
Petralia RS, Sans N, Wang YX et al (2004) Loss of GLUR2 alpha-amino-3-hydroxy-5-methyl-4-isoxazoleproprionic acid receptor subunit differentially affects remaining synaptic glutamate receptors in cerebellum and cochlear nuclei. Eur J Neurosci 19:2017–2029
Shimshek DR, Bus T, Kim J et al (2005) Enhanced odor discrimination and impaired olfactory memory by spatially controlled switch of AMPA receptors. PLoS Biol 3:e354
Tsabouri S, Tseretopoulou X, Priftis K et al (2014) Omalizumab for the treatment of inadequately controlled allergic rhinitis: a systematic review and meta-analysis of randomized clinical trials. J Allergy Clin Immunol Pract 2(332–340):e1
Verbruggen K, Van Cauwenberge P, Bachert C (2009) Anti-IgE for the treatment of allergic rhinitis–and eventually nasal polyps? Int Arch Allergy Immunol 148:87–98
Wang X, Zhu Y, Ni D et al (2017) Intranasal application of glucocorticoid alleviates olfactory dysfunction in mice with allergic rhinitis. Exp Ther Med 14:3971–3978
Zhang Y, Liu RB, Cao Q et al (2019) USP16-mediated deubiquitination of calcineurin A controls peripheral T cell maintenance. J Clin Invest 129:2856–2871
Acknowledgements
None.
Funding
The study was supported by the National Natural Science Foundation of China (81770978); Shandong Key R&D Program (Public Relations of Public Welfare Science and Technology, 2018GSF118012); Shandong Medical and Health Science and Technology Development Plan Project (2016WS0268); China Postdoctoral Science Foundation (20110491558); Shandong Natural Science Foundation (ZR2016HB66).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Li, S., Zhang, X., Li, Z. et al. Desloratadine Ameliorates Olfactory Disorder and Suppresses AMPA Receptor GluA1 Expression in Allergic Rhinitis Rat. Arch. Immunol. Ther. Exp. 68, 6 (2020). https://doi.org/10.1007/s00005-020-00569-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00005-020-00569-3