Abstract
Tissue Engineering (TE) applications are focused on the design and fabrication of computer-aided artificial bone scaffolds with developing Additive Manufacturing (AM) technologies. Three-dimensional (3D) bone scaffold is designed with Computer-Aided Design (CAD) software, it is controlled pore size, and porosity ratio and a systematic production process are followed. In this study, artificial bone scaffold design and manufacturing technologies developed with AM technology have been discussed. The first part of the study is the applications materialized through different design methods such as CAD-based design, image-based design, implicit surface design, Topology Optimization (TO), and space-filling curves, which are used in computer-aided artificial bone scaffold design. Secondly, working principles of various AM technologies such as material extrusion and vat photopolymerization, powder bed fusion, material jetting, and direct writing and advantages and limitations of implementing these technologies in TE are also evaluated. Finally, possible future areas of use of the AM technologies in TE are discussed.
Graphic abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the fabrication of porous artificial bone scaffolds, which plays a critical role in the healing process of damaged tissues, it is necessary to use bioactive and biocompatible materials with controllable degradation and resorption rate. An ideally structured scaffold design should provide the necessary support in the regeneration of tissue with appropriate physical and mechanical properties. However, the complex structure of natural tissue complicates the process of artificial bone scaffolding [1].
Cell attachment is affected by the shape and structure of 3D bone scaffolds, porosity rate, pore size, mechanical stiffness, and biodegradation. The latest studies have determined that must be used scaled structures rather than a homogeneous structure in complex natural textures. While small-porous structures allow the ingrowth of non-mineralized osteoid tissue, large-porous structures play a role in bone growth [2]. The ideal pore size has been accepted to be between 100 and 500 µm in studies conducted in the last 10 years. Recent studies have shown the beneficial effects of pore sizes between 0.7 and 1.2 mm [3, 4].
Important factors required to create high-quality scaffolds suitable for the natural structure are arranged as porosity, bioactivity, biocompatibility, biodegradability, mechanical strength of the scaffold, design of the scaffold, surface area and the fabrication technology used [5].
Scaffolds must first be biocompatible for cells to adhere, function normally, pass through the scaffold, and begin to proliferate before placing a new matrix. Porous structures play an active role in the formation of interconnections and high porosity. High porosity is of great significance at the sake of supporting cell proliferation and differentiation and having osteoblasts or osteoprogenitor cells and improving bone tissues [6]. Interconnected porosity is important for the provision of adequate diffusion to the cells and Extracellular Matrix (ECM) in the structure [7]. Pore sizes should be taken into account for cell migration and nutrient delivery. The level of mechanical strength must be adequate for the formed structure to be supported by the body and be resistant to surgical operations [8]. There should be a large surface area to facilitate the distribution of nutrients and metabolic waste. In the scaffolds' fabrication phase, a scaled-up process should be provided in accordance with mass fabrication in the laboratory environment [9].
Different technologies are used to manufacture 3D porous bone scaffolds according to the desired properties as part of the tissue regeneration studies. As an alternative to traditionally used processes such as gas foaming, solvent casting, particle filtration, and phase separation, studies on new fabrication technologies with different advantages such as controlled porosity, reproducibility, personalized design, and systematicity are on the increase. AM technologies make it possible to design and manufacture scaffolds with the porosity of the desired size and feature, as they can be used integrated with CAD software and minimize the need for manual intervention. Scaffolding designs can be constructed in layers by means of dissimilar AM methods depending on the material and fabrication techniques used.
This study is a comprehensive review that evaluates studies focusing on bone scaffold design and fabrication with AM for TE. In this context, different AM technologies used in bone scaffold fabrication, advantages, and disadvantages of the materials and methods used were evaluated. CAD-based design, image-based design, implicit surface design, TO and space-filling curves methods that are used in the artificial bone scaffold design methods through AM were investigated. According to the results, the limitations, advantages, and new research topics of AM use in TE applications were discussed.
The remainder of this article is organized as follows. In the second section, conventional and novel scaffold fabrication techniques are discussed. In the thirds section, scaffold architecture design methods are examined. AM technologies are presented in the fourth section, and studies carried out in this area are evaluated. Last section includes future trends and challenges about artificial bone scaffolds in TE.
Scaffold fabrication methods
With the developing technologies, research and studies carried out on TE focus on the bone's synthesis and regeneration rather than the healing of the defective bone. In this process, cell tissues and growth factors as well as the ECM properties should be examined thoroughly. The properties of ECM through biochemical and mechanical interactions can be mimicked [10]. Mechanical support, cellular activity, and protein production can be given as examples of these properties.
The bone scaffold ensures the maintenance of cell functions and the formation of contact points necessary for cells' growth. In cases where the bone cannot heal itself, bone graft or the method of moving the bone to another location in the body is widely used [8]. With these treatment methods, it is possible to overcome the problems of immune rejection, difficulty in finding donors, and pathogen transfer [8].
Different methods are used in bone regeneration studies and 3D artificial bone scaffold fabrication. We can gather these methods under two main headings as conventional and AM techniques. Conventional fabrication methods can be specified as solvent casting, particle/salt leaching, freeze-drying, phase separation, fiber bonding, foam gel, molding and gas foaming (Fig. 1) [11].
AM has created an alternative to conventional processes as a fabrication method that can be integrated into the computer to follow a systematic method and obtain reproducible structures in TE applications. 3D bone scaffolds are designed to have a controllable pore size and number in CAD systems and are produced with a non-random pore formation at parameters determined by AM technologies. The fact that micron-sized structures can be produced under intense supervision has caused TE studies to focus on this area [12]. AM technologies generally used in TE are material extrusion, vat photopolymerization, powder bed fusion, material jetting and direct writing systems. The conventional fabrication and AM technologies used as part of TE applications are shown in Fig. 1.
Conventional fabrication methods
Conventional fabrication methods are used within the scope of TE studies are known as gas foaming, freeze-drying, particle/salt filtration, solvent casting, sol–gel, phase separation, fibre bonding, molding and electrospinning [11].
The encounter of problems such as immune rejection, pain, and infection after implanting the artificial bone scaffold through these techniques has shown that conventional processes are not sufficient in mechanical strength and vascularization [13]. After the implantation, relaxation may occur due to incompatible mechanical properties between the host bone tissue and the artificial bone tissue [14]. It is also quite cumbersome to control the pore geometry, size, and interdependence, and distribution of these pores through conventional fabrication techniques. This leads to the formation of inconsistent and less connected scaffolds. For instance, in the solvent casting technique, depending on the salt particles' contact state, it may be possible that the pores do not bind together. It has been determined that 10–30% of the pores are interconnected in the gas foaming technique. In the fibre bonding technique, the fiber mesh braids' mechanical strength is weak [15].
Another disadvantage of these techniques is that they are not systematic and reproducible. It is quite difficult to attain homogeneous structures. Precise control of the pore shape and size and the interconnectedness of the pores is not possible. These conventional techniques, which are not practical enough for the fabrication of 3D scaffolds with desired properties, have the following disadvantages [16]:
-
Manual intervention,
-
Systematic/non-reproducible handling procedures,
-
Use of toxic organic solvents,
-
Use of pyrogens,
-
Shape limitations,
-
Limited cell growth.
Novel fabrication techniques
Scaffolds can be designed in desired pore size and ratio and produced in a single process step with CAD software. This method makes it possible to produce bone scaffolds with controlled porosity and various hardness levels [14]. Another advantage of this process is that scaffolds' mechanical strength can be calculated through Computer-Aided Engineering (CAE) software. With simulation algorithms, load-bearing properties can be evaluated in the pre-fabrication process following different material properties [12].
By virtue of the AM technologies, the interior and exterior architecture of scaffolding structures is divided into slices with appropriate software and built layer by layer, with high precision and control. The data required for models to be created in CAD systems are attained by medical imaging techniques such as Computer Tomography (CT) and Magnetic Resonance Imaging (MRI) [17].
In the AM, it is possible to achieve 3D bone scaffolds by using various biomaterials with desired cell properties. The scaffolds produced affect cell growth, proliferation, adhesion, and regulation through their micro properties [18]. AM includes a computer-controlled fabrication process. Models created through a CAD model with medical imaging techniques can be produced with minimum labour. The 3D scaffolds obtained are produced with high quality and accuracy, with interconnected porosity [19]. This technique is based on the principle of producing solid, liquid, and powder materials layer by layer via CAD and Computer-Aided Manufacturing (CAM) tools. In addition to the fabrication of high porous scaffolds, AM also provides precise control of reproducible, specialized architectures [20].
Scaffold architecture design
Scaffold performance is affected by the pore volume, pore size, and mechanical strength. Interconnected porosity is an important factor for the continued growth of bone tissue. Interconnected pores allow for removal of the waste material, vessel formation (vascularization), cell growth and transmission of nutrients to the scaffold's interior. High porosity is important to increase the surface area per unit volume [21]. In addition, an adequate pore size should be provided for cell migration and infiltration.
Other important factors required to create the scaffold structure and provide growth, other than porosity are biocompatibility, biodegradability, mechanical properties, scaffolding design, and fabrication technology. The scaffold structure's design affects the mechanical properties and cell behaviour of the bone [22]. In order to generate the random shaped complex structure of bone scaffold in a simplified manner on CAD software, different methods such as CAD-based design, image-based design, implicit surface design, TO and space-filling curves are utilized [20]. In these methods, artificial scaffold architectures of different sizes and numbers can be obtained by imitating the porous bone scaffold structure on a digital platform.
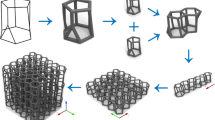
CAD based design
CAD-based design is the most widely used method for scaffolding design. Standard solid models such as a cube, cylinder, prism, etc. are repeated regularly to attain porous scaffold models [23]. With the micro-structured cellular units, which can be increased periodically in the X, Y and Z axis directions, the porous scaffolds' macro properties are described. In the Computer-Aided System for Tissue Scaffolds (CASTS) developed, the library of Platonic and Archimedes polyhedrons is used. In these scaffold libraries, polyhedrons are used as the cellular units and automate the scaffold design [24]. The cellular units thus designed are added to the library and stored in the database for later use. For the artificial bone scaffold to be designed in accordance with the physical and mechanical properties of natural bone, heterogeneous scaffolds can be formed by combining cellular units of different geometries and/or sizes (Fig. 2) [12].
Heterogeneous scaffold structures with polyhedrons obtained from CASTS library [25].
Image based biomimetic design
In order to create an image-based CAD model in the regeneration of a damaged bone, it is necessary to obtain anatomical data through medical imaging methods such as CT and MRI. In this method, it is necessary to achieve an analytical image of the damaged area to produce computational tissue models, distinguish heterogeneous tissue types, and show vascular structure [26]. The image of the damaged area obtained through CT and MRI data is then combined with the inner pore architecture created on a CAD platform by means of the Boolean operations and the scaffold image is created (Fig. 3) [27].
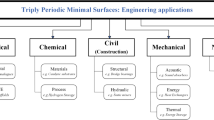
Implicit surface design
An implicit surface design method is used in TE applications to create bone scaffolds from complex models. Scaffold architectures are attained from surfaces that may be seen in biological tissues such as insect shells, butterfly wings, and shelled skeletons, increasing periodically [29]. Triply Periodic Minimal Surfaces (TPMS) is a type of implicit surface design method often found in natural structures. Scaffolding structures attained by this method can easily be produced by AM techniques.
Surface modeling methods used in traditional CAD applications are insufficient to create nanoscale designs. One of the methods used to obtain 3D models of complex and nano-sized designs is hyperbolic surfaces [30]. Hyperbolic surfaces, mostly seen in natural structures, are infinite and periodic in three independent directions.
Space-filling curves
In this method, layers in different sequences are created by changing the fabrication process's accumulation angle through AM technologies. By repeating these layers regularly, scaffolds with complex structure, high porosity and suitable mechanical properties are created. Deposition angle affects the number of contacts of struts forming the pores. Thus, pore control can be achieved by changing the deposition pattern [31]. The curves obtained with different alignment shapes are shown in Fig. 5.
Topology optimization (TO)
With TO, it is aimed to create scaffold structures with optimal pore number, size, and interconnections. The most suitable method for the fabrication of complex scaffolds obtained with TO is AM [32]. With this method, studies have focused on adapting the bone's elastic properties to the restrictions on porosity. Topological structures in different architectures obtained by this method are given in Fig. 4.
Architecture topologies [33].
Hollister et al. developed an image-based method for designing and manufacturing customized craniofacial biomaterial scaffolds [34]. It was stated that with this method, which utilized direct CT or MRI data, voxel density distribution was used to define scaffold topology and scaffold designs could be completed in less time. In the scaffold designs’ layout using TO, scaffold architectures are placed using the map of the density distribution in the scaffold obtained by the image-based design method [34].
In the CASTS system used in bone scaffold design, scaffold architects closest to natural bone structure can be obtained directly by using biomimetic based cellular units. Creating a rich library of cellular units by adding new geometric forms that were not used in scaffold design in previous studies to the CASTS system library will be a reference to other research and applications in the field of TE. Rather than having a homogeneous arrangement of cellular unit designs, it is possible to obtain heterogeneous functionally graded scaffold architectures at different scales. In addition to the use of a single type of cellular unit in scaffolding design, different sizes and shapes of pores can be obtained by using different geometries together. In the imaged-based design method, the damaged bone area can be imitated biomimetically to repair the scaffold whose damaged appearance is detected. Using CT data of directly damaged tissue makes it more likely to be successful in the implantation process. With the hyperbolic surfaces used in the implicit surface design method, it is easier to obtain amorphous structures used to imitate natural structures. In the TO method, it is advantageous in terms of the mechanical strength of the scaffold due to the development of designs that can show structural strength against the real loads to which the natural bone will be exposed.
Additive manufacturing (AM)
AM technologies play an important role in carrying out research and applications for bone regeneration. Advantages such as the ability to produce individual, free-shaped scaffolds with full control of pore size, shape, and interdependencies without the need for any molds have brought forward the AM. [35]. AM is the layer-by-layer fabrication of complex scaffolds created in CAD software. Layers refer to the shape in that section of the scaffold. Before printing, essential parameters such as powder packing density, powder flowability, layer thickness, binder drop volume, binder saturation and powder wettability need to be optimized to improve the quality of the resultant part [36]. 3D printed scaffolds with different geometries can be produced repeatedly [17]. In the last decade, biopolymers, bioceramics, biocomposites, and biometallic materials have been used to create the artificial skeleton closest to the structure of natural bone [37]. According to the material used and fabrication method, different AM technologies such as material extrusion, vat photopolymerization, powder bed fusion, material jetting, binder jetting and direct writing are used in AM. The materials and advantages and disadvantages of these technologies used in the biomedical field are given in Table 1.
It is advantageous compared to other techniques due to the material extrusion system's easy use, cost-effective, and high-resolution combinations. In this system, it is possible to create bone scaffolds with strut diameters in the range of several hundred micrometers [60]. It is the most suitable method for the production of artificial bone scaffolds with polymer materials. Vat Photopolymerization is the most sensitive technique among AM technologies. However, due to the need for post-production curing, hardening and shrinking of the scaffolds are disadvantageous in terms of measurement accuracy. The most advantageous technique in mechanical strength of scaffolds produced among AM technologies is powder bed systems. With these systems, high strength scaffolds are obtained by using metals such as Aluminum (Al), Titanium (Ti) and Vanadium (V) [61]. The scaffold resolution produced with powder bed systems depends on the laser diameter used. In addition, powder bed systems are the most expensive production technique among AM technologies. It is difficult to supply the powdered material used in production. In Material Jetting technique, it is an advantage that the cost is suitable, the production is fast, but the separation of the support material used in the production process from the scaffold is a huge problem. Binder Jetting has significant advantages such as suitable for the manufacture of almost all types of materials, ability to 3D printing with both metal and ceramic biomaterials, and no second material contamination problem for the support structure. But it can be needed extensive optimization for fabrication before the scanning for suitable binders and quality parts [36].
Material extrusion
The extrusion-based AM system, developed by S. Scott Crump in 1988, was commercialized under the name Fused Deposition Modelling (FDM) by Stratasys, but it is also known as Fused Filament Fabrication (FFF) [62]. In this system, the filament material is extruded downwards by the liquefier head with heat and deposited layer by layer (Fig. 5) [63]. In the material extrusion, the printing sensitivity depends on the extrusion nozzle, and the bone scaffolds printed would have appropriate biochemical and mechanical properties [64].
Schematic representation of the extrusion-based 3D printing system [65].
Synthetic polymers, bioactive ceramics and composites are widely used in the fabrication of bone scaffolds by this technology [66]. Synthetic polymers are preferred in TE studies thanks to their controlled degradation rates. The synthetic polymers most commonly used in bone scaffolding studies can be specified as Polylactic Acid (PLA) [67,68,69], Acrylonitrile Butadiene Styrene (ABS) [70, 71], Polycaprolactone (PCL) [72, 73] and Polyglycolide (PGA). Thermoplastics such as Polylactic-co-Glycolic Acid (PLGA), which are obtained by combining PLA, PCL and biomaterials, are used in TE applications thanks to their low melting temperatures [64]. Composite bone scaffolds with enhanced bioactivity can be created by mixing Hydroxyapatite (HA) particles with PLA in different mass proportions [39]. The mechanical properties of these hybrid scaffolds indicate that there is a low interaction between PLA and HA. This weak interaction in the composite can create defects that act as a stress concentrator and reduce the mechanical strength of the frame [74]. Composite PCL/TCP scaffolds, which are obtained by means of incorporating Tricalcium Phosphate (TCP), a bio-ceramic material, into the PCL building scaffolds, is another hybrid structure used in material extrusion method [40]. PCL/TCP scaffolds have different mechanical properties compared to PCL building scaffolds and get more quickly degraded in vivo. Other properties, such as crystallinity, are only modified by various treatment processes that seriously affect the degradation tract [38]. It has also been observed that PCL and PCL–TCP composite scaffolds degrade very differently under standard and accelerated degradation conditions [75].
Different approaches are used in order to improve the mechanical and biological properties of polymer and polymer-based composite bioavailable materials, which are frequently used in the production of 3D bone scaffolds. One of these techniques is loading the Young's modulus to the polymer with organic and inorganic fillers, which are used to determine the solid material's hardness degree [76]. Using two different polymer materials together is another approach used for this purpose.
FDM is also for ceramic materials and this technique is known as Fused Deposition of Ceramics (FDC). However, due to the fragile nature of ceramic materials, it is not possible to make flexible filaments in strip form. Therefore, ceramic materials are used in FDM technique as composite filaments of different densities together with thermoplastic binders [77]. Kalita et al. [78] has produced porous scaffold structures using Polypropylene (PP)/TCP composite filaments with FDM and the method is one of the first examples in the literature. The problem of inability to produce filaments from ceramic materials has been tried to be solved with indirect FDM (or indirect 3D printing). The study by Bose et al. [35] is a pioneering work for the solution of this problem. They have used indirect 3D printing method of alumina ceramic scaffolds with different pore size, porosity ration and volume. Similarly, porous scaffolds produced by Bose et al. [41] using calcium alumina material (CaO–Al2O3) are among the early studies using indirect FDM method. In the production of ceramic scaffolds with the indirect FDM method, β-tri-calcium phosphate (β-TCP) structures are used in addition to alumina material. Using this method, Darsell et al. [79], which produced porous scaffolds with gradient structure, used alumina ceramic as scaffolding material. In the study, it has been determined that the mechanical properties of the scaffolds deteriorated as the porosity increased.
In more recent TE studies, scaffolds made of ceramic structures such as Calcium Phosphate (CaP) and Bioactive Glass (BG) with high biocompatibility are produced [80]. In addition, β-TCP ceramics are used to produce bone graft by forming composite filaments with PLA and Polyethylene Glycol (PEG) matrices.
Vat photopolymerization
The photopolymerization system (Fig. 6) is the first system invented in 3D printing technologies [81]. Most known photopolymerization systems are Stereolithography (SLA), Digital Micromirror Device (DMD), Solid Ground Curing (SGC), Two-Photon Polymerization (2PP), Continuous Liquid Interface Production (CLIP), and Digital Light Processing (DLP) [82].
Different fabrication method based on the position of the beam in the photopolymerization system: (a) bottom-up fabrication technique, and (b) top-down fabrication technique [83].
In the photopolymerization system, although mostly polymerized liquid molecules are used, monomers and oligomers can also be used depending on the desired properties of the part to be produced. Acrylate-based resins that enable rapid fabrication by exhibiting high reactivity are also used in this method [84]. It is also possible to use ceramic, composite and metallic materials as well as polymeric materials [84]. Photopolymerization is capable of printing at high resolution and even nano-sized complex structures can be produced with high measurement and model accuracy. The low biocompatibility and biodegradation rates of the materials used in this system is a disadvantage [85]. Furthermore, the limitation of biocompatible photopolymers is another important problem of photopolymerization. This problem is tried to be overcome by mixing biocompatible materials such as HA with photopolymers [86]. However, Scalera et al. [87] note that the higher the percentage of HA mixed with the photopolymer, the lower the rate of the photopolymerization reaction. The cellular behavior of the materials used in the photopolymerization method can be increased by Micro-Stereolithography (MSTL) and biomimetic apatite coating methods [42]. It is possible to produce scaffolds with regular porosity by means of coating Polypropylene Fumarate (PPF)/Diethyl Fumarate (DEF) scaffolds used in this method with HA [88]. Another reason for PPF choice is excellent cellular adhesion property [89]. In addition, it has been observed that the hardness increases by increasing the concentration of nanoparticles in Nano-HA composite resins used to produce porous scaffolds in this method [43]. In this method, it can be obtained highly interconnected porous with biodegradable PCL resin and it is quite suitable method for solvent-free fabrication. PCL composites that combined with BG provide improved mechanical properties in dry and wet operating conditions [44]. In another study on the use of BG ceramics in photopolymerization, a new type of BG ceramic (AP40mod) has been developed to repair critical bone defects in rabbit jaws [91]. Bone scaffold produced with AP40mod has showed suitable mechanical properties with 52.7 MPa bending strength and good biological activity. When PLA skeleton is used with HA and Trientilen Glikol Dimetakrilat (TEGMA), mechanical properties have been improved [92]. It is possible to produce more flexible scaffolds with Trimetilen Carbonat (TMC)/Trimetilol Propan (TMP) [93]. Poly (d, l-lactide) (PDLLA) is used in bone scaffold applications because it is a biodegradable polymer that exhibits mechanical properties close to bone [94]. The high printing sensitivity of PDDLA-based resins with photopolymerization allows the use of scaffold designs with complex structures in these studies. Studies on 3D printing of polymer-free HA/TCP scaffolds by photopolymerization method are seen in the literature [95]. The HA/TCP scaffold produced by Kim et al. [95] has sufficient bone formation capability and provided superior stability for the defect site.
Powder bed fusion
In the powder bed fusion system (Fig. 7), the powdered material particles are combined with a laser or electron beam to create a 3D model of the desired part [96]. Different printing techniques are used in the powder bed fusion system based on the energy source and material used. These techniques are Selective Laser Sintering (SLS), Selective Laser Melting (SLM), Direct Metal Laser Sintering (DMLS), Electron Beam Melting (EBM), and Multi Jet Fusion (MJF) [97].
Schematic representation of the powder bed fusion 3D printing system [98].
The materials used in this system are in a variety that includes metallic powders such as steel, aluminum, titanium, stainless steel [99]. Thermoplastic materials can be used in SLS and SLM thanks to their low melting temperature and thermal conductivity. It is also possible to use ceramic and composite materials in SLS and SLM techniques [81]. Although, SLS is a method mostly used in 3D printing of polymer scaffolds, there are few studies in the literature regarding the printing of metal scaffolds with SLS. Biocompatible alloys such as Ti/Silica (SiO2) composites [100] and Ti–6Al–4 V [101] were used as scaffolding materials in these studies.
The use of ceramic materials in these systems does not give promising results due to low mechanical strength and low density [102]. However, using widely used solvent evaporation, dissolution–precipitation, mechanical mixing approaches, and two powder sintering mechanisms for the SLS technique, high performance porous ceramic scaffolds are obtained [103].
It has been determined that the powder bed fusion system is efficient in TE applications, especially in cardiac and bone TE. The fact that this system's required material is expensive and difficult to access limits the studies in this field. In addition, the fact that biocompatible powder particles are required for printing is presented as another limiting feature [104]. Hybrid scaffolds are produced by SLS method using β-TCP and polymeric mixed biomaterials [105]. 3D bone scaffolds are created using Poly-l-Lactic Acid (PLLA) microspheres with appropriate particle sizes for SLS processing [47]. It is also possible that 3D nanocomposite scaffolds that contain CaP/Poly-3-Hydroxybutyrate-co-3-Hydroxyvalerat (PHBV) and Carbonated Hydroxyapatite (CHAP)/PLLA can be created through SLS [46]. Sintered scaffolds are seen to possess completely interconnected porous structures and high porosity values. It has been observed that nanocomposite building scaffolds have great potential for TE applications by providing the conditions suitable for osteoblastic cell growth and differentiation. Nano-HAP bone scaffolds, too, can be produced by the SLS method as part of the TE applications [45].
High power intensity laser beam is used to melt and combine metallic powders in SLM method. It is possible to process polymer, ceramic and metal materials with this method [106]. However, it is seen that metal alloys are generally used in bone scaffold applications. Scaffolds produced with SLM provides high mechanical properties. But in this method, bending possibility and inconsistent mechanical properties may occur due to inhomogeneous heat distribution [107]. Alloys such as Ti and Ti–6Al–4V have promising potential for bone repair. Therefore, production of bone scaffolds with SLM are widely used [48, 108]. It has been observed that an elastic modulus similar to trabecular bone can be obtained in Ti scaffolds produced with SLM [109]. Bone scaffolds produced with Ti–6Al–4V material used extensively in SLM applications have elastic modulus in the cortical bone elastic modulus range [110]. The mechanical properties of the bone can be imitated more strongly with functionally graded scaffolds. Ti–6Al–4V porous scaffolds produced with SLM method have been seen to have mechanical properties closer to natural bone tissue than uniform scaffolds [111]. It is possible to increase the strength of porous titanium scaffolds produced with SLM by coating them with PCL and Poly-3-Hydroxybutyrate (P3HB) [112]. In recent studies besides Ti and its alloys, different materials such as Iron-Manganese (Fe–35Mn) are also used in SLM applications [113]. Nickel (Ni)/Ti alloys (nitinol) are of interest in bone scaffold studies due to their shape memory effect, super flexibility, biocompatibility, and corrosion resistance properties [49, 114]. Although SLM is successful for the manufacture of NiTi structures, porosity leads to higher surface area, which leads to higher corrosion rate and Ni ion oscillation [115].
Material jetting
In the material jetting system (Fig. 8), photopolymer materials are jetted from the print heads and deposited on the moving fabrication platform and solidified by curing with the help of Ultraviolet (UV) rays. After curing, the support material is carried by a blade. This process is repeated for each layer and the fabrication process is completed.
Schematic representation of 3D printing system via material jetting [116].
The material jetting system is the system that generates the highest layer thickness (16 mm) in the Z direction among all 3D printing systems. The most common materials used in this system are PLA, ABS, polyamide, and their composites [117]. The greatest advantage of this method is that it allows the fabrication of parts with high measurement accuracy and surface quality. The part produced has homogeneous mechanical and thermal properties, but the part's mechanical strength may be low [118]. The material jetting system is similar to the SLA technology in the photopolymerization system, but it is more advantageous as it does not require additional post-fabrication curing [118].
Most of the TE applications performed by material jetting method have been produced with hydrogels using bioprinting technology that focuses on the interaction between cells [119,120,121]. The mechanical properties required to obtain the appropriate hydrogel structure by evaluating cell–material interaction, cell density and distribution are among the research topics addressed in the material jetting method [51]. Potential of inkjet method as a TE technique depends on several factors such as fluid criteria, biocompatibility, and gelation mechanisms. These factors should be evaluated for materials and applications that will provide greater control over cell viability. It has been suggested that tandem gelation, using both physical and chemical gelation, is a promising method to produce robust 3D scaffolds [108]. In this method, fabrication of scaffolds with different mechanical properties is achieved using bioprinting out of PEG hydrogel material and with mixture of PEG diacrylate and Gelatine Methacrylate (GelMA) [122]. PCL with high biocompatibility and long degradation properties is one of the most remarkable materials recently. PLGA scaffold produced with this system has good biocompatibility and is osteoconductive when implanted in a suitable location, but it may not be osteoinductive [52]. It may be needed modification to improve the osteogenic performance of the scaffold [123]. For this reason, macro porous Alpha-tricalcium Phosphate (α-TCP) scaffolds used for the treatment of facial bone disorders (including maxillofacial deformities) have yielded successful results in this method [124].
Binder jetting
In the binder jetting method, a binder is used to produce parts with lower temperatures. In this method, the binders are sprayed on the powder particles on the build platform in accordance with the CAD file of the model to be produced with the printer head. Powder particles are spread evenly on the binder material with a metal cylinder (Fig. 9). This process continues similarly until the model is formed [125]. Binder selection, application and strength are important issues that will affect particle size and shape printing quality and process [54]. Compared to other AM methods, it enables high resolution printing without the use of support material in the production of parts with complex geometry [126].
Schematic representation of 3D printing system via binder jetting [81].
Metal, sand, and ceramic materials in powder form are used as dry or wet in the binder jetting system. Used the powder size and shape are effective on print quality [127]. While dry powder binder jetting and large particles are preferred for low surface area and better fluidity, wet powder binder jetting is mostly preferred for fine particles. The large surface area of fine particles can absorb moisture [128]. Powder size affects the mechanical strength and surface roughness of the final part by affecting the powder flowability. With the use of small powder, part density can be improved, and better surface finishing can be observed after binding spraying and signaling [127]. Small and large powders also can be used together. In this way, the pores between the large powders can be filled with fine powders to increase the fluidity during binder spraying [125]. Another aspect that affects the quality of the parts produced by binder jetting is the shape of the particles used. Particle shapes affect friction and flowability. In literature, it has been reported that spherical powders show better flowability [129, 130].
Scaffold structures are obtained by using polymeric, ceramic, metallic and composite materials in the binder jetting method. CaP and BG are often preferred for bone graft applications due to its high biocompatibility and compositional properties with bone. TCP–BG based composite structured scaffolds are used to produce bone scaffolds with binder jetting system [131]. Scaffolds obtained by using the combination of Binder Jetting and TCP–BG have high mechanical strength and suitable dissolution properties. Balla et al. [132] have produced a composite scaffold structure using water-based adhesive by blending CaP powders with Calcium Sulphate (CaSO4). In this study, cube, cylinder and gear geometry has been produced with the binder jetting method in 10–25 mm cross section dimensions [132]. Similarly, CaSO4, based quick absorption powders and relatively slow HA powders have been using for the production of scaffold structures in binder jetting systems [133]. PCL infiltration is performed in order to fill the gap between particles and to increase the performance of scaffold structures in printed composite structured bioceramics scaffolds [53].
Another important factor affecting the performance of scaffold structures such as porosity is the surface geometry. In order to observe the effect of surface geometry on mechanical strength and in-vitro performance, complex topographic surfaces of cylindrical bone scaffolds have been produced with TCP powders. The results show that the change in surface topography does not affect the mechanical strength, but it has been found to be successful in increasing the surface area [134]. Ti bone scaffolds with pore sizes up to 800 μm have been produced with a binder jetting system [56]. It has been shown that porous Ti scaffolds have a good surface area for cell proliferation and provide strong local adhesion.
Although Tantalum (Ta) has biocompatibility that can show high in vitro and in vivo performance, its high production cost and not allowing the production of modular scaffolding have limited the studies in this field [57]. Ta scaffolds with varying porosity have been manufactured for the first-time using Laser Engineered Net Shaping (LENS™) [57]. Very good cellular growth, adhesion and differentiation has been observed in Ta scaffolds.
Direct writing
Direct 3D printing can be accomplished with the direct writing system without the need for any masking process. With this system, micro and nano-sized parts can be printed by applying the working principle of other 3D printer technologies such as material extrusion and material jetting in the printing process [81]. Among the methods applied in this system, there are methods such as direct ink writing, direct writing with laser transfer, direct writing with thermal jetting, direct writing with beam deposition, and direct writing in liquid phase [81]. Among these methods, the most commonly used are liquid jet-based (Fig. 10) and laser transfer printing.
Schematic representation of the liquid jet-based direct writing method [135].
With laser transfer, there is no contact between the print head and the lower table material in the direct writing system, and parts are produced by the method of precipitation of laser-induced materials. In this system, polymeric, ceramic, organic, sol–gel, metal, and semiconductor materials are used. In the direct writing system with laser transfer, it is possible to precisely control and manufacture complex parts that cannot be produced with other 3D printer technologies [136].
It is possible to produce HA scaffolds using dispense-plotting and negative mold techniques in the direct writing method. In the dispense-plotting scaffolds, while higher intracellular proliferation was determined, a higher differentiation of cells was detected in the scaffolds produced with negative molds [137]. Hybrid scaffolds based on PCL and starch mixtures were produced by direct writing method [138]. Hierarchical Mesoporous Bioactive Glass (MBG) scaffolds are manufactured using Polyvinyl Alcohol (PVA) binder [139]. This method provided a new opportunity to solve the problems encountered in inorganic scaffolding materials such as low strength and high brittleness. Seyednejad et al. created polymer-based 3D scaffolds (Polyhydroxymethylglycoside-co-Ε Caprolactone, PHMGCL) using the melt-plotting method [50]. Luo et al. in the study, porous scaffolds made of hollow alginate fibres were produced by the 3D Plotting method. Such materials increase the possibility of forming tissue structures that are biodegradable through a preformed vascular system [58]. In another study, PLA and a bioactive CaP glass were coupled and were used to produce biodegradable scaffolds in two different patterns [59]. While data of scanning electron microscopy and micro-CT show that 3D scaffolds have fully interconnected porosity, uniform distribution of glass particles, and a controlled and repetitive structure, glass particles increase the scaffolds roughness. Mechanical tests have shown that the compressive strength depends on the scaffold's geometry and the presence of the glass.
Summary and future trends
In this study, design and fabrication techniques used to overcome the problems encountered in the fabrication of artificial bone scaffolds in conventional processes for TE were examined. In the fabrication of bone scaffolds with AM technologies, using CAD-based design, image-based design, implicit surface design, TO and space-filling curves, scaffolds with appropriate mechanical properties and performance can be designed in desired pore sizes and ratios.
In recent years, besides the introduced design methods, biomimetic based geometries are used in bone scaffold design studies. The use of biomimetic approach in designing scaffolding architectures or in direct imitation of the damaged area has been stated in recent studies that provide the most appropriate scaffold design in terms of porosity and mechanical strength [140,141,142]. Research results show that porous structures enable the formation of interconnections and support cell proliferation. Therefore, it is important that porosity and pore size can be controlled. During the design process, the bone's actual pore size and porosity ratio where the scaffold will be implanted should be considered. For example, cancellous bone, the pore size is 500–1000 µm and porosity is 50–90%, for cortical bone the pore size is < 500 µm and porosity is 3–12% [143]. It is very difficult or even impossible to do this control with traditional methods. All studies show that this is possible with CAD systems. The ability to obtain bone scaffolds with high mechanical strength by using an optimization algorithm with TO, used in CAD-based bone scaffold design has led to the focus of recent studies on this area. An experimental process is followed in the parameters used in mathematical modelling methods. The selected strut diameter and the distance between the layers created affect the results obtained.
Scaffold geometries, whose design and analysis processes are completed with CAD and CAE systems, can be created by depositing solid, liquid and powder materials in a layer-by-layer. A striking point in studies on bone scaffolds' structural analysis with CAE software is the uniform application of uniaxial loads to the entire surface. However, the loads on natural bone are much more complex. Since it is not possible to simulate these loads directly in the computer environment, different results can be seen in the analysis results. In addition, performing CAE studies to determine the stresses on the bone before the design will cause the design to progress with real data.
The materials used in scaffolding production must be biocompatible that will not harm the human body and can be accepted by the host tissue. Materials that do not show extreme immunogenicity and induced inflammatory response against organs, tissues and cells should be selected [144]. The artificial bone scaffold, which is implanted after production, must be biodegradable to provide temporary support to the damaged bone area. The decomposition rate of the scaffold must be compatible with the tissue's degradation rate in the human body. Therefore, the chemical and mechanical properties of the biodegradable polymers to be selected are important. By using biodegradable polymers and their composites obtained with ceramics, high-strength bone scaffolds are obtained in accordance with the biological properties of natural bone. Metal-based 3D prints provide the advantages of reduced tool cost, versatile design and easy production of complex model, in addition to one-step part consolidation [115]. Metallic printing methods such as SLM and porous metallic scaffolds such as Ti and alloys such as nitinol are used as bone scaffold materials.
There is no doubt that the use of AM in bone scaffold applications has created important opportunities such as the design and production of complex model, and the integration of biocompatible materials into the scaffold fabrication process. However, this process still involves considerable difficulties. There is still a need for improvement in 3D printers to achieve important mechanical properties such as high strength and low modulus in bone scaffolds [107]. Problems in printing surface roughness, micro and nano-sized geometries (for strut and pores) are challenges that need to be solved in 3D printing of scaffolds. Biocompatibility and biomechanical strength are the main challenges encountered in polymeric scaffolds [145]. The dissolution difficulties of the support materials used in polymeric printing can also be added. The solubility of the support material affects the pore size and porosity ratio, which affects the mechanical and biological performance of the scaffold. Besides, the relationship between degradation rate and in vitro and in vivo tissue growth rate is important. If degradation and tissue growth rates are not equal, the structure cannot be preserved and cannot serve as a scaffold [107]. Inadequate vascularization is another challenge that we must tackle in polymeric scaffolding applications.
The main obstacle to the use of such scaffolds is that metallic implants are not degradable [146]. Another major challenge is corrosion in metallic scaffolds and its induced ion release. As a result, undesirable conditions such as inflammation in the scaffold may occur [54]. The high cost of metallic printing devices is another challenge in using these processes in scaffold fabrication processes. In addition, we can count the adjustment of printing parameters, material supply and long production times among the difficulties of metallic printing. Materials used in metallic printing exhibit high mechanical properties and satisfactory biocompatibility, but especially in SLM, there is a possibility of bending of the scaffold due to inhomogeneous heat distribution and inconsistent mechanical properties may occur [107]. In these cases, coating with biocompatible polymers such as PCL can improve the mechanical properties of metallic scaffolds [112].
The fragile nature of ceramic is one of the most important challenges in 3D printing of ceramic scaffolds. In addition, the high sintering temperature and the limitation of the printing methods that can be used are important difficulties. It is not possible to make flexible filaments with ceramic materials. This difficulty is tried to be overcome with polymer–ceramic composite filaments. However, in composite applications, the size of the ceramic particles in the matrix structure should be well adjusted. Because ceramic particles that are not well sized can clog 3D printer nozzles. The printing difficulties of ceramics in the FDM method have been tried to be overcome with the indirect FDM. Other difficulties with the AM process include the impact of operational variables such as surface quality, part size, product quality across production batches versus 3D printers, production speed and printing parameters on part quality [54]. The minimization of these effects goes through the optimization of design and printing processes such as part design, material selection and composition, printing method, selection of the right device.
Polymeric, metallic, ceramic, hybrid, composite and functionally graded materials are one of the focal points of TE studies for AM [54]. Long design times are required for the design of Functional Graded (FG) structures and mostly 3D printers do not meet the expectations in producing FG scaffolds at the desired strength and module [107]. A similar situation is valid for bioprinting. Printing functionally graded structures with bioprinting is very difficult. The inclusion of living cells in the 3D printing process is a factor that increases scaffold biocompatibility. However, this situation causes limitations such as material and processing parameters [147]. In addition, as the number of layers increases, the printing of biomaterials becomes more difficult. Therefore, layer thickness, scaffold dimensions and other printing parameters must be carefully determined.
New methods and ideas should be generated to develop the personal design concept that comes to the fore with AM technologies and complete the scanning methods used and subsequent processes in a shorter time. With AM, research can be carried out on applications that will speed up the process steps to switch to an industrial-sized fabrication system and personalized applications. The development of applications that will enable the transfer of CT and MRI scans to the CAD environment in a short time in order to develop and implantation specific scaffold structures specific to the damaged area in the bone should be the focus of future studies. Cellular unit libraries created in CAD software must contain architectures with variable geometry that can be applied to different bone regions. With the units obtained from this library, functionally graded scaffolds with heterogeneous sequence suitable for the natural structure of the damaged bone area are obtained. One of the popular study areas used to obtain different scaffold architectures in the design of cellular units is TO. Studies should be conducted on creating micro-structured scaffolds with optimum properties through TO. Augmentation production technology and optimization techniques that will ensure the correct transfer of the complex natural bone structure to the CAD environment are another trend study area [148].
TE applications with AM technologies are a field of study that requires the comprehensive coordination of different disciplines. With the cooperation of design engineering, metallurgy and materials engineering, manufacturing engineering, biomedical engineering, and medicine, it may be possible to design and manufacture scaffolds closest to the natural bone structure. The existence of a multidisciplinary study is inevitable to produce optimized bone scaffold structures with different biomaterials and production technologies [54]. It is not possible to imitate the compositional and mechanical properties of the complex structure of the human body with a single material. The requirements of each material preferred for different AM technologies used in TE studies are different. In order to create scaffolds suitable for the structure of natural bone, research can be carried out on the development of biocompatible materials and biomaterials with different mechanical and bionic properties. It can be studied to evaluate scaffolds' performance in hybrid structures obtained with different composite materials and living cells.
The features of the devices used in tissue scaffolding are limited to AM. The devices mostly allow the production of one type of material. Required mechanical and biological properties are unobtainable with a single material for multi-material structures using production technologies such as FDC and LENS by 3D printing. However, it can be achieved with appropriate combinations of different materials [149]. Multiple nozzle structures and scaffolding structures to be obtained using multiple materials will be one of the trend studies in this area [148].
The use of Volumetric Printing (VP), 4D Printing (4DP), and 5D Printing (5DP) technologies in TE applications will bring new perspectives to the fabrication and applications of scaffolding geometries. A light-sensitive liquid is solidified in a tank connected to a rotating platform using a Digital Light Processor (DLP) projector in VP technology. On the other hand, 4DP is inspired by botanic systems by adding a concept of time to AM technologies. Functional materials are used as raw materials in the production of scaffolding structure in this technology [150]. 5DP enables precise production of small elements in scaffolding structures on a mobile platform. As these technologies open new opportunities in the production of bone skeletons, they are becoming the new focus for TE applications.
References
J. Feng, J. Fu, C. Shang, Z. Lin, B. Li, Porous scaffold design by solid T-splines and triply periodic minimal surfaces. Comput. Methods Appl. Mech. Eng. 336, 333–352 (2018). https://doi.org/10.1016/j.cma.2018.03.007
N. Yang, Z. Quan, D. Zhang, Y. Tian, Multi-morphology transition hybridization CAD design of minimal surface porous structures for use in tissue engineering. Comput. Aided Des. 56, 11–21 (2014). https://doi.org/10.1016/j.cad.2014.06.006
C. Ghayor, F.E. Weber, Osteoconductive microarchitecture of bone substitutes for bone regeneration revisited. Front. Physiol. 9, 960 (2018). https://doi.org/10.3389/fphys.2018.00960
F.E. Weber, Reconsidering osteoconduction in the era of additive manufacturing. Tissue Eng. B 25, 375–386 (2019). https://doi.org/10.1089/ten.teb.2019.0047
Y. Guo, K. Liu, Z. Yu, Tetrahedron-based porous scaffold design for 3D printing. Designs 3, 1–17 (2019)
X. Liu, P.X. Ma, Polymeric scaffolds for bone tissue engineering. Ann. Biomed. Eng. 32, 477–486 (2004). https://doi.org/10.1023/B:ABME.0000017544.36001.8e
E.A. Phelps, A.J. Garcia, Update on therapeutic vascularization strategies. Regen. Med. 4, 65–80 (2009). https://doi.org/10.2217/17460751.4.1.65
D.W. Hutmacher, Scaffold in tissue engineering bone and cartilage. Biomaterials 21, 2529–2543 (2000). https://doi.org/10.1016/S0142-9612(00)00121-6
S. Partap, F. Lyons, F.J. O’Brien, Scaffolds and surfaces, in Basic Engineering for Medics and Biologists. An ESEM Primer on Engineering for Medicine. ed. by T.C. Lee, P. Niederer (IOS Press, Nieuwe Hemweg, 2010)
A.J. Salgado, O.P. Coutinho, R.L. Reis, Bone tissue engineering: state of the art and future trends. Macromol. Sci. 4, 743–765 (2004). https://doi.org/10.1002/mabi.200400026
E. Sachlos, J.T. Czernuszka, Making tissue engineering scaffolds work. Review: the application of solid freeform fabrication technology to the production of tissue engineering scaffolds. Eur. Cell. Mater. 5, 39–40. https://doi.org/10.22203/eCM.v005a03
B. Starly, Biomimetic design and fabrication of tissue engineered scaffolds using computer aided tissue engineering, Doctoral Thesis, Drexel University, USA, 2006
S. Gómez, M.D. Vlad, J. López, E. Fernández, Design and properties of 3D scaffolds for bone tissue engineering. Acta biomater. 42, 341–350 (2016). https://doi.org/10.1016/j.actbio.2016.06.032
L. Wang, J. Kang, C. Sun, D. Li, Y. Cao, Z. Jin, Mapping porous microstructures to yield desired mechanical properties for application in 3D printed bone scaffolds and orthopedic implants. Mater. Des. 133, 62–68 (2017). https://doi.org/10.1016/j.matdes.2017.07.021
H. Cao, N. Kuboyama, A biodegradable porous composite scaffold of PGA/β-TCP for bone tissue engineering. Bone 46, 386–395 (2010). https://doi.org/10.1016/j.bone.2009.09.031
M.E. Hoque, Y.L. Chuan, I. Pashby, Extrusion based rapid prototyping technique: an advanced platform for tissue engineering scaffold fabrication. Biopolymers 97, 83–93 (2012). https://doi.org/10.1002/bip.21701
A.R.C. Santos, H.A. Almeida, P.J. Bártolo, Additive manufacturing techniques for scaffold-based cartilage tissue engineering: a review on various additive manufacturing technologies in generating scaffolds for cartilage tissue engineering. Virtual Phys. Prototyp. 8, 175–186 (2013). https://doi.org/10.1080/17452759.2013.838825
C. Mota, D. Puppi, F. Chiellini, E. Chiellini, Additive manufacturing techniques for the production of tissue engineering constructs. J. Tissue Eng. Regen. Med. 9, 174–190 (2015). https://doi.org/10.1002/term.1635
B. Thavornyutikarn, N. Chantarapanich, K. Sitthiseripratip, G.A. Thouas, Q. Chen, Bone tissue engineering scaffolding: computer-aided scaffolding techniques. Prog. Biomater. 3, 61–102 (2014). https://doi.org/10.1007/s40204-014-0026-7
K. Pramanik, I.D. Behera, Computer aided design of scaffolds for tissue engineering applications. Int. J. Comput. Intell. Healthc. Inform. 4, 105–109 (2011)
P. Habibovic, U. Gbureck, C.J. Doillon, D.C. Bassett, C.A.V. Blitterswijk, J.E. Barralet, Osteoconduction and osteoinduction of low-temperature 3D printed bio ceramic implants. Biomaterials 29, 944–953 (2008). https://doi.org/10.1016/j.biomaterials.2007.10.023
S.J. Hollister, Porous scaffold design for tissue engineering. Nat. Mater. 4, 518–524 (2005). https://doi.org/10.1038/nmat1421
Y. Yang, G. Wang, H. Liang, C. Gao, S. Peng, L. Shen, C. Shuai, Additive manufacturing of bone scaffolds. Int. J. Bioprint. 5, 1–25 (2019)
X. Wang, S. Xu, S. Zhou, W. Xu, M. Leary, P. Choong, Y.M. Xie, Topological design and additive manufacturing of porous metals for bone scaffolds and orthopaedic implants: a review. Biomaterials 83, 127–141 (2016). https://doi.org/10.1016/j.biomaterials.2016.01.012
J. An, J.E.M. Teoh, R. Suntornnond, C.K. Chua, Design and 3D printing of scaffolds and tissues. Engineering 1, 261–268 (2015). https://doi.org/10.15302/J-ENG-2015061
W. Sun, B. Starly, J. Nam, A. Darling, Bio-CAD modelling and its applications in computer-aided tissue engineering. Comput. Aided Des. 37, 1097–1114 (2005). https://doi.org/10.1016/j.cad.2005.02.002
M.H. Smith, C.L. Flanagan, J.M. Kemppainen, J.A. Sack, H. Chung, S. Das, S.J. Hollister, S.E. Feinberg, Computed tomography-based tissue-engineered scaffolds in craniomaxillofacial surgery. Int. J. Med. Robot. Comput. Assist. Surg. 3, 207–216 (2007). https://doi.org/10.1002/rcs.143
R.D. Bowles, H.H. Gebhard, J.P. Dyke, D.J. Ballon, A. Tomasino, M.E. Cunningham, L.J. Bonassar, Image-based tissue engineering of a total intervertebral disc implant for restoration of function to the rat lumbar spine. NMR Biomed. 25, 443–451 (2012). https://doi.org/10.1002/nbm.1651
S.C. Kapfer, S.T. Hyde, K. Mecke, C.H. Arns, G.E. Schröder-Turk, Minimal surface scaffold designs for tissue engineering. Biomaterials 32, 6875–6882 (2011). https://doi.org/10.1016/j.biomaterials.2011.06.012
S.T. Hyde, C. Oguey, From 2D hyperbolic forests to 3D Euclidean entangled thickets. Eur. Phys. J. B 16, 613–630 (2000). https://doi.org/10.1007/PL00011063
T.B. Woodfield, L. Moroni, J. Malda, Combinatorial approaches to controlling cell behaviour and tissue formation in 3D via rapid-prototyping and smart scaffold design. Comb. Chem. High Throughput Screen. 12, 562–579 (2009). https://doi.org/10.2174/138620709788681899
V.J. Challis, A.P. Roberts, J.F. Grotowski, L.C. Zhang, T.B. Sercombe, Prototypes for bone implant scaffolds designed via topology optimization and manufactured by solid freeform fabrication. Adv. Eng. Mater. 12, 1106–1110 (2010). https://doi.org/10.1002/adem.201000154
S.J. Hollister, C.Y. Lin, Computational design of tissue engineering scaffold. Comput. Methods Appl. Mech. Eng. 196, 2991–2998 (2007). https://doi.org/10.1016/j.cma.2006.09.023
S.J. Hollister, Scaffold design and manufacturing: from concept to clinic. Adv. Mater. 21, 3330–3342 (2009). https://doi.org/10.1002/adma.200802977
S. Bose, S. Sugiura, A. Bandyopadhyay, Processing of controlled porosity ceramic structures via fused deposition process, Scr. Mater. 41, 1009–1014 (1999). http://pascal-francis.inist.fr/vibad/index.php?action=getRecordDetail&idt=1989762.
S. Bose, S. Vahabzadeh, A. Bandyopadhyay, Bone tissue engineering using 3D printing. Mater. Today 16, 496–504 (2013). https://doi.org/10.1016/j.mattod.2013.11.017
X. Du, S. Fu, Y. Zhu, 3D printing of ceramic-based scaffolds for bone tissue engineering: an overview. J. Mater. Chem. B 6, 4397–4412 (2018). https://doi.org/10.1039/C8TB00677F
C.X. Lam, D.W. Hutmacher, J.T. Schantz, M.A. Woodruff, S.H. Teoh, Evaluation of polycaprolactone scaffold degradation for 6 months in vitro and in vivo. Biomed. Mater. Res. 90A, 906–919 (2009). https://doi.org/10.1002/jbm.a.32052
L.R. Jaidev, K. Chatterjee, Surface functionalization of 3D printed polymer scaffolds to augment stem cell response. Mater. Des. 161, 44–54 (2019). https://doi.org/10.1016/j.matdes.2018.11.018
L. Yuan, S. Ding, C. Wen, Additive manufacturing technology for porous metal implant applications and triple minimal surface structures: a review. Bioact. Mater. 4, 56–70 (2019). https://doi.org/10.1016/j.bioactmat.2018.12.003
S. Bose, J. Darsell, M. Kintner, H. Hosick, A. Bandyopadhyay, Pore size and pore volume effects on alumina and TCP ceramic scaffolds. Mater. Sci. Eng. 23, 479–486 (2003). https://doi.org/10.1016/S0928-4931(02)00129-7
P.X. Lan, J.W. Lee, Y.L. Seol, D.W. Cho, Development of 3D PPF/DEF scaffolds using micro-stereolithography and surface modification. J. Mater. Sci. Mater. Med. 20, 271–279 (2009). https://doi.org/10.1007/s10856-008-3567-2
A. Ronca, L. Ambrosio, D.W. Grijpma, Preparation of designed poly(d, l-lactide)/nanosized hydroxyapatite composite structures by stereolithography. Acta Biomater. 9, 5989–5996 (2013). https://doi.org/10.1016/j.actbio.2012.12.004
L. Elomaa, A. Kokkari, T. Närhi, J.V. Seppälä, Porous 3D modeled scaffolds of bioactive glass and photocrosslinkable poly (ε-caprolactone) by stereolithography. Compos. Sci. Technol. 74, 99–106 (2013). https://doi.org/10.1016/j.compscitech.2012.10.014
C. Shuai, C. Gao, Y. Nie, H. Hu, Y. Zhou, S. Peng, Structure and properties of nano-hydroxyapatite scaffolds for bone tissue engineering with a selective laser sintering system. Nanotechnology 22, 285703 (2011). https://doi.org/10.1088/0957-4484/22/28/285703
B. Duan, M. Wang, W.Y. Zhou, W.L. Cheung, Z.Y. Li, W.W. Lu, Three-dimensional nanocomposite scaffolds fabricated via selective laser sintering for bone tissue engineering. Acta Biomater. 6, 4495–4505 (2010). https://doi.org/10.1016/j.actbio.2010.06.024
S.H. Lee, W.Y. Zhou, M. Wang, W.L. Cheung, W.Y. Ip, Selective laser sintering of poly(l-lactide) porous scaffolds for bone tissue engineering. J. Biomim. Biomater. Tissue Eng. 1, 81–89 (2008). https://doi.org/10.4028/www.scientific.net/JBBTE.1.81
X. Ye, S. Leeflang, C. Wu, J. Chang, J. Zhou, Z. Huan, Mesoporous bioactive glass functionalized 3D Ti–6Al–4V scaffolds with improved surface bioactivity. Materials 10, 1244 (2017). https://doi.org/10.3390/ma10111244
H. Ibrahim, A. Jahadakbar, A. Dehghan, N.S. Moghaddam, A. Amerinatanzi, M. Elahinia, In vitro corrosion assessment of additively manufactured porous NiTi structures for bone fixation applications. Metals 8, 164 (2018). https://doi.org/10.3390/met8030164
I.T. Ozbolat, Y. Yu, Bioprinting toward organ fabrication: challenges and future trends. IEEE Trans. Biomed. Eng. 60, 691–699 (2013). https://doi.org/10.1109/TBME.2013.2243912
K. Hölzl, S. Lin, L. Tytgat, S. Van Vlierberghe, L. Gu, A. Ovsianikov, Bioink properties before, during and after 3D bioprinting. Biofabrication 8, 032002 (2016). https://doi.org/10.1088/1758-5090/8/3/032002
Z. Ge, X. Tian, B.C. Heng, V. Fan, J.F. Yeo, T. Cao, Histological evaluation of osteogenesis of 3D-printed poly-lactic-co-glycolic acid (PLGA) scaffolds in a rabbit model. Biomed. Mater. 4, 021001 (2009). https://doi.org/10.1088/1748-6041/4/2/021001
Z. Zhou, E. Cunningham, A. Lennon, H.O. McCarthy, F. Buchanan, S.A. Clarke, N. Dunne, Effects of poly (ε-caprolactone) coating on the properties of three-dimensional printed porous structures. J. Mech. Behav. Biomed. Mater. 70, 68–83 (2017). https://doi.org/10.1016/j.jmbbm.2016.04.035
S.A. Tofail, E.P. Koumoulos, A. Bandyopadhyay, S. Bose, L. O’Donoghue, C. Charitidis, Additive manufacturing: scientific and technological challenges, market uptake and opportunities. Mater. Today 21, 22–37 (2018). https://doi.org/10.1016/j.mattod.2017.07.001
S. Bose, A. Bhattacharjee, D. Banerjee, A.R. Boccaccini, A. Bandyopadhyay, Influence of random and 3D printed designed porosities on mechanical and biological properties of tricalcium phosphate-bioactive glass scaffolds. Addit. Manuf. (2021). https://doi.org/10.1016/j.addma.2021.101895
W. Xue, B.V. Krishna, A. Bandyopadhyay, S. Bose, Processing and biocompatibility evaluation of laser processed porous titanium. Acta Biomater. 3, 1007–1018 (2007). https://doi.org/10.1016/j.actbio.2007.05.009
V.K. Balla, S. Bodhak, S. Bose, A. Bandyopadhyay, Porous tantalum structures for bone implants: fabrication, mechanical and in vitro biological properties. Acta biomater. 6, 3349–3359 (2010). https://doi.org/10.1016/j.actbio.2010.01.046
Y. Luo, A. Lode, M. Gelinsky, Direct plotting of three-dimensional hollow fiber scaffolds based on concentrated alginate pastes for tissue engineering. Adv. Healthc. Mater. 2, 777–783 (2013). https://doi.org/10.1002/adhm.201200303
T. Serra, J.A. Planell, M. Navarro, High-resolution PLA-based composite scaffolds via 3-D printing technology. Acta Biomater. 9, 5521–5530 (2013). https://doi.org/10.1016/j.actbio.2012.10.041
A. Houben, J. Van Hoorick, J. Van Erps, H. Thienpont, S. Van Vlierberghe, P. Dubruel, Indirect rapid prototyping: opening up unprecedented opportunities in scaffold design and applications. Ann. Biomed. Eng. 45, 58–83 (2017). https://doi.org/10.1007/s10439-016-1610-x
A. Cheng, Z. Schwartz, A. Kahn, X. Li, Z. Shao, M. Sun, Y. Ao, B.D. Doyan, H. Chen, Advances in porous scaffold design for bone and cartilage tissue engineering and regeneration. Tissue Eng. B 25, 14–29 (2019). https://doi.org/10.1089/ten.teb.2018.0119
D. Pranzo, P. Larizza, D. Filippini, G. Percoco, Extrusion-based 3D printing of microfluidic devices for chemical and biomedical applications: a topical review. Micromachines 9, 374 (2018). https://doi.org/10.3390/mi9080374
B.N. Turner, S.A. Gold, A review of melt extrusion additive manufacturing processes: II. Materials, dimensional accuracy, and surface roughness, Rapid Prototyp. J. 21, 250–261 (2015). https://doi.org/10.1108/RPJ-02-2013-0017
S. Naghieh, M.K. Ravari, M. Badrossamay, E. Foroozmehr, M. Kadkhodaei, Numerical investigation of the mechanical properties of the additive manufactured bone scaffolds fabricated by FDM: the effect of layer penetration and post-heating. J. Mech. Behav. Biomed. Mater. 59, 241–250 (2016). https://doi.org/10.1016/j.jmbbm.2016.01.031
F. Ning, W. Cong, J. Wei, S. Wang, M. Zhang, Additive manufacturing of CFRP composites using fused deposition modeling: effects of carbon fiber content and length. In ASME 2015 International Manufacturing Science and Engineering Conference, June 8–12, Charlotte, North Carolina, USA, 2015
L. Roseti, V. Parisi, M. Petretta, C. Cavallo, G. Desando, I. Bartolotti, B. Grigolo, Scaffolds for bone tissue engineering: state of the art and new perspectives. Mater. Sci. Eng. C 78, 1246–1262 (2017). https://doi.org/10.1016/j.msec.2017.05.017
A. Gregor, E. Filová, M. Novák, J. Kronek, H. Chlup, M. Buzgo, J. Hošek, Designing of PLA scaffolds for bone tissue replacement fabricated by ordinary commercial 3D printer. J. Biol. Eng. 11, 31 (2017). https://doi.org/10.1186/s13036-017-0074-3
J. Germain, C.A. Fuentes, A.W van Vuure, A. des Rieux, C. Dupont-Gillain, 3D-printed biodegradable gyroid scaffolds for tissue engineering applications. Mater. Des. 151, 113–122 (2018). https://doi.org/10.1016/j.matdes.2018.04.037
R. Fairag, D.H. Rosenzweig, J.L. Ramirez-Garcialuna, M.H. Weber, L. Haglund, Three-dimensional printed polylactic acid scaffolds promote bone-like matrix deposition in vitro. ACS Appl. Mater. Interfaces 11, 15306–15315 (2019). https://doi.org/10.1021/acsami.9b02502
D.H. Rosenzweig, E. Carelli, T. Steffen, P. Jarzem, L. Haglund, 3D-printed ABS and PLA scaffolds for cartilage and nucleus pulposus tissue regeneration. Int. J. Mol. Sci. 16, 15118–15135 (2015). https://doi.org/10.3390/ijms160715118
C.G. Helguero, J.L. Amaya, D.E. Komatsu, S. Pentyala, V. Mustahsan, E.A. Ramirez, I. Kao, Trabecular scaffolds’ mechanical properties of bone reconstruction using biomimetic implants. Procedia CIRP 65, 121–126 (2017). https://doi.org/10.1016/j.procir.2017.04.033
T. Patrício, M. Domingos, A. Gloria, P. Bártolo, Characterisation of PCL and PCL/PLA scaffolds for tissue engineering. Procedia CIRP 5, 110–114 (2013). https://doi.org/10.1016/j.procir.2013.01.022
S. Hassanajili, A. Karami-Pour, A. Oryan, T. Talaei-Khozani, Preparation and characterization of PLA/PCL/HA composite scaffolds using indirect 3D printing for bone tissue engineering. Mater. Sci. Eng. C 104, 109960 (2019). https://doi.org/10.1016/j.msec.2019.109960
I. Bankole, S. Oladapo, A.O.M. Adeoye, S.A. Zahedi, 3D printing of bone scaffolds with hybrid biomaterials. Composites B 158, 428–436 (2018). https://doi.org/10.1016/j.compositesb.2018.09.065
C.X. Lam, M.M. Savalani, S.H. Teoh, D.W. Hutmacher, Dynamics of in vitro polymer degradation of polycaprolactone-based scaffolds: accelerated versus simulated physiological conditions. Biomed. Mater. 3, 034108 (2008). https://doi.org/10.1021/acsami.9b0250210.1088/1748-6041/3/3/034108
S. Maietta, T. Russo, R. De Santis, D. Ronca, F. Riccardi, M. Catauro, M. Martorelli, A. Gloria, Further theoretical insight into the mechanical properties of polycaprolactone loaded with organic–inorganic hybrid fillers. Materials 11, 312 (2018). https://doi.org/10.3390/ma11020312
Z. Chen, Z. Li, J. Li, C. Liu, C. Lao, Y. Fu, C. Liu, Y. Li, P. Wang, Y. He, 3D printing of ceramics: a review. J. Eur. Ceram. Soc. 39, 661–687 (2019). https://doi.org/10.1016/j.jeurceramsoc.2018.11.013
S.J. Kalita, S. Bose, H.L. Hosick, A. Bandyopadhyay, Porous calcium aluminate ceramics for bone-graft applications. J. Mater. Res. 17, 3042–3049 (2002)
J. Darsell, S. Bose, H. Hosick, A. Bandyopadhyay, From CT scans to ceramic bone grafts. J. Am. Ceram. Soc. 86, 1076–1080 (2003). https://doi.org/10.1111/j.1151-2916.2003.tb03427.x
S. Esslinger, A. Grebhardt, J. Jaeger, F. Kern, A. Killinger, C. Bonten, R. Gadow, Additive manufacturing of β-tricalcium phosphate components via fused deposition of ceramics (FDC). Materials 14, 156 (2021). https://doi.org/10.3390/ma14010156
I. Gibson, D.W. Rosen, B. Stucker, Additive Manufacturing Technologies, vol. 17 (Springer, New York, 2014).
J.R. Tumbleston, D. Shirvanyants, N. Ermoshkin, R. Janusziewicz, A.R. Johnson, D. Kelly, K. Chen, R. Pinschmidt, J.P. Rolland, A. Ermoshkin, E.T. Samulski, J.M. DeSimone, Continuous liquid interface production of 3D objects. Science 347, 1349–1352 (2015). https://doi.org/10.1126/science.aaa2397
J.C. Wang, M. Ruilova, Y.H. Lin, The development of an active separation method for bottom-up stereolithography system. In IEEE/SICE International Symposium on System Integration (SII), Taipei, Taiwan, 2017, pp. 108–114
C. Schmidleithner, D.M. Kalaskar, Stereolithography. In 3D Printing, ed. by D. Cvetković (IntechOpen). https://www.intechopen.com/books/3d-printing. Accessed 15 July 2020
L. Zhang, G. Yang, B.N. Johnson, X. Jia, Three-dimensional (3D) printed scaffold and material selection for bone repair. Acta Biomater. 84, 16–33 (2018). https://doi.org/10.1016/j.actbio.2018.11.039
O. Guillaume, M.A. Geven, D.W. Grijpma, T.T. Tang, L. Qin, Y.X. Lai, R.G. Richards, D. Eglin, Poly (trimethylene carbonate) and nano-hydroxyapatite porous scaffolds manufactured by stereolithography. Polym. Adv. Technol. 28, 1219–1225 (2017). https://doi.org/10.1002/pat.3892
F. Scalera, C.E. Corcione, F. Montagna, A. Sannino, A. Maffezzoli, Development and characterization of UV curable epoxy/hydroxyapatite suspensions for stereolithography applied to bone tissue engineering. Ceram. Int. 40, 15455–15462 (2014). https://doi.org/10.1016/j.ceramint.2014.06.117
J.W. Lee, G.S. Ahn, D.S. Kim, D.W. Cho, Development of nano- and microscale composite 3D scaffolds using PPF/DEF-HA and micro-stereolithography. Microelectron. Eng. 89, 1465–1467 (2009). https://doi.org/10.1016/j.mee.2008.12.038
J.W. Lee, P.X. Lan, B. Kim, G. Lim, D.W. Cho, 3D scaffold fabrication with PPF/DEF using micro-stereolithography. Microelectron. Eng. 84, 1702–1705 (2007). https://doi.org/10.1016/j.mee.2007.01.267
L. Elomaa, S. Teixeira, R. Hakala, H. Korhonen, D.W. Grijpma, J.V. Seppälä, Preparation of poly (ε-caprolactone)-based tissue engineering scaffolds by stereolithography. Acta biomater. 7, 3850–3856 (2011). https://doi.org/10.1016/j.actbio.2011.06.039
F. Xu, H. Ren, M. Zheng, X. Shao, T. Dai, Y. Wu, L. Tian, Y. Liu, B. Liu, J. Gunster, Y. Liu, Y. Liu, Development of biodegradable bioactive glass ceramics by DLP printed containing EPCs/BMSCs for bone tissue engineering of rabbit mandible defects. J. Mech. Behav. Biomed. Mater. 103, 103532 (2020). https://doi.org/10.1016/j.jmbbm.2019.103532
S. Tanodekaew, S. Channasanon, P. Uppanan, Preparation and degradation study of photocurable oligolactide–HA composite: a potential resin for stereolithography application. J. Biomed. Mater. Res. B 102, 604–611 (2014). https://doi.org/10.1002/jbm.b.33040
S.J. Lee, H.W. Kang, J.K. Park, J.W. Rhie, S.K. Hahn, D.W. Cho, Application of microstereolithography in the development of three-dimensional cartilage regeneration scaffolds. Biomed. Microdevices 10, 233–241 (2008). https://doi.org/10.1007/s10544-007-9129-4
S.A. Skoog, P.L. Goering, R.J. Narayan, Stereolithography in tissue engineering. J. Mater. Sci. Mater. Med. 25, 845–856 (2014). https://doi.org/10.1007/s10856-013-5107-y
J.W. Kim, B.E. Yang, S.J. Hong, H.G. Choi, S.J. Byeon, H.K. Lim, S.M. Chung, J.H. Lee, S.H. Byun, Bone regeneration capability of 3D printed ceramic scaffolds. Int. J. Mol. Sci. 21, 4837 (2020). https://doi.org/10.3390/ijms21144837
V. Bhavar, P. Kattire, V. Patil, S. Khot, K. Gujar, R. Singh, A review on powder bed fusion technology of metal additive manufacturing. In Additive Manufacturing Handbook (CRC Press, Boca Raton, 2017), pp. 251–253
T. Duda, L.V. Raghavan, 3D metal printing technology. IFAC-PapersOnLine 49, 103–110 (2016). https://doi.org/10.1016/j.ifacol.2016.11.111
S. Moylan, E. Whitenton, B. Lane, J. Slotwinski, Infrared thermography for laser-based powder bed fusion additive manufacturing processes. AIP Conf. Proc. 1581(1), 1191–1196 (2014)
M. Ashraf, I. Gibson, M.G. Rashed, Challenges and prospects of 3D printing in structural engineering. In 13th International Conference on Steel, Space and Composite Structures, Perth, WA, 2018.
F.H. Liu, R.T. Lee, W.H. Lin, Y.S. Liao, Selective laser sintering of bio-metal scaffold. Procedia CIRP 5, 83–87 (2013). https://doi.org/10.1016/j.procir.2013.01.017
F. Mangano, M. Bazzoli, L. Tettamanti, D. Farronato, M. Maineri, A. Macchi, C. Mangano, Custom-made, selective laser sintering (SLS) blade implants as a non-conventional solution for the prosthetic rehabilitation of extremely atrophied posterior mandible. Lasers Med. Sci. 28, 1241–1247 (2013). https://doi.org/10.1007/s10103-012-1205-1
D. Hagen, D. Kovar, J.J. Beaman, Effects of electric field on selective laser sintering of yttria-stabilized zirconia ceramic powder. In SFF Symposium Proceedings, pp 909–913 (2018)
A.N. Chen, J.M. Wu, K. Liu, J.Y. Chen, H. Xiao, P. Chen, C.H. Li, Y.S. Shi, High-performance ceramic parts with complex shape prepared by selective laser sintering: a review. Adv. Appl. Ceram. 117, 100–117 (2018). https://doi.org/10.1080/17436753.2017.1379586
S. Sohrabi-Jahromi, B. Bakhshandeh, Application of selective laser sintering in fabricating tissue engineering scaffolds. In 1st National Congress on Application of Biomaterials in Regenerative Medicine, Tehran, Iran, 2013.
L. Liulan, H. Qingxi, H. Xianxu, X. Gaochun, Design and fabrication of bone tissue engineering scaffolds via rapid prototyping and CAD. J. Rare Earths 25, 379–383 (2006). https://doi.org/10.1016/S1002-0721(07)60510-9
A. Wubneh, E.K. Tsekoura, C. Ayranci, H. Uludağ, Current state of fabrication technologies and materials for bone tissue engineering. Acta Biomater. 80, 1–30 (2018). https://doi.org/10.1016/j.actbio.2018.09.031
M. Bahraminasab, Challenges on optimization of 3D-printed bone scaffolds. Biomed. Eng. Online 19, 1–33 (2020). https://doi.org/10.1186/s12938-020-00810-2
P.H. Warnke, T. Douglas, P. Wollny, E. Sherry, M. Steiner, S. Galonska, S.T. Becker, I.N. Springer, J. Wiltfang, S. Sivananthan, Rapid prototyping: porous titanium alloy scaffolds produced by selective laser melting for bone tissue engineering. Tissue Eng. C 15, 115–124 (2009). https://doi.org/10.1089/ten.tec.2008.0288
A. Ataee, Y. Li, M. Brandt, C. Wen, Ultrahigh-strength titanium gyroid scaffolds manufactured by selective laser melting (SLM) for bone implant applications. Acta Mater. 158, 354–368 (2018). https://doi.org/10.1016/j.actamat.2018.08.005
S. Dhiman, S.S. Sidhu, P.S. Bains, M. Bahraminasab, Mechanobiological assessment of Ti–6Al–4V fabricated via selective laser melting technique: a review. Rapid Prototyp. J. 25, 1266–1284 (2019). https://doi.org/10.1108/RPJ-03-2019-0057
X.Y. Zhang, X.C. Yan, G. Fang, M. Liu, Biomechanical influence of structural variation strategies on functionally graded scaffolds constructed with triply periodic minimal surface. Addit. Manuf. 32, 101015 (2020). https://doi.org/10.1016/j.addma.2019.101015
M. Grau, J. Matena, M. Teske, S. Petersen, P. Aliuos, L. Roland, N. Grabow, H.M. Escobar, N.C. Gellrich, H. Haferkamp, I. Nolte, In vitro evaluation of PCL and P (3HB) as coating materials for selective laser melted porous titanium implants. Materials 10, 1344 (2017). https://doi.org/10.3390/ma10121344
D. Carluccio, C. Xu, J. Venezuela, Y. Cao, D. Kent, M. Bermingham, A.G. Demir, B. Previtali, Q. Ye, M. Dargusch, Additively manufactured iron–manganese for biodegradable porous load-bearing bone scaffold applications. Acta biomater. 103, 346–360 (2020). https://doi.org/10.1016/j.actbio.2019.12.018
Z. Gorgin Karaji, M. Speirs, S. Dadbakhsh, J.P. Kruth, H.I.E.D. Weinans, A.A. Zadpoor, S.I.E.D. Amin Yavari, Additively manufactured and surface biofunctionalized porous nitinol. ACS Appl. Mater. Interfaces 9, 1293–1304 (2017). https://doi.org/10.1021/acsami.6b14026
A. Bandyopadhyay, I. Mitra, S. Bose, 3D printing for bone regeneration. Curr. Osteoporos. Rep. 18, 505–514 (2020). https://doi.org/10.1007/s11914-020-00606-2
M. Sireesha, J. Lee, A.S.K. Kiran, V.J. Babu, B.B. Kee, S. Ramakrishna, A review on additive manufacturing and its way into the oil and gas industry. RSC Adv. 8, 22460–22468 (2018). https://doi.org/10.1039/C8RA03194K
S. Meteyer, X. Xu, N. Perry, Y.F. Zhao, Energy and material flow analysis of binder-jetting additive manufacturing processes. Procedia CIRP 15, 19–25 (2014)
A. Bournias-Varotsis, X. Han, R.A. Harris, D.S. Engstrøm, Ultrasonic additive manufacturing using feedstock with build-in circuitry for 3D metal embedded electronics. Addit. Manuf. 29, 100799 (2019). https://doi.org/10.1016/j.addma.2019.100799
T. Xu, W. Zhao, J.M. Zhu, M.Z. Albanna, J.J. Yoo, A. Atala, Complex heterogeneous tissue constructs containing multiple cell types prepared by inkjet printing technology. Biomaterials 34, 130–139 (2013). https://doi.org/10.1016/j.biomaterials.2012.09.035
Y. He, F. Yang, H. Zhao, Q. Gao, B. Xia, J. Fu, Research on the printability of hydrogels in 3D bioprinting. Sci. Rep. 6, 29977 (2016)
P. Ramiah, L.C. du Toit, Y.E. Choonara, P.P.D. Kondiah, V. Pillay, Hydrogel-based bioinks for 3D bioprinting in tissue regeneration. Front. Mater. 7, 76 (2020). https://doi.org/10.3389/fmats.2020.00076
H. Kotturi, A. Abuabed, H. Zafar, E. Sawyer, B. Pallipparambil, H. Jamadagni, M. Khandaker, Evaluation of polyethylene glycol diacrylate–polycaprolactone scaffolds for tissue engineering applications. J. Funct. Biomater. 8, 39 (2017). https://doi.org/10.3390/jfb8030039
C. Garot, G. Bettega, C. Picart, Additive manufacturing of material scaffolds for bone regeneration: toward application in the clinics. Adv. Funct. Mater. (2021). https://doi.org/10.1002/adfm.202006967
Y. Kanno, T. Nakatsuka, H. Saijo, Y. Fujihara, H. Atsuhiko, U.I. Chung, K. Hoshi, Computed tomographic evaluation of novel custom-made artificial bones, “CT-bone”, applied for maxillofacial reconstruction. Regen. Ther. 5, 1–8 (2016). https://doi.org/10.1016/j.reth.2016.05.002
G.A. Fielding, A. Bandyopadhyay, S. Bose, Effects of silica and zinc oxide doping on mechanical and biological properties of 3D printed tricalcium phosphate tissue engineering scaffolds. Dent. Mater. 28, 113–122 (2012). https://doi.org/10.1016/j.dental.2011.09.010
D. Ke, S. Bose, Effects of pore distribution and chemistry on physical, mechanical, and biological properties of tricalcium phosphate scaffolds by binder-jet 3D printing. Addit. Manuf. 22, 111–117 (2018). https://doi.org/10.1016/j.addma.2018.04.020
S. Bose, D. Ke, H. Sahasrabudhe, A. Bandyopadhyay, Additive manufacturing of biomaterials. Prog. Mater. Sci. 93, 45–111 (2018). https://doi.org/10.1016/j.pmatsci.2017.08.003
Y. Xia, P. Zhou, X. Cheng, Y. Xie, C. Liang, C. Li, S. Xu, Selective laser sintering fabrication of nano-hydroxyapatite/poly-ε-caprolactone scaffolds for bone tissue engineering applications. Int. J. Nanomed. 8, 4197–4213 (2013). https://doi.org/10.2147/IJN.S50685
D. Ke, W. Dernell, A. Bandyopadhyay, S. Bose, Doped tricalcium phosphate scaffolds by thermal decomposition of naphthalene: mechanical properties and in vivo osteogenesis in a rabbit femur model. J. Biomed. Mater. Res. B 103, 1549–1559 (2015). https://doi.org/10.1002/jbm.b.33321
D. Ke, S. Bose, Doped tricalcium phosphate bone tissue engineering scaffolds using sucrose as template and microwave sintering: enhancement of mechanical and biological properties. Mater. Sci. Eng. C 78, 398–404 (2017). https://doi.org/10.1016/j.msec.2017.03.167.
S. Bose, A. Bhattacharjee, D. Banerjee, A.R. Boccaccini, A. Bandyopadhyay, Influence of random and 3D printed designed porosities on mechanical and biological properties of tricalcium phosphate-bioactive glass scaffolds. Addit. Manuf. (2020). https://doi.org/10.1016/j.addma.2021.101895
V.K. Balla, S. Bose, A. Bandyopadhyay, Processing of bulk alumina ceramics using laser engineered net shaping. Int. J. Appl. Ceram. Technol. 5, 234–242 (2008). https://doi.org/10.1111/j.1744-7402.2008.02202.x
Z. Zhou, E. Cunningham, A. Lennon, H.O. McCarthy, F. Buchanan, N. Dunne, Development of three-dimensional printing polymer-ceramic scaffolds with enhanced compressive properties and tuneable resorption. Mater. Sci. Eng. C 93, 975–986 (2018). https://doi.org/10.1016/j.msec.2018.08.048
A.A. Vu, D.A. Burke, A. Bandyopadhyay, S. Bose, Effects of surface area and topography on mechanical properties of 3D printed tricalcium phosphate scaffolds for osteoblast proliferation in bone grafting applications. Addit. Manuf. (2021). https://doi.org/10.1016/j.addma.2021.101870
J.R. Raney, J.A. Lewis, Printing mesoscale architectures. MRS Bull. 40, 943–950 (2015). https://doi.org/10.1557/mrs.2015.235
S.M.F. Cruz, L.A. Rocha, J.C. Viana, Printing technologies on flexible substrates for printed electronics. In Flexible Electronics (IntechOpen, London, 2018), pp. 47–70
R. Detsch, F. Uhl, U. Deisinger, G. Ziegler, 3D-cultivation of bone marrow stromal cells on hydroxyapatite scaffolds fabricated by dispense-plotting and negative mould technique. J. Mater. Sci. Mater. Med. 19, 1491–1496 (2008). https://doi.org/10.1007/s10856-007-3297-x
J.M. Sobral, S.G. Caridade, R.A. Sousa, J.F. Mano, R.L. Reis, Three-dimensional plotted scaffolds with controlled pore size gradients: effect of scaffold geometry on mechanical performance and cell seeding efficiency. Acta Biomater. 7, 1009–1018 (2011). https://doi.org/10.1016/j.actbio.2010.11.003
C. Wu, Y. Luo, G. Cuniberti, Y. Xiao, M. Gelinsky, Three-dimensional printing of hierarchical and tough mesoporous bioactive glass scaffolds with a controllable pore architecture, excellent mechanical strength, and mineralization ability. Acta Biomater. 7, 2644–2650 (2011). https://doi.org/10.1016/j.actbio.2011.03.009
P. Datta, V. Vyas, S. Dhara, A.R. Chowdhury, A. Barui, Anisotropy properties of tissues: a basis for fabrication of biomimetic anisotropic scaffolds for tissue engineering. J. Bionic Eng. 16, 842–868 (2019). https://doi.org/10.1007/s42235-019-0101-9
Y. Yang, X. Song, X. Li, Z. Chen, C. Zhou, Q. Zhou, Y. Chen, Recent progress in biomimetic additive manufacturing technology: from materials to functional structures. Adv. Mater. 30, 1706539 (2018). https://doi.org/10.1002/adma.201706539
S. Vijayavenkataraman, L. Zhang, S. Zhang, J.Y. His Fuh, W.F. Lu: Triply periodic minimal surfaces sheet scaffolds for tissue engineering applications: an optimization approach toward biomimetic scaffold design. ACS Appl. Biomater. 1, 259–269 (2018). https://doi.org/10.1021/acsabm.8b00052
S. Zhang, S. Vijayavenkataraman, W.F. Lu, J.Y. Fuh, A review on the use of computational methods to characterize, design, and optimize tissue engineering scaffolds, with a potential in 3D printing fabrication. J. Biomed. Mater. Res. B 107, 1329–1351 (2019). https://doi.org/10.1002/jbm.b.34226
T.M. Shick, A.Z. Abdul Kadir, N.H.A. Ngadiman, A. Ma’aram, A review of biomaterials scaffold fabrication in additive manufacturing for tissue engineering, J. Bioact. Compat. Polym. 34, 415–435 (2019). https://doi.org/10.1177/0883911519877426
S. Bose, M. Roy, A. Bandyopadhyay, Recent advances in bone tissue engineering scaffolds. Trends Biotechnol. 30, 546–554 (2012). https://doi.org/10.1016/j.tibtech.2012.07.005
S.F.S. Shirazi, S. Gharehkhani, M. Mehrali, H. Yarmand, H.S.C. Metselaar, N.A. Kadri, N.A.A. Osman, A review on powder-based additive manufacturing for tissue engineering: selective laser sintering and inkjet 3D printing. Sci. Technol. Adv. Mater. (2015). https://doi.org/10.1088/1468-6996/16/3/033502
D.P. Forrestal, T.J. Klein, M.A. Woodruff, Challenges in engineering large customized bone constructs. Biotechnol. Bioeng. 114, 1129–1139 (2017). https://doi.org/10.1002/bit.26222
X. Zhou, Y. Feng, J. Zhang, Y. Shi, L. Wang, Recent advances in additive manufacturing technology for bone tissue engineering scaffolds. Int. J. Adv. Manuf. Technol. (2020). https://doi.org/10.1007/s00170-020-05444-1
A. Bandyopadhyay, S. Bose, S. Das, 3D printing of biomaterials. MRS Bull. 40, 108–115 (2015). https://doi.org/10.1557/mrs.2015.3
H. Qu, Additive manufacturing for bone tissue engineering scaffolds. Mater. Today Commun. 24, 101024 (2020). https://doi.org/10.1016/j.mtcomm.2020.101024
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors reported no potential conflict of interest.
Rights and permissions
About this article
Cite this article
Top, N., Şahin, İ., Gökçe, H. et al. Computer-aided design and additive manufacturing of bone scaffolds for tissue engineering: state of the art. Journal of Materials Research 36, 3725–3745 (2021). https://doi.org/10.1557/s43578-021-00156-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1557/s43578-021-00156-y