Abstract
Background
Studies have shown intra-arterial therapies to be effective in controlling neuroendocrine liver metastases (NELMs), but the evidence supporting the selection of specific methods is limited. This meta-analysis is the first to compare survival outcomes between transarterial chemoembolization (TACE) and transarterial radioembolization (TARE) in the treatment of NELM.
Methods
A systematic search according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines in PubMed and Embase databases was conducted in February 2020 for published studies comparing survival outcomes between TACE and TARE in the treatment of NELM.
Results
Six eligible cohort studies with a total of 643 patients were identified. The TACE and TARE groups were similar in terms of age, sex, hepatic tumor burden, tumor grade, and Eastern Cooperative Oncology Group (ECOG) score. The patients treated with TACE had significantly better overall survival (odds ratio [OR], 1.92; 95% confidence interval [CI] 1.14–3.22, p = 0.014) than those treated with TARE. Overall survival ranged from 16.8 to 81.9 months with TACE and from 14.5 to 66.8 months with TARE. No significant differences in hepatic progression-free survival (OR, 1.01; 95% CI 0.75–1.35; p = 0.96) or tumor response were observed within the first 3 months (OR, 2.87; 95% CI 0.81–10.21; p = 0.10) or thereafter (OR, 0.98; 95% CI 0.12–7.86; p = 0.99). The complication rates were similar between the two groups, with 6.9% of the TACE patients versus 8.5% of TARE patients reporting major complications (OR, 1.16; 95% CI 0.54–2.48; p = 0.71) and respectively 44.6% and 58.8% of the TACE and TARE patients reporting minor adverse events (OR, 1.08; 95% CI 0.39–2.99; p = 0.88).
Conclusions
Despite similar tumor responses, an overall survival benefit was associated with TACE treatment of NELM compared with TARE treatment. Randomized controlled trials are warranted to confirm this finding and clarify whether certain subpopulations benefit from different transarterial methods.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Neuroendocrine tumors (NETs) comprise a group of neoplasms with a heterogeneous presentation and prognosis. Most of these tumors originate from the gasteroenteropancreatic tract.1,2 Frequently, NETs are asymptomatic until they metastasize to the liver, which is a predominant site of metastatic deposits in up to 50% of cases.3,4
Neuroendocrine liver metastases (NELM) can cause significant symptoms related to tumor bulk and hormonal activity. Their presence also is associated with reduced overall survival (OS).3,5 The 5-year survival rates range from 14 to 54% among those with distant metastases depending on the site of the primary tumor.3,5
Fortunately, a variety of treatment options for treating NELM are available. These treatments are primarily aimed at improving quality of life by reducing local tumor bulk and the associated symptoms. Although surgical resection is the preferred therapy because it provides a better long-term outcome and the chance for cure, only a small percentage of patients are eligible for this therapy.6,7
When surgery is not an option, intra-arterial liver-directed therapies can be used with great success. These therapies target the hypervascular nature of NELM. Specific methods include bland transarterial embolization (TAE), conventional transarterial chemoembolization (TACE), drug-eluting beads for transarterial chemoembolization (DEB-TACE), and transarterial radioembolization (TARE). The TAE approach relies purely on ischemia-induced cell damage to achieve tumor cell destruction, whereas the other approaches combine an initial dose of locally delivered chemotherapy or radiation and a following embolization.
Intra-arterial therapies have proven efficacy in controlling unresectable NELM.8 They also have a favorable safety profile, with the most common adverse effect being a post-embolization syndrome characterized by fever, abdominal pain, nausea, and vomiting.8 For these reasons, intra-arterial liver-directed therapies currently are broadly included in the treatment guidelines for neuroendocrine tumors with hepatic-predominant disease.9,10,11,12 However, evidence to guide the selection of a specific method is limited.
To date, only a few retrospective cohort studies have directly compared the clinical outcomes and survival rates of TACE and TARE, and these studies have yielded mixed results. Most of the studies found no significant difference in survival outcomes, whereas one of the larger studies found a survival benefit associated with TACE.13,14,15,16,17 Singla et al.18 found that survival outcomes could be maximized with either treatment depending on the Ki67 score.
This study aimed to compare the survival and clinical outcomes between TACE and TARE in the treatment of NELM. This is the first meta-analysis on this subject and represents the largest group of patients analyzed to date.
Methods
Study Selection
In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, a systematic search of the PubMed and Embase databases was conducted 15 February 2020 for published studies comparing the survival outcomes between TACE and TARE in the treatment of NELM. The keywords used in the search included chemoembolization, TACE AND radioembolization, TARE, SIRT, yttrium-90 AND neuroendocrine liver metastasis, and NELM.
The inclusion criteria specified primary research study, patients with a diagnosis of NELM, at least one distinct group of patients treated with TACE and one distinct group treated with TARE, and reported mean or median OS. There were no restrictions on the timeframe or language of publication. Studies that described treatment of primary hepatic malignancies or did not include both TACE and TARE were excluded. Systematic reviews, case reports, and abstracts also were excluded.
Data Extraction
Two independent reviewers (L.N., A.E.) extracted data into a preformed spreadsheet and resolved discrepancies by consensus. The primary outcomes of this study were median OS and hepatic progression-free survival (HPFS). The secondary outcomes were tumor response, symptom response, and major or minor adverse events. None of the studies included crossover patients but did include outcomes for patients undergoing repeat and adjunctive therapies during the follow-up period.
Quality Assessment
The Newcastle-Ottawa Scale was used to assess the quality of each included study. Each study was assigned a numeric score in eight domains designed to evaluate sample selection, comparability of cohorts, and outcomes. The scores for the included studies ranged from 5 to 9, with 9 as the maximum possible score. The most common reason for point deductions was lack of control for bias in the original analyses (n = 4). The risk of bias also was increased in some studies by omission of a clear description of the data source (n = 1) and inadequate description of a loss to follow-up evaluation (n = 2). The methodologic quality and risk of bias are outlined in Table 1.
Statistical Analysis
Statistical analyses were performed using Comprehensive Meta-Analysis (Biostat, Englewood, New Jersey), version 3.0, and RevMan (The Nordic Cochrane Center, Copenhagen, Denmark) version 5.3. Medians were converted to means, and interquartile ranges and confidence intervals (CIs) were converted to standard deviations where applicable. Pooled means and standard deviations were calculated according to the Cochrane Handbook for Systematic Reviews of Interventions. Heterogeneity of the effect sizes between studies was detected using Cochran’s Q test and quantified using Higgin’s I2 test. Heterogeneity was considered significant at p values lower than 0.1 and at an I2 higher than 50%. A fixed-effects model was used to calculate the pooled odds ratio (OR) or standardized mean difference (SMD) for categorical data and the 95% confidence interval (CI) for quantitative data. In case of heterogeneity, a random-effects model was used.
Results
Characteristics of Included Studies
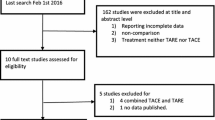
The study identified 344 published titles. After review of title, abstract, and full text where indicated, six retrospective cohort studies published between 2013 and 2020 were found to meet the inclusion criteria (Fig. 1). The meta-analysis included 643 patients with NELM. Of these 643 patients, 422 were treated with TACE and 221 were treated with TARE using yttrium-90 (Table 2). The patients in the TACE group were confirmed recipients of embolization to stasis in all but the smallest study (with 14 patients), in which the description was ambiguous.
Pooled Analysis for Clinical Characteristics of Patients
The clinical characteristics of the treatment groups are summarized in Fig. 2. The treatment groups did not differ significantly by age (SMD, –0.14; 95% CI –0.32 to 0.03; p = 0.11) or sex (female: OR, 0.99; 95% CI 0.69–1.42; p = 0.97). The primary tumor sites were similar between the groups including the pancreas (OR, 1.71; 95% CI 0.77–1.77; p = 0.32), the lung (OR, 0.76; 95% CI 0.53–1.1; p = 0.93), and gastrointestinal sites (OR, 1.27; 95% CI 0.46–3.94; p = 0.96).
The two groups did not differ significantly in terms of hepatic tumor burden (tumor burden >50%: OR, 1.71; 95% CI 0.96–3.04; p = 0.07) or tumor grade (G3: OR, 0.8; 95% CI 0.13–5.13; p = 0.82 vs G2: OR, 1.12; 95% CI 0.68–1.84; p = 0.66), although only three of the studies reported tumor grade and tumor burden. The Eastern Cooperative Oncology Group (ECOG) score, a standard measure of patient functional status and an important predictor of survival, also was similar between the treatment groups (ECOG ≥1: OR, 1.75; 95% CI 0.60–5.14; p = 0.31).
The two groups did not differ significantly regarding the presence of extrahepatic metastases (OR, 0.91; 95% CI 0.53–1.54; p = 0.72) or bilobular disease (OR, 0.82; 95% CI 0.48–1.41; p = 0.47). The history of resection or ablation of metastatic tumors was similar between the groups (OR, 1.20; 95% CI 0.71–2.02; p = 0.49). The TARE group was more likely to have received prior systemic chemotherapy (OR, 0.48; 95% CI 0.27–0.83; p = 0.009) and prior octreotide therapy (OR, 0.50; 95% CI 0.30–0.84; p = 0.009). The patients in the TACE group were significantly more likely to have undergone multiple chemoembolization treatment sessions, as is common (≥3 sessions: OR, 4.82; 95% CI 1.92–12.08; p < 0.001).
Pairwise Comparison of Survival
All six studies reported OS, and five studies reported hepatic progression-free survival. The median OS ranged from 16.8 to 81.9 months with TACE and from 14.5 to 66.8 months with TARE. The patients treated with TACE had significantly better OS (OR, 1.92; 95% CI 1.14–3.22; p = 0.014; Fig. 3). Surprisingly, there was no observable difference found in hepatic progression-free survival between the groups (OR, 1.01; 95% CI 0.75–1.35; p = 0.96; Fig. 3).
Pairwise Comparison of Treatment Response
Four studies reported radiographic tumor response, but only three of these studies used the standard Response Evaluation Criteria in Solid Tumours (RECIST) criteria. No significant difference between TACE and TARE in tumor response within the first 3 months was observed (OR, 2.87; 95% CI 0.81–10.2; p = 0.10) or thereafter (OR, 0.98; 95% CI 0.12–7.86; p = 0.99) (Fig. 4). Two studies reported symptom response. Among the patients who were symptomatic at presentation, 52.6% of those in the TACE group and 75% of those in the TARE group reported improvement in their symptoms. The groups demonstrated no significant difference in symptom response (OR, 0.30; 95% CI 0.06–1.45; p = 0.13).
Pairwise Comparison of Complications
The complication rates were similar between the treatment groups (Fig. 5), with 6.9% of the TACE-treated patients reporting major adverse events compared with 8.5% of the TARE-treated patients (OR, 1.16; 95% CI 0.54–2.48; p = 0.71). Similarly, 44.6% of the patients treated with TACE reported minor adverse events compared with 58.8% of the patients treated with TARE (OR, 1.08; 95% CI 0.39–2.99; p = 0.88). The common minor adverse events included abdominal pain, nausea, vomiting, anorexia, fatigue, fever, flushing, and elevations in aspartate aminotransferase (AST) or alanine aminotransferase (ALT).
Discussion
The number of NET patients is increasing, and these patients often present with NELM or eventually will experience NELM.14,18,19,20 Intra-arterial therapies have been proved effective in managing symptomatic and unresectable NELM, but to date, no high-quality evidence exists to support the use of a specific method.21,22,23 Although TARE is thought to have some advantages over TACE (e.g., ability to treat a complete liver lobe or miliary disease with less overall toxicity),14,24 the available literature comparing these treatments has yielded mixed results, leaving the choice of method largely up to institutional preference. This meta-analysis aimed to compare the effectiveness and survival outcomes between TACE and TARE in the management of NELM.
We found that TACE conferred a significantly longer OS than TARE. This finding is consistent with that of Minh et al.,13 who concluded from their propensity score analysis of 192 patients that conventional TACE was associated with a significantly better OS than TARE. Interestingly, the HPFS did not differ between the two groups.
We also found no significant difference in hepatic tumor response rates between TACE and TARE. This is consistent with previous studies reporting uniformly high tumor response rates in the form of regression or at least control of the disease in up to 95% of patients treated with TACE7,25,26 and up to 90% of patients treated with TARE.27,28,29
Prior studies have similarly demonstrated that the disease control does not necessarily correlate with the OS. In their systematic review, Jia and Wang et al.4 reported higher disease control rates and lower median survival rates with TARE than with TACE. However, in the absence of a difference in hepatic tumor response, the mechanism underlying the observed difference in OS remains unclear.
We recognize that the treatment groups have differences in baseline characteristics that might contribute to the OS difference, but we believe this is unlikely to be explained by these factors alone. Indeed, although the TACE group showed a slight but nonsignificant trend toward more extensive hepatic disease, they also tended to undergo more treatment sessions, as is consistent with this treatment method. Furthermore, Varker et al.30 previously demonstrated that repeat TACE does not significantly prolong OS or HPFS. The TARE patients were more likely to have undergone prior systemic chemotherapy, which might have been expected to confer improved survival outcomes but perhaps instead indicated that treatment-refractory disease had developed by the time they were considered for intra-arterial therapy. Despite these differences, the groups were found to be similar in terms of several important prognostic factors including ECOG score, tumor grade, and hepatic tumor burden.
We found no significant difference in symptom response between the two treatments. Both treatments offered symptom relief for at least half of the patients, confirming the value of the treatments in improving quality of life. Furthermore, the rates of major and minor complications did not differ significantly. Overall, the rate of major complications was low in both treatment groups, which is consistent with several previous studies demonstrating the safety of TACE and TARE for the treatment of NELM.13,14 Although laboratory markers of toxicity were not analyzed separately, we assumed that no clinically significant differences existed given the similarity of the groups in terms of adverse events.
These findings suggest that TACE may be superior to TARE in the treatment of unresectable NELM. Compared with TARE, TACE appears to offer improved OS duration, with comparable symptom response and side effects. Future prospective studies also should consider cost, number of treatments required, and quality of life.
This study had some limitations that should be acknowledged. The design of the retrospective studies that formed the basis of this meta-analysis has a relatively high level of inherent bias. We attempted to address this issue by describing how the composition of the treatment groups differed and by evaluating the degree of bias present using a standardized tool. Where possible, we attempted to focus our analyses on outcomes such as symptomatic and radiographic responses in the short period after the initial treatment. However, long-term outcomes such as survival would clearly have been affected by repeat or alternative treatments. Only one study17 differentiated the types of alternative treatments. The remaining studies included a general reference to octreotide therapy, with one study using it as an exclusion criterion. The specific type of octreotide therapy may affect OS. Evidence exists to show that peptide radionuclide therapy (PRRT) in advanced gastroenteropancreatic NET may offer a prolonged OS using 90-YDOTAo,Tyr3 compared with other radiolabeled somatostatin analogs.31 Furthermore, the NETTER-1 trial showed that 177Lu-Dototate PRRT had a significantly longer HPFS than octreotide long-acting repeatable therapy alone.32 Without this specific detail, it was difficult to assess and control for this source of bias. These limitations underscore the need for more highly controlled studies to compare intra-arterial therapies.
Conclusions
Despite similar hepatic tumor responses, our meta-analysis demonstrated an OS benefit associated with treating NELM with TACE instead of TARE. The TACE and TARE treatments offer comparable symptomatic relief with no significant differences in adverse effects. Randomized controlled trials are warranted to confirm these findings and clarify whether certain subpopulations might benefit from different intra-arterial methods.
References
Cives M, Strosberg JR. Gastroenteropancreatic neuroendocrine tumors. CA Cancer J Clin. 2018;68:471–87.
Dogeas E, Chong CCN, Weiss MJ, et al. Can echogenic appearance of neuroendocrine liver metastases on intraoperative ultrasonography predict tumor biology and prognosis? HPB Oxford. 2018;20:237–43.
Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26:3063–72.
Jia Z, Wang W. Yttrium-90 radioembolization for unresectable metastatic neuroendocrine liver tumor: a systematic review. Eur J Radiol. 2018;100:23–9.
Zeitels J, Naunheim K, Kaplan EL, Straus F. Carcinoid tumors: a 37-year experience. Arch Surg. 1982;117:732–7.
Bagante F, Spolverato G, Merath K, et al. Neuroendocrine liver metastasis: the chance to be cured after liver surgery. J Surg Oncol. 2017;115:687–95.https://doi.org/10.1002/jso.24563.
Bloomston M, Al-Saif O, Klemanski D, et al. Hepatic artery chemoembolization in 122 patients with metastatic carcinoid tumor: lessons learned. J Gastrointest Surg. 2007;11:264–71.
Dermine S, Palmieri L-J, Lavole J, et al. Nonpharmacological therapeutic options for liver metastases in advanced neuroendocrine tumors. J Clin Med. 2019;8:1907.
Pavel M, Costa F, Capdevila J, et al. ENETS consensus guidelines update for the management of distant metastatic disease of intestinal, pancreatic, bronchial neuroendocrine neoplasms (NEN) and NEN of unknown primary site. Neuroendocrinology. 2016;103:172–85.
Kulke MH, Anthony LB, Bushnell DL, et al. NANETS treatment guidelines: well-differentiated neuroendocrine tumors of the stomach and pancreas. Pancreas. 2010;39:735.
Boudreaux JP, Klimstra DS, Hassan MM, et al. The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: well-differentiated neuroendocrine tumors of the jejunum, ileum, appendix, and cecum. Pancreas. 2010;39:753–66.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: neuroendocrine and adrenal tumors. 2019.
Minh DD, Chapiro J, Gorodetski B, et al. Intra-arterial therapy of neuroendocrine tumour liver metastases: comparing conventional TACE, drug-eluting beads TACE and yttrium-90 radioembolisation as treatment options using a propensity score analysis model. Eur Radiol. 2017;27:4995–5005.
Egger ME, Armstrong E, Martin II RCG, et al. Transarterial chemoembolization vs radioembolization for neuroendocrine liver metastases: a multi-institutional analysis. J Am Coll Surg. 2020;230:363–70. https://doi.org/10.1016/j.jamcollsurg.2019.12.026.
Ozkan F, Peynircioglu B, Cil BE, et al. Transarterial chemo and radioembolization (yttrium90) of hepatic metastasis of neuroendocrine tumors: single-center experience. UHOD Uluslararasi Hematoloji-Onkoloji Dergisi. 2013;23:20–7.
Engelman ES, Leon-Ferre R, Naraev BG, et al. Comparison of transarterial liver-directed therapies for low-grade metastatic neuroendocrine tumors in a single institution. Pancreas. 2014;43:219–25. https://doi.org/10.1097/mpa.0000000000000030.
Chen JX, Rose S, White SB, et al. Embolotherapy for neuroendocrine tumor liver metastases: prognostic factors for hepatic progression-free survival and overall survival. Cardiovasc Intervent Radiol. 2017;40:69–80.
Singla S, LeVea CM, Pokuri VK, et al. Ki67 score as a potential predictor in the selection of liver-directed therapies for metastatic neuroendocrine tumors: a single institutional experience. J Gastrointest Oncol. 2016;7:441–8.
Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3:1335–42.
Nazario J, Gupta S. Transarterial liver-directed therapies of neuroendocrine hepatic metastases. Semin Oncol. 2010;37:118–26.
Peynircioǧlu B, Çil B, Bozkurt F, et al. Radioembolization for the treatment of unresectable liver cancer: initial experience at a single center. Diagnostic Interv Radiol. 2010;16:70–8. https://doi.org/10.4261/1305-3825.DIR.2693-09.1
Strosberg JR, Cheema A, Kvols LK. A review of systemic and liver-directed therapies for metastatic neuroendocrine tumors of the gastroenteropancreatic tract. Cancer Control. 2011;18:127–37.
Gaur SK, Friese JL, Sadow CA, et al. Hepatic arterial chemoembolization using drug-eluting beads in gastrointestinal neuroendocrine tumor metastatic to the liver. Cardiovasc Intervent Radiol. 2011;34:566–72.
Riaz A, Kulik LM, Mulcahy MF, et al. Yttrium-90 radioembolization in the management of liver malignancies. Semin Oncol. 2010;37:94–101.
Dhir M, Shrestha R, Steel JL, et al. Initial treatment of unresectable neuroendocrine tumor liver metastases with transarterial chemoembolization using streptozotocin: a 20-year experience. Ann Surg Oncol. 2017;24:450–9.
Dong XD, Carr BI. Hepatic artery chemoembolization for the treatment of liver metastases from neuroendocrine tumors: a long-term follow-up in 123 patients. Med Oncol. 2011;28:S286–90.
Kennedy AS, Dezarn WA, McNeillie P, et al. Radioembolization for unresectable neuroendocrine hepatic metastases using resin 90Y-microspheres: early results in 148 patients. Am J Clin Oncol Cancer Clin Trials. 2008;31:271–9.
Memon K, Lewandowski RJ, Mulcahy MF, et al. Radioembolization for neuroendocrine liver metastases: safety, imaging, and long-term outcomes. Int J Radiat Oncol Biol Phys. 2012;83:887–94.
Rhee TK, Lewandowski RJ, Liu DM, et al. 90Y radioembolization for metastatic neuroendocrine liver tumors: preliminary results from a multi-institutional experience. Ann Surg. 2008;247:1029–35.
Varker KA, Martin EW, Klemanski D, et al. Repeat transarterial chemoembolization (TACE) for progressive hepatic carcinoid metastases provides results similar to first TACE. J Gastrointest Surg. 2007;11:1680–5.
Valkema R, Pauwels S, Kvols LK, et al. Survival and response after peptide receptor radionuclide therapy with [90Y-DOTA0, Tyr3]octreotide in patients with advanced gastroenteropancreatic neuroendocrine tumors. Semin Nucl Med. 2006;36:147–56.
Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 trial of 177Lu-Dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376:125–35. https://doi.org/10.1056/NEJMoa1607427.
Disclosure
There are no conflicts of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ngo, L., Elnahla, A., Attia, A.S. et al. Chemoembolization Versus Radioembolization for Neuroendocrine Liver Metastases: A Meta-analysis Comparing Clinical Outcomes. Ann Surg Oncol 28, 1950–1958 (2021). https://doi.org/10.1245/s10434-020-09469-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09469-4