Abstract
Background
Transarterial chemoemobolization (TACE) is commonly used to treat metastatic carcinoid tumors; however, the management of progressive disease is less clear. We sought to determine if patients with disease progression after TACE would benefit from repeat TACE.
Methods
The records of 27 patients undergoing repeat TACE for radiologic or symptomatic progression after TACE for metastatic carcinoid were reviewed and compared to 122 undergoing first TACE. Overall and progression-free survivals were estimated by the Kaplan–Meier method.
Results
Mean disease-free interval after first TACE was 11.8 months. Radiologic response was observed in 61% compared to 82% after first TACE (p = 0.058); hormone response in 64% compared to 80% (p = 0.159); and symptomatic response in 77% compared to 92% (p = 0.053). The complication rate after repeat TACE was lower than after first TACE (p = 0.03). Median overall survival was similar after repeat (28.1 months) and first TACE (33.3 months) (p = 0.53). Progression-free survival was shorter after repeat TACE but not significantly so. No factor examined could predict survival after repeat TACE.
Conclusion
Repeat TACE for patients with hepatic carcinoid metastases failing first TACE or having evidence of disease progression is safe and offers a viable treatment option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carcinoid tumors are neuroendocrine malignancies characterized by an indolent growth pattern. The most frequent primary sites include the gastrointestinal tract, commonly ileum, and the bronchopulmonary system.1 The most frequent site of distant metastasis of carcinoid tumors is the liver, and the involvement is typically multicentric and diffuse.1 The presence of hepatic metastases is an important determinant of survival, with a 5-year survival of only 40% in patients having carcinoid liver metastases, compared to 100% in those without metastases.2 The optimal treatment for carcinoid hepatic metastases is complete resection, but at most 10% of patients have resectable disease.3 To realize benefit from cytoreduction, all of the primary tumor and at least 90% of the metastatic disease must be removed.3,4 Thus, although cytoreduction is recommended management, it is not achievable in the majority of patients. Systemic chemotherapy such as streptozotocin has provided disappointing results for the treatment of neuroendocrine tumors.5 Octreotide analogs are effective for management of symptoms related to the carcinoid syndrome by inhibition of polypeptide release, although their ability to inhibit tumor growth is mostly theoretical.6 However, over time the disease can become refractory to octreotide treatment.7
The use of hepatic artery embolization or chemoembolization (TACE) for neuroendocrine metastases has evolved over time. Hepatic metastases provide an ideal setting for regional therapies because tumors are preferentially supplied by branches of the hepatic artery; thus, selective devascularization can induce ischemia within the tumor while preserving normal parenchyma. This strategy is particularly useful for neuroendocrine tumors because they are highly vascular and thus particularly sensitive to ischemia.8,9 Thus, regional therapies such as TACE have been found to be efficacious in patients with symptoms refractory to octreotide and are the treatment of choice in patients whose disease is not amenable to resection.9–11
Although TACE has an established role in the treatment of hepatic neuroendocrine metastases, the management of patients who fail to respond to TACE or develop progressive disease after response to TACE remains a clinical challenge. Whereas most well-experienced centers advocate repeat TACE for progressive disease, the efficacy of such an approach has not been reported. We sought to determine if patients with disease progression after TACE could derive similar benefit from a second TACE procedure. The goal of this study was to determine the rate of response and overall survival in patients undergoing repeat TACE for hepatic carcinoid metastases. Furthermore, we wished to determine whether any factors related to the tumor or to the response to the first TACE procedure could predict survival after repeat TACE.
Materials and Methods
Patients
From the group of patients undergoing TACE for inoperable hepatic carcinoid metastases at the Ohio State University Medical Center between 1992 and 2004 (n = 122), a subset of patients (n = 27) underwent a second TACE procedure between January 1997 and May 2006 for treatment of radiologic or symptomatic progression. Patients undergoing TACE as a planned staged second procedure were not included. Both computerized records and paper charts were examined. Results were compared to those for first TACE. Approval for this study was obtained from the Institutional Review Board of the Ohio State University.
Eligibility Criteria and Patient Follow-Up
The eligibility criteria for initial TACE for metastatic carcinoid were detailed previously.12 Briefly, eligible patients were those with well- or moderately differentiated (atypical carcinoid) neuroendocrine carcinoma who had poorly controlled carcinoid-related symptoms on octreotide therapy, evidence of tumor progression in the liver, or significant tumor burden such that any progression could result in hepatic insufficiency rendering the patient ineligible for regional therapy. Patients with uncontrolled symptoms on octreotide therapy or asymptomatic patients with radiologic evidence of tumor progression in the previously treated region after first TACE were considered for repeat TACE. Patients undergoing planned stage TACE were not included in this study. Additional eligibility criteria included preserved hepatic and renal function (serum bilirubin <2 mg/dL and serum creatinine <2 mg/dL), normal coagulation profile, and adequate hematologic profile (leukocyte count >2,000/mL and platelet count >100,000/mL). Lobar portal vein occlusion was an absolute contraindication to TACE. All treatment decisions were made by a multidisciplinary team including the treating surgeon, medical oncologist, and interventional radiologist. After treatment, patients underwent clinical and radiologic evaluation at the discretion of the attending physician.
Embolization Procedure
Our approach to TACE has been described previously.12 Briefly, diagnostic angiography via the femoral approach at the time of TACE was first performed to review the hepatic arterial anatomy and confirm portal vein patency. A microcatheter was subsequently advanced through a 5-French sheath into the left or right hepatic artery. An emulsion of doxorubicin 30 mg, mitamycin 30 mg, cisplatin 50 mg, ioxaglate sodium, and ethiodized oil (37%) was injected. Additional embolic materials consisting of gelfoam, polyvinyl alcohol (PVA) particles, or Embospheres (Biosphere Medical, Inc., Rockland, MD) were then injected until flow in the hepatic artery ceased. Patients remained hospitalized as their clinical course dictated.
Assessment of Response
Radiologic response was assessed by computed tomography (CT), and was defined as any decrease in the size or number of hepatic lesions, or the development of significant calcifications within the lesions. Radiologic progression was defined as any increase in size or number of lesions at any time during follow-up. Symptomatic progression was defined as the worsening of symptoms or the requirement of increasing doses of octreotide to control symptoms. Finally, biochemical response to therapy was determined by assessment of serum pancreastatin levels.13
Statistical Analysis
Overall survival was determined from the time of repeat TACE until time of death from any cause as determined by hospital records or the Social Security Death Index (http://ssdi.rootsweb.com). Progression-free survival was calculated from the time of repeat TACE until radiologic, symptomatic, or serologic evidence of disease progression. Categorical data were compared using Fisher’s exact test and continuous data were compared using the Mann–Whitney U test. Overall survival and progression-free survival were estimated by the Kaplan–Meier method and curves were compared by log-rank analysis. The Cox proportional hazards model was used to determine prognostic variables. All analyses were completed using SPSS v.14 software (SPSS, Chicago, IL).
Results
Patients
The multidisciplinary team of the Neuroendocrine Tumor Program at The Ohio State Medical Center coordinates the treatment of patients undergoing TACE. We previously reported on 122 patients with inoperable hepatic carcinoid metastases who underwent TACE between January 1992 and December 2004.12 Of these 122 patients, a total of 27 (13 male, 14 female; median age 53) underwent a second TACE procedure for treatment of radiologic or symptomatic progression. This group of patients constituted the population for the present study. Patient characteristics are summarized in Table 1. The most common site of primary tumor was the small bowel, and half of these were in the ileum. The primary tumor had been resected in three-quarters of the patients. Before initial TACE, most patients were treated with somatostatin analogs. In the majority of patients (59%), the indication for repeat TACE was palliation of recurrent/progressive symptoms (Table 2).
Treatment Administered
Our traditional approach to TACE has been to treat all tumor-bearing portions of the liver in one sitting. Unilateral TACE was considered selectively in patients with particularly high tumor burden or those with poor underlying health. As such, two-thirds of the patients underwent whole liver TACE, and 26% underwent a unilateral (right or left) approach (Table 2).
Adverse Effects
As expected, all patients experienced transient (maximum duration 2–4 weeks) pain, fever, nausea, or fatigue after TACE (the so-called post-embolization syndrome). These were not considered complications. However, three patients (11%) developed complications, all of which resolved with medical management. One patient developed transient hyperbilirubinemia, one had hepatic encephalopathy, and one had supraventricular tachycardia. In contrast, among the original 122 patients undergoing the first TACE, complications occurred in 28 (23%). The difference in the rate of complications between first and repeat TACE was statistically significant (p = 0.03). Mortality of repeat TACE was nil, whereas mortality among the patients undergoing first TACE was 5% (6 patients) (p = NS).
Response to TACE
Radiologic response was observed in 61% (11 of 18) compared to 82% after first TACE (p = 0.058); hormone response was seen in 64% (14 of 22) compared to 80% after first TACE (p = 0.159); and symptomatic response was observed in 77% (17 of 22) compared to 92% after first TACE (p = 0.053).
Survival and Prognostic Factors
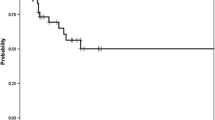
Overall median survival after repeat TACE (28.1 months) was similar to that after first TACE (33.3 months; p = 0.53, Fig. 1). Progression-free survival (median 5.0 months) was shorter after repeat TACE compared to initial TACE, but this difference was not statistically significant. No factor including age, comorbidity, site of primary tumor, resection of primary tumor, symptoms of carcinoid syndrome, or radiologic, hormone, or symptomatic response to the first TACE could predict survival after repeat TACE.
Discussion
Regional embolic therapy such as TACE is widely accepted for the management of hepatic metastases from carcinoid. In the era of novel regional therapies such as selective internal radiation therapy (SIRT), it remains to be seen whether repeat TACE or strategies such as SIRT should be considered in patients with disease progression after TACE. Whereas most well-experienced centers offer repeat TACE for patients failing initial TACE or having evidence of disease progression, the efficacy of repeat TACE relative to first-time treatment has not been described. Herein we report the results of 27 patients undergoing repeat TACE for radiologic or symptomatic progression. Repeat TACE was well tolerated, with only three patients (11%) experiencing complications. Survival was not different from first TACE.
Despite examination of several factors relating to the primary tumor and to response after initial TACE, we were unable to identify any factor predictive of survival. Nevertheless, long-term survival was possible in some patients. Factors examined as potential prognostic variables were age; presence of comorbidity; site of primary tumor; resection of primary tumor; symptoms of carcinoid syndrome; radiologic, hormone, or symptomatic response to the initial TACE; and radiologic, hormone, or symptomatic response to repeat TACE. In our previous report of patients undergoing initial TACE, pre-TACE levels of pancreastatin >5,000; the occurrence of complications; and lack of radiologic, symptomatic, or biochemical response to TACE were associated with decreased overall survival by univariate analysis.12 By multivariate analysis, only lack of symptomatic improvement after TACE was predictive of poor outcome.12 None of these factors was able to predict survival in the group of patients undergoing repeat TACE. Similarly, although others have suggested that carcinoid as compared to islet cell primary or resection of the primary before the need to address hepatic metastases were associated with survival advantage after liver-directed therapy, we have not found either of these to be prognostic in our experience.11,14
Serum level of pancreastatin, a split-product of chromogranin A, has proven utility as a sensitive marker for carcinoid tumors.15,16 Calhoun et al studied 31 patients with carcinoid tumors.17 Serum pancreastatin was elevated in 81% of patients, and was the only elevated peptide in 57%. Levels of multiple other peptides, including vasoactive intestinal peptide, pancreatic polypeptide, neurotensin, substance P, gastrin-releasing peptide, calcitonin, and gastrin were not consistently elevated.17 Similarly, we observed inconsistent elevation of tumor markers other than pancreastatin in a group of patients with metastatic neuroendocrine tumors treated on a Phase II trial of thalidomide.25 Our group previously found that decreased pancreastatin levels after TACE treatment may correlate with response to treatment, and proposed that an increase in pancreastatin level after a previous decrease may provide an indication for repeat TACE.13 Seventy-eight percent of patients treated with TACE experienced decreased or stable levels of pancreastatin after treatment; those whose pancreastatin levels did not decrease at least 20% after treatment all died within 8 months.13 The fact that pancreastatin response to TACE treatment was not able to predict survival in the present group of patients may be caused by the relatively small number of patients in this study.
The rates of radiologic, hormone (i.e., pancreastatin), and symptomatic response to TACE in this study were 61%, 64%, and 77%, respectively. Whereas these response rates were lower than after initial TACE, statistical significance was not reached. The rate of radiologic response, defined as any decrease in the size or number of hepatic lesions, was 61%. This compares favorably with results in the literature. There is inherent difficulty in objectively measuring radiographic response after regional therapy. Standardized criteria such as Response Evaluation Criteria in Solid Tumors (RECIST) assume equal distribution of drug to all areas of the tumor in a given organ and equate response to therapy with decrease in tumor size. Such assumptions do not hold true in regional therapy because drug distribution is less predictable and necrotic tumors often do not change (or may even increase in size) in response to therapy. Nevertheless, we currently track RECIST in our prospective database. In this study, we relied on the interpretation of the attending radiologist to determine response to therapy. Whereas this introduces a potential bias in this retrospective review, all radiologists were blinded to clinical information. Reported rates of symptom response vary between 66% and 100%, of marker response between 50% and 91%, and of morphologic (radiologic) response between 33% and 80%.18 Gupta et al. reviewed recent series of TACE for various neuroendocrine tumors and found the average rate of complete or partial radiologic response to be 32% (31 of 96 patients).11,19–24 Finally, symptomatic response was observed in 77% of patients in the present study. This is a particularly encouraging result given that most patients were on octreotide before TACE, and corroborates the results of others demonstrating the role of TACE in patients with octreotide-refractory symptoms.9–11
The median survival of 28.1 months in this study was not significantly different than survival of the larger group after the initial TACE procedure (33.3 months). This result again underscores the indolent nature of carcinoid tumors and the long-term survival possible, even with metastatic disease. Importantly, this finding suggests that repeat TACE has an important role in the management of progressive carcinoid metastases after initial TACE, providing symptom control and extension of survival similar to the first TACE procedure. Repeat TACE may be especially useful because patients with longstanding carcinoid metastases often have disabling symptoms refractory to medical management. Furthermore, the procedure was well tolerated with a low incidence of complications, making it well suited to a group of patients with advanced malignancy. Although we analyzed multiple factors related to the extent of primary tumor and patient response to first TACE, we were unable to identify any prognostic factors. Further studies in larger groups of patients may help to identify prognostic factors among this unique group of patients.
Conclusion
In this group of 27 patients undergoing repeat TACE for radiologic or symptomatic progression of hepatic carcinoid metastases, the procedure was well tolerated, with a small percentage of patients experiencing transient adverse effects. Interestingly, the incidence of complications was significantly lower in this group than in patients undergoing the first TACE. Radiologic, hormone, and symptomatic responses to repeat TACE were 60–80%; these results were not significantly different than among patients undergoing first TACE. The median overall survival of 28.1 months for repeat TACE was not different than that of patients undergoing first TACE, suggesting that repeat TACE is a useful and effective treatment for patients with progression of hepatic carcinoid metastases after previous regional embolic therapy. Repeat TACE should be considered at any point in the treatment algorithm of patients with progressive hepatic carcinoid metastases.
References
Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer 2003;97:934–959.
Madeira I, Terris B, Voss M, Denys A, Sauvanet A, Flejou JF, Vilgrain V, Belghiti J, Bernades P, Ruszniewski P. Prognostic factors in patients with endocrine tumors of the duodenopancreatic area. Gut 1998;43:422–427.
McEntee GP, Nagorney DM, Kvols LK, Moertel CG, Grant CS. Cytoreductive hepatic surgery for neuroendocrine tumors. Surgery 1990;108:1091–1096.
Osborne DA, Zervos EE, Strosberg J, Boe BA, Malafa M, Rosemurgy AS, Yeatman TJ, Carey L, Duhaine L, Kvols LK. Improved outcome with cytoreduction versus embolization for symptomatic hepatic metastases of carcinoid and neuroendocrine tumors. Ann Surg Oncol 2006;13:572–581.
Moertel CG, Johnson CM, McKusick MA, Martin JK Jr, Nagorney DM, Kvols LK, Kunselman S. The management of patients with advanced carcinoid tumors and islet cell carcinomas. Ann Intern Med 1994;120:302–309.
Schnirer II, Yao JC, Ahani HA. Carcinoid—a comprehensive review. Acta Oncol 2003;42:672–692.
Arnold R, Trautmann ME, Creutzfeldt W, Benning R, Neuhaus C, Jurgensen R, Stein K, Schafer H, Bruns C, Dennler HJ. Somatostatin analogue octreotide and inhibition of tumour growth in metastatic endocrine gastroenteropancreatic tumours. Gut 1996;38:430–438.
O’Toole D, Ruszniewski P. Chemoembolization and other ablative therapies for liver metastases of gastrointestinal tumours. Best Pract Res Clin Gastroenterol 2005;19:585–594.
Drougas JG, Lowell BA, Blair TK, Lopez RR, Wright JK, Chapman WC, Webb L, Mazer M, Meranze S, Pinson CW. Hepatic artery chemoembolization for management of patients with advanced metastatic carcinoid tumors. Am J Surg 1998;175:408–412.
Eriksson BK, Larsson EG, Skogseid BM, Lofberg AM, Lorelius LE, Oberg KE. Liver embolizations of patients with malignant neuroendocrine gastrointestinal tumors. Cancer 1998;83:2293–2301.
Gupta S, Yao JC, Ahrar K, Wallace MJ, Morello FA, Madoff DC, Murthy R, Hicks ME, Ajani JA. Hepatic artery embolization and chemoembolization for treatment of patients with metastatic carcinoid tumors: the M.D. Anderson experience. Cancer J 2003;9:261–267.
Bloomston M, Al-Saif O, Klemanski D, Pinzone JJ, Martin EW, Palmer B, Guy G, Khabiri H, Ellison EC, Shah MH. Hepatic artery chemoembolization in 122 patients with metastatic carcinoid tumor: lessons learned. J Gastrointest Surg 2007;11:264-271.
Desai DC, O’Dorisio TM, Schirmer WJ, Jung SS, Khabiri H, Villanueva V, Martin EW Jr. Serum pancreastatin levels predict response to hepatic artery chemoembolization and somatostatin analogue therapy in metastatic neuroendocrine tumors. Regul Pept 2001;96:113–117.
Yao KA, Talamonti MS, Nemcek A, Angelos P, Chrisman H, Skarda J, Benson AB, Rao S, Joehl RJ. Indications and results of liver resection and hepatic chemoembolization for metastatic gastrointestinal neuroendocrine tumors. Surgery 2001;130:677–685.
Oberg K. The ultimate biochemical diagnosis of gastro-enteropancreatic tumours. Digestion 1996;57(suppl 1):45–47.
Stidsberg M, Oberg K, Li Q, Engstrom U, Lundqvist G. Measurements of chromogranin A, chromogranin B (secretogranin 1), chromogranin C (secretogranin II) and pancreastatin in plasma and urine from patients with carcinoid tumors and endocrine pancreatic tumors. J Endocrinol 1995;144:49–59.
Calhoun K, Toth-Fejel S, Cheek J, Pommier R. Serum peptide profiles in patients with carcinoid tumors. Am J Surg 2003;186:28–31.
Ruszniewski P, Malka D. Hepatic arterial chemoembolization in the management of advanced digestive endocrine tumors. Digestion 2000;62(Suppl I):79–83.
Roche A, Girish BV, de Baere T, Baudin E, Boige V, Elias S, Lasser P, Schlumberger M, Ducreux M. Trans-arterial chemoembolization as first-line treatment for hepatic metastases from endocrine tumors. Eur Radiol 2003;13:136–140.
Dominguez S, Denys A, Madeira I, Hammel P, Vilgrain V, Menu Y, Bernades P, Ruszniewski P. Hepatic arterial chemoembolization with streptozotocin in patients with metastatic digestive endocrine tumours. Eur J Gastroenterol Hepatol 2000;12:151–157.
Hajarizadeh H, Ivancev K, Mueller CR, Gletcher WS, Woltering EA. Effective palliative treatment of metastatic carcinoid tumors with intra-arterial chemotherapy/chemoembolization combined with octreotide acetate. Am J Surg 1992;163:479–483.
Kim YH, Ajani HA, Carrasco CH, Dumas P, Richli W, Lawrence D, Chuang V, Wallace S. Selective hepatic arterial chemoembolization for liver metastases in patients with carcinoid tumor or islet cell carcinoma. Cancer Investig 1999;17:474–478.
Ruszniewski P, Rougier P, Roche A, Legmann P, Sibert A, Hochlaf S, Ychou M, Mignon M. Hepatic arterial chemoembolization in patients with liver metastases of endocrine tumors. A prospective Phase II study in 24 patients. Cancer 1993;71:2624–2630.
Therasse E, Breittmayer F, Roche A, DeBaere T, Indushekar S, Ducreux M, Lasser P, Elias D, Rougier P. Transcatheter chemoembolization of progressive carcinoid liver metastases. Radiology 1993;189:541–547.
Varker KA, Campbell J, Shah MH. Phase II study of thalidomide in patients with metastatic carcinoid and islet cell tumors. Cancer Chemother Pharmacol; DOI 10.1007/s00280-007-0521-9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Varker, K.A., Martin, E.W., Klemanski, D. et al. Repeat Transarterial Chemoembolization (TACE) for Progressive Hepatic Carcinoid Metastases Provides Results Similar to First TACE. J Gastrointest Surg 11, 1680–1685 (2007). https://doi.org/10.1007/s11605-007-0235-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0235-7