Abstract
Background
The role of neoadjuvant chemotherapy (NCT) for high-risk soft tissue sarcoma (STS) is questioned. This study aimed to define which patients may experience a survival advantage with NCT.
Methods
All the patients from the U.S. Sarcoma Collaborative database (2000–2016) who underwent curative-intent resection of high-grade, primary truncal/extremity STS size 5 cm or larger were included in this study. The primary end points were recurrence-free survival (RFS) and overall survival (OS).
Results
Of the 4153 patients, 770 were included in the study. The median tumor size was 10 cm, and 669 of the patients (87%) had extremity tumors. The most common histology was undifferentiated pleomorphic sarcoma (UPS), found in 42% of the patients. Of the 770 patients, 216 (28%) received NCT. The patients who received NCT had deeper, larger tumors (p < 0.001). Of the patients with tumors 5 cm or larger and 8 cm or larger, NCT was not associated with improved RFS or OS. However for the patients with tumors 10 cm or larger, NCT was associated with improved 5-year RFS (51% vs 40%; p = 0.053) and 5-year OS (58% vs 47%; p = 0.043). By location, the patients with extremity tumors 10 cm or larger but not truncal tumors had improved 5-yearr RFS (54% vs 42%; p = 0.042) and 5-year OS (61% vs 47%; p = 0.015) with NCT. According to histology, no subtype had improved RFS or OS with NCT, although the patients with UPS had a trend toward improved 5-year RFS (56% vs 42%; p = 0.092) and 5-year OS (66% vs 52%; p = 0.103) with NCT.
Conclusion
For the patients with high-grade STS, NCT was associated with improved RFS and OS when tumors were 10 cm or larger and located in the extremity. However, no histiotype-specific advantage was identified. Future studies assessing the efficacy of NCT may consider focusing on these patients, with added focus on histology-specific strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Soft tissue sarcoma (STS) of the trunk and extremity are conventionally considered high-risk for distant recurrence if they are larger than 5 cm with intermediate- or high-grade histology.1 Although standard treatment with surgery and radiation provides local control, high-risk STS has a high propensity for distant spread, which leads to death from metastatic disease in up to 50% of patients.2,3
Perioperative chemotherapeutic strategies are used to reduce the risk of recurrent disease and to treat micro-metastases, increase the chances of limb salvage, and serve as a biologic test of chemo-responsiveness. The majority of clinical trials testing the efficacy of these regimens, however, are in the adjuvant setting and demonstrate only marginal survival benefit.4,5,6,–7 Even in the preoperative setting, few data exist to justify the use of neoadjuvant chemotherapy (NCT) for patients with high-risk STS, resulting in uncertainty as to which patients would most likely benefit.8,9
The rarity and heterogeneity of the biologic behavior among STS subtypes poses the largest obstacle in designing a study to demonstrate the efficacy of NCT in truncal and extremity STS. Previous studies have attempted to use strict tumor size cutoff values, specific sarcoma locations, and select histologic subtypes to select patients for randomized control trials, but these selection criteria often are disparate even among studies.10,11,12,13,14,15,–16
In this era of personalized medicine, in which individually tailored treatment strategies are key, a recent study from Gronchi et al.11 attempted to demonstrate the benefit of neoadjuvant histiotype-tailored chemotherapy regimens over standard regimens, but this study was unable to demonstrate a survival benefit with a histiotype-specific approach. Other groups have used nomograms and retrospective review of clinical data to identify clinical and pathologic factors associated with improved outcomes with NCT, but to date no consensus has been formed.17,18,19,20,–21 Collectively, these previous studies underscore the critical importance of selecting a uniform group of patients with STS when investigating the efficacy of chemotherapeutic treatment strategies.
Given the heterogeneous selection criteria in previous clinical trials, the current study aimed to define clinicopathologic factors related to improved survival with the use of NCT for patients who undergo curative-intent resection of high-risk truncal and extremity STS. We sought to identify specifically what tumor size, tumor location, and histologic subtype of STS would be related to improved outcomes with the use of NCT.
Methods
Patients were identified from the United States Sarcoma Collaborative (USSC) database, a collaboration of seven U.S.-based academic tertiary referral centers (Emory University, The Ohio State University, Stanford University, University of Chicago, Medical College of Wisconsin, Wake Forest University and Washington University in St. Louis). Institutional review board (IRB) approval was obtained from each institution before data collection.
All patients who underwent curative-intent resection of a high-grade, primary truncal or extremity STS larger than 5 cm were included in the study. Patients with multi-focal or recurrent tumors and those who died within 30 days after surgery were excluded. Patients who received only adjuvant chemotherapy also were excluded.
Clinicopathologic and survival data were collected using retrospective review of the electronic medical record. Pathologic examination of tissue specimens was reviewed by expert sarcoma pathologists at each institution. Staging was based on the American Committee on Cancer (AJCC) 7th edition guidelines.22 High-grade tumors were defined as French Federation Nationale des Centres de Lutte Contra le Cancer (FNCLCC) grades 2 or 3 (G2 or G3) per the AJCC tumor-node-metastasis (TNM) staging system. Tumor depth was defined as superficial or deep relative to the investing muscular fascia in the subcutaneous tissue (tumors superficial to the investing muscular fascia but with invasion into the fascia were classified as deep). Final resection status was defined as R0 (complete gross tumor clearance with negative microscopic margins), R1 (complete gross tumor clearance with positive microscopic margins), and R2 (incomplete gross tumor clearance).
The patients were analyzed at increasing tumor size values of 5 cm or larger, 8 cm or larger, and 10 cm or larger. The primary aim was to assess the association between the receipt of NCT and survival outcomes for each tumor size group. The primary end points were recurrence-free survival (RFS), defined as the time from the date of surgery to the date of first recurrence, and overall survival (OS), defined as the time from the date of surgery to the date of death. Disease recurrence was defined strictly as the radiographic recurrence of disease.
Statistical analysis was performed using SPSS 22.0 software (IBM Inc., Armonk, NY, USA). Chi-square analysis was used to compare categorical variables, and Student’s t test was used for continuous variables. Uni- and multivariable Cox regression analyses were used to determine the association of preoperative clinicopathologic factors and survival. Kaplan–Meier survival plots for RFS and OS were constructed to compare patients who did and did not receive NCT. Statistical significance was defined by a p value lower than 0.05.
Results
Of the 4153 patients in the database, 770 had primary high-grade tumors 5 cm or larger (≥ 8 cm: 529 patients; ≥ 10 cm: 411 patients). The clinical and pathologic factors are listed in Table 1. The average tumor size for our entire cohort was 12 ± 6 cm, and 87% (n = 669) of the patients with tumors 5 cm or larger had STS located in the extremity (89% of ≥ 8-cm tumors were in the extremity; 90% of ≥ 10-cm tumors were in the extremity).
The most common histologic type of tumor was undifferentiated pleomorphic sarcoma (UPS), found in 321 (42%) of the patients, followed by synovial sarcoma, found in 62 patients (8%), and myxofibrosarcoma, found in 69 patients (8%). Other histologic types represented were leiomyosarcoma, found in 50 patients (7%); dedifferentiated liposarcoma, found in 22 patients (3%); and myxoid liposarcoma, found in 15 patients (2%). For 216 patients (28%) with tumors 5 cm or larger, NCT was administered (≥ 8 cm: 168 patients [32%]; ≥ 10 cm: 138 patients [34%]), the majority of which was doxorubicin-based (≥ 5 cm: 163 patients [21%]; ≥ 8 cm: 128 patients [24%]; ≥ 10 cm: 104 patients [25%]).
In the entire cohort, the patients who received NCT were younger (age 51 vs 64 years; p < 0.001) and more likely to be male (62% vs 54%; p = 0.049) and functionally independent (98% vs 94%; p = 0.043) with deeper (98% vs 91%; p = 0.002) and larger tumors (13 vs 11 cm; p = 0.004) than the patients who did not receive chemotherapy. The median follow-up period was 26 months.
Tumor Size and Survival
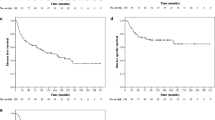
In the analysis of survival outcomes by tumor size for all tumor sites and histologies, the patients in our entire cohorts with tumors 5 cm or larger showed no association between NCT and improved RFS (5-year RFS: 52% vs 47%; p = 0.230) or OS (5-year OS: 62% vs 58%; p = 0.356) compared with no NCT (Fig. 1a, b). Similarly, for the patients with tumors 8 cm or larger, NCT was not associated with improved RFS (5-year RFS: 50% vs 42%; p = 0.148) or improved OS (5-year OS: 57% vs 52%; p = 0.205) compared with no NCT (Fig. 1c, d). However for the patients with tumors 10 cm or larger, the receipt of NCT was associated with improved RFS (5-year RFS: 51% vs 40%; p = 0.053) and improved OS (5-year OS: 58% vs 47%; p = 0.043) compared with no NCT (Fig. 1e, f).
Kaplan–Meier survival curves demonstrating the association of neoadjuvant chemotherapy with improved recurrence-free survival and overall survival for patients with soft tissue sarcoma (STS) larger than 10 cm (e, f), but not for patients with tumors larger than 5 cm (a, b) or larger than 8 cm (c, d)
Tumor Location and Survival
When tumors were stratified by location (trunk vs extremity), the patients with tumors 5 cm or larger and 8 cm or larger did not show an association of NCT with RFS or OS. Furthermore, among the patients with tumors 10 cm or larger in the trunk, NCT was not associated with improved RFS (5-year RFS: 24% vs 28%; p = 0.551) or improved OS (5-year OS: 30% vs 49%; p = 0.337) compared with no NCT (Fig. 2a, b). However for the patients with tumors 10 cm or larger in the extremity, NCT was associated with improved RFS (5-year RFS: 54% vs 42%; p = 0.042) and improved OS (5-year OS: 51% vs 47%; p = 0.015) compared with no NCT (Fig. 2c, d).
Tumor Histology and Survival
In the histology-specific analysis, no subtype (UPS, synovial sarcoma, or myxofibrosarcoma), regardless of tumor size or tumor location, was associated with RFS or OS. However, among the patients who had tumors 10 cm or larger with UPS histology, NCT showed a trend toward improved RFS (5-year RFS: 56% vs 42%; p = 0.092) and improved OS (5-year OS: 66% vs 52%; p = 0.103) compared with no NCT, although this difference was not statistically significant (Fig. 3a, b).
Cox Regression Analysis and Preoperative Factors
For the previously identified subset of patients with tumors 10 cm or larger located in the extremity, preoperative factors associated with RFS and OS were considered. In the univariate analysis, increasing body mass index (BMI) was associated with decreased RFS (hazard ratio [HR] 1.03; 95% confidence interval [CI] 1.0–1.1; p = 0.018) and the receipt of NCT was associated with increased RFS (HR 0.70; 95% CI 0.50–0.99; p = 0.043). In the multivariable analysis, only increasing BMI was associated with RFS (HR 1.03; 95% CI 1.0–1.1; p = 0.015; Table 2). In the univariate analysis, decreased OS was associated with increasing tumor size (HR 1.03; 95% CI 1.0–1.06; p = 0.038), whereas improved OS was associated with receipt of neoadjuvant radiation (HR 0.64; 95% CI 0.45–0.93; p = 0.018) and receipt of NCT (HR 0.63; 95% CI 0.43–0.92; p = 0.016). In the multivariable analysis, tumor size was associated with worse OS (HR 1.03; 95% CI 1.00–1.01; p = 0.033), and receipt of NCT was associated with improved OS (HR 0.68; 95% CI 0.46–0.99; p = 0.044).
Discussion
In our multi-institutional cohort of patients, NCT was associated with improved RFS and OS survival for patients who underwent resection of a primary high-grade extremity STS larger than 10 cm, but not larger than 5 or 8 cm. These findings were not seen in patients with truncal tumors, although the subset analysis for patients with truncal tumors likely was underpowered. Histology-specific advantages with NCT were not identified, although this analysis likely was underpowered as well. Based on these findings, future studies assessing the efficacy of NCT may consider amending the selection criteria to focus on patients with high-grade extremity STS larger than 10 cm, with an added focus on histology-specific strategies.
Increasing tumor size is used as a prognostic marker in the AJCC 8th edition, in which tumors 5–10 cm are T2 lesions, tumors 10–15 cm are T3 lesions, and tumors larger than 15 cm are T4 lesions.23 Patients with high-grade T2 lesions are classified as having stage 3A disease, whereas patients with high-grade T3 or T4 tumors are classified as having stage 3b disease. Our study mirrors this size discrimination because we did not see a survival advantage with NCT for patients with T2 lesions, but only for those with lesions classified as T3 or higher.
Previous studies investigating the usefulness of NCT retrospectively have used a variety of size cutoffs including 5 and 8 cm.10,17,18,–19,21,24 Similar to our study, Grobmyer et al.18 found in their retrospective review of 356 patients with high-grade STS larger than 5 cm that the survival advantage seen with NCT likely was driven by those tumors larger than 10 cm.
A variety of prospective studies that have investigated the role of chemotherapy in the adjuvant and neoadjuvant settings have used either no size cutoff or cutoffs of STS larger than 5 cm or larger than 8 cm.10,11,12,–13,15,16 Although the study by Woll et al.7 using doxorubicin/ifosfamide and lenograstim was in the adjuvant setting (European Organisation for Research and Treatment of Cancer [EORTC] 62931), it showed that the patients most likely to benefit from chemotherapy had larger, high-grade tumors. A more recent analysis of the EORTC 62931 used the prognostic nomogram Sarculator to stratify the study patients into three categories using patient age, tumor size, tumor grade, and tumor histology.25 This updated analysis found that the cohort of patients predicted to have the lowest OS based on the Sarculator was the only group to show an improved survival with adjuvant chemotherapy (HR 0.46). These findings again are concordant with the results in our study demonstrating a survival advantage with NCT for patients with large, high-risk tumors.
When tumor location is considered, primary tumor site is regarded as the chief tumor characteristic for STS in guiding treatment decisions. For example, STS originating in the retroperitoneum is staged and managed separately from those originating in the trunk/extremity or head and neck.22,23 Most staging systems and treatment strategies, however, combine superficial truncal and extremity STS, and little published literature separates these two entities. The aforementioned randomized control trial from Woll et al.7 suggested that patients with large, grade 3 extremity tumors were more likely to benefit from adjuvant chemotherapy than patients with tumors located in the trunk or head and neck, although this difference was not statistically significant in the final analysis.7
The current study found that patients with extremity tumors, but not truncal tumors, larger than 10 cm had a survival advantage with NCT. The analysis of the truncal cohort likely was underpowered because 41 patients had truncal tumors larger than 10 cm, and 362 patients had extremity tumors larger than 10 cm. Further study to investigate the role of NCT for patients with high-grade truncal STS is required.
Besides tumor site and grade, the histologic subtype of STS primarily drives the biologic behavior for the majority of tumors. Due to the rarity of STS, histology-specific analysis has been difficult to achieve in both prospective and retrospective studies. Even in the current study, although the highest represented histologic subtype was UPS, in 42% of the patients, the next most common subtypes were synovial sarcoma, in only 8% of the patients, and myxofibrosarcoma in 8% of the patients.
Given these limitations in the investigation of specific histologic subtype responses to NCT, the randomized phase 3 clinical trial of Gronchi et al.11 was especially illuminating to our understanding of histology-tailored treatment strategies. The study randomized 287 patients with five specific histologic subtypes (UPS, myxoid liposarcoma, synovial sarcoma, malignant peripheral nerve sheath tumor, and leiomyosarcoma) to either a standard chemotherapeutic regimen or a histology-tailored regimen. Although no benefit was demonstrated by the histology-tailored strategy, this study confirmed the ability to recruit patients with STS to investigate histology-specific treatment responses in a randomized setting. Given our observations in the retrospective cohort of the current study, in which patients with UPS had a trend toward improved RFS survival and OS with NCT, we agree with the Italian group that the search for histology-specific treatment regimens in STS should continue.
Our study was limited by its retrospective design, which posed several limitations in analysis. The number of cycles, the administration, and the type of NCT administered between institutions was not standardized during the study period. Although the majority of patients who received NCT underwent anthracycline-based chemotherapy, this study had no standard protocol. Furthermore, the decision to administer neoadjuvant radiotherapy also was not standardized between institutions, and although accounted for in our multivariable model of patients with extremity tumors larger than 10 cm, our study did not investigate the role of radiation in these patients. Finally, surgical conduct and pathologic examination was not standardized between institutions, although all the institutions included in this multi-center study are considered high-volume centers for sarcoma expertise.
Conclusion
In our multi-institutional cohort, NCT was associated with improved RFS and OS for patients with resection of high-grade extremity STS 10 cm or larger but not STS 5 cm or larger or 8 cm or larger. Future studies assessing the efficacy of NCT may consider amending the selection criteria to focus on these patients, with added focus on histology-specific strategies.
References
Davis LE, Ryan CW. Preoperative therapy for extremity soft tissue sarcomas. Curr Treat Options Oncol. 2015;16:25.
Singh AS, Eilber FC. Neoadjuvant therapy for soft-tissue sarcomas: one size does not fit all. Oncology Williston Park. 2016;30:107–8.
Weitz J, Antonescu CR, Brennan MF. Localized extremity soft tissue sarcoma: improved knowledge with unchanged survival over time. J Clin Oncol. 2003;21:2719–25.
Bramwell VH, Mouridsen HT, Santoro A, Blackledge G, Somers R, Verwey J, et al. Cyclophosphamide versus ifosfamide: final report of a randomized phase II trial in adult soft tissue sarcomas. Eur J Cancer Clin Oncol. 1987;23:311–21.
Judson I, Verweij J, Gelderblom H, Hartmann JT, Schöffski P, Blay JY, et al. Doxorubicin alone versus intensified doxorubicin plus ifosfamide for first-line treatment of advanced or metastatic soft-tissue sarcoma: a randomised controlled phase 3 trial. Lancet Oncol. 2014;15:415–23.
Lorigan P, Verweij J, Papai Z, Rodenhuis S, Le Cesne A, Leahy MG, et al. Phase III trial of two investigational schedules of ifosfamide compared with standard-dose doxorubicin in advanced or metastatic soft tissue sarcoma: a European Organisation for Research and Treatment of Cancer Soft Tissue and Bone Sarcoma Group Study. J Clin Oncol. 2007;25:3144–50.
Woll PJ, Reichardt P, Le Cesne A, Bonvalot S, Azzarelli A, Hoekstra HJ, et al. Adjuvant chemotherapy with doxorubicin, ifosfamide, and lenograstim for resected soft-tissue sarcoma (EORTC 62931): a multicentre randomised controlled trial. Lancet Oncol. 2012;13:1045–54.
Benjamin RS. Adjuvant and neoadjuvant chemotherapy for soft tissue sarcomas: a personal point of view. Tumori. 2017;103:213–6.
Rothermundt C, Fischer GF, Bauer S, Blay JY, Grünwald V, Italiano A, et al. Pre- and postoperative chemotherapy in localized extremity soft tissue sarcoma: a European Organization for Research and Treatment of Cancer Expert Survey. Oncologist. 2018;23:461–7.
Gortzak E, Azzarelli A, Buesa J, Bramwell VH, Van Coevorden F, Van Geel AN, et al. A randomised phase II study on neo-adjuvant chemotherapy for “high-risk” adult soft-tissue sarcoma. Eur J Cancer. 2001;37:1096–103.
Gronchi A, Ferrari S, Quagliuolo V, Broto JM, Pousa AL, Grignani G, et al. Histotype-tailored neoadjuvant chemotherapy versus standard chemotherapy in patients with high-risk soft-tissue sarcomas (ISG-STS 1001): an international, open-label, randomised, controlled, phase 3, multicentre trial. Lancet Oncol. 2017;18:812–22.
Kraybill WG, Harris J, Spiro IJ, Ettinger DS, DeLaney TF, Blum RH, et al. Long-term results of a phase 2 study of neoadjuvant chemotherapy and radiotherapy in the management of high-risk, high-grade, soft tissue sarcomas of the extremities and body wall: Radiation Therapy Oncology Group Trial 9514. Cancer. 2010;116:4613–21.
Kraybill WG, Harris J, Spiro IJ, Ettinger DS, DeLaney TF, Blum RH, et al. Phase II study of neoadjuvant chemotherapy and radiation therapy in the management of high-risk, high-grade, soft tissue sarcomas of the extremities and body wall: Radiation Therapy Oncology Group Trial 9514. J Clin Oncol. 2006;24:619–25.
Meyer JM, Perlewitz KS, Hayden JB, Doung YC, Hung AY, Vetto JT, et al. Phase I trial of preoperative chemoradiation plus sorafenib for high-risk extremity soft tissue sarcomas with dynamic contrast-enhanced MRI correlates. Clin Cancer Res. 2013;19:6902–11.
Spencer RM, Junior SA, Ferreira FO, Stevanato Filho PR, Kupper BE, Silva ML, et al. Neoadjuvant hypofractionated radiotherapy and chemotherapy in high-grade extremity soft tissue sarcomas: phase 2 clinical trial protocol. JMIR Res Protoc. 2017;6:e97.
Tseng WW, Zhou S, To CA, Thall PF, Lazar AJ, Pollock RE, et al. Phase 1 adaptive dose-finding study of neoadjuvant gemcitabine combined with radiation therapy for patients with high-risk extremity and trunk soft tissue sarcoma. Cancer. 2015;121:3659–67.
Bedi M, King DM, Shivakoti M, Wang T, Zambrano EV, Charlson J, et al. Prognostic variables in patients with primary soft tissue sarcoma of the extremity and trunk treated with neoadjuvant radiotherapy or neoadjuvant sequential chemoradiotherapy. Radiat Oncol. 2013;8:60.
Grobmyer SR, Maki RG, Demetri GD, Mazumdar M, Riedel E, Brennan MF, et al. Neoadjuvant chemotherapy for primary high-grade extremity soft tissue sarcoma. Ann Oncol. 2004;15:1667–72.
Mahmoud O, Tunceroglu A, Chokshi R, Benevenia J, Beebe K, Patterson F, et al. Overall survival advantage of chemotherapy and radiotherapy in the perioperative management of large extremity and trunk soft tissue sarcoma; a large database analysis. Radiother Oncol. 2017;124:277–84.
Mullen JT, Kobayashi W, Wang JJ, Harmon DC, Choy E, Hornicek FJ, et al. Long-term follow-up of patients treated with neoadjuvant chemotherapy and radiotherapy for large, extremity soft tissue sarcomas. Cancer. 2012;118:3758–65.
Pasquali S, Colombo C, Pizzamiglio S, Verderio P, Callegaro D, Stacchiotti S, et al. High-risk soft tissue sarcomas treated with perioperative chemotherapy: improving prognostic classification in a randomised clinical trial. Eur J Cancer. 2018;93:28–36.
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual (7th ed.). New York: Springer; 2010.
Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK (eds) AJCC Cancer Staging. 8th ed. vol. 8. New York: Springer; 2017.
Mack LA, Crowe PJ, Yang JL, Schachar NS, Morris DG, Kurien EC, et al. Preoperative chemoradiotherapy (modified Eilber protocol) provides maximum local control and minimal morbidity in patients with soft tissue sarcoma. Ann Surg Oncol. 2005;12:646–53.
Pasquali S, Pizzamiglio S, Touati N, Litiere S, Marreaud S, Kasper B, et al. The impact of chemotherapy on survival of patients with extremity and trunk wall soft tissue sarcoma: revisiting the results of the EORTC-STBSG 62931 randomised trial. Eur J Cancer. 2019;109:51–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
No financial or material disclosures to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zaidi, M.Y., Ethun, C.G., Tran, T.B. et al. Assessing the Role of Neoadjuvant Chemotherapy in Primary High-Risk Truncal/Extremity Soft Tissue Sarcomas: An Analysis of the Multi-institutional U.S. Sarcoma Collaborative. Ann Surg Oncol 26, 3542–3549 (2019). https://doi.org/10.1245/s10434-019-07639-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07639-7